Abstract
Articular cartilage repair is a sophisticated process that has is being recently investigated. There are several different approaches that are currently reported to promote cartilage repair, like cell-based therapies, biologics, and physical therapy. Cell-based therapies involve the using stem cells or chondrocytes, which make up cartilage, to promote the growth of new cartilage. Biologics, like growth factors, are also being applied to enhance cartilage repair. Physical therapy, like exercise and weight-bearing activities, can also be used to promote cartilage repair by inducing new cartilage growth and improving joint function. Additionally, surgical options like osteochondral autograft, autologous chondrocyte implantation, microfracture, and others are also reported for cartilage regeneration. In the current literature review, we aim to provide an up-to-date discussion about these approaches and discuss the current research status.
Keywords: chondrogenesis, osteoarthritis, tissue engineering, mesenchymal stem cells, surgical repair
Introduction
Articular cartilage, a form of connective tissue, covers the surface of bodily joints like the hip and knee. It is a smooth and durable tissue that provides a low-friction surface for bones to move against each other. This is due to its unique structure and composition. The collagen fibers in the cartilage give it strength and elasticity, while the high-water content helps to lubricate the joint and absorb shock. Chondrocytes, which are the cells that produce and maintain cartilage, also have a vital role in maintaining its integrity and health.1
However, when this tissue is damaged, it can lead to significant pain and mobility issues since it is difficult to regenerate because it is avascular.2 Articular cartilage damage might develop due to various factors, such as injury, overuse, or degenerative diseases such as osteoarthritis. Younger individuals may experience cartilage damage because of sports injuries, while older individuals may experience it because of natural wear and tear on the joints. Risk factors for cartilage damage include being overweight, having a history of joint injuries, and having certain genetic conditions. The commonest cartilage damage is associated with osteoarthritis, a degenerative condition resulting in the cartilage breakdown in a joint.3 Osteoarthritis is marked by cartilage degeneration, and bone spurs formation, leading to significant pain and limited mobility. Moreover, cartilage damage can lead to joint degeneration and even disability in severe cases, greatly impacting a person’s quality of life.4,5
Current practices used for cartilage damage and repair include a range of options like medications, rest, physical therapy, and surgical procedures.6,7 The intensity of inflammation and pain can be decreased by medications like non-steroidal anti-inflammatory drugs (NSAIDs). Improving strength and flexibility of affected joint might also be achieved by physical therapy. Surgical approaches, like osteochondral autograft transplantation system (OATS), autologous chondrocyte implantation (ACI), and microfracture may be necessary in some cases, particularly when there is severe joint degeneration or a lack of response to other treatments. Moreover, cellular therapy has been introduced in this field to promote cartilage repair and regeneration with promising results.8 Mesenchymal stromal cells (MSCs) differentiations into chondrocytes have been studied, leading to the formation of cartilaginous materials. In laboratory studies, MSCs were able to form cartilage-like tissue when cultured with the proper growth factors and scaffolds.9 Additionally, MSCs have been shown to produce molecules that promote the growth and maintenance of cartilage, such as collagen and proteoglycans.6,8 In the current literature review, we aim to discuss the current practices used for articular cartilage repair.
Methods
A comprehensive search was run through academic databases such as PubMed, Scopus, and Web of Science to find relevant articles. No limitations were applied to the search whether by country, date, or language of publication to retrieve as much evidence. However, we mainly focused on studies published within the last ten years to make the current discussion up-to-date. The search was performed using different keywords related to the field of this literature review, such as “articular cartilage”, “cartilage repair”, “cartilage regeneration”, and “chondrocyte transplantation”. Our evidence was generated from original investigations mainly and reviews were considered and reviewed to extract any relevant information or articles.
Microfracture Technique
Microfracture is a surgical modality that can be applied for cartilage damage with standard arthroscopy portals drill holes.10 The procedure involves making small fractures in the bone beneath the damaged cartilage, which stimulates the growth of new cartilage. The technique is usually conducted on patients with small to medium size cartilage defects. It involves using a sharp instrument to create multiple small fractures in the underlying bone, which bleeds and forms a clot. The clot, in turn, leads to forming of a fibrocartilage repair tissue. A literature review of microfracture for treating articular cartilage damage found that the procedure can significantly enhance function and pain within a short period.11 Nevertheless, Kreuz et al demonstrated that repaired tissues gradually deteriorate within 18–24 months following knee surgery because of increased susceptibility to mechanical forces. Overall, it was reported that microfracture surgery increases the production of fibrocartilage, which is biomechanically and chemically not as effective as hyaline cartilage.
In terms of the specific outcomes of microfracture, studies have found that the procedure can lead to enhancements in knee function and pain, together with an increase in the amount of cartilage in the knee.12 In a meta-analysis of five trials assessing the effectiveness of microfracture of the knee, Negrin et al13 indicated that the modality is associated with a significant postoperative clinical improvement. However, various limitations and significant heterogeneity among the included trials were reported by the authors. In 2022, Fortier et al14 published another meta-analysis to assess the clinical and MRI findings of microfracture of knee focal chondral lesions conducted with and without augmentation. After analyzing the results of 14 studies that recruited 744 patients, the authors found that microfracture combined with augmentation was associated with a remarkable enhancement in different scores compared to the other group. Besides, it is vital to consider that microfracture is most suitable in cases with small to medium-sized cartilage defects and may not be suitable for larger defects.15–19 Additionally, the success of the procedure may be influenced by the patient’s age and overall health, together with the specific type and location of the cartilage damage.
Nano-fracture, on the other hand, is a more novel surgical approach that enhances cartilage surfacing characteristics and increases bone marrow access by developing deeper cell channels in a more reproducible way.20 Another alternative approach is subarachnoid abrasions or drillings, done by K wires or drill bits within cartilage defects and up to the subchondral bone.21 A motorized burr usually does debride chondral defects. However, it has been shown that cyst formation, hypertrophy, and thermal necrosis might complicate this approach.22 Accordingly, evidence indicates that microfracture should be considered superior to this technique.23 In addition, a 43-month follow-up study showed that improvements in clinical outcomes of small-to-medium-sized osteochondral lesions were similar between microfracture and subchondral drilling techniques.24
Osteochondral Grafting
Osteochondral grafting is a surgical procedure that aim to transplant healthy cartilage and bone from one body region to an injured one. The goal of the procedure is to repair or replace the damaged tissue and restore normal joint function.25–27 One of the most used techniques for osteochondral grafting is ACI. This procedure involves harvesting healthy cartilage cells from the patient’s own body, growing them in a lab, and then transplanting them back into the damaged area.28 Studies have shown that ACI can effectively repair cartilage defects and improve joint function. Nevertheless, the process requires a lot of technical skill and requires specialized equipment and expertise.29–31 Another technique that has been used for osteochondral grafting is the use of allografts, which are transplantations of tissue from a donor. This technique has the advantage of being readily available, but it is related to an elevated risk of rejection and infection.6,7,26,27
Mosaicplasty and OATS are the two types of osteochondral grafting. Both techniques involve transplanting healthy bone and cartilage from one body area to an impacted one. Mosaicplasty is a surgical technique that involves the transplanting small plugs of sound bone and cartilage from a non-weight-distributed joint area to a damaged one. The plugs are typically taken from the patient’s own body and are carefully matched to the size and shape of the defect. The plugs are then placed into the defects using small drilling instruments. The aim of this technique is to repair the defect and normalize joint function. Mosaicplasty has been shown to be effective for treating small to medium-sized defects. However, it is not recommended for larger defects or for patients with significant joint degeneration.32–35
OATS is a surgical modality that is done by transplanting cylindrical plugs of sound bone and cartilage from a non-weight-distributing joint region to a damaged one. OATS procedure is similar to mosaicplasty, but the plugs are cylindrical and are typically taken from the patient’s body. The plugs are then placed within defects using a special drill, and it targets repairing the damage and regain sound joint functions. OATS has been shown to be effective for treating small to medium-sized defects, and it is recommended for larger defects or for patients with significant joint degeneration.6,7,33 Both Mosaicplasty and OATS have been extensively studied and were deemed safe and effective for treating knee defects. These procedures were reportedly related to improved patient outcomes, including reduced pain and improved function. However, it is essential to consider the need for long-term follow-up studies to fully understand the long-term effectiveness and safety of these procedures.7 Table 1 presents the advantages and disadvantages of all surgical techniques that might be used for cartilage repair. It should be noted that the appropriateness of a certain technique relies on the individual patient’s case and should be discussed with a specialist. Not all techniques are available in every location, and some are still considered experimental.
Table 1.
Advantages and Disadvantages of the Different Surgical Techniques Reported for Cartilage Repair
| Technique | Advantages | Disadvantages |
|---|---|---|
| Microfracture | Minimally invasive procedure- Cost-effective- Can be performed arthroscopically- Low risk of complications- Can be used for small to medium-sized cartilage defects | May not be suitable for large cartilage defects - Limited long-term success rates - May not be as durable as other techniques - Recovery time can be longer |
| Osteochondral Autograft Transfer System (OATS) | Considered the gold standard for cartilage repair - Can be applied for large cartilage defects - Provides long-term success rates - Durable and provides good mechanical strength | Invasive procedure - Requires a second surgical site for donor tissue - Risk of adverse events related to the donor site - Long recovery time |
| Autologous Chondrocyte Implantation (ACI) | Can be applied for large cartilage injuries - Provides long-term success rates - Durable and provides good mechanical strength - No need for a second surgical site | Invasive procedure - Requires laboratory cultivation of chondrocytes - Risk of complications associated with the implantation process - Long recovery time |
| Allograft Cartilage Implantation | Can be applied for large cartilage defects - No need for a second surgical site | Risk of disease dissemination with allograft tissue - Risk of immune response to the allograft tissue - Limited long-term success rates |
| Matrix-induced Autologous Chondrocyte Implantation (MACI) | Good repair potential, normal hyaline cartilage formed, less invasive than traditional ACI | High cost, long recovery time, risk of complications |
Cellular Therapy
Overview
MSCs are a type of adult stem cell investigated for their potential in repairing cartilage damage. MSCs can differentiate into various cell types, including cartilage cells, and have been shown to have anti-inflammatory and regenerative characteristics. In terms of regenerating cartilage damage, MSCs differentiations into chondrocytes have been studied, leading to the formation of cartilaginous materials. In laboratory studies, MSCs were able to form cartilage-like tissue when cultured with the proper growth factors and scaffolds.9 Additionally, MSCs have been shown to produce molecules that promote the growth and maintenance of cartilage, such as collagen and proteoglycans.6,8
MSCs have also been studied for their ability to modulate the immune response in conditions such as osteoarthritis. MSCs have been shown to reduce inflammation and promote healing in animal models of osteoarthritis. This is thought to be owing to the capability of MSCs to suppress the actions of pro-inflammatory cells and promote the activity of anti-inflammatory cells. Another area of research for MSCs in cartilage repair is their potential use in cell-based therapies. In these therapies, MSCs are isolated from a patient’s own tissue and then expanded in the laboratory before being re-injected into the affected joint.36 This approach avoids the need for invasive surgery and the use of foreign materials, such as artificial implants. Additionally, the use of a patient’s own cells reduces the risk of rejection or immune response. In clinical trials, MSCs have been shown to be safe and well tolerated in humans, with minimal side effects reported. However, the results of these studies are still preliminary, and more research is warranted to determine the long-term safety and efficacy of MSC-based therapies for cartilage repair.
