Abstract
The U.S. drug overdose crisis has been described as a national disaster that has affected all communities. But overdose rates are higher among some subpopulations and in some places than they are in others. This article describes demographic (sex, racial/ethnic, age) and geographic variation in fatal drug overdose rates in the United States from 1999 to 2020. Across most of that timespan, rates were highest among young and middle-age (25–54 years) White and American Indian males and middle-age and older (45+ years) Black males. Rates have been consistently high in Appalachia, but the crisis has spread to several other regions in recent years, and rates are high across the urban-rural continuum. Opioids have been the main contributor, but overdoses involving cocaine and psychostimulants have also increased dramatically in recent years, demonstrating that our problem is bigger than opioids. Evidence suggests that supply-side interventions are unlikely to be effective in reducing overdoses. I argue that the U.S. should invest in policies that address the upstream structural drivers of the crisis.
Keywords: opioids, drug overdose, demographic differences, geographic differences
Fatal drug overdose rates in the U.S. increased 445 percent from 1999 to 2020, claiming the lives of over one million Americans. The primary contributor has been opioids, due largely to their comparative lethality relative to other commonly used substances. Indeed, 75 percent of overdoses between 1999 and 2020 involved opioids (author calculations). However, deaths involving cocaine, psychostimulants with abuse potential (primarily methamphetamine), and prescription benzodiazepines (a sedative) also increased over this period, demonstrating that our problem is bigger than opioids alone. Despite the billions of dollars invested and numerous policies enacted to combat the drug overdose epidemic, overdose rates continue to climb, and the COVID-19 pandemic appears to have exacerbated these long-term trends (National Center for Health Statistics [NCHS] 2022).
The U.S. drug overdose crisis has been described as a national crisis affecting all groups and geographic areas. However, overdose rates are higher and have increased more in some subpopulations and places than others. A report released by the National Academies of Sciences, Engineering, and Medicine (NASEM; 2021), examining mortality trends among U.S. working-age (25–64 years) non-Hispanic (NH) Whites, NH Blacks, and Hispanics, found that fatal drug overdose rates from 1999 to 2017 were highest among White males 25 to 44 years old and Black males 55 to 64 years old. Hoopsick, Homish, and Leonard (2021) examined fatal overdoses involving specific opioids among U.S. Whites, Blacks, and Hispanics ages 45 to 64 from 1999 to 2018, finding that Whites had the highest rates involving prescription opioids, while Blacks had significantly higher rates from heroin and synthetic opioids. In terms of geographic differences, analyses show that rates have been highest over the past two decades in Appalachia and the desert Southwest, with larger swaths of the country (New England, parts of the Industrial Midwest, and eastern Oklahoma) experiencing surging rates since the mid-2010s (Monnat et al. 2019; Peters et al. 2020). Whereas overdoses involving prescription opioids have generally been highest in nonmetro areas, overdoses involving heroin and synthetic opioids have been higher in metro areas (Rigg et al. 2018; Peters et al. 2020).
This article presents a broad overview of where and among whom the contemporary drug overdose crisis has had its most pronounced effects. I do this by presenting a comprehensive summary of demographic (age group, sex, racial/ethnic) and geographic variation in fatal drug overdose trends from 1999 to 2020. I consider a wider range of age groups than prior analyses that tend to focus on working-age adults, include American Indians and Asians, update analyses to 2020 (the most recent year for which data are available and the year with the highest overdose rate in the U.S. to date), and consider variation across the different waves of the overdose crisis, wherein different drugs have played a primary role during different periods.
My analyses also extend beyond opioids to consider the role of other high-risk drugs—cocaine, psychostimulants with abuse potential, and benzodiazepines. The consideration of overdoses involving high-risk drugs other than opioids is important for at least two reasons. First, the contributions of these drugs to overdoses have increased dramatically in recent years, and rates involving cocaine have historically been higher among Blacks than among Whites. Second, due to inconsistencies in coroner and medical examiner training and experience, many death certificates either do not identify or misclassify the specific drugs involved in the overdose. For these two reasons, restricting the presentation of trends to deaths involving opioids on the death certificate would both mischaracterize the overdose crisis and undercount deaths involving drugs in the U.S., particularly for certain demographic groups. I intentionally keep the analyses descriptive, not testing hypotheses or explanations for the trends observed.
In the next section, I provide background that can help us understand the intersecting roles of supply factors in driving rising rates of overdose overall and demand factors in increasing the vulnerability of some groups more than others. I conclude the article by identifying areas for future research and by providing policy recommendations to reduce overdoes rates in the short term and reduce drug use initiation in the longer term.
Factors Driving the Contemporary Drug Overdose Crisis
The past three-decade rise in drug overdoses in the U.S. has been described as a “perfect storm” of the flooding of the market with highly addictive and cheap narcotics (supply) combined with underlying chronic and increasing vulnerability of certain U.S. population subgroups to these drugs (demand) (Monnat 2020a; NASEM 2021). Both supply and demand trends have been driven by U.S federal and state policy choices, corporate behaviors, and a neoliberal policy regime that prioritizes maximizing profit over protecting population health.
The supply side
The contemporary U.S. overdose crisis has unfolded across four waves (see Figure 1), with the potency of drugs increasing in each subsequent wave, drastically increasing the risk of overdose among people who use drugs.
FIGURE 1.
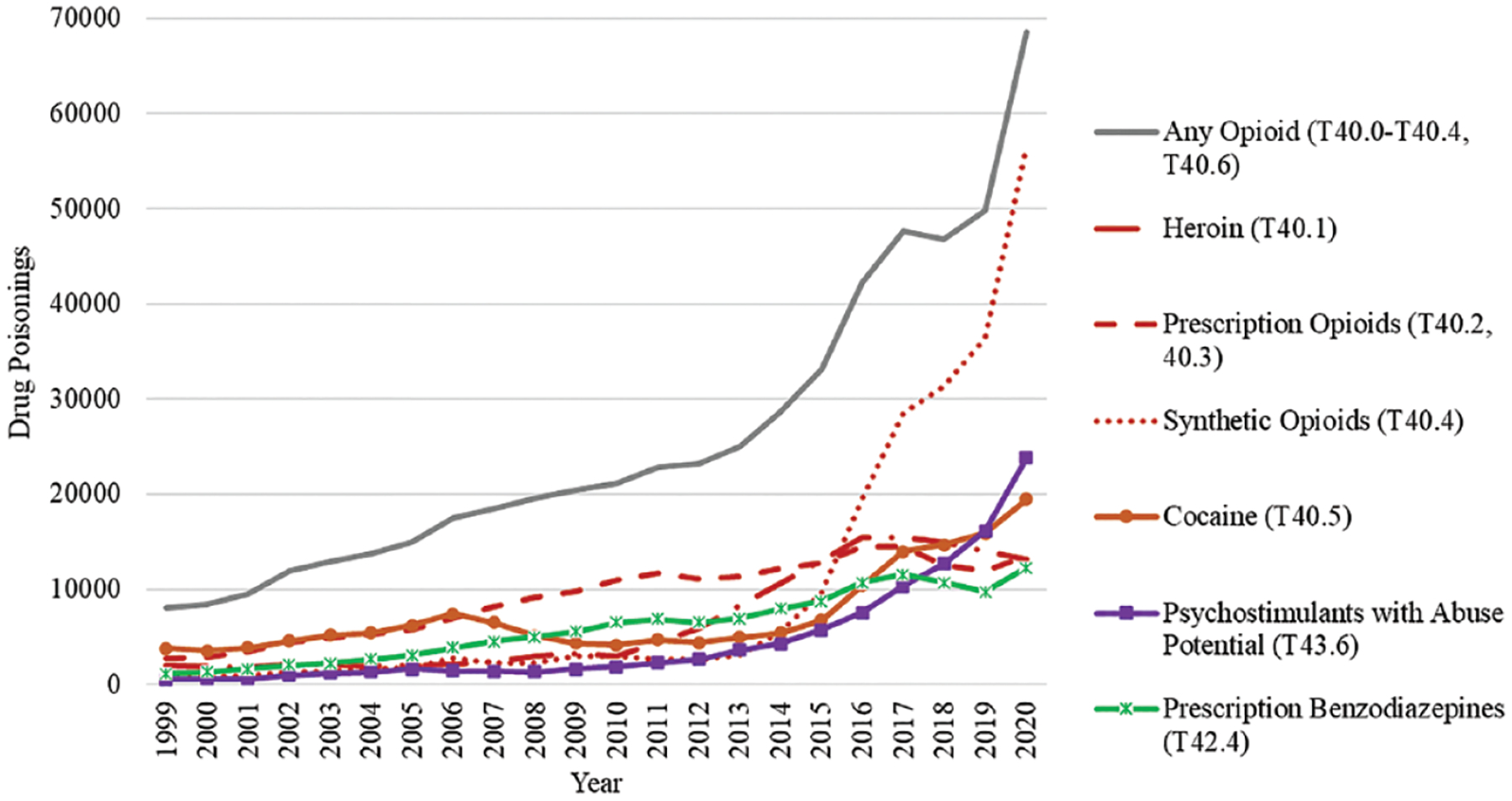
Fatal Drug Poisonings by Drug Type, United States, 1999–2020
SOURCE: CDC WONDER (Wide-Ranging Online Data for Epidemiologic Research), Multiple Cause of Death Files (NCHS 2021).
NOTE: Includes deaths with an underlying cause International Classification of Disease (ICD)-10 code of X40-X44, X60-X64, X85, Y10-Y14. T-codes represent the drug involved in the overdose, based on multiple cause of death coding. Categories are not mutually exclusive because deaths may involve more than one drug.
Wave 1: Prescription opioids.
The first wave (late 1990s to early 2010s) was characterized by a surge in overdoses from prescription opioids. Sales of prescription opioids are estimated to have quadrupled between 1999 and 2011 (CDC 2011), and deaths involving prescription opioids increased 325 percent over this period (author calculation). Overdose rates have been found to be significantly higher in counties with higher opioid prescribing rates (Monnat 2018, 2019; Peters et al. 2020; Ruhm 2019). A vast literature describes the policy failures and corporate practices that led to massive increases in opioid prescribing (Alpert et al. 2019; NASEM 2021; Quinones 2015, 2021; Van Zee 2009). These include weak government regulations on pharmaceutical distribution and marketing; Purdue Pharma’s introduction of OxyContin® (a potent, highly addictive, and easily abused opioid) in 1996; the failure of the U.S. Food and Drug Administration (FDA) to properly evaluate OxyContin’s efficacy and potential addiction risks prior to approval; patient advocacy groups, funded by pharmaceutical companies, that pushed the medical field to recognize pain as the fifth vital sign and aggressively treat it; aggressive marketing, physician kickbacks, and disinformation campaigns by Purdue and other pharmaceutical companies to increase prescribing; the proliferation of unregulated high-volume pain clinics (“pill mills”) where physicians prescribed large quantities of opioids and benzodiazepines with little diagnosis or follow-up; the failure of pharmaceutical distributors, dispensers, and pharmacy chains to monitor and investigate suspicious prescribing practices; the failure of most state licensing and monitoring boards to monitor possible fraud and overprescribing; the failure of public and private insurers to develop adequate checks to determine whether the prescriptions were appropriate; and slow action by the U.S. Drug Enforcement Agency (DEA) to detect and prevent opioid diversion.
Wave 2: Heroin.
As policy-makers and physicians caught on to the surge in prescription opioid overdoses, they enacted policies to reduce prescribing and deter diversion and abuse, including instituting prescribing limits, establishing prescription drug monitoring programs, and requiring pain clinics to provide medical records to support prescribing. Purdue also reformulated OxyContin into an abuse-deterrent version in 2010. Collectively, these changes stimulated the growth of a “thick market” for heroin (a cheaper and more potent opiate), ushering in the second wave of the overdose crisis (early to mid-2010s) (Alpert et al. 2018; Cicero and Surratt 2012; Pitt, Humphreys, and Brandeau 2018; Powell and Pacula 2021). Heroin is pharmacologically similar to, though more potent than (in terms of morphine milligram equivalents), prescription opioids. Given its composition as a powder, it is also easier to manipulate for use via nonoral routes (e.g., snorting, injection), which means the morphine hits the central nervous and respiratory systems more quickly, increasing the risk of overdose.
