Abstract
Background
Despite the increased frequency of cephalomedullary fixation for unstable intertrochanteric hip fractures, failure with screw cut-out and varus collapse remains a significant failure mode. Proper positioning of implants into the femoral neck and head directly influences the stability of fracture fixation. Visualization of the femoral neck and head can be challenging and failure to do so may lead to poor results; Obstacles include patient positioning, body habitus, and implant application tools. We present the “Winquist View,” an oblique fluoroscopic projection that shows the femoral neck in profile, aligns the implant and cephalic component, and assists in implant placement.
Methods
With the patient in the lateral position, the legs are scissored when possible. Following standard reduction techniques, the Winquist view is used to check reduction prior to surgical draping. Intraoperatively, we rely on a perfect image to place implants in the ideal portion of the femoral neck, with a trajectory that achieves the center-center or center-low position of the femoral neck. This is achieved by incorporating the anterior-posterior, lateral, and Winquist view.
Results
We present 3 patients who underwent fixation with a cephalomedullary nail for intertrochanteric hip fractures. The Winquist view facilitated excellent visualization and positioning in all cases. All postoperative courses were uneventful, without failures or complications.
Conclusion
While standard intraoperative imaging may be adequate in many cases, the Winquist view facilitates optimal implant positioning and fracture reduction. With lateral imaging, implant insertion guides may obscure visualization of the femoral neck during which Winquist view is the most helpful.
Level of Evidence: V
Keywords: femoral neck, intraoperative imaging, patient positioning, hip fracture, intertrochanteric fracture
Introduction
Cephalomedullary fixation of intertrochanteric hip fractures (OTA 31-A) is favored by most orthopedic surgeons. The American Academy of Orthopedic Surgeons recently revised its clinical practice guidelines to give a strong recommendation for the use of cephalomedullary nails for the fixation of unstable intertrochanteric hip fractures.
Despite the increased use of cephalomedullary fixation, failure with screw cut out and varus collapse remains a concerning mode of failure. Factors that are documented to increase the risk of cut-out include fracture reduction, screw penetration, and excessive tip-apex distance (TAD). This points to the need for precise screw placement in the femoral head, a technical step that is dependent on fluoroscopic imaging.
Clear visualization of the femoral neck with intraoperative fluoroscopy is vital in the treatment of proximal femur and femoral neck fractures. Various implants in these situations include intramedullary nails with cephalomedullary fixation, hip screws, and other fixed angle devices such as blade plates or dynamic condylar screws. Failure to appropriately position implants in the femoral head and neck have led to early failures1-3 and can lead to less favorable outcomes after revision surgery.2
At our institution, we prefer positioning patients in the lateral decubitus position for intramedullary nailing. In comparison to the supine position, it facilitates easier access to the surgical starting point (whether piriformis or trochanteric) and avoids posterior angulation of proximal femoral fractures which commonly occurs during supine positioning.
To assist in viewing the head and neck segment of the proximal femur, we use an oblique fluoroscopic projection we call the “Winquist view” based upon Dr. Winquist’s instruction (Figure 1A). This view is obtained by rotating /tilting the image intensifier to display a lateral view of the femoral neck and head in a collinear manner (Figure 1B and 1C).
Figure 1A.

Winquist View.
Figure 1B to 1C.

(1B) Schematic representing lateral patient positioning and appropriate intraoperative fluoroscopy position taking into account an average femoral anteversion of 10 degrees. Obtaining this angle in addition to the neck-shaft angle comprises the Winquist view. (1C) Schematic representing lateral patient positioning and appropriate intraoperative fluoroscopy position taking into account an average neck-shaft angle of 130 degrees. Obtaining this angle in addition to the anteversion angle comprises the Winquist view.
Methods
With the patient in the lateral position, we prefer to scissor the legs when possible (Figure 2A-C). Standard reduction techniques are employed during this step. These include traction, hip flexion, and limb rotation. At this point, we routinely check reduction prior to surgical draping and first use the Winquist view. Occasionally, we will have to modify patient positioning to obtain better imaging at this step. Once we confirm that adequate imaging can be obtained, we proceed with the case as usual with the implant of choice.
Figure 2A to 2C.

