Abstract
Objectives
The number of susceptibility loci currently associated with vasculitis is lower than in other immune-mediated diseases due in part to small cohort sizes, a consequence of the low prevalence of vasculitides. This study aimed to identify new genetic risk loci for the main systemic vasculitides through a comprehensive analysis of their genetic overlap.
Methods
Genome-wide data from 8467 patients with any of the main forms of vasculitis and 29 795 healthy controls were meta-analysed using ASSET. Pleiotropic variants were functionally annotated and linked to their target genes. Prioritised genes were queried in DrugBank to identify potentially repositionable drugs for the treatment of vasculitis.
Results
Sixteen variants were independently associated with two or more vasculitides, 15 of them representing new shared risk loci. Two of these pleiotropic signals, located close to CTLA4 and CPLX1, emerged as novel genetic risk loci in vasculitis. Most of these polymorphisms appeared to affect vasculitis by regulating gene expression. In this regard, for some of these common signals, potential causal genes were prioritised based on functional annotation, including CTLA4, RNF145, IL12B, IL5, IRF1, IFNGR1, PTK2B, TRIM35, EGR2 and ETS2, each of which has key roles in inflammation. In addition, drug repositioning analysis showed that several drugs, including abatacept and ustekinumab, could be potentially repurposed in the management of the analysed vasculitides.
Conclusions
We identified new shared risk loci with functional impact in vasculitis and pinpointed potential causal genes, some of which could represent promising targets for the treatment of vasculitis.
Keywords: Systemic vasculitis; Polymorphism, Genetic; Autoimmunity
WHAT IS ALREADY KNOWN ON THIS TOPIC
The genetic component of systemic vasculitides is still largely unknown, mainly due to the low prevalence of these disorders.
Combination of genome-wide data from different traits, through cross-phenotype association studies, is a powerful tool to identify new genetic risk loci shared across related diseases.
WHAT THIS STUDY ADDS
Meta-analysis of large-scale summary statistics of the main forms of vasculitis allowed identification of 16 risk loci with a pleiotropic role in these disorders.
Functional annotation of the identified cross-phenotype associations led to the prioritisation of causal genes with a potential effect in vasculitis.
Many of the pleiotropic variants affect genes encoding proteins that are therapeutic targets of drugs indicated for other pathologies; these could potentially be repurposed for the treatment of the analysed vasculitides.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
A better understanding of the key molecular pathways shared across different forms of systemic vasculitis may help to identify common therapeutic mechanisms that lead to improved clinical management of these disorders.
Introduction
Systemic vasculitides comprise a heterogeneous group of immune-mediated disorders characterised by blood vessel inflammation. According to the Chapel Hill Consensus Conference, the most common vasculitides can be classified into three main categories based on the distribution of the predominant type of vessel involvement.1 Large-vessel vasculitis, including giant cell arteritis (GCA) and Takayasu’s arteritis (TAK), is characterised by the inflammation of the aorta and its main branches; medium vessel vasculitis, which comprises Kawasaki disease (KD) and polyarteritis nodosa, mainly affects the major visceral arteries and their branches; and, finally, small vessel vasculitis, which affects arterioles, small arteries, capillaries and venules, can be subdivided into ANCA-associated vasculitis (AAV) that includes eosinophilic granulomatosis with polyangiitis (EGPA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA), and immune complex vasculitis, including IgA vasculitis (IgAV). In addition, other vasculitides such as Behçet’s disease (BD) involve vessels of any size. Since inflammation can affect vessels of various sizes and locations, these diseases show a wide spectrum of clinical manifestations, many of which are shared among them.2–4
The aetiology of the vasculitides is still unclear; however, it is well known that they are complex disorders caused by the interaction between multiple genetic and environmental factors. Although several large-scale genetic scans have been performed in vasculitis,5 only a few loci have been consistently associated with these disorders, including the human leucocyte antigen (HLA) region, which represents the main genetic risk locus for all of them.5 This limited knowledge of their genetic component, as compared with other immune-mediated disorders, is likely due to the low prevalence of vasculitides, which greatly limits the statistical power of genetic studies.
In the last years, combined analysis of the results of large-scale genetic studies of different diseases, through cross-phenotype association studies, has made it possible to overcome the obstacle of sample size, leading to the identification of genetic risk loci shared among related disorders. This approach has already been used to explore the genetic overlap across vasculitides, specifically between KD and IgAV, using genome-wide association study (GWAS) data,6 and among GCA, TAK, AAV and IgAV, using Immunochip data.7 8
Nevertheless, these studies did not include some of the main forms of vasculitis and/or lacked the greater genomic coverage offered by the GWAS platform compared with the Immunochip. The purpose of the current study was, therefore, to comprehensively assess the genetic overlap among the major phenotypes of systemic vasculitis by combining GWAS data of GCA, TAK, KD, IgAV, BD and AAV as a single phenotype.
Methods
Study cohort
A total of 8467 patients with vasculitis, including 2134 GCA, 1091 TAK, 405 KD, 215 IgAV, 3197 BD, 914 AAV (MPA and GPA; 268 MPO-positive and 478 PR3-positive), 159 ANCA-positive EGPA and 352 ANCA-negative EGPA, and 29 795 healthy individuals were included in the study. A mixed population was analysed, including mainly Europeans (77.8%), but also Turkish (15.8%), Asians (5.8%) and Middle Easterners (0.64%). All the analysed datasets came from previously published GWAS,6 9–12 except for BD for which we included two case/control sets, one from a previous GWAS (BDGWAS) (obtained from dbGAP, accession number: phs000272.v1.p1) and one from a recent Immunochip study (BDIchip).13 14 To avoid overlap between cases of BD, we selected only those SNPs from the GWAS that were not included in the Immunochip study. In addition, several control sets, specifically those from Italy, Spain and UK, overlapped among diseases, which was taken into account for the later meta-analysis, as described below. A summary of the cohorts included in the study is provided in online supplemental table 1.
ard-2022-223697supp001.xlsx (391.2KB, xlsx)
Patient and public involvement
Patients or the public were not involved in any of the stages of our research.