Key to the surge in the heroin supply in the U.S. was the consolidation of supply chains in Mexico, thanks in part to DEA crackdowns on heroin suppliers in Colombia. The disruption to Colombian drug cartels created an opening for Mexican suppliers. Between 2005 and 2016, Mexican drug suppliers increased their control of the heroin market from 50 to 90 percent (DEA 2017). In addition to providing a cheaper and more consistently available supply and distributing it across a much wider swath of the U.S. than in the past, the heroin from Mexico was more refined and more potent than the heroin previously available in the U.S., dramatically increasing overdose risk. Between 2010 and 2016, overdoses involving heroin increased by over 400 percent (author calculation).
Wave 3: Synthetic opioids.
The third wave began in the mid-2010s, when suppliers and dealers began increasingly adulterating heroin and other drugs with synthetic opioids (fentanyl and fentanyl analogs) and producing counterfeit pills containing fentanyl but made to look identical to legitimate prescription pills. In 2021, the DEA reported that the number of fake pills containing fentanyl had increased 430 percent since 2019, with 40 percent of what they seized containing potentially lethal doses (DEA 2021). Synthetic opioids like fentanyl are more potent than heroin, so fentanyl is cheaper per volume to produce and easier to smuggle. Cartels also prefer working with synthetic opioids because it is easier to control production. Unlike growing the poppies required for heroin, synthetic opioids are not affected by climate challenges, and cartels can bypass poppy farmers by manufacturing in labs. Deaths involving synthetic opioids increased over 900 percent between 2014 and 2020.
Wave 4: Polysubstance overdoses.
The fourth (and current) wave is characterized by a polysubstance overdose crisis, primarily involving fentanyl, cocaine, and methamphetamine. One reason is the increasing fentanyl adulteration of a wide range of illicit drugs, with dealers adding fentanyl to various other products to increase their potency (Quinones 2021). However, polysubstance use is also the norm among people with opioid use disorders (Cicero, Ellis, and Kasper 2020). Polysubstance use is certainly not new. For example, “speed-balling,” (combining an opioid and a stimulant) is found in the literature as early as the 1950s (Piro et al. 2019). However, the increase in the relative potency of substances over time has likely been the largest contributor to the increase in overdoses involving multiple substances. The increasing role of methamphetamine in overdose deaths is particularly notable. Part of the reason researchers, policy-makers, and the media have ignored methamphetamine is that it historically has not led to many overdoses. Unlike opioids, methamphetamine does not suppress respiration, so risk of overdose has been lower. However, methamphetamine is now the second largest contributor to overdose deaths after synthetic opioids, with deaths involving methamphetamine increasing 50 percent between 2019 and 2020.
Increased production, distribution, and access to increasingly potent (and cheaper) methamphetamine in the U.S. over the past few years has certainly played a major role (Quinones 2021). But demand for methamphetamine also appears to have increased. Many people who use opioids are increasingly turning to methamphetamine as a substitute or supplement to their opioid use (Quinones 2021). Ellis, Kasper, and Cicero (2018) suggest that the sedative effects of opioids and the stimulant effects of methamphetamine may establish an equilibrium for users that enables them to function and/or that the concomitant use of these drugs produces a “roller-coaster” high with two separate sensations that are pleasurable to users.
Across these four waves that have spanned 30 years, fatal drug overdose rates increased across all age groups, all racial/ethnic groups, both males and females, and all geographic areas in the U.S. However, as I describe later, these waves, and the overdose crisis more generally, have affected different populations and places in the U.S. in different ways.
To be sure, supply factors were an essential spark. The increase in the availability and lethality of drugs increased the risk of overdose among both long-term and new users. However, supply factors cannot explain why some groups and some places have been more affected than others. Population health disparities defy a simple explanation. Disparities are driven by complex interactions between policies, economic and social conditions, institutional responses, and underlying population vulnerabilities.
The demand side—root causes
Understanding why certain groups of people and places appear to be more vulnerable than others to the surge in exposure to opioids and other drugs requires understanding the full range of proximate to distal risk factors for substance use, addiction, and overdose (Dasgupta, Beletsky, and Ciccarone 2018). Proximate risk factors include mental health and psychological ill-being, trauma, physical pain, and social relationships. These proximate factors in turn are influenced by various social determinants of health. Poverty, housing, employment, health care availability and quality, material resources, economic opportunities, and criminal justice system involvement and incarceration have been identified as social determinants of substance use and overdose (Dasgupta, Beletsky, and Ciccarone 2018). Exposure to these social determinants is driven by upstream structural factors, including state and federal policy choices and macroeconomic trends. Differential exposure to these factors from the distal to the proximate contributes to disparities in drug overdose.
When the media started raising concerns about rising drug overdose rates in the mid-2010s, much of the attention was on unprecedented increases among middle-aged Whites without a college degree (Case and Deaton 2015, 2017). This was a group with historically low rates of using the types of drugs with high risk of overdose (e.g., heroin). In attempting to explain increases in this group, Case and Deaton implicated a rising tide of despair (proximate risk factor) related to structural changes in economic, family, and social conditions. They suggested that the life circumstances of less-educated Whites had been eroding since at least the 1980s, when the cohort who was now dying in middle age (in the 2010s) was beginning their initial life course transitions into the labor force and family formation. The long-term erosion of economic opportunity and stability included declines in wages, labor force participation, job quality, and unions; a rise in divorce and single parenthood; and changes in religious and social participation. These long-term trends could be felt both individually and collectively and may have manifested in stress, hopelessness, and harmful coping mechanisms among the groups that previously had little experience with declining opportunity.
Due to the lack of long-term longitudinal data that captures measures of psychological and economic well-being and substance use, it has been difficult to draw a causal link between changes in psychological well-being and drug overdose mortality trends (NASEM 2021). However, there is substantial descriptive evidence to show that psychological well-being has declined in recent decades, particularly among working-age Whites without a four-year degree (Cherlin 2018; Gaydosh et al. 2019; Goldman, Glei, and Weinstein 2018; Graham and Pinto 2019; Graham, Pinto, and Juneau 2017; Muennig et al. 2018). Muennig et al. (2018) found that these declines were not restricted to working-age Whites; mental health worsened across all age and racial/ethnic groups over the period (Muennig et al. 2018). Graham and Pinto (2019) connected trends in psychological well-being to drug-related mortality, finding a strong association between lack of hope, high levels of worry, and county-level rates of drug, alcohol, and suicide mortality among less-educated Whites in the U.S. Qualitative research conducted in communities in long-term decline in Appalachia also suggests strong links between psychological distress and substance use (Chen 2015; McLean 2016; Silva 2019). Bolstering this argument is that other causes of death that may be connected to psychological well-being and harmful coping behaviors—suicide, alcohol-related mortality, and deaths from certain types of cardiometabolic diseases—also increased among working-age Whites over the past three decades (Stein et al. 2017; Case and Deaton 2020; Monnat 2020b; NASEM 2021). Moreover, American Indians who have long suffered from structurally induced poverty, limited economic opportunity, and collective trauma also have high rates of substance use and substance-related deaths (Whitesell et al. 2012).
Macro-level economic and social changes (driven by U.S. federal and state policy choices) are among the hypothesized structural drivers of the rise in both psychological ill-being and drug overdose, and these changes may help to explain why rates have risen more in some types of places than others. Thanks to economic restructuring, which drastically reduced employment and job quality among those without a 4-year college degree, along with 40+ years of federal deregulation; devolution of federal authority to states; and disinvestments in safety nets, infrastructure, and institutions, many places in the U.S. were primed to be vulnerable to opioids—drugs that numb both physical and psychological pain. These processes did not affect places or populations equally. Places dependent on industries like mining and manufacturing (clustered throughout Appalachia and the industrial Midwest) were among the hardest hit by economic restructuring, de-unionization, and declining economic opportunities, making them high-risk environments for substance misuse (Keyes et al. 2014; McLean 2016). Indeed, drug overdose rates have been higher in counties characterized by more economic and family distress, such as higher rates of poverty, unemployment, disability, no college degree, public assistance receipt, divorce and separation, and single-parent families (Monnat 2018, 2019; Monnat et al. 2019). Importantly, prescribing practices themselves were not place-neutral. Pharmaceutical companies targeted, and widespread opioid prescribing first emerged in the most economically vulnerable places in the U.S., including Ohio, Kentucky, and West Virginia, before they moved across the rest of the country (Keyes et al. 2014; Quinones 2015; Van Zee 2009).
The geographic distribution of economic decline and the deterioration of decent-paying working-class jobs correspond (with the expected time lag) to the geographic distribution of drug overdose. Rising economic distress occurred concomitantly with changes to families, including a long-term demographic trend toward lower marriage rates, increasing single-parent families, and increasing multiple-partner fertility (Burton et al. 2013). Engagement with social-capital-promoting institutions, such as religious organizations and community groups, has also been in long-term decline, with research suggesting that counties with the lowest levels of social capital also have the highest overdose rates (Zoorob and Salemi 2017). Viewing these trends from within a Durkheimian sociological lens of “anomie” (Durkheim 1897/1966), these factors may mean that growing shares of some population subgroups and places (particularly those for whom declining opportunity was a new experience) began feeling increasingly isolated, disconnected, unstable, and without purpose or meaning in their lives.
There is also empirical evidence to support the hypothesis that macroeconomic changes have contributed to the unequal geographic distribution of drug overdose, with researchers finding causal effects of changes in county-level unemployment rates (Hollingsworth, Ruhm, and Simon 2017), international trade exposure (Pierce and Schott 2020), automotive plant closures (Venkataramani et al. 2020), and automation (O’Brien, Bair, and Venkataramani 2022) on changes in drug-related mortality rates. Potentially helping to explain why overdose rates increased earlier and more quickly among working-age Whites than among working-age Blacks, both Hollingsworth, Ruhm, and Simon (2017) and Pierce and Schott (2020) found effects of unemployment and international trade exposure only on drug overdose mortality among Whites. The collapse of local economies, social institutions, and family structures experienced by lower-educated Whites since the 1990s is similar in many ways to the decline experienced by their Black counterparts in the 1970s to 1990s. The collapse of inner-city economies and institutions was likewise accompanied by a drug crisis, although, as has been described in detail elsewhere, the previous drug crises in the U.S. were addressed in a much more punitive, racialized, and stigmatizing manner than the contemporary one.
The supply and demand factors summarized above are not competing explanations. Rather, they collectively help us understand why overdoes rates increased when they did, the role different drugs and their increasing lethality have played over time, and why certain populations and places may have been more vulnerable than others to increased exposure to these substances.
In the next section, I present a comprehensive description of demographic and geographic differences in fatal drug overdose rates since 1999. I also consider these differences in the context of the waves of the epidemic described above by describing differences in the substances involved in overdoses across these different demographic and geographic groups.
Data and Methods
The analyses use publicly available data on fatal drug poisonings1 for 1999 to 2020 from the U.S. Centers for Disease Control and Prevention (CDC) WONDER (Wide-Ranging Online Data for Epidemiologic Research) (NCHS 2021). I use 1999 as the base year because International Classification of Disease (ICD) codes were updated that year, from ICD-9 to ICD-10. Those updates affected the classification of specific drug classes. The use of 1999 does not imply that the overdose crisis began in that year. Overdoses started to tick up in the early 1990s (NASEM 2021). Drug poisoning (overdose) deaths are those with an ICD-10 underlying cause of death code of X40–X44 (accidental poisoning), X60–X64 (intentional self-poisoning), X85 (assault by drugs), or Y10–Y14 (poisoning, undetermined intent).