(2A) Intraoperative set up. (2B) Proper positioning of intraoperative fluoroscopy with the patient in the lateral position – our preferred patient position for complex proximal femur fractures of the intertrochanteric and subtrochanteric varieties. Note the C-arm position taking the femoral anteversion and neck-shaft angle into consideration. (2C) Intraoperative example utilizing the Winquist view.
Intraoperatively, we rely on a perfect image to place implants in the ideal portion of the femoral neck and with a trajectory that achieves the center-center position of the femoral head. This goal is accomplished by incorporating data from all intraoperative views including the anterior-posterior (AP) view, the lateral view, and the Winquist view. Often, particularly with standard lateral imaging, the implant insertion guides obscures adequate visualization of the femoral neck. It is in this situation that the Winquist view is the most helpful.
Case Report
Case 1: A 61-year-old female fell at home after tripping over a lamp cord. She sustained a left intertrochanteric hip fracture (see Figures 4A-B). After appropriate medical evaluation, she underwent closed reduction and internal fixation with a cephalomedullary nail. The surgical procedure and post-operative course had no complications and were uneventful (Figures 3, 4C-E).
Figure 4A to 4E.

(4A, 4B) Injury films including an AP and Lateral view of Case 1’s left intertrochanteric hip fracture. (4C) Post-operative lateral image of Case 1. (4D) Post-operative Winquist view of Case 1. (4E) Post-operative AP image of Case 1.
Figure 3.

Intraoperative image of the Winquist view with patient in Figure 2A and 2B.
Case 2: A 66-year-old female fell down the stairs at her home after tripping. She sustained a left reverse oblique intertrochanteric hip fracture (Figures 5A-B). After correction of an elevated INR, she was brought to the operating room and underwent an open reduction and internal fixation with a cephalomedullary nail. The patient’s intraoperative and post-operative courses had no complications and were uneventful (Figures 5C-E)
Figure 5A to 5E.
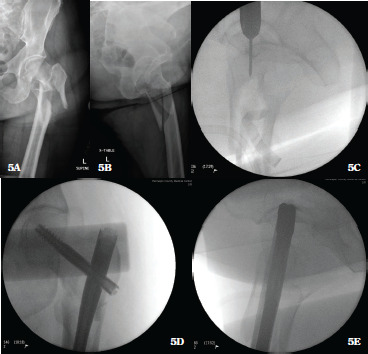
(5A) Preoperative AP image of Case 2’s left intertrochanteric fracture. (5B) Preoperative lateral image of Case 2’s left intertrochanteric fracture. (5C) Intraoperative example of utilizing the Winquist view to obtain perfect positioning of a guide pin into the femoral neck. (5D) Final intraoperative AP image of Case 2. (5E) Intraoperative lateral image of Case 2 demonstrating optimal position of guide.
Case 3: A 75-year-old male was chipping ice off his roof and fell 10 feet to the ground. He sustained a left intertrochanteric hip fracture (Figures 6A-B). After undergoing medical evaluation and normalization of his INR, he underwent an open reduction and internal fixation with a cephalomedullary nail. His intraoperative and post-operative courses were uneventful (Figures 6C-E).
Figure 6A to 6F.