Overall, MSCs have shown promise in the treatment of cartilage damage and repair. Their ability to differentiate into cartilage cells and modulate the immune response make them an attractive option for cell-based therapies. However, more research is needed to fully understand the mechanisms of MSCs action and to optimize the conditions for their use in clinical practice.37–39 It is important to mention that MSCs are not a panacea for the cartilage repair, there are still many challenges to overcome before these cells can be used in a clinical setting. There is a need for more research to understand the optimal conditions for MSC proliferation, survival, and differentiation in vivo, as well as the optimal routes of administration and cell dosages. Additionally, more studies are warranted to assess the prolonged effectiveness and safety of MSC-based therapies for cartilage repair. Despite these challenges, treating damaged cartilages by MSC is promising, and further research in this area could lead to new and effective treatments for this debilitating condition.8,40,41
Among the challenges that might hinder using MSC is their long-term effectiveness and safety, which has been investigated by some studies. All indicators of cartilage regeneration were steady throughout a seven-year follow-up period, as reported by Park et al,42 which provides cause for optimism. Moreover, high tibial osteotomies with and without BMSCs were compared for their long-term (over 10 years) efficacy by Yamasaki et al.43 There was no statistically significant change in Hospital for Special Surgery Knee-Rating Scale ratings between both groups at any time throughout the study’s follow-up period. Seven patients out of a total of 12 in the initial cohorts have accessible follow-up data. Another long-term (follow-up for ten years) cohort study also compared the safety and efficacy of BMSCs and ACI in 36 patients and found that both modalities had comparable outcomes at the end of the follow-up period, providing evidence for the safe and efficacious administration of BMSCs for cartilage repair.44 Favorable findings were also reported in a 5-year follow-up report, which demonstrated that the outcomes of BMSCs for osteoarthritis were favorable, although the reported outcomes were for only three patients. Other 2-year follow-up studies can also be found in the literature.45,46 However, the results of these studies might be biased due to remarkable heterogeneities between the study groups, and long-term outcomes cannot be ruled out due to the inadequate follow-up period.
The risk of tumor formation after cellular therapy represents the major challenge when it comes to assessing the long-term safety of these modalities. The possibility of malignant transformation after in vitro growth was first observed in early studies.47,48 However, it was later discovered that the discrepancies may have resulted from cell line cross-contamination,49 and subsequent evaluations have tended to back up the safety of BMSCs.50,51 Wakitani et al52 conducted a clinical investigation with 41 patients who had intra-articular BMSC implantation and found no evidence of tumor development up to 137 months postoperatively. In line with the positive safety data presented in these studies, Teo et al44 indicated that no clinical indications of tumor development in their BMSC group was noticed at up to 10 years of follow-up.
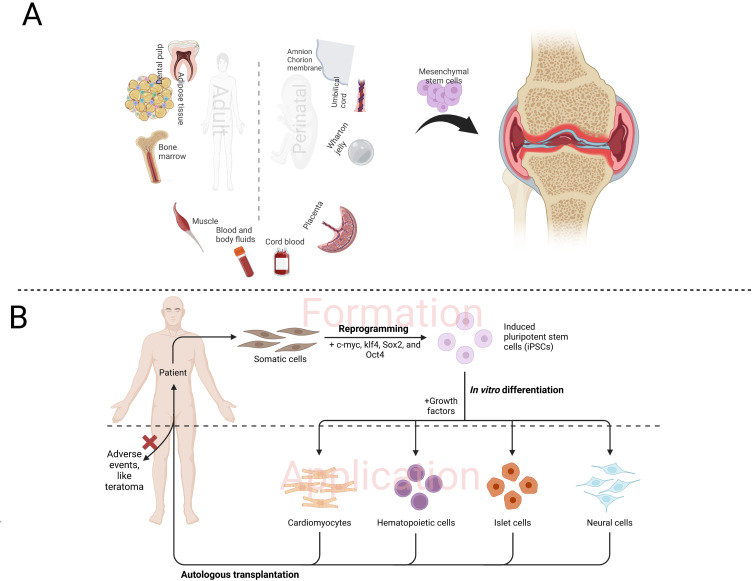
MSCs can be obtained from different sources, like adipose tissue, peripheral blood, and bone marrow (Figure 1A).9,53 Although the efficacy of these modalities has been indicated, various issues, like in vitro premature differentiation, and stem cell heterogeneity remain unsolved.8,54 In contrast to the bone marrow, which is the traditional source of MSCs, adipose tissue-derived MSCs (AMSCs) are gaining popularity because of their accessibility, purportedly increased proliferative ability, and anti-inflammatory characteristics. In addition to being given as a culture expanded MSC population, AMSCs may also be given as a part of a combination of heterogeneous cells called Stromal Vascular Fraction (SVF),55 which includes AMSCs along with other cell types such as pericytes, endothelial cells, smooth muscle cells, fibroblasts, and so on. Although AMSCs are present in SVF, they cannot be considered MSCs according to the precise definition since they express various cell markers and have different features.56
Figure 1.
Sources and application of mesenchymal stem cells (A) and induced pluripotent cells (B) for articular cartilage repair.
Clinical results for patients with cartilage injuries may be improved by MSC-based treatments due to their ability to stimulate the regeneration of hyaline-like cartilage. This disease-modifying strategy is quite unlike the standard palliative care approach. Immunohistological staining of type II collagen or expression of glycosaminoglycan in the regenerated tissue reminiscent of hyaline cartilage has been used in previous in vitro investigations to demonstrate the chondrogenic differentiation potential of AMSCs.57–59 The safety of administering MSCs has also been assessed in animal experiments,60,61 lending support to the in vitro findings. Histological findings concerning type II collagen production and integration, as well as biochemical findings, such as an increase in the glycosaminoglycans content, indicate the ability of MSCs isolated from bone marrow and synovium to cause hyaline-like cartilage regeneration. Administration of AMSCs to human knees has been linked to possible cartilage repair in early investigations.62 Biomarker analyses, imaging findings, and histology findings all point to the existence of hyaline-like cartilage regeneration.63 Histological staining performed by Koh et al64 showed that patients who received microfracture in conjunction with AMSC administration showed a higher degree of staining for safranin O and type II collagen, indicating the presence of hyaline cartilage regeneration. The Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) software compares the shape and signal intensity of the imaged regenerated cartilage to that of the surrounding natural hyaline cartilage. Because of this, it may be inferred that the regenerated cartilage has hyaline-like features from the increased MOCART score after AMSC delivery.63 The quality of the regenerated cartilage was evaluated by Freitag et al using T2-weighted imaging in addition to MOCART, and they discovered that the cartilage gradually matured over time.65,66 These findings support the hypothesis that AMSCs may give rise to human cartilage with properties similar to hyaline. However, the long-term effects of AMSC treatment on cartilage healing are uncertain, with the average follow-up duration being just 18.3 months.63 After two years post-treatment, cartilage degeneration was found by Jo et al.67 This may have been owing to the knee joint being desensitized to AMSC therapy or simply the necessity for another AMSC injection.
Promising findings in cartilage repair were also found with the application of induced pluripotent stem cells (iPSCs) (Figure 1B).68 These modalities might surpass the above limitations. However, genomic modifications remain a controversial issue that intervenes against their clinical application. Genetically modified cells were also reported as effective candidates for tissue regeneration since they can induce the synthesis of hyaline matrix, chondrogenic differentiation, together with production of pro-inflammatory mediators.69
Paracrine factors are released by cells in the form of EVs, such as exosomes. Exosomes are prevalent in all body fluids, including saliva, blood, urine, and milk,70–73 and serve a role in cell-cell communication. Their payload is cell-specific.74 Repair of injured cartilage may be aided by exosomes.75,76 Stem cell differentiation is boosted by exosomes.77,78 Injured cartilage additionally benefits from their ability to dampen inflammation.79 In order to reduce immune rejection during cartilage healing, exosomes are used.80 Hyaline cartilage development is also a potential outcome of exosome therapy. The use of EVs in treatment may reduce inflammation. Exosomes generated from MSCs have been shown to inhibit IL-1 production.81 Inflammatory responses during disc degeneration are also associated with IL-1, the most prominent proinflammatory mediator.82,83 By inhibiting inflammatory mediators and NLRP3 inflammasome activation, exosomes generated from mesenchymal stem cells were shown to decrease the course of intervertebral disc (IVD) degeneration in separate research.84 Pyroptosis is a kind of programmed cell death induced by proinflammatory signals, although it may be avoided by inhibiting the NLRP3 pathway. Regulation of pyroptosis and inhibition of the NLRP3 pathway by exosomal miR-410 from MSCs. Macrophage polarization has recently been the subject of therapy for osteoarthritis. Macrophages are immune cells that may be either proinflammatory (M1) or anti-inflammatory (M2).85 They are located in the synovial lining. Exosomes extracted from BMSCs have been shown to decrease inflammation by modulating macrophage polarization, namely by preventing the development of M1 macrophages and encouraging the creation of M2 macrophages.86
Various in vivo and animal studies investigated the administration of EVs for cartilage repair. In an animal model of osteoarthritis, He et al found that exosomes produced from BMSCs increased collagen type II synthesis and decreased MMP13 protein expression.87 In vitro research on degenerated nucleus pulposus cells demonstrated that BMSC-derived exosomes stimulated ECM synthesis.88 Therefore, it seems that EVs have distinct functions in restoring cartilage ECM. Although chondrocyte numbers are modest in normal cartilage, these cells play an important role in cartilage regeneration by synthesizing extracellular matrix. Since chondrocyte numbers decrease after cartilage damage, some therapeutic intervention is necessary to keep them at a stable level. Stem cell differentiation into chondrocytes is one method for keeping the chondrocyte population stable. By blocking the Notch1 pathway, EVs from nucleus pulposus cells direct MSC to develop into cells similar to those seen in the nucleus pulposus.89 Chondrogenic differentiation may also be targeted by miRNA, a component of EVs. In their study, Li et al90 found that miR-8485 from exosomal chondrocytes stimulated differentiation of BMSCs into chondrocytes by activating the Wnt/-catenin pathways. Improving cartilage regeneration requires not only the differentiation of stem cells into chondrocytes but also the proliferation of these cells at the site of damage. MiRNA is one example of EV cargo that has been proven to stimulate chondrocyte proliferation in research settings.91–93 EV treatment may prevent further chondrocyte depletion from apoptosis and autophagy. It was shown by Cheng et al94 that miR-21 in exosomes produced from mesenchymal stem cells inhibited apoptosis in cells of the nucleus pulposus. Similarly, EVs have been demonstrated to be useful in preventing IVD degeneration due to apoptosis triggered by the endoplasmic reticulum.95,96 The number of chondrocytes may be kept constant throughout cartilage healing by preventing apoptosis and promoting cell growth.
