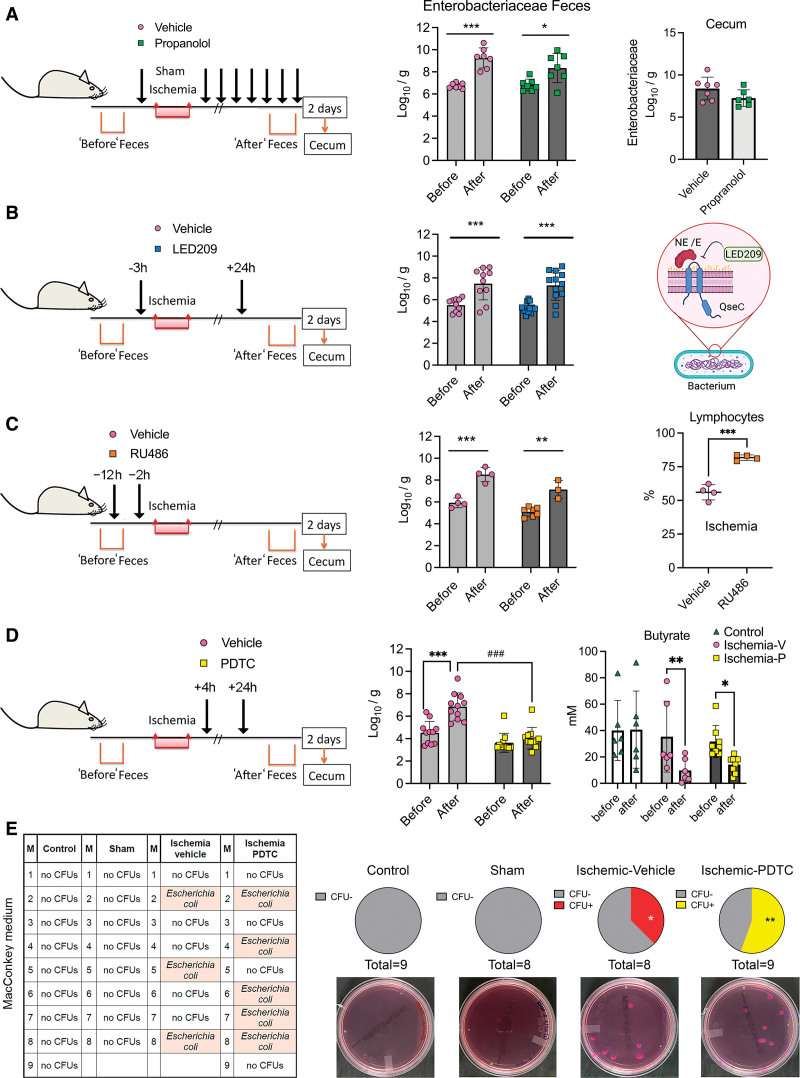
Figure 6.
The postischemic Enterobacteriaceae bloom is dependent on gut inflammation but does not mediate lung colonization with opportunistic Enterobacteria. Mice received treatments aimed to attenuate the Enterobacteriaceae expansion induced by stroke, as assessed in feces obtained before ischemia and 2 d postischemia. In some groups, we studied the cecal bacteria 2 d postischemia. Values are the mean±SD (Log10 colony forming units [CFUs]/g feces), symbols correspond to individual mice. We analyzed feces data with 2-way ANOVA-repeated measures design/Sidak multiple comparison test, and cecal data with Student t test. A, Mice were treated with propranolol (30 mg/kg; n=7) or vehicle (saline; n=7) IP immediately before ischemia, 0, 4, 8, 12, 24, 28, 32, and 36 h postischemia. The feces after ischemia showed increase in Enterobacteriaceae in the vehicle (***P=0.0009) and propranolol (*P=0.0348) groups. B, Mice received treatment with bacterial membrane-bound histidine sensor kinase quorum-sensing (QseC) inhibitor N-phenyl-4-(3-phenylthioureido)benzenesulfonamide (LED209; 16 mg/kg; n=12) or vehicle (n=10) orally 3 h before ischemia and 24 h postischemia. Fecal Enterobacteria increased after ischemia compared to before ischemia in both groups, (vehicle:**P=0.0042; LED209:***P=0.001; 2-way ANOVA-repeated measures design/Sidak test). LED209 inhibits the binding of catecholamines to the bacterial Qsec receptor (created by BioRender.com). C, Mice received RU486 (25 mg/kg; n=4) or vehicle (n=7) 12 h and 2 h before ischemia. Ischemia increased Enterobacteriaceae in feces of vehicle (***P=0.0002) and RU486 (**P=0.0093) groups. The % of lymphocytes (mean±SD) was higher after RU486 than vehicle (n=4 per group; P<0.001, Mann-Whitney U test). RU486 increased mortality (see Figure S7C). D, Mice received pyrrolidine dithiocarbamate (PDTC; 25 mg/kg) or vehicle (n=11 per group) IP 4 and 24 h postischemia. Ischemia increased Enterobacteriaceae in the vehicle (***P<0.001) but not the PDTC (P=0.5715) groups. Fecal Enterobacteriacea content after ischemia was lower in the PDTC than the vehicle group (***P<0.001). Ischemic mice, both vehicle (n=6) and PDTC (n=8) groups showed reduced butyrate vs the value before ischemia (**P=0.0063 and *P=0.0322, respectively; 2-way ANOVA-repeated-measure design/Šídák test), whereas controls (n=6) did not. E, The lungs of control (n=9), sham (n=8), or ischemic mice receiving either PDTC (n=9) or vehicle (n=8) were seeded on MacConkey agar, which selects Gram− bacteria. There was no bacterial growth in lungs of control or sham mice, but we detected colonies in ischemic mice receiving vehicle or PDTC (*P=0.027 and **P=0.006 vs sham, and *P=0.022 and **P=0.004 vs control, respectively). There were no differences between mice receiving vehicle or PDTC (P=0.228; 1-sided χ2). By matrix-assisted laser desorption/ionization-time-offlight mass spectrometry, we identified Escherichia coli. E indicates epinephrine; M, the mouse code number per group; and NE, norepinephrine.