(6A) Preoperative AP image of Case 3’s intertrochanteric fracture. (6B) Preoperative lateral image of Case 3’s intertrochanteric fracture. (6C) Intraoperative image utilizing the Winquist view to see the fracture reduction adequately as well as guidewire placement across the femoral neck. Rotation of the C-arm in the Winquist view both anterior and posterior confirms appropriate cephalic screw position. (6D) Post-operative Winquist view of Case 3 with implant across femoral neck. (6E) Post-operative AP view of Case 3 with implant across femoral neck. (6F) Post-operative lateral view of Case 3 with implant across femoral neck.
Discussion
The importance of utilizing TAD to establish optimal screw positioning was first presented by Baumgartner et al. The authors concluded that screw cut out could be avoided in patients with a sliding hip screw, if the surgeon maintains a TAD of less than 25 mm.4 Since this landmark paper, the importance of avoiding an excessive TAD and maintaining a center-center position has been extrapolated to the nails and lag screws positions to avoid implant failure.5
Complete visualization of the femoral neck is critical to ensure appropriate placement of implants through the femoral neck and into the femoral head. Failure to place implants in the correct position or failure to achieve adequate fracture reduction has led to fixation construct failures and poor patient outcomes.1,2,6-10 Hoffer et al. in a retrospective series of 76 cases reported appropriate lag screw placement in only 55% of cases-included in their series were 5 lag screws in “at risk” positions including superior on AP view (3 patients) and anterior on lateral view (2 patients).11 While standard AP and lateral intraoperative imaging may be adequate in the many surgical cases, we feel that the application of the Winquist view can aid in implant positioning and fracture reduction. This may be particularly important in academic medical centers or for surgeons with less experience.11
The purpose of the present report is to introduce orthopedic surgeons to the Winquist view, providing another method for better visualization of the femoral neck to use in the treatment of fractures involving the placement of implants in this region.
Conclusion
Proper positioning of implants into the femoral neck and head has been shown to directly influence the stability of fracture fixation. The Winquist view can be performed to facilitate optimal visualization of the femoral neck to use in the treatment of fractures. This may be particularly important in academic medical centers or for surgeons with less experience. The routine utilization of this view adds another tool for the surgeon to use to optimize outcomes in the care of these patients.
References
- 1.Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79:969–971. doi: 10.1302/0301-620x.79b6.7949. [DOI] [PubMed] [Google Scholar]
- 2.Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001;83:643–650. doi: 10.2106/00004623-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Alho A, Benterud JG, Solovieva S. Internally fixed femoral neck fractures. Early prediction of failure in 203 elderly patients with displaced fractures. Acta Orthop Scand. 1999;70:141–144. doi: 10.3109/17453679909011252. [DOI] [PubMed] [Google Scholar]
- 4.Baumgaertner MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Shannon SF, Yuan BJ, Cross WW, 3rd, et al. Short Versus Long Cephalomedullary Nails for Pertrochanteric Hip Fractures: A Randomized Prospective Study. J Orthop Trauma. 2019;33:480–486. doi: 10.1097/BOT.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 6.Reikerås O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54:18–23. doi: 10.3109/17453678308992864. [DOI] [PubMed] [Google Scholar]
- 7.Reikerås O, Høiseth A. Femoral Neck Angles in Osteoarthritis of the Hip. Acta Orthopaedica Scandinavica. 1982;53:781–784. doi: 10.3109/17453678208992292. [DOI] [PubMed] [Google Scholar]
- 8.Heinz T, Vécsei V. [Complications and errors in use of the gamma nail. Causes and prevention]. Chirurg. 1994;65:943–952. [PubMed] [Google Scholar]
- 9.Haidukewych GJ, Berry DJ. Salvage of failed treatment of hip fractures. J Am Acad Orthop Surg. 2005;13:101–109. doi: 10.5435/00124635-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt AH, Asnis SE, Haidukewych G i., et al. Femoral neck fractures. Instr Course Lect. 2005;54:417–445. [PubMed] [Google Scholar]
- 11.Hofer M, Chevalley F, Garofalo R, et al. Use of trochanteric nail for proximal femoral extracapsular fractures. Orthopedics. 2006;29:1109–1114. doi: 10.3928/01477447-20061201-18. [DOI] [PubMed] [Google Scholar]