Tissue Engineering
Tissue engineering is a captivating and cutting-edge method for regenerating the tissue found in joints.97 The technique involves the utilization of growth factors (GF), scaffolds, and cells to replicate the intricate three-dimensional microenvironment present in joints, which necessitates the collaboration between these various elements. However, reproducing this complexity is essential and there are still many challenges that need to be addressed, such as determining the optimal cell population, the suitable scaffold materials, and the appropriate GF applications.98,99 Two categories have been suggested for cartilage repair by tissue engineering, including scaffold-based and independent methods.
Scaffolds
Scaffold-dependent approaches use synthetic or natural biomaterials to create an environment that supports cell growth and interactions, while independent methods do not rely on scaffolds.100 Various natural materials have been reported in the literature for cartilage repair and regeneration (Table 2). Hydrogel-based scaffolds have become a popular treatment strategy for cartilage defects. They can be injected to fill irregular shaped defects, mimic the natural environment and be minimally invasive. Recently, sol-gel phase transition-generated thermogels have also been applied for cartilage regeneration. One example is a PLGA-PEG-PLGA thermogel that solidifies at body temperature and has demonstrated encouraging outcomes in repairing a full-thickness cartilage defect of a rabbit model. Although initial mechanical stability is a major characteristic of scaffolds, they have numerous drawbacks such as toxicity associated with degradation, hindrance to remodeling, stress shielding, and alteration of cell characteristics.100 Therefore, researchers have focused on innovating scaffold-free approaches. For instance, cohesive tissue microarchitecture can be successfully produced by 3D bioprinting, which entails maintains a production with characteristics like in vivo conditions.101 Hydrogels are frequently employed as the printing medium, a method known as bio-ink dependent hybrid bioprinting.101,102 The selection of bioink is vital as it can impact cell-matrix interactions and cell spreading, and the chondrocyte phenotype can differ in hyaline cartilage and fibrocartilage.103
Table 2.
Advantages, Disadvantages, and Sources of Common Natural Products for Cartilage Regeneration and Repair
| Material | Advantages | Disadvantages | Sources |
|---|---|---|---|
| Collagen | It is a natural and biocompatible material, promotes cell growth and differentiation | Not very stable | Animal sources such as bones, tendons, skin, and cartilage |
| Chitosan | Biocompatible, non-toxic, promotes cell growth and differentiation | Poor mechanical properties | Shells of crustaceans such as shrimp, crab, and lobster |
| Hyaluronan | Lubricates joints, promotes cell growth and differentiation | Expensive to produce | Rooster comb, umbilical cord, and synovial fluid |
| Alginate | Non-toxic, biocompatible, can be used in hydrogels | Poor mechanical properties | Brown seaweed |
| Fibrin | Promotes cell growth and differentiation, forms a strong clot | Limited degradation | Blood plasma |
| Polylactic acid (PLA) | Biocompatible, can be used in 3D printing | Poor mechanical properties | Renewable resources such as corn starch and sugarcane |
| Polyethylene glycol (PEG) | Biocompatible, can be used in hydrogels | Expensive to produce | Petroleum-based or biosynthetic |
| Polycaprolactone (PCL) | Biocompatible, can be used in 3D printing | Poor mechanical properties | Renewable resources such as castor oil and sugarcane |
| Silk fibroin | Biocompatible, strong and flexible | Expensive to produce | Silkworm cocoons |
| Gelatin | Biocompatible, can be used in hydrogels | Poor mechanical properties | Animal by-products such as bones and skin |
| Polyvinyl alcohol (PVA) | Biocompatible, can be used in hydrogels | Poor mechanical properties | Petroleum-based or biosynthetic |
| Agarose | Biocompatible, can be used in hydrogels | Expensive to produce | Red seaweed |
| Cellulose | Biocompatible, abundant, and renewable | Poor mechanical properties | Plant sources such as wood and cotton |
| Gellan gum | Biocompatible, can be used in hydrogels | Expensive to produce | Bacteria |
| Chondroitin sulfate | Promotes cell growth and differentiation | Expensive to produce | Animal sources such as cartilage and bones |
| Hydrogel-based scaffolds | Biocompatible, can mimic the extracellular matrix | Poor mechanical properties | Natural or synthetic polymers, like chitosan, collagen, and hyaluronan, alginate |
Another scaffold-free technique is cell-sheet engineering, where transplantable hyaline-like cartilage tissue can be deployed through 3D MSC sheets, which has demonstrated encouraging results in chondrogenic differentiation.104 Currently, in vitro investigations are the main source of evidence regarding the function of tissue microenvironment in regulating articular cartilage and chondrocyte phenotype, indicating the need for future in vivo investigations. Having more insight into how MSCs and chondrocytes are impacted by microenvironment might aid in developing novel therapeutic approaches. For example, the application of scaffolds with chondrogenic GFs might enhance implantation parameters and boost cartilage synthesis.105
Moreover, scaffolds serve as time-controlled means of distribution for EVs by sequestering them at the damaged area and distributing them at regular intervals. Diffusion, polymer breakdown and degradation, and swelling are among mechanisms that might lead to the release of medicines or EVs from a scaffold.106 Scaffolds, either solid or hydrogel, are required to capture EVs and sustain their release. One of the most popular hydrophilic polymers utilized in cartilage tissue engineering is hydrogel. It may be used as a cartilage replacement due to its favorable mechanical properties.107 Hydrogel, which may be made from either natural or synthetic polymers to resemble the ECM, will regulate the release of EVs that are encapsulated inside it. Exosomes produced from stem cells may be trapped within a photo-induced crosslinking hydrogel to speed up cartilage healing.108 ECM and gelatin methacrylate hydrogel scaffolds impregnated with embryonic stem cells related EVs were shown to stimulate cartilage regeneration by Chen et al.109 Thus, research suggests that the transport of EVs for cartilage healing relies heavily on biomaterial. Research into the potential uses of different biomaterials for EV delivery in cartilage regeneration is warranted.
Growth Factors and Platelet-Rich Plasma
Natural GFs and anti-inflammatory agents are becoming a prevalent treatment for various musculoskeletal disorders. These biologic compounds can accelerate tissue healing and regeneration through various mechanisms, such as modulation of metalloproteinases and inflammatory markers, cell recruitment, and matrix remodeling and synthesis. Additionally, GF can control stem cell differentiation and protein synthesis, influencing cellular interactions. Specific GF, such as BMP-2 (Bone Morphogenetic Protein 2), VEGF (Vascular endothelial growth factor), and TGF-β1 (Transforming growth factor beta 1), regulate osteogenesis, angiogenesis, and chondrogenesis, respectively.110 The potential role of GF in regenerating tissues and reducing pain has sparked attention in their application as therapeutics for musculoskeletal injuries.
Recent advancements in understanding the role and importance of GF in tissue engineering have led to deeper discoveries and research in this field. GF promote and facilitate new tissue regeneration through regulation of cellular protein synthesis and interaction with defined transmembrane receptors. GF binding to these receptors stimulates cell signal transduction pathways, which in turn triggers cell differentiation, growth, proliferation, adhesion, survival, and migration. While a great therapeutic potential has been reported with GF application for cartilage repair and regeneration, healthcare authorities have not approved the clinical use.
Obtaining physiological proportions of GFs is feasible through an economic source, that is platelet-rich plasma (PRP). The efficacy and safety of this modality has been widely approved since it was applied for tissue regeneration in different medical fields. PRP is mainly composed of highly concentrated platelets within a blood derivative product, where regeneration characteristics can be observed in these platelets since they contain effective GFs. For instance, it has been reported that various GFs were included in α platelet granules, like IGF-1 (Insulin-like Growth Factor 1), FGF (Fibroblast growth factor), EGF (Epidermal growth factor), VEGF, TGF-β1, and PDGF (Platelet-derived growth factor) (Table 3). Clinically, the application of PRP was evidenced to be effective, safe, and feasible because it can be easily prepared. Moreover, it has been successfully applied together with scaffolds and microfracture surgical techniques for cartilage repair and regeneration. Intra-articular application of PRP has been widely evidenced for managing osteoarthritis, affecting the knee particularly. However, specifying the most suitable PRP remains controversial since different types with various characteristics and compositions are available due to different preparation techniques.
Table 3.
A Summary to Most Common Growth Factors Used for Cartilage Repair and Regeneration
| Growth Factor | Mechanism of Action | Delivery System | Time of Delivery | Dose* |
|---|---|---|---|---|
| Platelet-derived growth factor (PDGF) | Stimulate chondrocyte proliferation and matrix production | Hydrogel | Immediate | 10–100 ng/mL |
| Fibroblast growth factor (FGF) | Nanoparticle | Immediate | 10–100 ng/mL | |
| Insulin-like growth factor (IGF) | Hydrogel | Immediate | 10–100 ng/mL | |
| Vascular endothelial growth factor (VEGF) | Hydrogel | Immediate | 10–100 ng/mL | |
| Bone morphogenetic protein (BMP) | Microsphere | Immediate | 2–20 ng/mL | |
| Epidermal growth factor (EGF) | Hydrogel | Immediate | 10–100 ng/mL | |
| Transforming growth factor-beta (TGF-beta) | Microsphere | Immediate | 2–20 ng/mL | |
| Interleukin-1 (IL-1) | Hydrogel | Immediate | 10–100 ng/mL | |
| Platelet-rich plasma (PRP) | Contains various growth factors that promote tissue repair | Injected | Immediate | Varies |
Note: *Doses are remarkably variable and are usually determined by different factors, including patient’s status, severity of damage, and type of therapy used.