To examine demographic variation, I extracted annual age-sex-race specific rates (deaths per 100,000 population) for males and females ages 15 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, and 65+ for NH Whites, NH Blacks, Hispanics, NH American Indian/Alaska Natives (AIANs), and NH Asians. I visualize annual trends in rates and present coefficients from linear regression models. The coefficients represent the average differences in fatal overdose rates for each demographic group compared to the identified reference group. I present models for the period 1999 to 2020 overall and separate models for wave 1 (1999–2010), wave 2 (2011–2015), and waves 3 and 4 (2016–2020). Varying the year cut points for the waves by a year in either direction did not meaningfully affect the findings.
To determine which geographic areas have been most affected, I present similar analysis by U.S. Census region (Northeast, Midwest, South, and West) and urban-rural continuum using the NCHS Urban-Rural Classification Scheme for Counties(large central metro, large fringe metro, medium metro, small metro, micropolitan [nonmetro], noncore [nonmetro]). To visualize spatial trends in fatal drug poisonings at the county level, I calculated age-adjusted rates using the National Vital Statistics System restricted use death certificate files and the U.S. Census Bureau’s bridged-race population estimates.
Tables in the online appendix present annual rates and rates of change for each demographic and geographic group.
Results
Demographic differences
Figure 2 presents trends in age-sex-race specific fatal drug poisoning rates from 1999 to 2020. Considering the 22-year period overall, males consistently had higher rates than females, and ages 25 to 54 had higher rates than the younger or older age groups. Racial/ethnic differences varied by age group and wave. Table 1 presents coefficients from regression models representing the average differences in rates across the period for males by age group and racial/ethnic group. Hispanic and Asian males had significantly lower rates than White males across all age groups (p < .05). Rates for AIANs were not significantly different from Whites in any age groups. Blacks had significantly lower rates than Whites among ages 15 to 44. Among ages 45 to 54, Blacks had comparable rates as Whites; and among ages 55 to 64 and 65+, Blacks had significantly higher rates than Whites. These differences were generally consistent across the waves of the epidemic, with some variation in trends depending on the specific age group of interest. Of note, the older Black male disadvantage (ages 55+) became especially pronounced in waves 3 and 4, with Black males ages 55 to 64 having an average rate that was 43 deaths per 100,000 population higher than White males. Overall, the highest rates among males have been for Blacks ages 45 to 54 (39.9) and 55 to 64 (41.7); AIANs ages 25 to 34 (37.7), 35 to 44 (41.2), and 45 to 54 (36.3); and Whites ages 25 to 34 (39.6), 35 to 44 (38.6), and 45 to 54 (33.8). For a full ranking, see online appendix Table A13.
FIGURE 2.
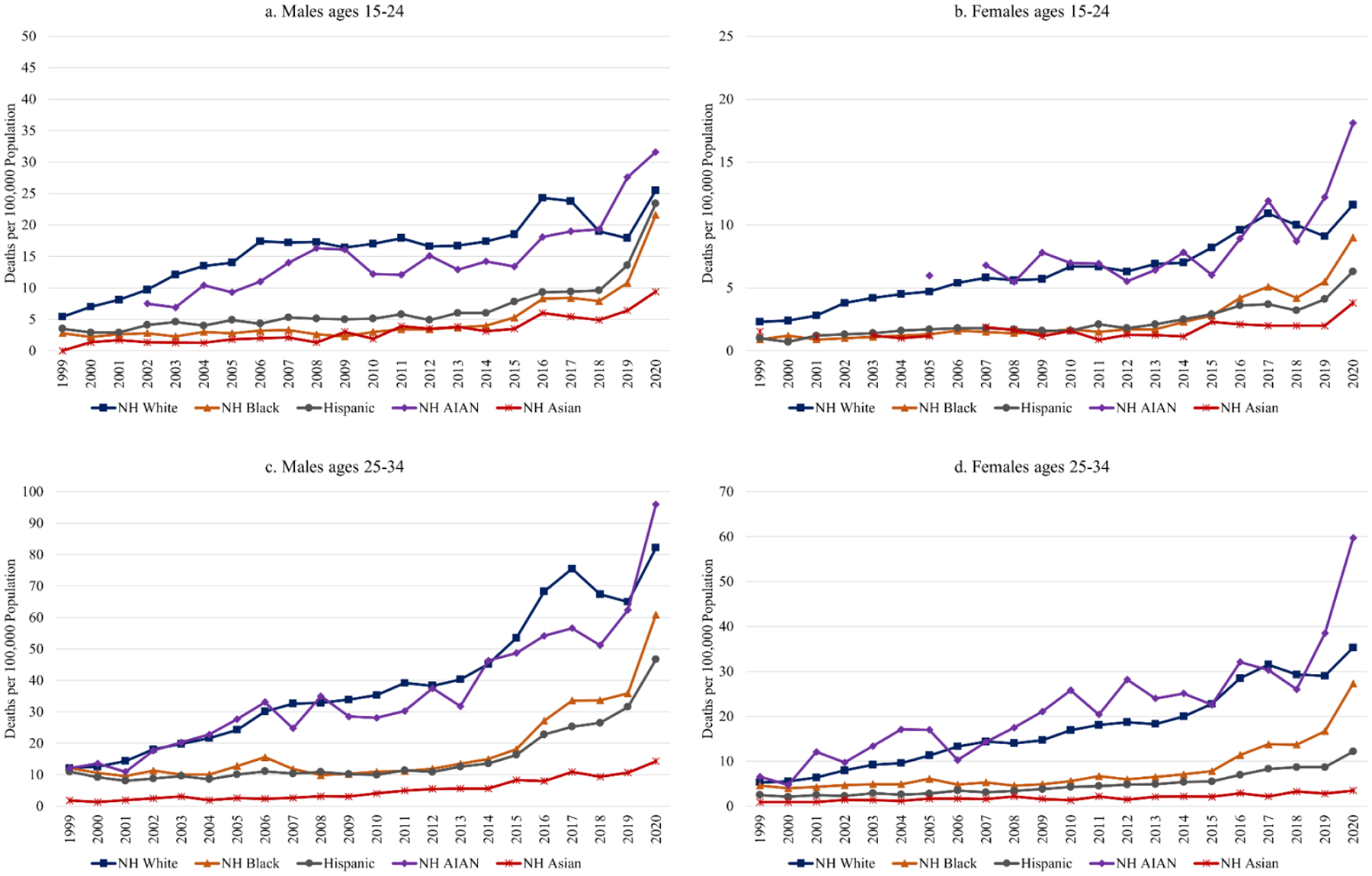
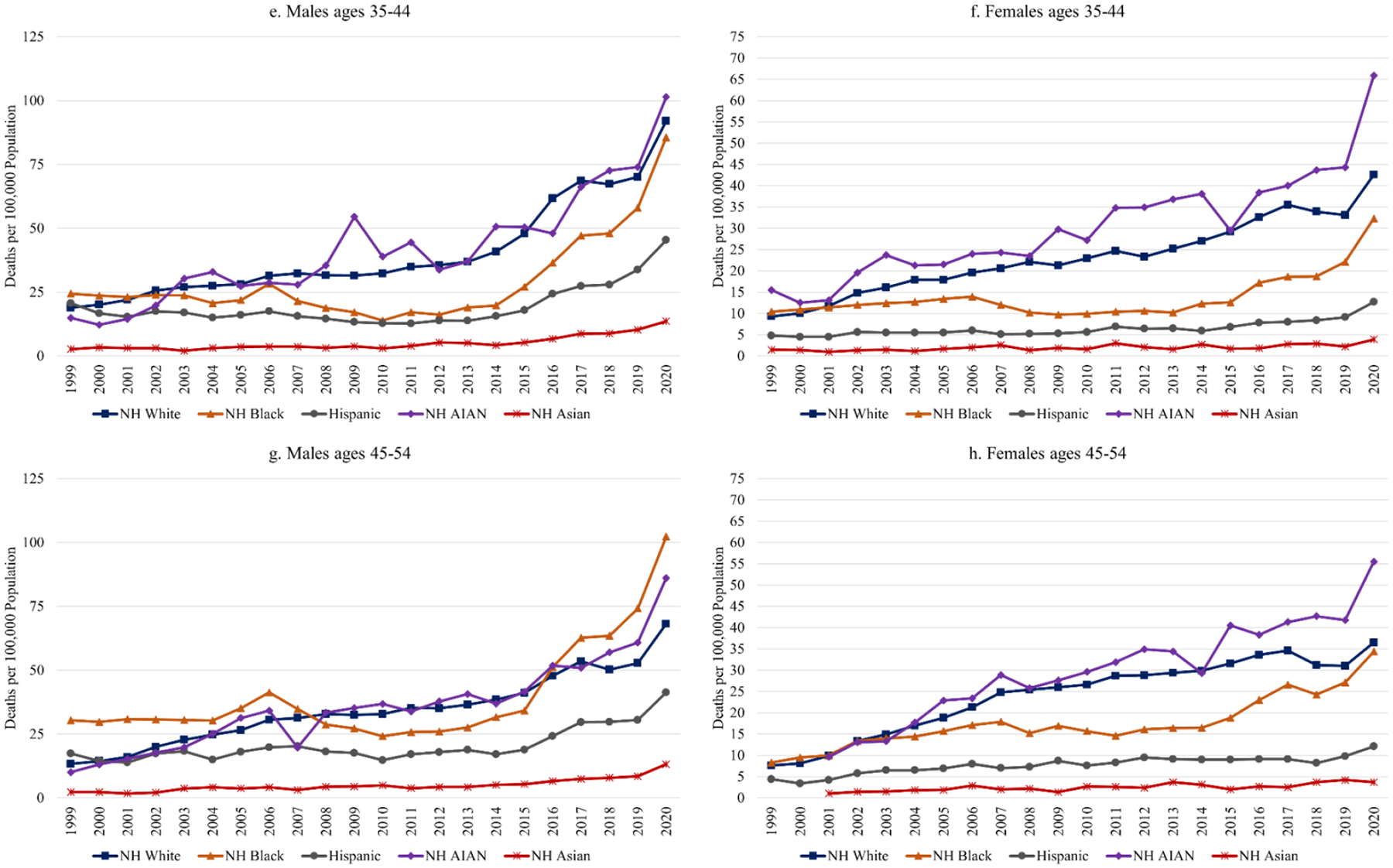
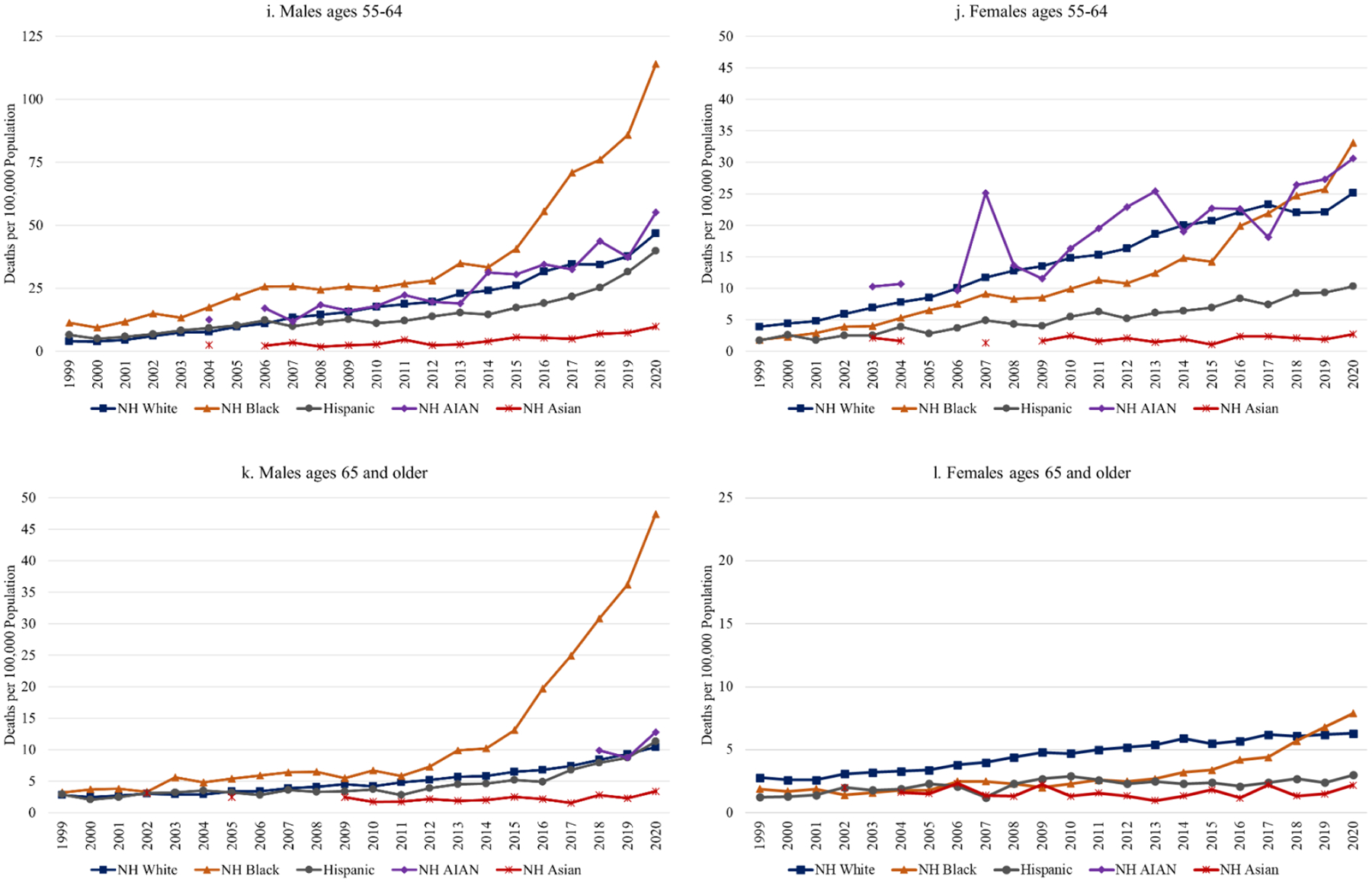
Age-Race-Sex Specific Fatal Drug Poisoning Rates, 1999–2020
SOURCE: CDC WONDER, Multiple Cause of Death Files (NCHS 2021).
