Abstract
Introduction and importance
Duodenal duplication cysts are a rare subtype of alimentary tract duplications cysts, consisting of 7 % of all the duplications. The clinical presentation is variable, depending on the size, location and mass effect. Most duodenal duplication cysts abut the second or third portion of the native duodenum. The standard treatment of choice for symptomatic enteric duplication cysts is complete surgical removal. In our case, by examining the abdomen, ectopic pancreatic tissue was found on the wall of the transverse colon, along with Meckel's diverticulum, 50 cm from the ileocecal junction.
Case presentation
We present a newborn case presented to the hospital with a history of abdominal mass with jaundice. Abdominal ultrasonography and CT scan show the presence of a cystic mass without specifying its exact source. By opening the abdomen, it was found at the expense of the duodenum, and it was excised and On histopathological analysis, a duodenal duplication cyst was diagnosed. The literature was reviewed and the approach to duodenal duplication cyst in neonates is discussed.
Clinical discussion
Duodenal duplication cysts are rare, even so should be taken into consideration when a mass is found. A thorough imaging investigation is crucial in establishing the diagnosis along with histopathology.
Conclusion
When diagnosing a Duodenal duplication cysts, the cyst must be completely removed because potential risk of malignant transformation.
Keywords: Case report, Duodenal duplication cyst, Pediatric surgery, Neonate
Highlights
-
•
Duodenal duplication cysts are rare and often asymptomatic.
-
•
These cysts are located on the same side as the mesentery and which can occur anywhere from the digestive tract.
-
•
The basic treatment is the complete excision of the cyst down to the common wall with the removal of the remaining mucous.
-
•
We must always keep in mind that these are cysts have potential risk of malignant transformation.
1. Introduction
Duplications of the digestive tract are rare spherical or tubular structures that may occur anywhere in the tract from the mouth to the anus [1]. Ladd introduced the term “duplication of the digestive tract” in the hope of clarifying nomenclature that previously included descriptive terms such as enteric or enterogenic cysts, giant diverticula, ileal, jejunal, or colonic duplication, and an unusual Meckel's diverticulum.
Gastrointestinal duplications are rare congenital anomalies, of which duodenal duplication cyst is an even rarer subtype, accounting for 7 % of all duplications [2].
A duplication cyst is characterised by being located in or immediately adjacent to the wall of the GI tract, being on the mesenteric side, sharing a common blood supply, and having a muscular wall with mucosa of any type, including ectopic gastric, pancreatic, or respiratory tissue [3]. There are several theories to explain GI duplications, e.g. For example, the theory of abortive twins, the theory of persistent embryologic diverticula, and the theory of aberrant luminal recanalization [4]. Intestinal duplication most commonly occurs in infancy or early childhood and can occur from infancy to 52 years of age. They may be asymptomatic, as in infants, or more commonly present as vague abdominal pain, nausea and vomiting, or a palpable abdominal mass.
In rare cases, they may remain asymptomatic until adulthood, and in 38 % of patients, the diagnosis is not made until after 20 years of age [5]. Duodenal duplication cysts are usually benign lesions; however, three cases have been reported in which malignant tumours have formed inside [[6], [7]].
The literature has been reviewed, and the approach to duodenal duplication cysts in neonates is discussed.
This case is described in accordance with the criteria of SCARE [19].
2. Presentation of case
2.1. Patient information
We describe the case of a male child who was born by cesarean section after a gestation period of 38 weeks, without any problems during the observation of pregnancy or during delivery. After birth, the child had a good Apgar index and a birth weight of 3.6 kg. The infant's postpartum history began with vomiting of food after each milk feeding and progressed to an episode of biliary vomiting with accompanying jaundice without fever or diarrhea with good urination on the third day. The mother stated that there was no family history of congenital anomalies, no infections during pregnancy, and no medications.
On the sixth day after birth, a swollen epigastrium was noted, after which the parents visited the hospital.
3. Clinical findings
3.1. Clinical examination
On the child's arrival at the hospital, a clinical examination was performed because the child had a good general condition without cyanosis or pallor, with mild dehydration and no increase in fever. On examination, jaundice was noted, and the child had no physical abnormalities; his heart rate was 120 beats per minute. On abdominal examination, the abdomen was soft with a palpable mass in the epigastrium and right hypochondrium that was mobile on examination, with no adhesion to the anterior abdominal wall or evidence of dermatitis. The rest of the body systems were normal.
4. Diagnostic assessment
Laboratory examinations revealed a hemoglobin of 11.8 g/dL, total white blood cell count of 9000/mm3, platelet count of 763,000/mm3, total bilirubin15.