Small Molecules
Small molecules are widely studied for their potential in cartilage repair and regeneration. The main goal of these studies is to find new ways to stimulate the cartilage regeneration and to promote the growth of new cartilage tissue. The main targets of these small molecules are the signaling pathways, enzymes, and receptors involved in cartilage formation and maintenance.111,112 One of the main ways that small molecules can promote cartilage repair and regeneration is by stimulating chondrogenesis, inducing cartilage formation. Studies have shown that promoting stem cell differentiation into chondrocytes can be done by small molecules such as BMP-7, BMP-2, and TGF-beta. Furthermore, they can promote the synthesis of collagen, and proteoglycans, which mainly form the extracellular matrix (ECM) of cartilage.113
Another way that small molecules can promote cartilage repair and regeneration is by modulating ECM. Some studies have shown that small molecules such as PEG (Polyethylene glycol)-hydrogels and hyaluronic acid can promote the formation of new ECM and aid in cartilage repair and regeneration.114–116 Additionally, other small molecules can target enzymes such as MMPs (Matrix Metalloproteinases) and aggrecanases that degrade cartilage, helping to preserve the cartilage matrix. Inhibiting inflammation is also an important aspect for promoting cartilage repair and regeneration. Inflammation can cause damage to cartilage and inhibit the repair process. Studies have shown that small molecules such as celecoxib and curcumin can reduce inflammation and promote cartilage repair and regeneration by inhibiting the production of inflammatory mediators such as prostaglandins and TNF (tumor necrosis factor)-alpha.117
Examples of small molecules include Kartogenin, compound TD-198946, molecule [i,2], Salidroside, BNTA, and berberine chloride, which have been reported to stimulate chondrocyte differentiation and proliferation through different pathways, including regulation of CBFβ-RUNX1 signaling, upregulation of Runx1 expression, improving the transcription of chondrogenic markers including aggrecan and SOX9, and induction of superoxide anion elimination.111,113,116,118–124 Moreover, promoting angiogenesis is also essential for cartilage repair and regeneration. Blood vessels supply oxygen and nutrients to the cartilage, and without them, the repair process is hindered. Studies have shown that small molecules such as VEGF and FGF can promote the growth of new blood vessels and aid in cartilage repair and regeneration125,126 (Table 3). It is important to note that while small molecules have shown promising results in promoting cartilage repair and regeneration in preclinical studies, more clinical research is needed to confirm their safety and efficacy in humans. Additionally, it is important to consider the potential side effects and toxicity of these molecules, and to evaluate their long-term effectiveness.127
Pharmaco-Therapy
Various pharmacological modalities have been proposed for the management of articular cartilage injuries. However, the evidence supporting these treatments is limited and inconsistent. Non-steroidal anti-inflammatory drugs (NSAIDs) are the most used pharmacological treatment for articular cartilage injuries. These drugs reduce inflammation and pain, but their long-term use may have negative effects on cartilage repair. Studies have shown that NSAIDs inhibit the proliferation and differentiation of chondrocytes, the cells responsible for cartilage repair, and may delay healing. Therefore, the use of NSAIDs should be limited to the acute phase of injury and used with caution in chronic injuries.128–130 Glucocorticoids, another commonly used class of drugs based on their local anti-inflammatory action,131,132 have been shown to have long-term negative effects on cartilage repair. These drugs inhibit chondrocyte proliferation and matrix synthesis and may lead to chondrocyte death, in addition to having other adverse events.133–135 Therefore, the use of glucocorticoids for the treatment of articular cartilage injuries should also be limited.
Hyaluronic acid (HA) is a naturally occurring substance found in the synovial fluid of joints and were suggested to treat injured articular cartilages. Studies have indicated that HA can improve the functions of affected joints and decrease painful sensations in individuals with osteoarthritis by reducing oxygen free radicals-induced damage, decreasing inflammation mediated by reducing the production and release of arachnoid acid and prostaglandin E2, stimulating endogenous production of hyaluronic acid, and enhancing joint viscoelasticity.136,137 The favorable advantages were reported among various trials and reviews among patients with knee osteoarthritis.138 However, some limitations regarding intra-articular injection of such viscosupplements should be considered.139–143
Prolotherapy (or regenerative injection therapy) is a treatment that involves the injection of a solution (usually a mixture of dextrose and lidocaine) into the affected joint to stimulate the biological healing processes of the body. The theory behind prolotherapy is that the injection of the solution induces a controlled inflammatory response, leading to the recruitment of cells responsible for tissue repair and regeneration, such as mesenchymal stem cells, to the injury site.144,145 The evidence on the effectiveness of prolotherapy for the treatment of articular cartilage injuries is mixed. Evidence from animal studies indicates the cartilage-specific anabolic growth, and biopsies show the remarkable ability to form fibrocartilage, and hyaline-like cartilage mixtures.144 A meta-analysis of four randomized controlled trials, revealed that prolotherapy is remarkably superior to exercise for treating knee osteoarthritis. The authors of the review also pointed out that the studies included in the review had limitations related to the methodology, like inadequate population size, and that larger and more rigorous trials are warranted to establish the safety and efficacy of prolotherapy for the treatment of articular cartilage injuries.145 More recently, Wang et al146 published a meta-analysis of five studies that recruited 319 individuals and indicated the efficacy of hypertonic dextrose prolotherapy with a favorable safety profile. However, they also suggested that further investigations are warranted to evaluate the prolonged outcomes of these modalities and better understand the underlying mechanism.
Glucosamine and chondroitin sulfate are dietary supplements that are commonly used to treat osteoarthritis and other types of joint pain. Glucosamine is a naturally occurring compound that is believed to stimulate the production of proteoglycans that are vital components of cartilage. Chondroitin sulfate is a component of proteoglycans and is believed to protect cartilage from damage.147,148 The effectiveness of glucosamine and chondroitin sulfate for the treatment of articular cartilage injuries is mixed.149 Some studies have shown that these supplements can enhance the functions of the joints and decreases pain in individuals with osteoarthritis. However, other studies have failed to find significant benefits from the treatment. A meta-analysis, which included 29 randomized controlled trials, found that glucosamine and chondroitin sulfate alone, but not in combination, significantly reduce pain (as measured by VAS) in patients with knee osteoarthritis. However, the authors of the meta-analysis also noted that the included investigations had limitations related to the methodology, and that larger and more methodologically-enhanced investigations are warranted to establish the safety and efficacy of these supplements for treating injuries of articular cartilages.150 A more recent meta-analysis of randomized studies found the impact of chondroitin sulfate on pain to be moderate, with a significant impact on functional status. However, various limitations to these findings were reported, indicating the need for additional future studies.151
Miscellaneous Approaches
Several interventions have been studied to understand their effectiveness in treating cartilage damage, including exercise, physical therapy, braces, and weight loss. Exercise, specifically weight-bearing and muscle strengthening exercises, have been found to be beneficial in improving joint function and reducing pain in individuals with cartilage damage. Weight-bearing exercises such as walking, running, and hiking, help to promote the growth and repair of cartilage by providing the necessary mechanical stimulus.152–154 Moreover, muscle-strengthening exercises, such as resistance training and weightlifting, not only improve muscle strength but also help to take pressure off the affected joint, reducing pain and improving function. However, it has been previously demonstrated that combining dry needling with exercises is not very effective in reducing disability or pain.155 On the other hand, Tai Chi, a form of low-impact exercise, can also be effective in improving knee function and reducing pain in individuals with knee osteoarthritis.154 Favorable effects of muscle strengthening exercises were also reported for postmenopausal women with osteoarthritis in a systematic review by Alonso Pérez et al.156 Moreover, in cases with carpometacarpal joint osteoarthritis, a proprioceptive exercise program may enhance force sensing accuracy.157 Physical therapy can also be a highly effective intervention for cartilage damage. Physical therapists can provide manual therapy to reduce pain and inflammation,158 and education on how to properly move and protect the affected joint.159 Additionally, physical therapists can provide exercises that target the affected joint, including range of motion exercises and strength training, which can help to improve joint function and reduce pain.160 However, it has been shown that other approaches, like interferential therapy, therapeutic ultrasound, and transcutaneous nerve stimulation have negligible benefits on cartilage damage.161
Braces, such as knee or ankle braces, can provide support and reduce stress on the affected joint. These braces can help to reduce pain and improve function by redistributing the load on the joint and can also be helpful in individuals who have difficulty maintaining proper posture or alignment during movement.162,163 Weight loss is another important intervention for cartilage damage, as obesity is a risk factor for cartilage damage. Excess weight puts added stress on the joints, which can accelerate cartilage damage. By losing weight, the pressure on the joints is reduced, and the risk of cartilage damage progression is decreased.164,165
Limitations and Implications
Various techniques have been developed and tested for articular cartilage generation and repair. While these techniques have shown promising therapeutic potentials, various limitations still need to be addressed. For example, the long-term outcomes of these modalities are not yet fully understood, and there is a need for more research to better understand the mechanisms of cartilage repair and regeneration. The long-term safety of MSCs was reported in some studies. There is still a need for further evidence with larger randomized studies because of the biased designs of the currently available reports. However, clinicians are encouraged to start considering these promising modalities because of their favorable advantages and enhanced outcomes over other therapeutics with limited clinical capacities and favorable outcomes of regeneration and repair.
Another limitation is the difficulty in achieving adequate cell survival and integration into the host tissue with cell-based therapies. This is a significant challenge that needs to be addressed to enhance the outcomes of these therapies. Using synthetic and natural scaffolds in scaffold-based therapies is also limited by the difficulty in achieving optimal properties for cell growth and differentiation, as well as being able to interact with the host tissues. Additionally, the ability to compare and evaluate the results of different studies is limited by the shortage of using standardized methods and techniques among these studies, making it difficult to evaluate the effectiveness of these techniques and determine which methods are most effective for a given patient population. Future clinical studies are encouraged to strengthen the current evidence of human clinical applicability and safety of these approaches.
When researching EVs, it is crucial to have proper identification and potency requirements to assure quality control and consistency. Although there is compelling data supporting the utilization of EVs for cartilage healing, certain considerations are needed beforehand. Before using EVs in clinical practice, larger animal models ought to be researched. Large animal models allow for the study of partial- and full-thickness chondral, in addition to osteochondral repair.114 Due to the variable nature of EV content, further research on the selection and upkeep of EV parental cells is required. Targeted treatment is significant since no panacea exists. Given the difficulty of isolating EVs of high purity in big quantities, it is also important to find ways to maximize output from EV manufacturing on a massive scale. The most popular approach to EV isolation, ultracentrifugation, has drawbacks including poor purity and EV aggregation.115 Alternative methods, such as tangential flow filtering, exist for achieving repeatable manufacturing on a massive scale.116 There has to be uniformity in the procedures used to mass manufacture EVs for use as a therapeutic agent in cartilage repair. Additional investigations are needed to ensure the effectiveness and safety of engineered EVs for targeted cartilage treatment.
The right amount of EVs and how to administer them are also crucial. EVs are rapidly eliminated by the body’s circulatory system, requiring a greater dosage, or trapping in biomaterial to maintain their effectiveness. Hydrogel scaffolds have a promising potential as a transport medium. Despite the popularity of live cell transplantation, the lack of cells in EV-based treatment gives it a better possibility for healing. Current surgical procedures for repairing cartilage defects may be modified to include the implantation of EV-loaded scaffolds at the location of the lesion. It is envisaged that by optimizing the EV dose in the scaffold, this method may reduce the need for further procedures and improve postoperative patient comfort. Hyaline cartilage may be regenerated when EVs are employed therapeutically, such as in the case of an articular cartilage damage. The pharmacokinetics of EVs is another important factor in drug discovery. In addition, the product quality of EVs has to be standardized, including storage conditions (such as temperature and expiry date). The research on the role of EVs in repairing cartilage damage is encouraging, however there are several obstacles to the practical use of EVs for cartilage regeneration. Healthcare expenditures may be greatly reduced if the therapeutic potential of EVs was better understood and if more people had access to them.
