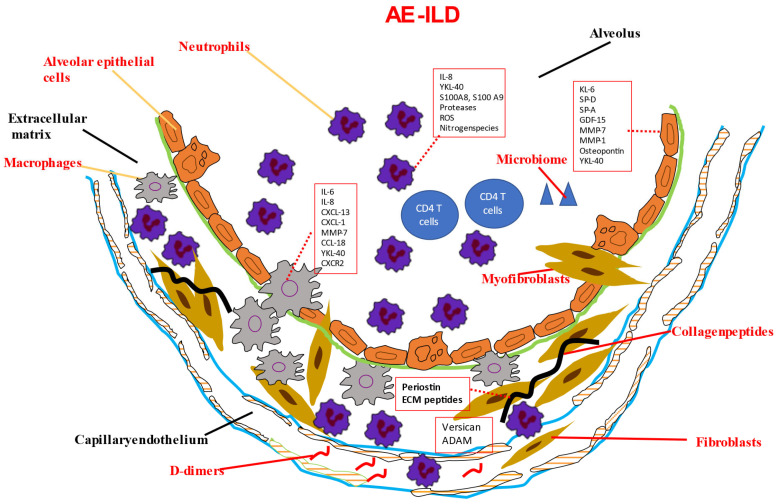
Figure 1.
Potential biomarkers in AE-ILD and their cellular source. Due to various stimuli (infections, microaspiration, air pollution, stress, intrinsic acceleration of the underlying fibrosis), injured alveolar epithelial cells and disrupted epithelial barrier lead to the secretion of KL-6, SP-A, and SP-D. Increased KL-6 promotes fibroblast activation through TGF-b signaling. SP-D further aggregates ECM deposition. Matrix metalloproteinase-mediated degradation of collagen leads to the release of versican and ADAM. Periostin is also a marker of increased matrix turnover. During AE-ILDs, lung inflammation is driven by upregulation of macrophage activation pathways. IL-8 and CXCL1 mainly contribute to the neutrophil influx. Neutrophils release numerous proteases and produce reactive oxygen species. Vascular and endothelial damage contributes to the influx of neutrophils.