NOTE: To abide by CDC suppression rules, rates are not shown for groups in years when there were fewer than 10 deaths in that group.
TABLE 1.
Coefficients from Ordinary Least Squares Regression Models Predicting Racial/Ethnic Differences in Fatal Drug Poisoning Rates by Age Group for Males, 1999–2020
| Overall (1999–2020) | Wave 1 (1999–2010) | Wave 2 (2011–2015) | Waves 3 and 4 (2016–2020) | |||||
|---|---|---|---|---|---|---|---|---|
| Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | |
| Ages 15–24 | ||||||||
| Intercept | 16.03 | <.001 | 12.93 | <.001 | 17.42 | <.001 | 22.10 | <.001 |
| Black | −11.05 | <.001 | −10.18 | <.001 | −13.46 | <.001 | −10.70 | .003 |
| Hispanic | −9.33 | <.001 | −8.62 | <.001 | −11.32 | <.001 | −9.04 | .009 |
| AIAN | −2.49 | .096 | −3.38 | .006 | −3.88 | <.001 | 1.02 | .748 |
| Asian | −12.86 | <.001 | −11.28 | <.001 | −13.86 | <.001 | −15.68 | <.001 |
| Ages 25–34 | ||||||||
| Intercept | 39.21 | <.001 | 23.98 | <.001 | 43.00 | <.001 | 71.68 | <.001 |
| Black | −21.20 | <.001 | −12.71 | <.001 | −29.36 | <.001 | −33.42 | <.001 |
| Hispanic | −23.95 | <.001 | −14.15 | <.001 | −30.34 | <.001 | −41.10 | <.001 |
| AIAN | −3.32 | .462 | −1.10 | .621 | −4.38 | .178 | −7.60 | .306 |
| Asian | −34.03 | <.001 | −21.43 | <.001 | −37.30 | <.001 | −61.02 | <.001 |
| Ages 35–44 | ||||||||
| Intercept | 40.19 | <.001 | 27.36 | <.001 | 39.22 | <.001 | 71.94 | <.001 |
| Black | −11.31 | .019 | −5.62 | .028 | −19.38 | <.001 | −16.90 | .064 |
| Hispanic | −20.88 | <.001 | −11.36 | <.001 | −24.44 | <.001 | −40.18 | <.001 |
| AIAN | 1.46 | .758 | 0.77 | .759 | 4.08 | .187 | 0.50 | .954 |
| Asian | −35.17 | <.001 | −24.16 | <.001 | −34.46 | <.001 | −62.32 | <.001 |
| Ages 45–54 | ||||||||
| Intercept | 34.40 | <.001 | 24.82 | <.001 | 37.28 | <.001 | 54.50 | <.001 |
| Black | 5.29 | 0.206 | 6.33 | .010 | −8.24 | <.001 | 16.30 | .041 |
| Hispanic | −13.93 | 0.001 | −7.73 | .002 | −19.32 | <.001 | −23.40 | .005 |
| AIAN | 1.48 | .723 | −0.51 | .831 | 0.90 | .574 | 6.82 | .371 |
| Asian | −29.50 | <.001 | −21.39 | <.001 | −32.70 | <.001 | −45.78 | <.001 |
| Ages 55–64 | ||||||||
| Intercept | 18.73 | <.001 | 9.62 | <.001 | 22.28 | <.001 | 37.04 | <.001 |
| Black | 17.31 | <.001 | 9.27 | <.001 | 10.50 | <.001 | 43.44 | <.001 |
| Hispanic | −4.19 | .367 | −0.50 | .784 | −7.66 | <.007 | −9.56 | .204 |
| AIAN | 2.18 | .638 | 1.56 | .392 | 2.26 | .387 | 3.58 | .628 |
| Asian | −15.29 | .001 | −7.76 | <.001 | −18.44 | <.001 | −30.20 | <.001 |
| Ages 65+ | ||||||||
| Intercept | 5.03 | <.001 | 3.36 | <.001 | 5.60 | <.001 | 8.46 | .001 |
| Black | 7.07 | <.001 | 1.71 | .001 | 3.66 | <.001 | 23.34 | <.001 |
| Hispanic | −0.58 | .739 | −0.26 | .615 | −1.40 | .131 | −0.54 | .869 |
| AIAN | 0.26 | .881 | 0.31 | .549 | 0.15 | .870 | 0.27 | .936 |
| Asian | −3.12 | .075 | −1.75 | .001 | −3.54 | <.001 | −6.02 | .078 |
NOTE: Coefficients represent the average difference in the fatal drug poisoning rate (deaths per 100,000 population) during the period identified at the top of the column. NH Whites are the reference category. P-values represent the statistical significance of difference between each racial/ethnic group and NH Whites within each age- and sex-specific category.
Among females, average rates over the period were significantly lower for Blacks, Hispanics, and Asians compared to Whites in every age group, except among ages 55 to 64, where the rate for Blacks was not significantly different from that for Whites (Table 2). AIAN females had significantly higher rates than White females among ages 25 to 44 and comparable rates in the other age groups. These differences were generally consistent across the waves, with some variation in the direction and significance of differences between Whites, Blacks, and AIANs depending on age group. Of note, the gap between AIAN females and the other racial/ethnic groups has widened in the last three years among ages 35 to 44 and 45 to 54. Overall, the highest average rates among females have been for AIANs ages 25 to 34 (22.6), 35 to 44 (29.7), 45 to 54 (28.4), and 55 to 64 (17.9); Whites ages 25 to 34 (17.4), 35 to 44 (22.3), and 45 to 54 (23.8); and Blacks ages 45 to 54 (17.8).
TABLE 2.
Coefficients from Ordinary Least Squares Regression Models Predicting Racial/Ethnic Differences in Fatal Drug Poisoning Rates by Age Group for Females, 1999–2020
| Overall (1999–2020) | Wave 1 (1999–2010) | Wave 2 (2011–2015) | Waves 3 and 4 (2016–2020) | |||||
|---|---|---|---|---|---|---|---|---|
| Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | |
| Ages 15–24 | ||||||||
| Intercept | 6.37 | <.001 | 4.49 | <.001 | 7.02 | <.001 | 10.24 | <.001 |
| Black | −3.95 | <.001 | −3.22 | <.001 | −5.02 | <.001 | −4.64 | .002 |
| Hispanic | −4.11 | <.001 | −3.04 | <.001 | −4.74 | <.001 | −6.06 | <.001 |
| AIAN | 0.35 | .622 | 0.12 | .796 | −0.48 | .253 | 1.72 | .203 |
| Asian | −4.86 | <.001 | −3.29 | <.001 | −5.65 | <.001 | −7.86 | <.001 |
| Ages 25–34 | ||||||||
| Intercept | 17.28 | <.001 | 10.72 | <.001 | 19.58 | <.001 | 30.72 | <.001 |
| Black | −9.29 | <.001 | −5.83 | <.001 | −12.76 | <.001 | −14.14 | .004 |
| Hispanic | −12.47 | <.001 | −7.73 | <.001 | −14.56 | <.001 | −21.74 | <.001 |
| AIAN | 4.38 | .048 | 3.42 | .013 | 4.48 | <.001 | 6.60 | .138 |
| Asian | −15.38 | <.001 | −9.30 | <.001 | −17.56 | <.001 | −27.78 | <.001 |
| Ages 35–44 | ||||||||
| Intercept | 23.24 | <.001 | 17.02 | <.001 | 25.88 | <.001 | 35.54 | <.001 |
| Black | −9.43 | <.001 | −5.44 | <.001 | −14.66 | <.001 | −13.76 | .002 |
| Hispanic | −16.80 | <.001 | −11.76 | <.001 | −19.38 | <.001 | −26.34 | <.001 |
| AIAN | 6.87 | .002 | 4.32 | .002 | 8.94 | <.001 | 10.92 | .010 |
| Asian | −21.26 | <.001 | −15.44 | <.001 | −23.66 | <.001 | −32.82 | <.001 |
| Ages 45–54 | ||||||||
| Intercept | 24.05 | <.001 | 17.82 | <.001 | 29.68 | <.001 | 33.38 | <.001 |
| Black | −6.51 | .006 | −3.82 | .085 | −13.20 | <.001 | −6.30 | .016 |
| Hispanic | −16.35 | <.001 | −11.46 | <.001 | −20.70 | <.001 | −23.72 | <.001 |
| AIAN | 3.88 | .096 | 0.84 | .701 | 4.52 | .003 | 10.54 | <.001 |
| Asian | −21.71 | <.001 | −16.07 | <.001 | −26.92 | <.001 | −30.02 | <.001 |
| Ages 55–64 | ||||||||
| Intercept | 14.11 | <.001 | 8.75 | <.001 | 18.18 | <.001 | 22.92 | <.001 |
| Black | −2.35 | .225 | −2.92 | .056 | −5.48 | <.001 | 2.14 | .304 |
| Hispanic | −8.86 | <.001 | −5.40 | <.001 | −12.00 | <.001 | −14.00 | <.001 |
| AIAN | 1.89 | .329 | 1.05 | .485 | 3.72 | .004 | 2.08 | .318 |
| Asian | −12.45 | <.001 | −7.34 | <.001 | −16.55 | <.001 | −20.62 | <.001 |
| Ages 65+ | ||||||||
| Intercept | 4.55 | <.001 | 3.56 | <.001 | 5.40 | <.001 | 6.10 | <.001 |
| Black | −1.50 | .001 | −1.58 | <.001 | −2.52 | <.001 | −0.30 | .780 |
| Hispanic | −2.38 | <.001 | −1.63 | <.001 | −2.98 | <.001 | −3.58 | .003 |
| AIAN | −0.23 | .596 | 0.10 | .826 | −1.07 | <.001 | −0.19 | .858 |
| Asian | −3.01 | <.001 | −2.02 | <.001 | −3.99 | <.001 | −4.41 | <.001 |
NOTE: Coefficients represent the average difference in the fatal drug poisoning rate (deaths per 100,000 population) during the period identified at the top of the column. NH Whites are the reference category. P-values represent the statistical significance of difference between each racial/ethnic group and NH Whites within each age- and sex-specific category.