Conclusion
Articular cartilage repair and regeneration is a complex field that has been the focus of numerous studies in recent years. Various treatment modalities have been reported, including interventional and conservative techniques. The main limitation of interventional techniques is the lack of long-term data supporting their feasibility in the clinical settings. Cellular therapies ACI seem to be the most favorable approaches with favorable outcomes and enhanced safety profiles. EVs may be designed and loaded with biomaterials to regulate their release, increasing their potential as a therapeutic tool. With the right plans in place, EV treatment for cartilage regeneration will become more widely available and efficient. If EV products are to be used in clinical settings, they will need to be standardized to assure their safety.
Funding Statement
This study was supported by Yantai Science and Technology Innovation Development Plan Project (No. 2022MSGY072), for development and research of autologous chondrocytes to construct living transparent Articular cartilage Implants.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sophia Fox AJ, Bedi A, Rodeo SA. The basic science of articular cartilage: structure, composition, and function. Sports Health. 2009;1(6):461–468. doi: 10.1177/1941738109350438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiang H, Jiang CC. Repair of articular cartilage defects: review and perspectives. J Formos Med Assoc. 2009;108(2):87–101. doi: 10.1016/s0929-6646(09)60039-5 [DOI] [PubMed] [Google Scholar]
- 3.Borrelli J, Olson SA, Godbout C, Schemitsch EH, Stannard JP, Giannoudis PV. Understanding articular cartilage injury and potential treatments. J Orthop Trauma. 2019;33(Suppl 6):S6–s12. doi: 10.1097/bot.0000000000001472 [DOI] [PubMed] [Google Scholar]
- 4.Chubinskaya S, Haudenschild D, Gasser S, Stannard J, Krettek C, Borrelli J. Articular cartilage injury and potential remedies. J Orthop Trauma. 2015;29(Suppl 12):S47–S52. doi: 10.1097/bot.0000000000000462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilder FV, Hall BJ, Barrett JP, Lemrow NB. History of acute knee injury and osteoarthritis of the knee: a prospective epidemiological assessment. The Clearwater Osteoarthritis Study. Osteoarthritis Cartilage. 2002;10(8):611–616. doi: 10.1053/joca.2002.0795 [DOI] [PubMed] [Google Scholar]
- 6.Liu Y, Shah KM, Luo J. Strategies for articular cartilage repair and regeneration. Front Bioeng Biotechnol. 2021;9:770655. doi: 10.3389/fbioe.2021.770655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solanki K, Shanmugasundaram S, Shetty N, Kim S-J. Articular cartilage repair & joint preservation: a review of the current status of biological approach. J Clin Orthopaed Trauma. 2021;22:101602. doi: 10.1016/j.jcot.2021.101602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roseti L, Grigolo B. Current concepts and perspectives for articular cartilage regeneration. J Exp Orthop. 2022;9(1):61. doi: 10.1186/s40634-022-00498-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang S, Tian G, Li X, et al. Research progress on stem cell therapies for articular cartilage regeneration. Stem Cells Int. 2021;2021:8882505. doi: 10.1155/2021/8882505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391:S362–9. doi: 10.1097/00003086-200110001-00033 [DOI] [PubMed] [Google Scholar]
- 11.Steadman JR, Rodkey WG, Briggs KK. Microfracture: its history and experience of the developing surgeon. Cartilage. 2010;1(2):78–86. doi: 10.1177/1947603510365533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erggelet C, Vavken P. Microfracture for the treatment of cartilage defects in the knee joint - A golden standard? J Clin Orthop Trauma. 2016;7(3):145–152. doi: 10.1016/j.jcot.2016.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Negrin L, Kutscha-Lissberg F, Gartlehner G, Vecsei V. Clinical outcome after microfracture of the knee: a meta-analysis of before/after-data of controlled studies. Int Orthop. 2012;36(1):43–50. doi: 10.1007/s00264-011-1364-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fortier LM, Knapik DM, Dasari SP, et al. Clinical and magnetic resonance imaging outcomes after microfracture treatment with and without augmentation for focal chondral lesions in the knee: a systematic review and meta-analysis. Am J Sports Med. 2022;3635465221087365. doi: 10.1177/03635465221087365 [DOI] [PubMed] [Google Scholar]
- 15.Goyal D, Keyhani S, Lee EH, Hui JH. Evidence-based status of microfracture technique: a systematic review of level I and II studies. Arthroscopy. 2013;29(9):1579–1588. doi: 10.1016/j.arthro.2013.05.027 [DOI] [PubMed] [Google Scholar]
- 16.Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37(10):2053–2063. doi: 10.1177/0363546508328414 [DOI] [PubMed] [Google Scholar]
- 17.Kreuz PC, Steinwachs MR, Erggelet C, et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14(11):1119–1125. doi: 10.1016/j.joca.2006.05.003 [DOI] [PubMed] [Google Scholar]
- 18.Bae DK, Yoon KH, Song SJ. Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy. 2006;22(4):367–374. doi: 10.1016/j.arthro.2006.01.015 [DOI] [PubMed] [Google Scholar]
- 19.Riedl M, Rupp M, Walter N, et al. Practical relevance of institutional guidelines in translational large animal studies of cartilage repair-a multidisciplinary survey. Medicina. 2022;58(12):254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao L, Goebel LKH, Orth P, Cucchiarini M, Madry H. Subchondral drilling for articular cartilage repair: a systematic review of translational research. Dis Model Mech. 2018;11(6):124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen H, Sun J, Hoemann CD, et al. Drilling and microfracture lead to different bone structure and necrosis during bone-marrow stimulation for cartilage repair. J Orthop Res. 2009;27(11):1432–1438. doi: 10.1002/jor.20905 [DOI] [PubMed] [Google Scholar]
- 22.Ozmeriç A, Alemdaroğlu KB, Aydoğan NH. Treatment for cartilage injuries of the knee with a new treatment algorithm. World J Orthop. 2014;5(5):677–684. doi: 10.5312/wjo.v5.i5.677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choi JI, Lee KB. Comparison of clinical outcomes between arthroscopic subchondral drilling and microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2140–2147. doi: 10.1007/s00167-015-3511-1 [DOI] [PubMed] [Google Scholar]
- 24.LaPrade RF, Botker JC. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20(7):e69–73. doi: 10.1016/j.arthro.2004.06.022 [DOI] [PubMed] [Google Scholar]
- 25.Rowland R, Colello M, Wyland DJ. Osteochondral autograft transfer procedure: arthroscopic technique and technical pearls. Arthrosc Tech. 2019;8(7):e713–e719. doi: 10.1016/j.eats.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cook JL, Stoker AM, Stannard JP, et al. A novel system improves preservation of osteochondral allografts. Clin Orthop Relat Res. 2014;472(11):3404–3414. doi: 10.1007/s11999-014-3773-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richter DL, Schenck RC, Wascher DC, Treme G. Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health. 2016;8(2):153–160. doi: 10.1177/1941738115611350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welch T, Mandelbaum B, Tom M. Autologous chondrocyte implantation: past, present, and future. Sports Med Arthrosc Rev. 2016;24(2):85–91. doi: 10.1097/jsa.0000000000000115 [DOI] [PubMed] [Google Scholar]
- 29.Mistry H, Connock M, Pink J, et al. Autologous chondrocyte implantation in the knee: systematic review and economic evaluation. Health Technol Assess. 2017;21(6):1–294. doi: 10.3310/hta21060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chimutengwende-Gordon M, Donaldson J, Bentley G. Current solutions for the treatment of chronic articular cartilage defects in the knee. EFORT Open Rev. 2020;5(3):156–163. doi: 10.1302/2058-5241.5.190031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brittberg M. Autologous chondrocyte implantation--technique and long-term follow-up. Injury. 2008;39(Suppl 1):S40–S49. doi: 10.1016/j.injury.2008.01.040 [DOI] [PubMed] [Google Scholar]
- 32.Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889–895. doi: 10.1056/nejm199410063311401 [DOI] [PubMed] [Google Scholar]
- 33.Bentley G, Greer RB. Homotransplantation of isolated epiphyseal and articular cartilage chondrocytes into joint surfaces of rabbits. Nature. 1971;230(5293):385–388. doi: 10.1038/230385a0 [DOI] [PubMed] [Google Scholar]
- 34.Reverte-Vinaixa MM, Joshi N, Diaz-Ferreiro EW, Teixidor-Serra J, Dominguez-Oronoz R. Medium-term outcome of mosaicplasty for grade III-IV cartilage defects of the knee. J Orthop Surg. 2013;21(1):4–9. doi: 10.1177/230949901302100104 [DOI] [PubMed] [Google Scholar]
- 35.Inderhaug E, Solheim E. Osteochondral autograft transplant (mosaicplasty) for knee articular cartilage defects. JBJS Essent Surg Tech. 2019;9(4):e34. doi: 10.2106/JBJS.ST.18.00113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park YB, Ha CW, Rhim JH, Lee HJ. Stem cell therapy for articular cartilage repair: review of the entity of cell populations used and the result of the clinical application of each entity. Am J Sports Med. 2018;46(10):2540–2552. doi: 10.1177/0363546517729152 [DOI] [PubMed] [Google Scholar]
- 37.Olmsted-Davis EA, Gugala Z, Camargo F, et al. Primitive adult hematopoietic stem cells can function as osteoblast precursors. Proc Natl Acad Sci U S A. 2003;100(26):15877–15882. doi: 10.1073/pnas.2632959100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kacena MA, Gundberg CM, Horowitz MC. A reciprocal regulatory interaction between megakaryocytes, bone cells, and hematopoietic stem cells. Bone. 2006;39(5):978–984. doi: 10.1016/j.bone.2006.05.019 [DOI] [PubMed] [Google Scholar]