Abdominal ultrasonography revealed a 4.5 × 3.8 cm cyst in the epigastric region that was not fused to the liver or kidney and extended to the umbilical region, the origin of which could not be determined.
A computed tomography scan (CT) of the abdomen revealed a cystic mass with opaque contents approximately 5 × 5 cm in diameter between the liver and the right kidney, with the posterior border approaching the right kidney (Fig. 1A–B). It could be a duplication cyst or a mesenteric cyst.
Fig. 1.
A: CT/cross coronal view of the Abdominal showing A cyst of 5 ∗ 5 cm in size with liquid content appears without adhesion to the liver or gallbladder and is located near the stomach.
B: CT/cross axial view, showing A cyst without adhesion to the liver and reaches the right kidney without adhesion with it.
5. Therapeutic intervention
Based on the present clinical picture, open surgery was indicated. The procedure was performed at our tertiary college teaching hospital. It was performed by a pediatric surgery specialist with 32 years of pediatric surgical experience. In addition to being a pediatric surgery specialist with 10 years of pediatric surgery experience.
the patient was taken for an exploratory laparotomy under general anesthesia. Upon reaching the peritoneal cavity, an approximately 6 cm × 7 cm × 6 cm spherical cystic mass was noted attached to the pylorus of the stomach to the third part of the duodenum over the mesenteric border (Fig.2-A).
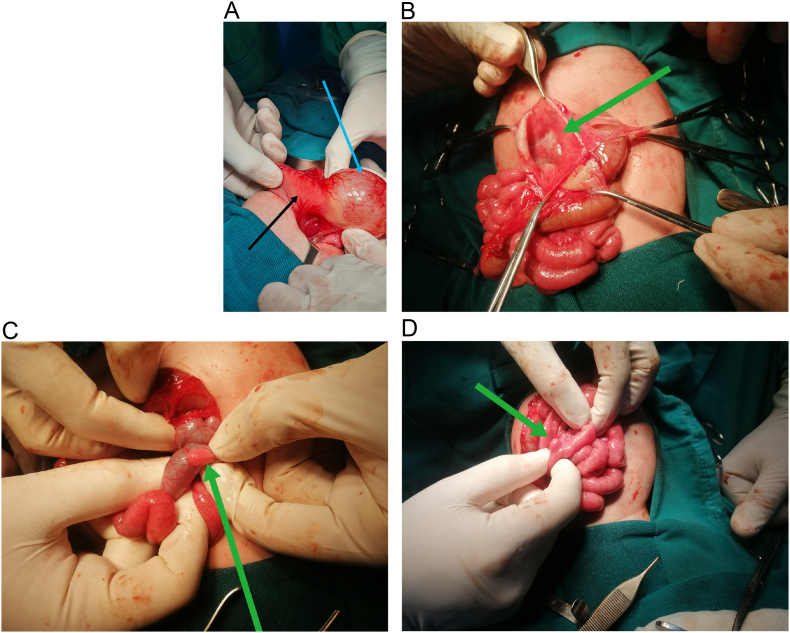
Fig. 2.
A: Intraoperative image prior to excision, showing the cyst, with the blue arrow indicating the cyst and the green arrow indicating the duodenum.
B:: Intraoperative image, showing the cyst after it has opened and the cavity within it has been viewed.
C: An intraoperative image showing ectopic pancreatic tissue on the wall of the transverse colon.
D: An intraoperative image showing Meckel's diverticulum.
The entire 1st and 2nd parts of the duodenum were not seen separately from the mass. The cyst was dissected out of the mesenteric layer. About 150 ml of seromucous fluid was drained. The cyst was opened wide to check whether there was a connection to the pylorus or duodenum (Fig. 2-B), and luminal continuation was cross-checked by insufflation of 50 ml air via the NGT. The cyst wall was removed up to 0.5 cm from the common wall and sent for histopathologic examination. The remnants of the cyst mucosa were electrocauterized. Inspection of the entire abdominal cavity revealed that there was ectopic pancreatic tissue on the wall of the transverse colon (Fig. 2-C), in addition to Meckel's diverticulum, at a distance of approximately 50 cm from the ileocecal junction (Fig. 2-D).