The role different drugs have played in these trends can be observed in online appendix Figures A1 (males by race/ethnicity), A2 (females by race/ethnicity), and A3 (by age group). There are several important observations. First, prescription opioids were the largest contributor to overdoses for White and AIAN males and females in all age groups throughout most of the period. However, prescription opioids were not a major factor for Blacks and Hispanics. Among Black males and females, cocaine was the largest contributor throughout the 2000s and early 2010s. In fact, throughout the early 2000s, when public health officials started to raise alarms about increases in prescription opioid overdoses among Whites, cocaine overdoses were as high or higher among Black males. Second, heroin has made a much smaller contribution to overdoses among females than among males and in older age groups than in younger age groups. For White females, rates of overdose involving prescription benzodiazepines were higher than those involving heroin throughout the entire period. Third, overdoses involving synthetic opioids started to surge in 2016 and have made the largest contribution to overdoses among Whites, Blacks, and Hispanics since then. However, among AIANs up until 2020, rates of overdose involving methamphetamine had been higher than those involving synthetic opioids. Methamphetamine has also made substantial contributions to overdoses among Whites and Hispanics in recent years. Collectively, these trends illustrate that an overemphasis on opioids masks the nature and magnitude of the overdose crisis and does so in a way that marginalizes the overdose experiences of people of color.
Geographic differences
Figure 3 displays temporal trends in fatal drug poisoning rates by region, and Table 3 presents coefficients from regression models representing average differences overall and by wave. Overall, there were not significant regional differences when considering the timespan as a whole. However, in wave 1, the average rate was significantly lower in the Midwest compared to the West, but the average difference was only 2 deaths per 100,000 population. In addition, by wave 3, average rates in the Northeast, Midwest, and South were all significantly higher compared to the West, ranging from 5 to 12 deaths per 100,000 population higher on average. The large spikes in these three regions in 2017 (see Figure 3) were major contributors to their divergence from the trends in the West.
FIGURE 3.
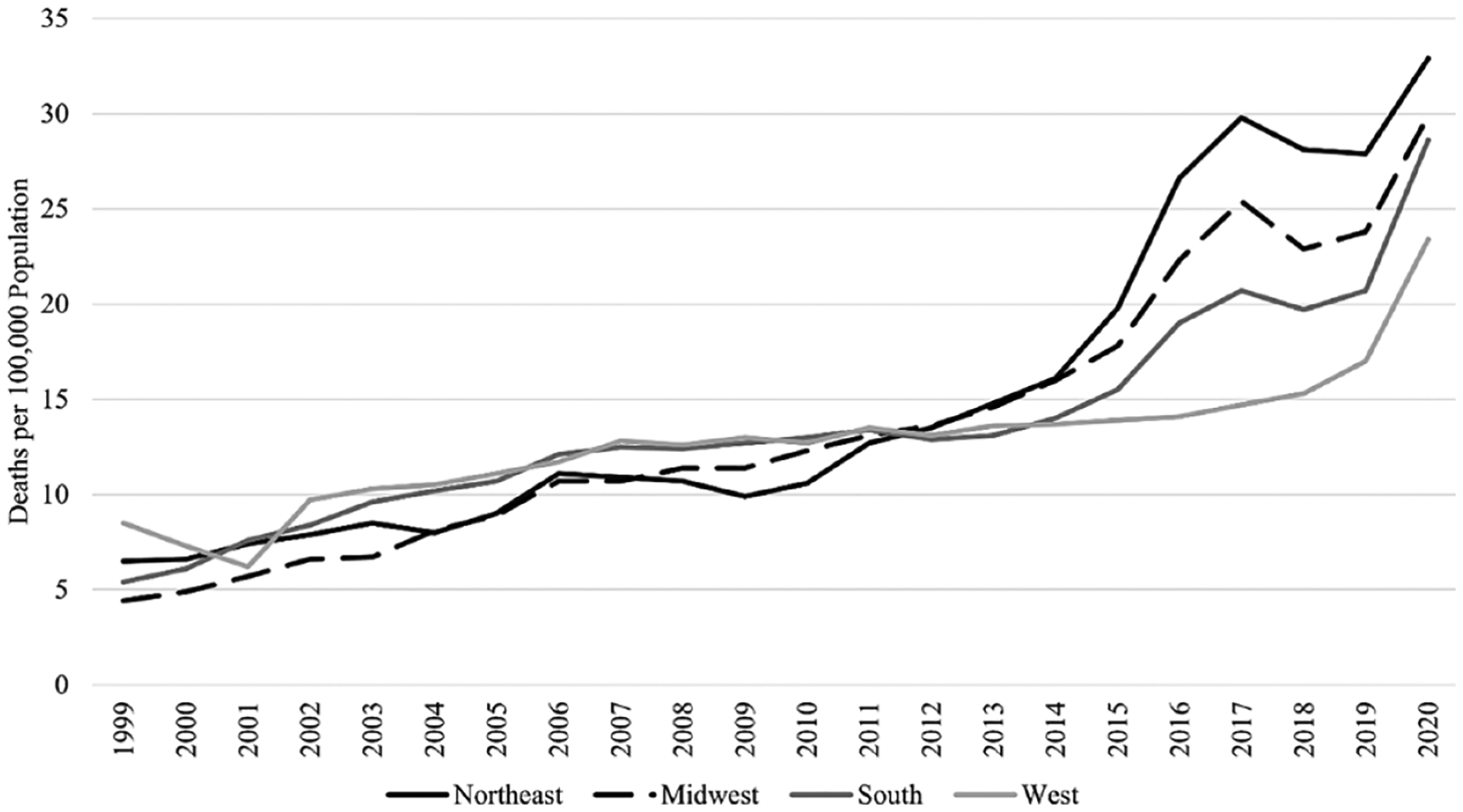
Fatal Drug Poisoning Rates by Region, 1999–2020
SOURCE: CDC WONDER, Multiple Cause of Death Files (NCHS 2021).
NOTE: Rates are age adjusted.
TABLE 3.
Coefficients from Ordinary Least Squares Regression Models Predicting Regional Differences in Fatal Drug Poisoning Rates, 1999–2020
| Overall (1999–2020) | Wave 1 (1999–2010) | Wave 2 (2011–2015) | Waves 3 and 4 (2016–2020) | |||||
|---|---|---|---|---|---|---|---|---|
| Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | |
| Intercept (ref = West) | 12.67 | <.001 | 10.53 | <.001 | 13.56 | <.001 | 16.90 | <.001 |
| Northeast | 2.30 | .241 | −1.61 | .106 | 1.82 | .125 | 12.16 | <.001 |
| Midwest | 1.02 | .607 | −2.05 | .041 | 1.46 | .212 | 7.96 | .002 |
| South | 0.89 | .648 | −0.48 | .629 | 0.22 | .847 | 4.84 | .036 |
NOTE: Rates are age adjusted. Coefficients represent the average difference in the fatal drug poisoning rate (deaths per 100,000 population) over the period identified at the top of the column. West is the reference region.
The county-level maps presented in Figure 4 demonstrate that there is also substantial variation within regions. Throughout most of wave 1, the highest rates were clustered in central Appalachia and small clusters in the Southwest. By wave 2, high rates spread to cover a wider range of Appalachia, parts of the industrial Midwest, and several counties in Oklahoma and Missouri. By waves 3 and 4, rates had increased substantially across New England and along the East Coast. Of the 100 counties with highest rates in 2018 to 2020 (see Figure 4), nearly half (45) are in Appalachia, and rates were high across several counties in the mid-Atlantic, Florida, southern Louisiana, and the Southwest. Throughout all waves, rates have remained comparatively low in the Mississippi Delta, most parts of Texas, and throughout much of the Great Plains (with the exception of counties with large AIAN populations).
FIGURE 4.