- 39.Dominici M, Pritchard C, Garlits JE, Hofmann TJ, Persons DA, Horwitz EM. Hematopoietic cells and osteoblasts are derived from a common marrow progenitor after bone marrow transplantation. Proc Natl Acad Sci U S A. 2004;101(32):11761–11766. doi: 10.1073/pnas.0404626101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zaffagnini M, Boffa A, Andriolo L, Raggi F, Zaffagnini S, Filardo G. Orthobiologic injections for the treatment of hip osteoarthritis: a systematic review. J Clin Med. 2022;11(22):6663. doi: 10.3390/jcm11226663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cavallo C, Boffa A, de Girolamo L, et al. Bone marrow aspirate concentrate quality is affected by age and harvest site. Knee Surg Sports Traumatol Arthrosc. 2022. doi: 10.1007/s00167-022-07153-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park YB, Ha CW, Lee CH, Yoon YC, Park YG. Cartilage regeneration in osteoarthritic patients by a composite of allogeneic umbilical cord blood-derived mesenchymal stem cells and hyaluronate hydrogel: results from a clinical trial for safety and proof-of-concept with 7 years of extended follow-up. Stem Cells Transl Med. 2017;6(2):613–621. doi: 10.5966/sctm.2016-0157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamasaki S, Mera H, Itokazu M, Hashimoto Y, Wakitani S. Cartilage repair with autologous bone marrow mesenchymal stem cell transplantation: review of preclinical and clinical studies. Cartilage. 2014;5(4):196–202. doi: 10.1177/1947603514534681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Teo AQA, Wong KL, Shen L, et al. Equivalent 10-year outcomes after implantation of autologous bone marrow–derived mesenchymal stem cells versus autologous chondrocyte implantation for chondral defects of the knee. Am J Sports Med. 2019;47(12):2881–2887. doi: 10.1177/0363546519867933 [DOI] [PubMed] [Google Scholar]
- 45.Nejadnik H, Hui JH, Feng Choong EP, Tai BC, Lee EH. Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. Am J Sports Med. 2010;38(6):1110–1116. doi: 10.1177/0363546509359067 [DOI] [PubMed] [Google Scholar]
- 46.Chahla J, Piuzzi NS, Mitchell JJ, et al. Intra-articular cellular therapy for osteoarthritis and focal cartilage defects of the knee: a systematic review of the literature and study quality analysis. J Bone Joint Surg Am. 2016;98(18):1511–1521. doi: 10.2106/jbjs.15.01495 [DOI] [PubMed] [Google Scholar]
- 47.Houghton J, Stoicov C, Nomura S, et al. Gastric cancer originating from bone marrow-derived cells. Science. 2004;306(5701):1568–1571. doi: 10.1126/science.1099513 [DOI] [PubMed] [Google Scholar]
- 48.Røsland GV, Svendsen A, Torsvik A, et al. Long-term cultures of bone marrow-derived human mesenchymal stem cells frequently undergo spontaneous malignant transformation. Cancer Res. 2009;69(13):5331–5339. doi: 10.1158/0008-5472.Can-08-4630 [DOI] [PubMed] [Google Scholar]
- 49.Torsvik A, Røsland GV, Svendsen A, et al. Spontaneous malignant transformation of human mesenchymal stem cells reflects cross-contamination: putting the research field on track - letter. Cancer Res. 2010;70(15):6393–6396. doi: 10.1158/0008-5472.Can-10-1305 [DOI] [PubMed] [Google Scholar]
- 50.Casiraghi F, Remuzzi G, Abbate M, Perico N. Multipotent mesenchymal stromal cell therapy and risk of malignancies. Stem Cell Rev Rep. 2013;9(1):65–79. doi: 10.1007/s12015-011-9345-4 [DOI] [PubMed] [Google Scholar]
- 51.Peeters CM, Leijs MJ, Reijman M, van Osch GJ, Bos PK. Safety of intra-articular cell-therapy with culture-expanded stem cells in humans: a systematic literature review. Osteoarthritis Cartilage. 2013;21(10):1465–1473. doi: 10.1016/j.joca.2013.06.025 [DOI] [PubMed] [Google Scholar]
- 52.Wakitani S, Okabe T, Horibe S, et al. Safety of autologous bone marrow-derived mesenchymal stem cell transplantation for cartilage repair in 41 patients with 45 joints followed for up to 11 years and 5 months. J Tissue Eng Regen Med. 2011;5(2):146–150. doi: 10.1002/term.299 [DOI] [PubMed] [Google Scholar]
- 53.Reissis D, Tang QO, Cooper NC, et al. Current clinical evidence for the use of mesenchymal stem cells in articular cartilage repair. Expert Opin Biol Ther. 2016;16(4):535–557. doi: 10.1517/14712598.2016.1145651 [DOI] [PubMed] [Google Scholar]
- 54.Filardo G, Perdisa F, Roffi A, Marcacci M, Kon E. Stem cells in articular cartilage regeneration. J Orthop Surg Res. 2016;11:42. doi: 10.1186/s13018-016-0378-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bourin P, Bunnell BA, Casteilla L, et al. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 2013;15(6):641–648. doi: 10.1016/j.jcyt.2013.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–317. doi: 10.1080/14653240600855905 [DOI] [PubMed] [Google Scholar]
- 57.Hass R, Kasper C, Böhm S, Jacobs R. Different populations and sources of human mesenchymal stem cells (MSC): a comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal. 2011;9(1):1–14. doi: 10.1186/1478-811X-9-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vinardell T, Thorpe SD, Buckley CT, Kelly DJ. Chondrogenesis and integration of mesenchymal stem cells within an in vitro cartilage defect repair model. Ann Biomed Eng. 2009;37(12):2556–2565. doi: 10.1007/s10439-009-9791-1 [DOI] [PubMed] [Google Scholar]
- 59.de Vries–van Melle ML, Narcisi R, Kops N, et al. Chondrogenesis of mesenchymal stem cells in an osteochondral environment is mediated by the subchondral bone. Tissue Eng Part A. 2014;20(1–2):23–33. doi: 10.1089/ten.tea.2013.0080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bornes TD, Adesida AB, Jomha NM. Mesenchymal stem cells in the treatment of traumatic articular cartilage defects: a comprehensive review. Arthritis Res Ther. 2014;16(5):1–19. doi: 10.1186/s13075-014-0432-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.To K, Zhang B, Romain K, Mak C, Khan W. Synovium-derived mesenchymal stem cell transplantation in cartilage regeneration: a PRISMA review of in vivo studies. Front Bioengine Biotechnol. 2019;7:314. doi: 10.3389/fbioe.2019.00314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pak J. Regeneration of human bones in Hip osteonecrosis and human cartilage in knee osteoarthritis with autologous adipose-tissue-derived stem cells: a case series. J Med Case Rep. 2011;5:296. doi: 10.1186/1752-1947-5-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meng HY, Lu V, Khan W. Adipose tissue-derived mesenchymal stem cells as a potential restorative treatment for cartilage defects: a PRISMA review and meta-analysis. Pharmaceuticals. 2021;14(12):1280. doi: 10.3390/ph14121280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koh Y-G, Kwon O-R, Kim Y-S, Choi Y-J, Tak D-H. Adipose-derived mesenchymal stem cells with microfracture versus microfracture alone: 2-year follow-up of a prospective randomized trial. Arthroscopy. 2016;32(1):97–109. doi: 10.1016/j.arthro.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 65.Freitag J, Wickham J, Shah K, Li D, Norsworthy C, Tenen A. Mesenchymal stem cell therapy combined with arthroscopic abrasion arthroplasty regenerates cartilage in patients with severe knee osteoarthritis: a case series. Regen Med. 2020;15(8):1957–1977. doi: 10.2217/rme-2020-0128 [DOI] [PubMed] [Google Scholar]
- 66.Freitag J, Shah K, Wickham J, Li D, Norsworthy C, Tenen A. Evaluation of autologous adipose-derived mesenchymal stem cell therapy in focal chondral defects of the knee: a pilot case series. Regen Med. 2020;15(6):1703–1717. doi: 10.2217/rme-2020-0027 [DOI] [PubMed] [Google Scholar]
- 67.Jo CH, Chai JW, Jeong EC, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a 2-year follow-up study. Am J Sports Med. 2017;45(12):2774–2783. doi: 10.1177/0363546517716641 [DOI] [PubMed] [Google Scholar]
- 68.Castro-Viñuelas R, Sanjurjo-Rodríguez C, Piñeiro-Ramil M, et al. Induced pluripotent stem cells for cartilage repair: current status and future perspectives. Eur Cell Mater. 2018;36:96–109. doi: 10.22203/eCM.v036a08 [DOI] [PubMed] [Google Scholar]
- 69.Steinert AF, Nöth U, Tuan RS. Concepts in gene therapy for cartilage repair. Injury. 2008;39(Suppl 1):S97–113. doi: 10.1016/j.injury.2008.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sun Y, Huo C, Qiao Z, et al. Comparative proteomic analysis of exosomes and microvesicles in human saliva for lung cancer. J Proteome Res. 2018;17(3):1101–1107. doi: 10.1021/acs.jproteome.7b00770 [DOI] [PubMed] [Google Scholar]
- 71.Li S, Li Y, Chen B, et al. exoRBase: a database of circRNA, lncRNA and mRNA in human blood exosomes. Nucleic Acids Res. 2017;46(D1):D106–D112. doi: 10.1093/nar/gkx891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cho S, Yang HC, Rhee WJ. Development and comparative analysis of human urine exosome isolation strategies. Process Biochem. 2020;88:197–203. doi: 10.1016/j.procbio.2019.09.017 [DOI] [Google Scholar]
- 73.Vaswani K, Mitchell MD, Holland OJ, et al. A method for the isolation of exosomes from human and bovine milk. J Nutr Metab. 2019;2019:5764740. doi: 10.1155/2019/5764740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang Y, Liu Y, Liu H, Tang WH. Exosomes: biogenesis, biologic function and clinical potential. Cell Biosci. 2019;9(1):19. doi: 10.1186/s13578-019-0282-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sun H, Hu S, Zhang Z, Lun J, Liao W, Zhang Z. Expression of exosomal microRNAs during chondrogenic differentiation of human bone mesenchymal stem cells. J Cell Biochem. 2019;120(1):171–181. doi: 10.1002/jcb.27289 [DOI] [PubMed] [Google Scholar]
- 76.Vonk LA, van Dooremalen SFJ, Liv N, et al. Mesenchymal stromal/stem cell-derived extracellular vesicles promote human cartilage regeneration in vitro. Theranostics. 2018;8(4):906–920. doi: 10.7150/thno.20746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim YG, Park U, Park BJ, Kim K. Exosome-mediated bidirectional signaling between mesenchymal stem cells and chondrocytes for enhanced chondrogenesis. Biotechnol Bioprocess Engine. 2019;24(5):734–744. doi: 10.1007/s12257-019-0332-y [DOI] [Google Scholar]
- 78.Woo CH, Kim HK, Jung GY, et al. Small extracellular vesicles from human adipose-derived stem cells attenuate cartilage degeneration. J Extracell Vesicles. 2020;9(1):1735249. doi: 10.1080/20013078.2020.1735249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Harting MT, Srivastava AK, Zhaorigetu S, et al. Inflammation-stimulated mesenchymal stromal cell-derived extracellular vesicles attenuate inflammation. Stem Cells. 2018;36(1):79–90. doi: 10.1002/stem.2730 [DOI] [PubMed] [Google Scholar]
- 80.Abraham A, Krasnodembskaya A. Mesenchymal stem cell-derived extracellular vesicles for the treatment of acute respiratory distress syndrome. Stem Cells Transl Med. 2020;9(1):28–38. doi: 10.1002/sctm.19-0205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang S, Teo KYW, Chuah SJ, Lai RC, Lim SK, Toh WS. MSC exosomes alleviate temporomandibular joint osteoarthritis by attenuating inflammation and restoring matrix homeostasis. Biomaterials. 2019;200:35–47. doi: 10.1016/j.biomaterials.2019.02.006 [DOI] [PubMed] [Google Scholar]