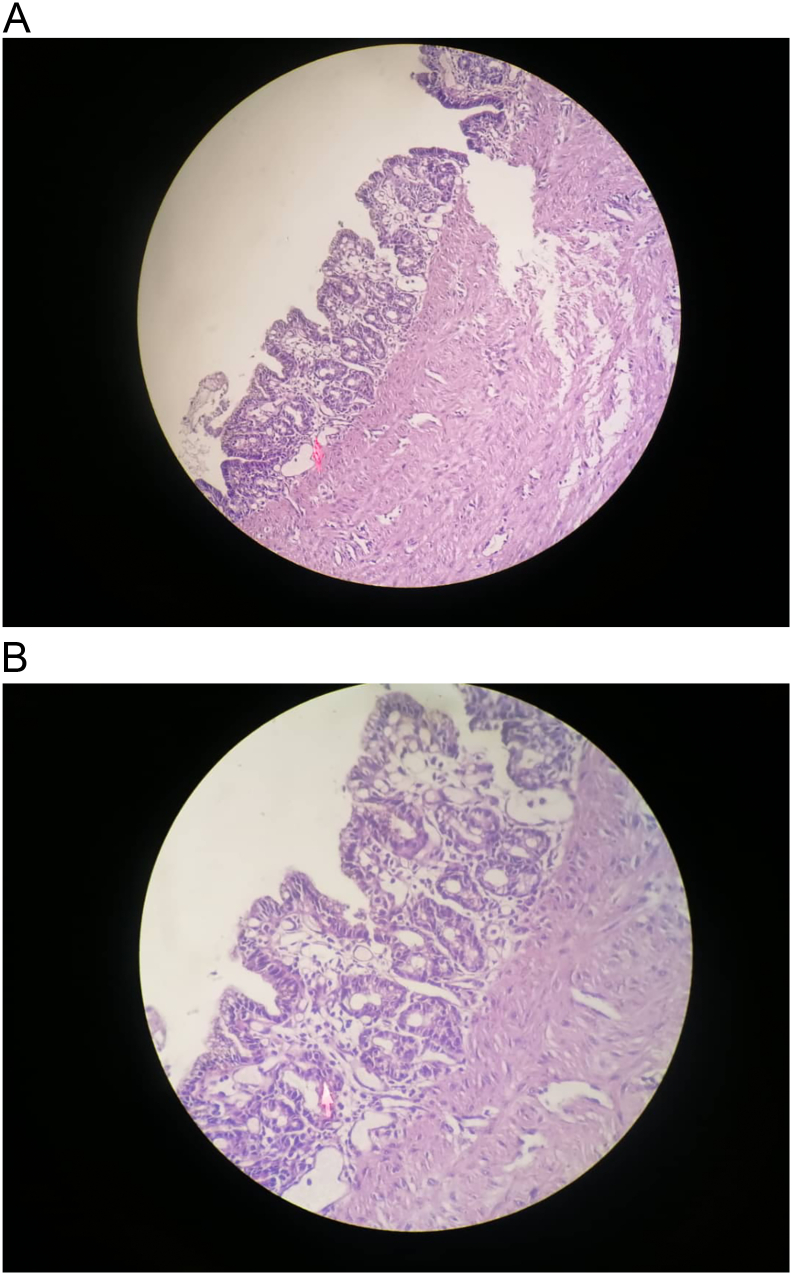
Histopathologic examination shows muscle layers in the cyst wall and epithelial cells of the lining in the lower view (Fig. 3A).
Fig. 3.
A: Histopathological analysis of the resected mass, Low-light view of the muscular layers in the cyst wall and the lining epithelial cells.
B: Histopathological analysis of the resected mass, High-resolution view of the mucosa of the duplication cyst (atrophic duodenal mucosa consisting of villi and crypts with Brunner glands).
High-resolution view of the mucosa of the duplication cyst (atrophic duodenal mucosa consisting of villi and crypts with Brunner glands) (Fig. 3B).
On the third day after surgery, the child was started on oral nutrition and was discharged from the hospital after one week in good general condition and with good oral intake.
6. Discussion
Abdominal masses in infants have different manifestations, with 65 % of them occurring in the flanks (55 % of which are of renal origin), 20 % intraperitoneal, and 15 % in the pelvis [8]. The intraperitoneal masses may be of gastrointestinal (GI) (15 %) or hepatobiliary (5%) origin. GI The masses are usually mesenteric cysts, enteric duplication cysts, omental cysts, and meconium cysts or meconium ileus [9].
The clinical presentation varies depending on the size, location, and effect of the mass. In neonates, the cyst often presents as an asymptomatic abdominal mass with physical signs of abdominal distension or a palpable abdominal mass.
Small bowel duplication cysts are the most common. GI tract duplication cysts are the most common cysts of the GI tract and may be associated with all three segments: Duodenum, Ileum (44 %), and Jejunum [10]. Most duodenal duplication cysts are adjacent to the second or third segment of the native duodenum and share common smooth muscle layers [18]. They may be lined with duodenal mucosa, ectopic gastric mucosa, and pancreatic or respiratory epithelium [11]. Grossly, most duodenal duplications are cystic and usually communicate with the pancreatic or biliary ducts. In contrast, some tubular duodenal duplications may communicate with the natural duodenal lumen [11].