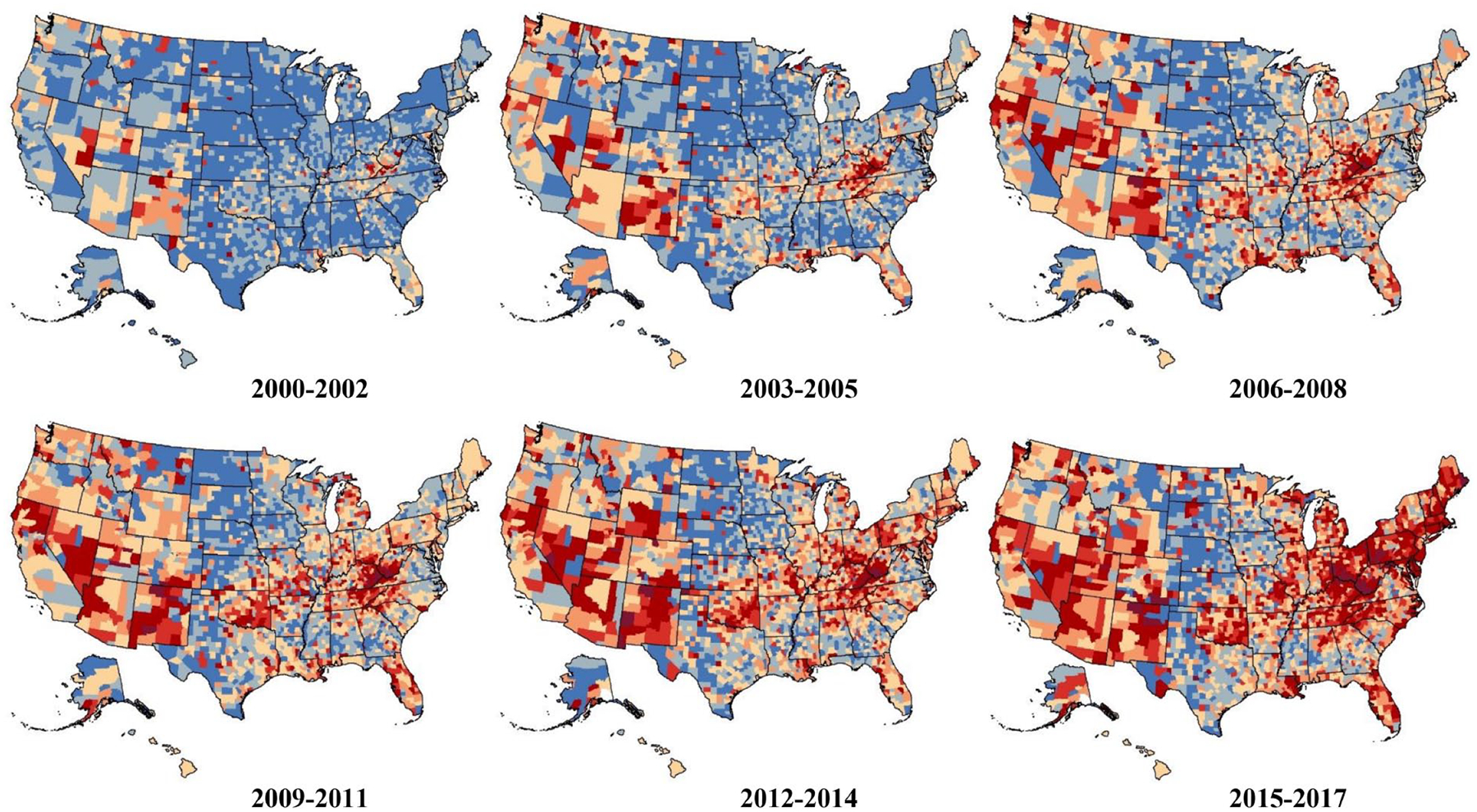
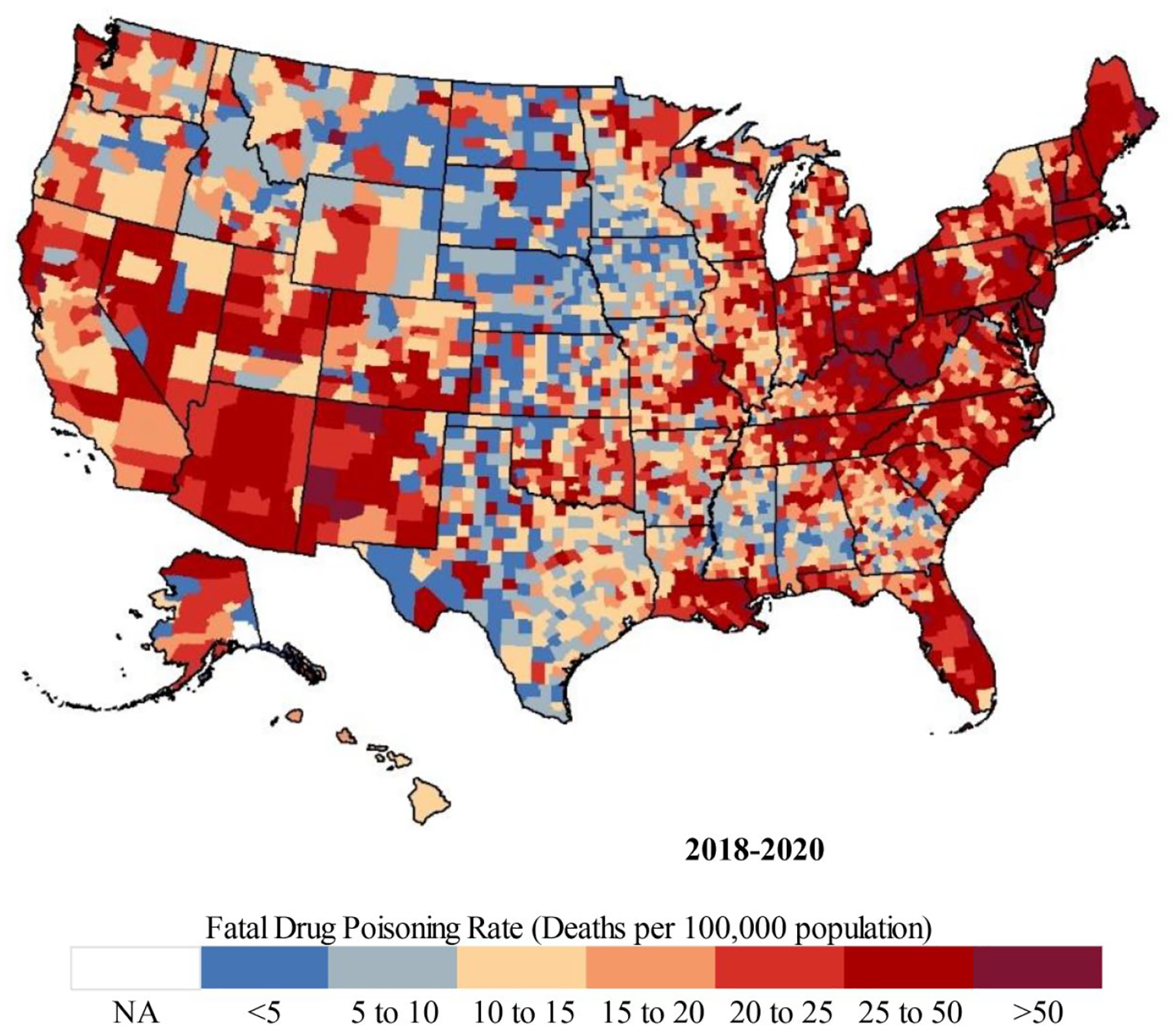
Fatal Drug Poisoning Rates by County, 2000–2020
SOURCE: NCHS, National Vital Statistics System restricted use death certificate files, 2000–2020.
NOTE: Rates are age adjusted. Deaths are pooled across three years to avoid large fluctuations that can occur in counties with small populations and low death counts. NA = data not available.
Analyses of trends involving specific drugs show that prescription opioids were the dominant driver throughout the 2000s and early-2010s only in the South and West (see online appendix Figure B1). In the Northeast, cocaine started out as the primary driver until 2006, after which prescription opioid overdoses surpassed those from cocaine. In the Midwest, rates of overdose involving prescription opioids and cocaine were comparable until 2007, when overdoses involving cocaine started to decline and those involving prescription opioids continued to increase. Heroin played a major role only throughout the early- to mid-2010s and only in the Northeast and Midwest. In fact, in both the South and the West, heroin overdose rates did not surpass prescription opioid overdose rates in any year. By the mid-2010s (wave 3), synthetic opioids were the primary contributor in all regions except the West, where methamphetamine played a larger role. Methamphetamine is now the second most common substance involved in overdoses (after synthetic opioids) in the Midwest and South, while cocaine is the second most common substance in the Northeast.
Finally, Figure 5 shows fatal drug poisoning rates across the urban-rural continuum for 1999 to 2020, and Table 4 presents coefficients from regression models. There were not significant differences in average rates across the urban-rural continuum for the period 1999 to 2020 overall, nor in waves 1 and 2. By waves 3 and 4, the average rate was significantly higher in medium metro counties (compared to nonmetro noncore counties). Nonmetro counties did have the highest average annual increases and largest overall increases from 1999 to 2020 (online appendix Table B2).
FIGURE 5.
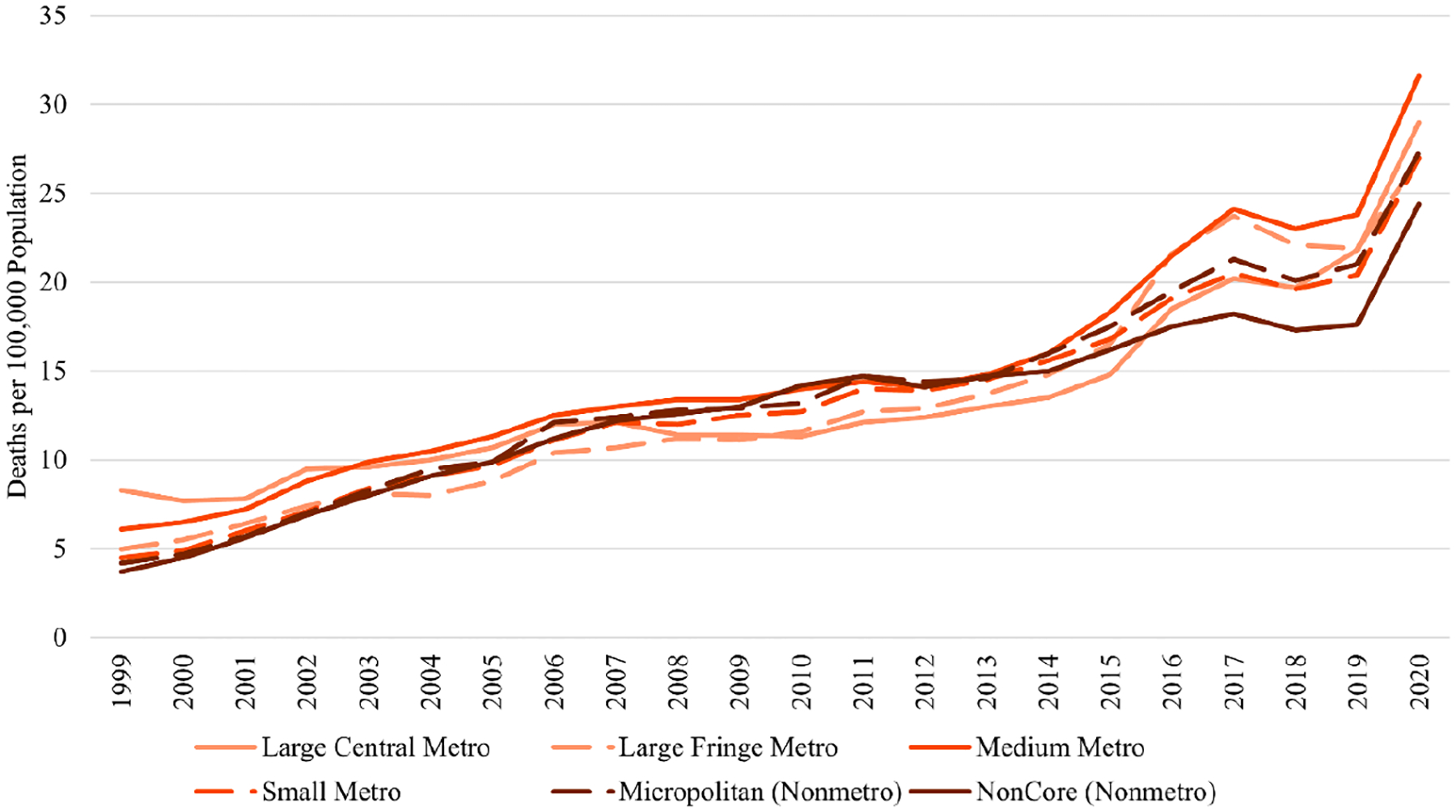
Fatal Drug Poisoning Rates by Urban-Rural Continuum, 1999–2020
SOURCE: CDC WONDER, Multiple Cause of Death Files (NCHS 2021).
NOTE: Rates are age adjusted.
TABLE 4.
Coefficients from Ordinary Least Squares Regression Models Predicting Urban-Rural Continuum Differences in Fatal Drug Poisoning Rates, 1999–2020
| Overall (1999–2020) | Wave 1 (1999–2010) | Wave 2 (2011–2015) | Waves 3 and 4 (2016–2020) | |||||
|---|---|---|---|---|---|---|---|---|
| Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | Avg. Diff. in Rate | Pr > |t| | |
| Intercept (ref = nonmetro noncore) | 12.75 | <.001 | 9.24 | <.001 | 14.94 | <.001 | 19.00 | <.001 |
| Large central metro | 0.74 | .676 | 0.91 | .438 | −1.78 | .043 | 2.84 | .192 |
| Large fringe metro | 0.47 | .788 | −0.56 | .633 | −0.82 | .337 | 4.24 | .057 |
| Medium metro | 2.16 | .220 | 1.31 | .265 | 0.58 | .492 | 5.80 | .011 |
| Small metro | 0.50 | .778 | −0.07 | .955 | 0.02 | .981 | 2.32 | .284 |
| Nonmetro micropolitan | 0.84 | .633 | 0.15 | .898 | 0.50 | .553 | 2.84 | .192 |
NOTE: Rates are age-adjusted. Coefficients represent the average difference in the fatal drug poisoning rate (deaths per 100,000 population) over the period identified at the top of the column. Nonmetro noncore is the reference category.
Despite few significant differences in rates overall, the contributions of specific drugs to overdoses vary across the urban-rural continuum (online appendix Figure B2). Prescription opioid overdoses rose more rapidly outside of large metro counties during wave 1, and prescription opioids were the largest contributor to overdoses (by far) until 2016 in small and medium metro counties and nonmetro counties. Cocaine played an important role in large central and fringe metro counties in both the early years and more recent years of the crisis. During wave 2, heroin was a major contributor only in metro counties. During waves 3 and 4, synthetic opioid overdoses surged in all metro status categories, with methamphetamine playing an increasingly important role since the mid-2010s across all categories and cocaine playing an important role in large and medium metro counties.