- 82.Zhang J, Zhang J, Zhang Y, et al. Mesenchymal stem cells-derived exosomes ameliorate intervertebral disc degeneration through inhibiting pyroptosis. J Cell Mol Med. 2020;24(20):11742–11754. doi: 10.1111/jcmm.15784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yang W, Yu XH, Wang C, et al. Interleukin-1β in intervertebral disk degeneration. Clin Chim Acta. 2015;450:262–272. doi: 10.1016/j.cca.2015.08.029 [DOI] [PubMed] [Google Scholar]
- 84.Xia C, Zeng Z, Fang B, et al. Mesenchymal stem cell-derived exosomes ameliorate intervertebral disc degeneration via anti-oxidant and anti-inflammatory effects. Free Radic Biol Med. 2019;143:1–15. doi: 10.1016/j.freeradbiomed.2019.07.026 [DOI] [PubMed] [Google Scholar]
- 85.Fernandes TL, Gomoll AH, Lattermann C, Hernandez AJ, Bueno DF, Amano MT. Macrophage: a potential target on cartilage regeneration. Front Immunol. 2020;11:111. doi: 10.3389/fimmu.2020.00111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang J, Rong Y, Luo C, Cui W. Bone marrow mesenchymal stem cell-derived exosomes prevent osteoarthritis by regulating synovial macrophage polarization. Aging. 2020;12(24):25138–25152. doi: 10.18632/aging.104110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.He L, He T, Xing J, et al. Bone marrow mesenchymal stem cell-derived exosomes protect cartilage damage and relieve knee osteoarthritis pain in a rat model of osteoarthritis. Stem Cell Res Ther. 2020;11(1):276. doi: 10.1186/s13287-020-01781-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lu K, Li HY, Yang K, et al. Exosomes as potential alternatives to stem cell therapy for intervertebral disc degeneration: in-vitro study on exosomes in interaction of nucleus pulposus cells and bone marrow mesenchymal stem cells. Stem Cell Res Ther. 2017;8(1):108. doi: 10.1186/s13287-017-0563-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lan WR, Pan S, Li HY, et al. Inhibition of the Notch1 pathway promotes the effects of nucleus pulposus cell-derived exosomes on the differentiation of mesenchymal stem cells into nucleus pulposus-like cells in rats. Stem Cells Int. 2019;2019:8404168. doi: 10.1155/2019/8404168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li Z, Wang Y, Xiang S, et al. Chondrocytes-derived exosomal miR-8485 regulated the Wnt/β-catenin pathways to promote chondrogenic differentiation of BMSCs. Biochem Biophys Res Commun. 2020;523(2):506–513. doi: 10.1016/j.bbrc.2019.12.065 [DOI] [PubMed] [Google Scholar]
- 91.Rong Y, Zhang J, Jiang D, et al. Hypoxic pretreatment of small extracellular vesicles mediates cartilage repair in osteoarthritis by delivering miR-216a-5p. Acta Biomater. 2021;122:325–342. doi: 10.1016/j.actbio.2020.12.034 [DOI] [PubMed] [Google Scholar]
- 92.Yan L, Liu G, Wu X. Exosomes derived from umbilical cord mesenchymal stem cells in mechanical environment show improved osteochondral activity via upregulation of LncRNA H19. J Orthop Translat. 2021;26:111–120. doi: 10.1016/j.jot.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhao C, Chen JY, Peng WM, Yuan B, Bi Q, Xu YJ. Exosomes from adipose‑derived stem cells promote chondrogenesis and suppress inflammation by upregulating miR‑145 and miR‑221. Mol Med Rep. 2020;21(4):1881–1889. doi: 10.3892/mmr.2020.10982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cheng X, Zhang G, Zhang L, et al. Mesenchymal stem cells deliver exogenous miR-21 via exosomes to inhibit nucleus pulposus cell apoptosis and reduce intervertebral disc degeneration. J Cell Mol Med. 2018;22(1):261–276. doi: 10.1111/jcmm.13316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liao Z, Luo R, Li G, et al. Exosomes from mesenchymal stem cells modulate endoplasmic reticulum stress to protect against nucleus pulposus cell death and ameliorate intervertebral disc degeneration in vivo. Theranostics. 2019;9(14):4084–4100. doi: 10.7150/thno.33638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xiang H, Su W, Wu X, et al. Exosomes derived from human urine-derived stem cells inhibit intervertebral disc degeneration by ameliorating endoplasmic reticulum stress. Oxid Med Cell Longev. 2020;2020:6697577. doi: 10.1155/2020/6697577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Atala A, Kasper FK, Mikos AG. Engineering complex tissues. Sci Transl Med. 2012;4(160):160rv12. doi: 10.1126/scitranslmed.3004890 [DOI] [PubMed] [Google Scholar]
- 98.Camarero-Espinosa S, Rothen-Rutishauser B, Foster EJ, Weder C. Articular cartilage: from formation to tissue engineering. Biomater Sci. 2016;4(5):734–767. doi: 10.1039/C6BM00068A [DOI] [PubMed] [Google Scholar]
- 99.Beris AE, Lykissas MG, Papageorgiou CD, Georgoulis AD. Advances in articular cartilage repair. Injury. 2005;36(Suppl 4):S14–23. doi: 10.1016/j.injury.2005.10.007 [DOI] [PubMed] [Google Scholar]
- 100.Wasyłeczko M, Sikorska W, Chwojnowski A. Review of synthetic and hybrid scaffolds in cartilage tissue engineering. Membranes. 2020;10(11):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Moldovan NI, Moldovan L, Raghunath M. Of balls, inks and cages: hybrid biofabrication of 3D tissue analogs. Int J Bioprint. 2019;5(1):167. doi: 10.18063/ijb.v5i1.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Laternser S, Keller H, Leupin O, Rausch M, Graf-Hausner U, Rimann M. A novel microplate 3D bioprinting platform for the engineering of muscle and tendon tissues. SLAS Technol. 2018;23(6):599–613. doi: 10.1177/2472630318776594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Daly AC, Critchley SE, Rencsok EM, Kelly DJ. A comparison of different bioinks for 3D bioprinting of fibrocartilage and hyaline cartilage. Biofabrication. 2016;8(4):045002. doi: 10.1088/1758-5090/8/4/045002 [DOI] [PubMed] [Google Scholar]
- 104.Thorp H, Kim K, Kondo M, Grainger DW, Okano T. Fabrication of hyaline-like cartilage constructs using mesenchymal stem cell sheets. Sci Rep. 2020;10(1):20869. doi: 10.1038/s41598-020-77842-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chen L, Liu J, Guan M, Zhou T, Duan X, Xiang Z. Growth factor and its polymer scaffold-based delivery system for cartilage tissue engineering. Int J Nanomedicine. 2020;15:6097–6111. doi: 10.2147/ijn.S249829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pezzana C, Agnely F, Bochot A, Siepmann J, Menasché P. Extracellular vesicles and biomaterial design: new therapies for cardiac repair. Trends Mol Med. 2021;27(3):231–247. doi: 10.1016/j.molmed.2020.10.006 [DOI] [PubMed] [Google Scholar]
- 107.Chuang E-Y, Chiang C-W, Wong P-C, Chen C-H. Hydrogels for the application of articular cartilage tissue engineering: a review of hydrogels. Adv Mater Sci Engine. 2018;2018:4368910. doi: 10.1155/2018/4368910 [DOI] [Google Scholar]
- 108.Liu X, Yang Y, Li Y, et al. Integration of stem cell-derived exosomes with in situ hydrogel glue as a promising tissue patch for articular cartilage regeneration. Nanoscale. 2017;9(13):4430–4438. doi: 10.1039/c7nr00352h [DOI] [PubMed] [Google Scholar]
- 109.Chen P, Zheng L, Wang Y, et al. Desktop-stereolithography 3D printing of a radially oriented extracellular matrix/mesenchymal stem cell exosome bioink for osteochondral defect regeneration. Theranostics. 2019;9(9):2439–2459. doi: 10.7150/thno.31017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Du X, Cai L, Xie J, Zhou X. The role of TGF-beta 3 in cartilage development and osteoarthritis. Bone Res. 2023;11(1):2. doi: 10.1038/s41413-022-00239-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Li T, Liu B, Chen K, Lou Y, Jiang Y, Zhang D. Small molecule compounds promote the proliferation of chondrocytes and chondrogenic differentiation of stem cells in cartilage tissue engineering. Biomed Pharmacother. 2020;131:110652. doi: 10.1016/j.biopha.2020.110652 [DOI] [PubMed] [Google Scholar]
- 112.Chawla S, Mainardi A, Majumder N, et al. Chondrocyte hypertrophy in osteoarthritis: mechanistic studies and models for the identification of new therapeutic strategies. Cells. 2022;11(24):248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Johnson K, Zhu S, Tremblay MS, et al. A stem cell-based approach to cartilage repair. Science. 2012;336(6082):717–721. doi: 10.1126/science.1215157 [DOI] [PubMed] [Google Scholar]
- 114.Zheng Z, Chen F, Zhang X. Editorial: potential of extracellular matrix molecules in pharmaceutical development. Editorial. Front Pharmacol. 2021;11. doi: 10.3389/fphar.2020.636026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gao Y, Liu S, Huang J, et al. The ECM-cell interaction of cartilage extracellular matrix on chondrocytes. Biomed Res Int. 2014;2014:648459. doi: 10.1155/2014/648459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shi Y, Hu X, Cheng J, et al. A small molecule promotes cartilage extracellular matrix generation and inhibits osteoarthritis development. Nat Commun. 2019;10(1):1914. doi: 10.1038/s41467-019-09839-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhang W, Chen R, Xu X, et al. Construction of biocompatible hydrogel scaffolds with a long-term drug release for facilitating cartilage repair. Front Pharmacol. 2022;13:922032. doi: 10.3389/fphar.2022.922032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xu X, Shi D, Shen Y, et al. Full-thickness cartilage defects are repaired via a microfracture technique and intraarticular injection of the small-molecule compound kartogenin. Arthritis Res Ther. 2015;17(1):20. doi: 10.1186/s13075-015-0537-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yan H, Yu T, Li J, et al. Kartogenin improves osteogenesis of bone marrow mesenchymal stem cells via autophagy. Stem Cells Int. 2022;2022:1278921. doi: 10.1155/2022/1278921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang H, Fang W, Zhao T, et al. Real-time MRI monitoring of GelMA-based hydrogel-loaded kartogenin for in situ cartilage regeneration. Front Bioeng Biotechnol. 2022;10:940735. doi: 10.3389/fbioe.2022.940735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Yano F, Hojo H, Ohba S, et al. A novel disease-modifying osteoarthritis drug candidate targeting Runx1. Ann Rheum Dis. 2013;72(5):748–753. doi: 10.1136/annrheumdis-2012-201745 [DOI] [PubMed] [Google Scholar]
- 122.Park J, Lee SY. A review of osteoarthritis signaling intervention using small-molecule inhibitors. Medicine. 2022;101(32):e29501. doi: 10.1097/md.0000000000029501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang Y, Zhao Q. Salidroside attenuates interleukin-1β-induced inflammation in human osteoarthritis chondrocytes. J Cell Biochem. 2018. doi: 10.1002/jcb.27076 [DOI] [PubMed] [Google Scholar]