Many theories have been proposed to explain these conditions, including the abortive twin theory, the split notochord theory, and the intrauterine vascular event theory; however, the most widely accepted explanation is that they are the result of entrapment of a diverticulum during embryogenesis [12].
Several congenital anomalies may occur in association with duplications, most commonly duplications of the thoracic, midgut, and hindgut regions. Spinal anomalies such as bifid or hemivertebrae vertebrae or vertebral fusions may also occur; they are most commonly associated with thoracic and hindgut duplications. Other congenital malformations recorded include congenital heart disease, esophageal atresia, congenital diaphragmatic hernia, congenital lung malformations, and myelomeningocele with foregut duplications; intestinal malrotation or (less commonly) intestinal atresia with midgut duplications; and genitourinary duplications, bladder exstrophy, and anus imperforate with hindgut duplications [13].
To diagnose such cysts, a US examination is usually performed first, followed by a CT examination to examine related structures and to describe the anatomy of the cyst. Depending on the clinical presentation, further investigations may be required. If hemorrhage is present, a technetium-99 m-pertechnetate radionuclide examination may be ordered to identify heterotopic gastric mucosa. For a duodenal cyst with suspected bile duct communication. Magnetic resonance cholangiography or, in older children, endoscopic retrograde cholangiopancreatography (ERCP) is useful [[13], [14]].
The standard treatment of choice for symptomatic enteric duplication cysts is complete surgical removal [17].
Although the treatment of asymptomatic cases is controversial, surgical excision is often advocated due to the risk of serious complications and the potential risk of malignant transformation [16].
and can be performed for simple cysts, but sometimes it is advisable to perform marsupialization or partial excision with mucosectomy in complex conditions such as a cyst on the medial side of the 2nd or 3rd part of the duodenum with possible bile duct or luminal communication or in the presence of a shared muscle wall [[13], [14], [15]]. Preoperatively, we found that the cyst was closely associated with the pylorus, 1st, 2nd, and 3rd parts of the duodenum, so we performed marsupialization and excision of the cyst up to 0. 5 cm of the common wall and cauterized the remaining mucosa to prevent future complications such as recurrence, bleeding, or infection.
If there is doubt about a cystobiliary connection, the cyst can be aspirated, and if aspiration yields bile, a tabletop cholangiogram or cholecystectomy can be performed, followed by insertion of a fine probe or catheter distally to look for a connection [13].
Nowadays, there are also increasing minimally invasive treatment options, which include endoscopic marsupialization of the duodenal duplication cyst.
7. Conclusion
It is necessary to consider duodenal duplication cyst as a differential diagnosis when detecting an abdominal mass with gastric outlet obstruction and the presence of vomiting. The diagnosis is confirmed by performing an ultrasound of the abdomen by an expert or by performing a CT scan of the abdomen. The rule is complete surgical removal of the cyst by open surgery, with some surgeons performing the endoscopic approach to removal, which is difficult to perform. Duodenal cysts are considered one of the rare types of GI tract duplication and may sometimes cause jaundice due to biliary obstruction, pancreatitis or gastrointestinal bleeding. The basic diagnostic tools are ultrasound of the abdomen, CT scan, magnetic resonance imaging (MRI) may be used in some cases, and Ercp. Surgical treatment methods vary according to the location of the cyst and the ability to perform a complete cyst excision.
Abbreviations
Ethical approval
Ethical approval for this study (Ethical Committee N° NAC 207) was provided by the Ethical Committee NAC of Pediatric University Hospitals, Damascus, SYRIA on 4 May 2023.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
KA, HM: Who wrote, originally drafted, edited, visualized, validated, literature reviewed the manuscript.
MAA: pediatric surgery specialist, who performed and supervised the operation.
HA: Professor of pediatric surgery, head of pediatrics surgery department in university pediatrics hospital, supervision, and review of the manuscript
SQ: A pathologist participated in preparing and reviewing the manuscript.
NE: Professor in neonatology, Head of NICU in Children Hospital.
KA: Conceptualization, resources, and the corresponding author who submitted the paper for publication.
All authors read and approved the final manuscript.
Guarantor
Khaled Alomar
Research registration
N/A
Consent of patient
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available because the Data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Conflict of interest statement
The authors declare that they have no competing interests.
