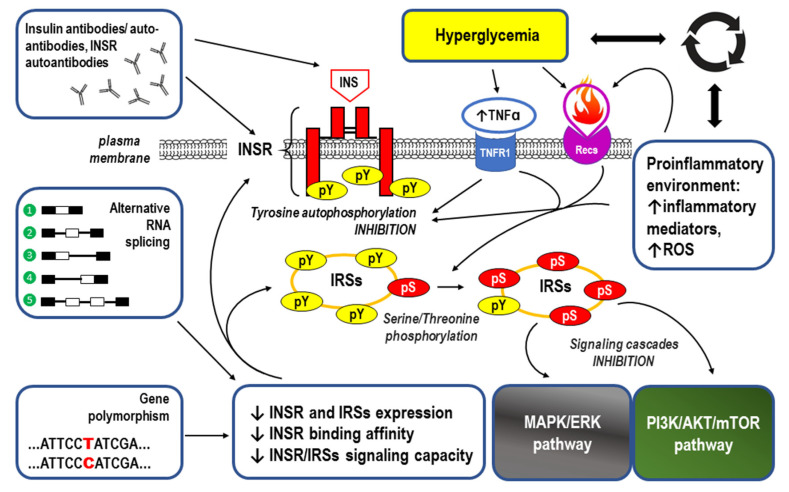
Figure 5.
The main underlying causes/mechanisms of insulin resistance (IR) (successive boxes going counter-clockwise from the top-left): Antibodies including autoantibodies antibodies can be produced against both insulin (INS) and the insulin receptor (INSR). Type B IR syndrome is a rare disorder caused by autoantibodies to the insulin receptor [125,134]. Alternative RNA splicing events including ❶—exon retention, ❷—exon skipping, ❸—alternative 5′ donor sites, ❹—alternative 3′ acceptor sites, and ❺—mutually exclusive exons can lead to a splicing mutation that may occur in both introns and exons and disrupt existing splice sites, create new ones, or activate the cryptic ones [135]. Type A IR is caused by a mutation in the INSR gene [136,137]. Defects in the INSR structure and function may be caused by the common type 2 diabetes (T2D) Gly971Arg polymorphism that is responsible for altered tyrosine phosphorylation at a specific site in insulin receptor substrate 1 (IRS-1) [138]. Both alternative RNA splicing and gene polymorphism may significantly affect INSR/IRSs downstream signaling, producing IR-dependent inhibition of the MAPK/ERK and PI3K/AKT/mTOR pathways [122,123,129,139]. A proinflammatory environment and hyperglycemia create a vicious cycle of the complex cause-and-effect relationship, causing IR through inhibition of the tyrosine autophosphorylation (pY) within the INSR and serine/threonine phosphorylation (pS) of the insulin receptor substrates (IRSs). Reactive oxygen species (ROS) and signaling via membrane-bound receptors for tumor necrosis factor receptor 1 (TNFR1) and the receptors for other proinflammatory cytokines (Recs) play crucial roles [122,123,126,140].