Discussion
The U.S. is now in the third decade of a devastating drug overdose crisis that has claimed over one million lives. The economic, social, and personal tolls of this crisis have been substantial, and some population subgroups and geographic areas are bearing heavier burdens than others. This article has focused on the groups and places that have been most affected by fatal overdoses, but we should bear in mind that these overdose deaths represent only a tiny fraction of those suffering from substance use disorders. A large share of people who suffer from substance use disorders are in need of mental health and substance use treatment and social services. In addition, as several of the articles in this volume show, the effects of the crisis ripple beyond those who die to include families, friends, first responders, service providers, and employers. Below, I point to several key takeaways that advance our understanding of who has been most affected by the contemporary U.S. overdose crisis, demonstrating that the most affected groups have varied over time and that different drugs (including nonopioid drugs) have contributed to the trends.
The first main takeaway is that the consequences of the overdose crisis have been felt unequally across demographic groups. Among all age groups and all racial/ethnic groups, rates were consistently higher among males than among females. This is consistent with data showing greater prevalence of use of almost all types of illicit drugs and higher risk use among males (National Institute on Drug Abuse 2020). The age patterns observed (higher rates among working-age adults) are also consistent with life course patterns of substance use. Although most drug use is initiated and prevalence is highest during adolescence and early adulthood (Rigg, Monnat, and Chavez 2018; Verdery et al. 2020), overdose rates are higher in young adulthood and middle age because younger people tend to increase the amount of drugs they use as their tolerance to drugs increase (Scholl et al. 2019). However, the increasing lethality of the drug supply means that even recreational use, which is common among adolescents and young adults, puts people at risk of overdose.
In terms of racial/ethnic differences, Hispanics and Asians consistently had lower rates than the other groups, regardless of age and sex. In the younger ages (15–44), White and American Indian males and females had the highest rates throughout the entire study period. However, in the older age groups (55 and older), Black males had the highest rates. The older Black male disadvantage has been especially pronounced since the mid-2010s. Rates among older Black females also surpassed those of their White peers in the last couple of years. These trends demonstrate that the overdose crisis has not disproportionately affected Whites. To be sure, rates rose earlier among younger and working-age Whites than among Blacks. Given that the early wave of the overdose crisis was driven by prescription opioids, lower rates of physician prescribing of opioids to Blacks likely played an important role (Morden et al. 2021). In more recent years, the increasing contamination of heroin and cocaine with fentanyl is likely a major explanation for the surge in overdose rates among Blacks. Researchers who aim to test the role of psychological well-being on overdose trends will need to contend with why overdose rates are higher in the younger age groups among White and AIAN males but higher in the older age groups among Black males. Explanations may have to do with the timing of declining opportunities (i.e., earlier for Blacks) in the communities where these groups are concentrated.
Second, overdose rates vary substantially across different parts of the U.S. While there were not significant regional differences in average overdose rates in waves 1 and 2, rates were highest in the Northeast in waves 3 and 4. The surge in overdoses in the Northeast has been driven largely by fentanyl, with cocaine also playing an important role. Most fentanyl coming to the U.S. in the mid- to late 2010s was coming from China and relied on access to shipping ports. Fentanyl-involved overdoses started to increase faster and earlier in the Northeast and Midwest due to those regions’ proximity to shipping ports. However, most fentanyl now enters the U.S. from Mexico, opening up the West and South to cheap massive supplies of the lethal drug (Quinones 2021).
Despite the perception that rural areas have been disproportionately affected, average overdose rates were statistically comparable across the rural-urban continuum for most of the study period. By wave 3, the most rural counties had the lowest overall rate of all county types, and medium-sized metro counties had the highest rate. However, as is clear by observing the county-level maps, rural America is not monolithic. While some rural counties have among the lowest rates in the country, others have among the highest. Indeed, most of the counties with the highest rates are in the heart of Appalachia—downtrodden places with a long history of economic decline and substance use, multiple adverse health outcomes, and high rates of premature mortality in general.
Finally, this article demonstrates that our problem is bigger than opioids. Overdoses involving prescription opioids rose earlier and more rapidly outside of large metro counties, and cocaine and heroin played larger roles in large metro counties. This is consistent with research by Peters et al. (2020) that examined drug-specific overdose rates through 2016. While prescription opioids were the largest contributor to overdoses among Whites throughout most of the study period, they were never the largest contributor among Blacks. Heroin overdoses were a large contributor only for a short period and only in metro counties in the Northeast and Midwest. Although synthetic opioids (fentanyl) continue to be the largest contributor among most groups and in most places, the roles of other drugs, such as cocaine and methamphetamine, are large and growing. Among Blacks, cocaine was the largest contributor to overdoses until 2016 (playing a far greater role than prescription opioids or heroin), and it remains the second largest contributor to date after synthetic opioids. Methamphetamine is now the second most common drug involved in overdoses overall and the most common among American Indians and in the western region of the U.S. Methamphetamine is also playing an increasingly important role in overdoses among Whites and Hispanics. Even though overdose rates tend to be lower from methamphetamine than from opioids (because opioids depress breathing and methamphetamine does not), methamphetamine has devastating effects on the physical and mental health of users, with many adverse conditions leading to premature mortality that is not captured in overdose data due to the nuances of death certification.
The increasing share of overdoses that involve nonopioid drugs illustrate that the terminology of the “opioid epidemic” is overly simplistic and outdated (Peppin, Raffa, and Schatman 2020). Our problem is bigger than opioids. Focusing on one substance, like opioids, risks masking the nature and magnitude of the overdose crisis, and it does so in ways that marginalize the overdose experiences of people of color and certain geographic areas. Moreover, a focus on opioids means that policies and treatment interventions tend to focus on limiting supply of that specific substance (e.g., prescribing limits, border interdiction) or developing and funding treatment and harm reduction approaches that are limited to opioid use (e.g., Narcan, medication assisted therapies) rather than addressing the underlying causes of widespread use and overdose.
This article presents the most comprehensive portrait to date of where and among whom the contemporary drug overdose crisis has taken the most severe toll, but these analyses were limited in several ways, presenting opportunities for future research and analysis. First, it was beyond the scope of this article to test potential explanations for the observed differences. There will not be one explanation that captures all the different types of variation (age group, racial/ethnic, sex, geographic). Instead, as with other population health disparities, the explanations are likely to be multilevel (moving from the structural to the proximate) and multidimensional. The role of psychological well-being has generated substantial attention. While several studies have aimed to examine the role of psychological well-being (at both the individual and place levels), the data necessary to establish causality has been limited. Qualitative research offers insights for scientists who seek to develop and test how “despair” is related to demographic and geographic trends in drug use and overdose (Chen 2015; McLean 2016; Silva 2019). Beyond the critical qualitative research, it is essential that U.S. agencies who fund research invest in longitudinal data collection across the life course with large enough samples to enable robust analysis of subgroup and place-level differences. Much like what is currently done in the National Longitudinal Study of Adolescent to Adult Health (AddHealth), longitudinal surveys should capture a wide range of information on substance use, economic and employment indicators, psychological well-being, physical health, living arrangements, social relationships, and other factors that may influence substance use. Data infrastructure efforts should include linking individual-level survey and biomarker data with mortality data and with data that characterize individuals’ residential, macroeconomic, and policy settings across the life course.
Related to this is the fact that research on upstream factors that drive the proximate risk factors for overdose (i.e., the causes of the causes of the causes) is scant. This is partly because causal research is prioritized over descriptive research, especially in certain disciplines. It is difficult to do causal research on upstream drivers. Researchers cannot randomize 40 years of economic restructuring to study its “cause” on drug overdose disparities. Yet existing research provides suggestive evidence that these long-term processes matter substantially when it comes to overdose trends. We can learn a lot from descriptive research. By privileging causal research, we hamstring ourselves from advocating for truly transformative upstream solutions and, instead, default to incremental (typically ineffective) solutions that target individual behaviors. We need research that explores how long-term changes in federal and state policies and macroeconomic conditions affect substance use and overdose.
Third, I was unable to present trends by socioeconomic status (SES), even though SES is likely to be a major determinant of drug overdose. National Vital Statistics System (death certificate) data do not include information on decedents’ income, prohibiting the examination of mortality trends by income level. Although most death certificates do include decedents’ educational attainment, there are well-established issues of accuracy, availability, and quality of the educational attainment field on death certificates (NASEM 2021; Rostron, Boies, and Arias 2010; Sorlie and Johnson 1996). Others have shown that increases in drug overdoses over the past three decades have been concentrated among individuals without a four-year college degree (Case and Deaton 2015, 2017, 2020; Geronimus et al. 2019; Ho 2017; Sasson 2016).
Finally, there is already evidence that the COVID-19 pandemic has exacerbated the long-term drug overdose crisis (NCHS 2021). Overdose rates surged for all demographic and geographic groups between 2019 and 2020 (and have continued to do so since 2020). Researchers should examine how various federal, state, and local COVID-19 mitigation policies, economic changes, changes in treatment availability and modalities, and changes to the U.S. drug supply over this period contributed to the recent surge in drug overdose deaths.
Policy implications
The U.S. has enacted various policies to quell the overdose epidemic. Substantial efforts have focused on curbing supply (prescribing limits, prescription drug monitoring programs, interdiction, mass incarceration). Yet overdose rates continue to increase in the face of these supply-side interventions. Supply is important, but it does not occur in a vacuum. As long as there is demand for substances, suppliers will find a way to meet that demand, and people with substance use disorders will use whatever substance is available to meet their needs. This suggests that policies should instead focus on (1) making drug use as safe as possible for existing users (to reduce overdose rates in the short term) and (2) preventing risky drug use initiation to reduce overdose rates in the long term.
In the immediate term, harm reduction approaches are essential. These include increasing access to medication assisted treatment (MAT), Narcan (the opioid overdose reversal drug), and fentanyl test strips so users can check whether the product they are using contains fentanyl. But these strategies are only tourniquets.
Among the biggest failures of U.S. public health is that we invest most of our resources into tackling problems after they emerge rather than investing in the institutions and community-level infrastructure that will prevent problems from emerging. This explains why we spend more money on health care than any other advanced country, and yet U.S. life expectancy is declining. Insofar as government policies and actions have gotten us into this mess, the government must play a role in addressing the crisis. The U.S. has disinvested in the very institutions that help build strong and resilient communities and instead has enacted policies that aim to maximize corporate profit almost always at the expense of population health. Early childhood is a key target for preventive interventions. For example, PROSPER is an evidence-based program that links children and parents with schools to promote prosocial interactions and reduce substance use. But interventions are also needed to reinvigorate left-behind communities. Good economic policy is good public health policy. This means that we must invest in policies that increase the availability of secure livable wage jobs and safe affordable housing. O’Brien, Bair, and Venkataramani’s (2022) finding that state Medicaid program generosity substantially mitigated the effects of automation on drug overdose mortality suggests that economic policies can play a role in buffering or exacerbating local area economic conditions. The need for long-term investments means that policy-makers and the public need to get comfortable with the idea that policy impacts may not be instantaneous. This is difficult in a political environment where politicians are constantly working toward reelection, but we did not get into this mess overnight, and we cannot expect that short-term downstream solutions will get us out of it.
Supplementary Material
Acknowledgments
The author acknowledges research funding from the National Institute on Drug Abuse (U01 DA055972) and the National Institute on Aging (NIA)–funded Center for Aging and Policy Studies at Syracuse University (P30AG066583) and support from two research networks funded by the NIA (R24 AG065159 and 2R24 AG045061), the NICHD (National Institute of Child Health and Human Development)-funded Population Research Institute at Pennsylvania State University State (P2CHD041025), the Rural Population Research Network – a U.S. Department of Agriculture (USDA) Agricultural Experiment Station Multistate Research Project (W5001), and the Syracuse University Lerner Center for Public Health Promotion and Population Health.