References
- 1.Stern L.E., Warner B.W. Gastrointestinal duplications. Semin. Pediatr. Surg. 2000;9:135–140. doi: 10.1053/spsu.2000.7565. [DOI] [PubMed] [Google Scholar]
- 2.Mba M.I.G.H.W., Md P.M.J., Peter S.S.D., MD . 7th ed. Elsevier; 2019. Ashcraft’s Pediatric Surgery: Expert Consult-Online+Print. [E-book] [Google Scholar]
- 3.Macpherson R.I. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063–1080. doi: 10.1148/radiographics.13.5.8210590. [DOI] [PubMed] [Google Scholar]
- 4.Edwards H. Congenital diverticula of the intestine: with report of a case exhibiting heterotopia. Br. J. Surg. 1929;17:7–21. [Google Scholar]
- 5.Chen J.J., Lee H.C., Yeung C.Y., Chan W.T., Jiang C.B., Sheu J.C. Metaanalysis: the clinical features of the duodenal duplication cyst. J. Pediatr. Surg. 2010;45:1598–1606. doi: 10.1016/j.jpedsurg.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 6.Falk G.L., Young C.J., Parer J. Adenocarcinoma arising in a duodenal duplication cyst: a case report. Aust. N. Z. J. Surg. 1991;61:551–553. doi: 10.1111/j.1445-2197.1991.tb00289.x. [DOI] [PubMed] [Google Scholar]
- 7.Inoue M., Nishimura O., Andachi H., Koga S. Early cancer of duodenal duplication. a case report. Gastroenterol. Jpn. 1979;14:233–237. doi: 10.1007/BF02774072. [DOI] [PubMed] [Google Scholar]
- 8.Standardized Toolbox of Education for Pediatric Surgery Abdominal Masses of Childhood. American Pediatric Surgical Association Committee of Education, 2012-13.
- 9.Tiwari C., Shah H., Waghmare M., Makhija D., Khedkar K. Cysts of gastrointestinal origin in children: varied presentation. Pediatr. Gastroenterol. Hepatol. Nutr. 2017;20:94–99. doi: 10.5223/pghn.2017.20.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamvakopoulos G.S., Sams V., Preston P., Stebbings W.S.L. Irondeficiency anaemia caused by an enterolith-filled jejunal duplication cyst. Ann. R. Coll. Surg. Engl. 2004 Nov;86(6):W49–W51. doi: 10.1308/147870804119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khanna P.C., Gawand V., Nawale A.J., et al. Complete large bowel duplication with paraduodenal cyst: prenatal sonographic features. Prenat. Diagn. 2004;24:312–314. doi: 10.1002/pd.864. [DOI] [PubMed] [Google Scholar]
- 12.Mourra N., Chafai N., Bessoud B., Reveri V., Werbrouck A., Tiret E. Colorectal duplication in adults: report of seven cases and review of the literature. J. Clin. Pathol. 2010 Dec;63(12):1080–1083. doi: 10.1136/jcp.2010.083238. [DOI] [PubMed] [Google Scholar]
- 13.Puri P., Höllwarth M.E. Springer Publishing; 2019. Pediatric Surgery. [Google Scholar]
- 14.Dipasquale V., Barraco P., Faraci S., Balassone V., De Angelis P., Di Matteo F.M., et al. Duodenal duplication cysts in children: clinical features and current treatment choices. Biomed. Hub. 2020;5:152–164. doi: 10.1159/000508489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salazar E., Sin E.I., Low Y., Khor C.J.L. Insulated-tip knife: an alternative method of marsupializing a symptomatic duodenal duplication cyst in a 3-year-old child. VideoGIE. 2018;3:356–357. doi: 10.1016/j.vgie.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hata H., Hiraoka N., Ojima H., Shimada K., Kosuge T., Shimoda T. Carcinoid tumor arising in a duplication cyst of the duodenum. Pathol. Int. 2006;56(5):272–278. doi: 10.1111/j.1440-1827.2006.01957.x. [DOI] [PubMed] [Google Scholar]
- 17.Chen J.-J., Lee H.-C., Yeung C.-Y., Chan W.-T., Jiang C.-B., Sheu J.-C. Meta-analysis: the clinical features of the duodenal duplication cyst. J. Pediatr. Surg. 2010 Aug;45(8):1598–1606. doi: 10.1016/j.jpedsurg.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Guarise A., Faccioli N., Ferrari M., et al. Duodenal duplication cyst causing severe pancreatitis: imaging findings and pathological correlation. World J. Gastroenterol. 2006;12:1630–1633. doi: 10.3748/wjg.v12.i10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available because the Data were obtained from the hospital computer-based in-house system. Data are available from the corresponding author upon reasonable request.