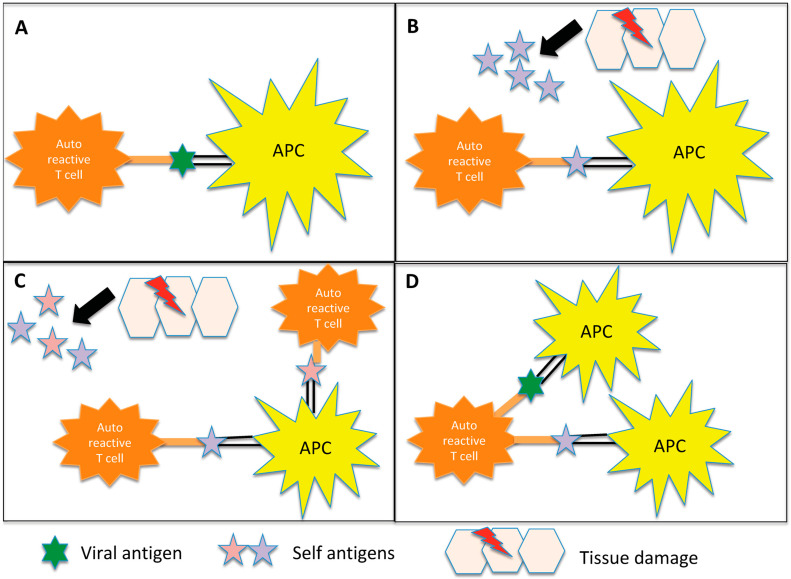
Figure 1.
Representation of the potential inflammation-mediated mechanisms underlying autoimmunity triggered by infections. (A) Molecular mimicry: In certain instances, the antigens found on pathogens may bear a resemblance to self-antigens present in the body. This similarity can result in the activation of autoreactive T cells, which erroneously identify self-antigens as foreign. Notably, in demyelinating diseases, antigen-presenting cells (APCs) present myelin components to autoreactive CD4+ T cells, initiating the cascade of autoimmune responses. (B) Bystander activation: The virus induces a profound inflammatory response, resulting in significant damage to the surrounding tissue. Consequently, additional autoantigens become exposed and antigen-presenting cells (APCs) present these autoantigens to autoreactive CD4+ T cells. (C) Epitope spreading: Initially, the immune response may target a specific antigen derived from the infecting pathogen. However, as time progresses, the immune response can expand to encompass other self-antigens that share structural similarities or associations with the initial target antigen. In demyelinating diseases, for instance, viral infections can lead to the destruction of oligodendrocytes. Subsequent fragmentation of myelin in the inflammatory milieu exposes additional antigens, contributing to a self-perpetuating cycle of myelin destruction. (D) Dual T cell receptor: Certain T lymphocytes possess the capability to express multiple T cell receptors, allowing them to recognize both viral and myelin antigens. Consequently, these dual-specificity T cells can activate responses against both types of antigens simultaneously.