Footnotes
“Drug poisoning” is the official term used by the CDC to describe fatal overdose deaths. It is also the terminology used in the ICD-10 codes as detailed in the previous footnote.
Supplemental Material
Supplemental material for this article is available online.
References
- Alpert AE, Evans WN, Lieber EM, and Powell D 2019. Origins of the opioid crisis and its enduring impacts. NBER Working Paper no. 26500, National Bureau of Economic Research, Cambridge, MA. Available from https://www.nber.org/papers/w26500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton Linda M., Lichter Daniel T., Baker Regina S., and Eason John M.. 2013. Inequality, family processes, and health in the “new” rural America. American Behavioral Scientist 57 (8): 1128–51. [Google Scholar]
- Case Anne, and Deaton Angus. 2015. Rising morbidity and mortality in midlife among White non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences 112 (49): 15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Anne, and Deaton Angus. 23 March 2017. Morbidity and mortality in the 21st century. Brookings. Available from https://www.brookings.edu/bpea-articles/mortality-and-morbidity-in-the-21st-century/ (accessed 5 January 2022). [Google Scholar]
- Case Anne, and Deaton Angus. 2020. Deaths of despair and the future of capitalism. Princeton, NJ: Princeton University Press. [Google Scholar]
- Chen Victor Tan. 2015. Cut loose: Jobless and hopeless in an unfair economy. Berkeley, CA: University of California Press. [Google Scholar]
- Cherlin Andrew J. 2018. Psychological health and socioeconomic status among non-Hispanic Whites. Proceedings of the National Academy of Sciences 115 (28): 7176–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero Thedore, Ellis Matthew, and Kasper Zachary. 2020. Polysubstance use: A broader understanding of substance use during the opioid crisis. American Journal of Public Health 110 (2): 224–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero Theodore J., and Surratt Hilary L.. 2012. Effect of abuse-deterrent formulation of OxyContin. New England Journal of Medicine 367:187–89. [DOI] [PubMed] [Google Scholar]
- Dasgupta Nabarun, Beletsky Leo, and Ciccarone Daniel. 2018. Opioid crisis: No easy fix to its social and economic determinants. American Journal of Public Health 108 (2): 182–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim Emile. 1897/1966. Suicide. New York, NY: Free Press. [Google Scholar]
- Ellis Matthew S., Kasper Zachary A., and Cicero Theodore J.. 2018. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug and Alcohol Dependence 193 (1): 14–20. [DOI] [PubMed] [Google Scholar]
- Gaydosh Lauren, Hummer Robert A., Hargrove Taylor W., Halpern Carolyn T., Hussey Jon M., Whitsel Eric A., Dole Nancy, and Harris Kathleen Mullan. 2019. The depths of despair among US adults entering midlife. American Journal of Public Health 109 (5): 774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T., Bound John, Waidmann Timothy A., Rodriguez Javier M., and Timpe Brenden. 2019. Weathering, drugs, and whack-a-mole: Fundamental and proximate causes of widening educational inequity in U.S. life expectancy by sex and race, 1990–2015. Journal of Health and Social Behavior 60 (2): 222–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman Noreen, Glei Dana A., and Weinstein Maxine. 2018. Declining mental health among disadvantaged Americans. Proceedings of the National Academy of Sciences 115 (28): 7290–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham Carol, and Pinto Sergio. 2019. Unequal hopes and lives in the USA: Optimism, race, place, and premature mortality. Journal of Population Economics 32:665–733. [Google Scholar]
- Graham Carol, Pinto Sergio, and Juneau John II. 2017. The geography of desperation in America. Brookings. Available from https://www.brookings.edu/research/the-geography-of-desperation-in-america/ (accessed 6 January 2022). [Google Scholar]
- Ho Jessica Y. 2017. The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992–2011. Demography 54 (3): 1175–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth Alex, Ruhm Christopher J., and Simon Kosali. 2017. Macroeconomic conditions and opioid abuse. Journal of Health Economics 56:222–33. [DOI] [PubMed] [Google Scholar]
- Hoopsick Rachel A., Homish Gregory G., and Leonard Kenneth E.. 2021. Differences in opioid overdose mortality rates among middle-age adults by race/ethnicity and sex, 1999–2018. Public Health Reports 136 (2): 192–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes Katherine M., Magdalena Cerdá Joanne E. Brady, Havens Jennifer R., and Galea Sandro. 2014. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health 104 (2): E52–E59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean Katherine. 2016. “There’s nothing here”: Deindustrialization as risk environment for overdose. International Journal of Drug Policy 29:19–26. [DOI] [PubMed] [Google Scholar]
- Monnat Shannon M. 2018. Factors associated with county-level differences in U.S. drug-related mortality rates. American Journal of Preventive Medicine 54 (5): 611–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat Shannon M. 2019. The contributions of socioeconomic and opioid supply factors to U.S. drug mortality rates: Urban-rural and within-rural differences. Journal of Rural Studies 68:319–35. [Google Scholar]
- Monnat Shannon M. 2020a. Opioid crisis in the rural U.S. In Rural families and communities in the United States, eds. Glick Jennifer E., McHale Susan M., and King Valarie, 117–43. New York, NY: Springer. [Google Scholar]
- Monnat Shannon M. 2020b. Trends in U.S. working-age non-Hispanic White mortality: Rural-urban and within-rural differences. Population Research and Policy Review 39 (5): 805–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat Shannon M., Peters David J., Berg Mark, and Hochstetler Andrew. 2019. Using census data to understand county-level differences in overall drug mortality and opioid-related mortality by opioid type. American Journal of Public Health 109:1084–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morden Nancy E., Chyn Deanna, Wood Andrew, and Meara Ellen. 2021. Racial inequality in prescription opioid receipt—role of individual health systems. New England Journal of Medicine 385:342–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig Peter A., Reynolds Megan, Fink David S., Zafari Zafar, and Geronimus Arline T.. 2018. America’s declining well-being, health, and life expectancy: Not just a White problem. American Journal of Public Health 108 (12): 1626–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. 2021. High and rising mortality rates among working-age adults. Washington, DC: The National Academies Press. Available from 10.17226/25976. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2021. Underlying cause of death 1999–2020. CDC WONDER online database Atlanta, GA: Centers for Disease Control and Prevention. Available from http://wonder.cdc.gov/ucd-icd10.html (accessed 5 January 2022). [Google Scholar]
- National Center for Health Statistics. 2022. Provisional drug overdose death counts. Available from https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm (accessed 10 June 2022).
- National Institute on Drug Abuse. 2020. Sex and gender differences in substance use. Available from https://nida.nih.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use (accessed 10 June 2022).
- O’Brien Rourke, Bair Elizabeth F., and Venkataramani Atheendar S.. 2022. Death by robots? Automation and working-age mortality in the United States. Demography 59 (2): 607–28. [DOI] [PubMed] [Google Scholar]
- Peppin John F., Raffa Robert B., and Schatman Michael E.. 2020. The polysubstance overdose-death crisis. Journal of Pain Research 13:3405–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters David. J., Monnat Shannon M., Hochstetler Andrew, and Berg Mark. 2020. The opioid hydra: Understanding mortality epidemics and pandemics across the rural-urban continuum. Rural Sociology 85 (3): 589–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce Justin R., and Schott Peter K.. 2020. Trade liberalization and mortality: Evidence from US counties. American Economic Review: Insights 2 (1): 47–64. [Google Scholar]
- Piro Luigia, Martinotti Giovanni, Santacroce Rita, Vannini Chiara, Montemitro Chiara, Giorgetti Raffaele, Schifana Fabrizio, Fracticelli Silvia, Baroni Gaia, and di Giannantonio Massino. 2019. Substance screening in a sample of “clubbers”: Discrepancies between self-reporting and urinalysis. Evidence Based Psychiatric Care 5:10–16. [Google Scholar]
- Pitt Allison L., Humphreys Keith, and Brandeau Margaret L.. 2018. Modeling health benefits and harms of public policy responses to the US opioid epidemic. American Journal of Public Health 108 (10): 1394–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell David, and Pacula Rosalie Liccardo. 2021. The evolving consequences of OxyContin reformulation on drug overdoses. American Journal of Health Economics 9 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinones Sam. 2015. Dreamland: The true tale of America’s opiate epidemic. New York, NY: Bloomsbury Press. [Google Scholar]
- Quinones Sam. 2021. The least of us: True tales of America and hope in the time of fentanyl and meth. New York, NY: Bloomsbury Press. [Google Scholar]
- Rigg Khary K., Katherine McLean Shannon M. Monnat, Sterner Glenn E III, and Verdery Ashton M.. 2018. Opioid misuse initiation: implications for intervention. Journal of Addictive Diseases 37 (3–4): 111–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg Khary K., Monnat Shannon M., and Chavez Melody N.. 2018. Opioid-related mortality in rural America: Geographic heterogeneity and intervention strategies. International Journal of Drug Policy 57:119–29. [DOI] [PubMed] [Google Scholar]
- Rostron Brian L., Boies John L., and Arias Elizabeth. 2010. Education reporting and classification on death certificates in the United States. Vital and Health Statistics. Series 2, Data Evaluation and Methods Research 1–21. [PubMed] [Google Scholar]
- Ruhm Christopher. 2019. Drivers of the fatal drug epidemic. Journal of Health Economics 64:25–42. [DOI] [PubMed] [Google Scholar]
- Sasson Isaac. 2016. Diverging trends in cause-specific mortality and life years lost by educational attainment: Evidence from United States vital statistics data, 1990–2010. PLoS ONE 11 (10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl Lawrence, Seth Puja, Kariisa Mbabazi, Wilson Nana, and Baldwin Grant. 2019. Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity and Mortality Weekly Report 67 (5152): 1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva Jennifer M. 2019. We’re still here: Pain and politics in the heart of America. New York, NY: Oxford University Press. [Google Scholar]
- Sorlie Paul D, and Johnson Norman J.. 1996. Validity of education information on the death certificate. Epidemiology 7 (4): 437–39. [DOI] [PubMed] [Google Scholar]
- Stein Elizabeth M., Gennuso Keith P., Ugboaja Donna C., and Remington Patrick L.. 2017. The epidemic of despair among White Americans: Trends in the leading causes of premature death, 1999–2015. American Journal of Public Health 107 (10): 1541–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Drug Enforcement Administration. 2017. National drug threat assessment. DEA-DCT-DIR-040-17. Available from https://www.dea.gov/documents/2017/10/01/2017-national-drug-threat-assessment (accessed 10 June 2022).
- U.S. Drug Enforcement Administration. 2021. Sharp increase in fake prescription pills containing fentanyl and meth. Available from https://www.dea.gov/alert/sharp-increase-fake-prescription-pills-containing-fentanyl-and-meth (accessed 10 June 2022).
- Van Zee Art. 2009. The promotion and marketing of OxyContin: Commercial triumph, public health tragedy. American Journal of Public Health 99 (2): 221–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkataramani Atheendar S., Bair Elizabeth F., O’Brien Rourke L., and Tsai Alexander C.. 2020. Association between automotive assembly plant closures and opioid overdose mortality in the United States: A difference-in-differences analysis. JAMA Internal Medicine 180 (2): 254–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdery Ashton M., England Kira, Chapman Alexander, Luo Liying, McLean Katherine, and Monnat Shannon. 2020. Visualizing age, period, and cohort patterns of substance use in the U.S. opioid crisis. Socius 6:2378023120906944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell Nancy R., Beals Janette, Big Crow Cecelia, Mitchelle Christina M., and Novins Douglas K.. 2012. Epidemiology and etiology of substance use among American Indians and Alaska Natives. American Journal of Drug and Alcohol Abuse 38 (5): 376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob Michael J., and Salemi Jason L.. 2017. Bowling alone, dying together: The role of social capital in mitigating the drug overdose epidemic in the United States. Drug and Alcohol Dependence 173:1–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