- 124.Wu M, Hu R, Wang J, et al. Salidroside suppresses IL-1β-induced apoptosis in chondrocytes via phosphatidylinositol 3-kinases (PI3K)/Akt signaling inhibition. Med Sci Monit. 2019;25:5833–5840. doi: 10.12659/msm.917851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nagao M, Hamilton JL, Kc R, et al. Vascular endothelial growth factor in cartilage development and osteoarthritis. Sci Rep. 2017;7(1):13027. doi: 10.1038/s41598-017-13417-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473(7347):298–307. doi: 10.1038/nature10144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ngo HX, Garneau-Tsodikova S. What are the drugs of the future? Medchemcomm. 2018;9(5):757–758. doi: 10.1039/c8md90019a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.da Costa BR, Pereira TV, Saadat P, et al. Effectiveness and safety of non-steroidal anti-inflammatory drugs and opioid treatment for knee and Hip osteoarthritis: network meta-analysis. BMJ. 2021;375:n2321. doi: 10.1136/bmj.n2321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and Hip osteoarthritis: a network meta-analysis. Lancet. 2017;390(10090):e21–e33. doi: 10.1016/s0140-6736(17)31744-0 [DOI] [PubMed] [Google Scholar]
- 130.Magni A, Agostoni P, Bonezzi C, et al. Management of osteoarthritis: expert opinion on NSAIDs. Pain Ther. 2021;10(2):783–808. doi: 10.1007/s40122-021-00260-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Jüni P, Hari R, Rutjes AW, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015;2015(10):Cd005328. doi: 10.1002/14651858.CD005328.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Smedslund G, Kjeken I, Musial F, Sexton J, Østerås N. Interventions for osteoarthritis pain: a systematic review with network meta-analysis of existing cochrane reviews. Osteoarthr Cartil Open. 2022;4(2):100242. doi: 10.1016/j.ocarto.2022.100242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Garg N, Perry L, Deodhar A. Intra-articular and soft tissue injections, a systematic review of relative efficacy of various corticosteroids. Clin Rheumatol. 2014;33(12):1695–1706. doi: 10.1007/s10067-014-2572-8 [DOI] [PubMed] [Google Scholar]
- 134.McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–388. doi: 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 135.Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, Hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi: 10.1016/j.joca.2019.06.011 [DOI] [PubMed] [Google Scholar]
- 136.Evaniew N, Simunovic N, Karlsson J. Cochrane in CORR®: viscosupplementation for the treatment of osteoarthritis of the knee. Clin Orthop Relat Res. 2014;472(7):2028–2034. doi: 10.1007/s11999-013-3378-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Presti D, Scott JE. Hyaluronan-mediated protective effect against cell damage caused by enzymatically produced hydroxyl (OH.) radicals is dependent on hyaluronan molecular mass. Cell Biochem Funct. 1994;12(4):281–288. doi: 10.1002/cbf.290120409 [DOI] [PubMed] [Google Scholar]
- 138.Pereira TV, Jüni P, Saadat P, et al. Viscosupplementation for knee osteoarthritis: systematic review and meta-analysis. BMJ. 2022;378:e069722. doi: 10.1136/bmj-2022-069722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jackson DW, Evans NA, Thomas BM. Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am. 2002;84(9):1522–1527. doi: 10.2106/00004623-200209000-00003 [DOI] [PubMed] [Google Scholar]
- 140.Patel A, Chadwick N, von Beck K, et al. Ultrasound-guided joint interventions of the lower extremity. Skeletal Radiol. 2022. doi: 10.1007/s00256-022-04168-5 [DOI] [PubMed] [Google Scholar]
- 141.Hussein M. An accurate full-flexion anterolateral portal for needle placement in the knee joint with dry osteoarthritis. J Am Acad Orthop Surg. 2017;25(7):e131–e137. doi: 10.5435/jaaos-d-16-00338 [DOI] [PubMed] [Google Scholar]
- 142.Telikicherla M, Kamath SU. Accuracy of needle placement into the intra-articular space of the knee in osteoarthritis patients for viscosupplementation. J Clin Diagn Res. 2016;10(2):Rc15–7. doi: 10.7860/jcdr/2016/17127.7275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Toda Y, Tsukimura N. A comparison of intra-articular hyaluronan injection accuracy rates between three approaches based on radiographic severity of knee osteoarthritis. Osteoarthritis Cartilage. 2008;16(9):980–985. doi: 10.1016/j.joca.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 144.Reeves KD, Sit RW, Rabago DP. Dextrose prolotherapy: a narrative review of basic science, clinical research, and best treatment recommendations. Phys Med Rehabil Clin N Am. 2016;27(4):783–823. doi: 10.1016/j.pmr.2016.06.001 [DOI] [PubMed] [Google Scholar]
- 145.Sit RW, Chung V, Reeves KD, et al. Hypertonic dextrose injections (prolotherapy) in the treatment of symptomatic knee osteoarthritis: a systematic review and meta-analysis. Sci Rep. 2016;6:25247. doi: 10.1038/srep25247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wang J, Liang J, Yao J, et al. Meta-analysis of clinical trials focusing on hypertonic dextrose prolotherapy (HDP) for knee osteoarthritis. Aging Clin Exp Res. 2022;34(4):715–724. doi: 10.1007/s40520-021-01963-3 [DOI] [PubMed] [Google Scholar]
- 147.Uebelhart D, Thonar EJ, Delmas PD, Chantraine A, Vignon E. Effects of oral chondroitin sulfate on the progression of knee osteoarthritis: a pilot study. Osteoarthritis Cartilage. 1998;6(Suppl A):39–46. doi: 10.1016/s1063-4584(98)80011-3 [DOI] [PubMed] [Google Scholar]
- 148.Urbi Z, Azmi NS, Ming LC, Hossain MS. A concise review of extraction and characterization of chondroitin sulphate from fish and fish wastes for pharmacological application. Curr Issues Mol Biol. 2022;44(9):3905–3922. doi: 10.3390/cimb44090268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gallagher B, Tjoumakaris FP, Harwood MI, Good RP, Ciccotti MG, Freedman KB. Chondroprotection and the prevention of osteoarthritis progression of the knee: a systematic review of treatment agents. Am J Sports Med. 2015;43(3):734–744. doi: 10.1177/0363546514533777 [DOI] [PubMed] [Google Scholar]
- 150.Simental-Mendía M, Sánchez-García A, Vilchez-Cavazos F, Acosta-Olivo CA, Peña-Martínez VM, Simental-Mendía LE. Effect of glucosamine and chondroitin sulfate in symptomatic knee osteoarthritis: a systematic review and meta-analysis of randomized placebo-controlled trials. Rheumatol Int. 2018;38(8):1413–1428. doi: 10.1007/s00296-018-4077-2 [DOI] [PubMed] [Google Scholar]
- 151.Honvo G, Bruyère O, Geerinck A, Veronese N, Reginster JY. Efficacy of chondroitin sulfate in patients with knee osteoarthritis: a comprehensive meta-analysis exploring inconsistencies in randomized, placebo-controlled trials. Adv Ther. 2019;36(5):1085–1099. doi: 10.1007/s12325-019-00921-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the US bone and joint initiative. Semin Arthritis Rheum. 2014;43(6):701–712. doi: 10.1016/j.semarthrit.2013.11.012 [DOI] [PubMed] [Google Scholar]
- 153.Smith JK. Exercise as an adjuvant to cartilage regeneration therapy. Int J Mol Sci. 2020;21(24):9471. doi: 10.3390/ijms21249471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chen J, Zhou R, Feng Y, Cheng L. Molecular mechanisms of exercise contributing to tissue regeneration. Signal Transduct Target Ther. 2022;7(1):383. doi: 10.1038/s41392-022-01233-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sánchez Romero EA, Fernández-Carnero J, Calvo-Lobo C, Ochoa Sáez V, Burgos Caballero V, Pecos-Martín D. Is a combination of exercise and dry needling effective for knee OA? Pain Med. 2020;21(2):349–363. doi: 10.1093/pm/pnz036 [DOI] [PubMed] [Google Scholar]
- 156.Alonso Pérez JL, Martín Pérez S, Battaglino A, Villafañe JH, Alonso-Sal A, Sánchez Romero EA. An up-date of the muscle strengthening exercise effectiveness in postmenopausal women with osteoporosis: a qualitative systematic review. J Clin Med. 2021;10(11):2229. doi: 10.3390/jcm10112229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Cantero-Tellez R, García-Orza S, Sánchez Romero EA, Battaglino A, Cruz-Gambero L, Cuadros-Romero M. Effect of a proprioceptive exercise program on force sense for carpometacarpal joint osteoarthritis: a pilot study. Top Geriatr Rehabil. 2021;37(4):222–226. doi: 10.1097/TGR.0000000000000336 [DOI] [Google Scholar]
- 158.Sánchez-Romero EA, González-Zamorano Y, Arribas-Romano A, et al. Efficacy of manual therapy on facilitatory nociception and endogenous pain modulation in older adults with knee osteoarthritis: a case series. Appl Sci. 2021;11(4):1895. doi: 10.3390/app11041895 [DOI] [Google Scholar]
- 159.Sinatti P, Sánchez Romero EA, Martínez-Pozas O, Villafañe JH. Effects of patient education on pain and function and its impact on conservative treatment in elderly patients with pain related to hip and knee osteoarthritis: a systematic review. Int J Environ Res Public Health. 2022;19(10):6194. doi: 10.3390/ijerph19106194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Nguyen C, Lefèvre-Colau MM, Poiraudeau S, Rannou F. Rehabilitation (exercise and strength training) and osteoarthritis: a critical narrative review. Ann Phys Rehabil Med. 2016;59(3):190–195. doi: 10.1016/j.rehab.2016.02.010 [DOI] [PubMed] [Google Scholar]
- 161.Sharma L. Osteoarthritis year in review 2015: clinical. Osteoarthritis Cartilage. 2016;24(1):36–48. doi: 10.1016/j.joca.2015.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Duivenvoorden T, Brouwer RW, van Raaij TM, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;2015(3):Cd004020. doi: 10.1002/14651858.CD004020.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hunter CW, Deer TR, Jones MR, et al. Consensus guidelines on interventional therapies for knee pain (STEP Guidelines) from the American Society of Pain and Neuroscience. J Pain Res. 2022;15:2683–2745. doi: 10.2147/jpr.S370469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Anandacoomarasamy A, Leibman S, Smith G, et al. Weight loss in obese people has structure-modifying effects on medial but not on lateral knee articular cartilage. Ann Rheum Dis. 2012;71(1):26–32. doi: 10.1136/ard.2010.144725 [DOI] [PubMed] [Google Scholar]
- 165.Aaboe J, Bliddal H, Messier SP, Alkjær T, Henriksen M. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage. 2011;19(7):822–828. doi: 10.1016/j.joca.2011.03.006 [DOI] [PubMed] [Google Scholar]