Quality control and imputation of the GCA, BDGWAS and AAV datasets
For TAK, KD, IgAV, BDIchip and EGPA, summary statistics from the previous studies6 10 12 13 were used for the cross-disease meta-analysis. However, in the case of GCA, AAV and BDGWAS, data from previous GWAS9 11 14 were not imputed or imputed with small reference panels and, therefore, genotypic data were newly imputed using a larger reference panel to increase the number of single-nucleotide polymorphisms (SNPs) to analyse.
First, stringent quality controls were applied to each GCA cohort and the BDGWAS. Specifically, we individually analysed ten independent case/control sets for GCA and one for BD. GWAS data were filtered prior to imputation using PLINK V.1.9 software (www.cog-genomics.org/plink/1.9/).15 SNPs with low allele frequency (minor allele frequency <1%), low genotyping rate (<98%) and deviating from Hardy-Weinberg equilibrium (p<0.001) were removed. In addition, duplicates and first-degree relatives as well as individuals with successful call rates <95% were discarded. Finally, sex chromosomes were removed from further analyses.
SNP genotype imputation of GCA and BDGWAS datasets was performed using the Michigan Imputation Server V.1.0.316 and the TOPMed Imputation Server (https://imputation.biodatacatalyst.nhlbi.nih.gov/), with the HRC reference panel (HRC V.r1.1 2016) and the TOPMed Imputation Reference panel, respectively. A probability threshold for merging genotypes of r2=0.9 was applied. After imputation, principal component (PC) analysis was performed with PLINK 1.9 and the GCTA64 (Genome-wide Complex Trait Analysis) software17 and R-base under GNU Public licence V.2. Around 100 000 independent SNPs were selected and used to calculate the first ten PCs per individual. Individuals showing >4 SD from the cluster centroid were excluded by considering them as outliers.
In the case of the AAV cohort, prephasing and genome-wide SNP imputation were performed using Eagle2 and Minimac3, respectively, on the Michigan Imputation Server V.1.0.3 (HRC V.r1.1 2016). Postimputation, SNPs with MAF <0.01 or r2 <0.3 were removed from the dataset using BCFtools V.1.2.
The total number of SNPs and individuals that remained in the final filtered GCA, BDGWAS and AAV datasets is shown in online supplemental table 2.
Statistical analysis of the GCA, BDGWAS and AAV datasets
First, we performed independent association analyses for GCA, BDGWAS and AAV. In the case of GCA and BDGWAS, each case/control set was analysed by logistic regression including the first 10 PCs as covariates in PLINK 1.9, whereas case–control association testing of the AAV dataset was performed using a linear mixed model with BOLT-LMM software V.2.3.2.18 Then, for GCA, for which 10 independent case/control sets were available, we combined the different cohorts using an inverse variance weighted meta-analysis in METASOFT.19.
Cross-disease meta-analysis
Summary statistics of the eight phenotypes of vasculitis were used to identify those SNPs showing shared associations with at least two of the analysed disorders. We used ASSET20 to perform a subset-based meta-analysis, which allows identifying the best subset containing those diseases contributing to the overall association signal. Specifically, ASSET explores all possible subsets of phenotypes to identify the strongest association signal and then evaluates the significance of the signal while accounting for multiple tests required by the subset search. Since part of the control individuals included in the analysis were shared among different datasets (online supplemental table 1), correlation matrices were used to adjust for this overlapping. We tested all the SNPs shared by at least two summary statistics. Considering the complexity of the HLA region and that the associations within this locus with the different forms of vasculitis are well established, this region (Chr6: 20–40 MB) was excluded from further analysis. After cross-disease meta-analysis, those SNPs showing p values lower than 5E-08 were considered as statistically significant and, of these, we only focused on those signals for which more than one disease contributed to the association. In the case of SNPs for which opposite effects across diseases were found, they were considered as significant when both positively and negatively associated subsets showed p values lower than 0.05. When several SNPs were statistically significant within the same loci, those including the higher number of phenotypes in the best subset were considered as lead SNPs. In addition, for each pleiotropic locus, signals reaching genome-wide significance and showing r2 <0.1 were considered as independent.
Moreover, taking into account that MPO-positive and PR3-positive AAV patients can be considered as two genetically different entities, ASSET meta-analysis was also performed including both subgroups of AAV as two independent phenotypes.
Functional annotation of genetic variants and gene prioritisation
Next, to identify potential target genes of the identified pleiotropic variants, we used the SNP2GENE function of FUMA GWAS (Functional Mapping and Annotation of GWAS).21 Functional annotation of the predefined independent lead SNPs, and their proxies (r2 >0.6), were obtained to prioritise potential causal genes. Specifically, FUMA maps SNPs to genes based on three strategies, positional mapping, expression quantitative trait loci (eQTL) mapping and chromatin interaction mapping. In addition, using epigenomic data from the Roadmap Epigenomic Project, enhancers and promoters were also annotated to significantly interaction regions. Additionally, we also assessed the overlap of the cross-phenotype signals with splicing QTL obtained from the GTEx project (V.8). For the functional annotation, we only focused on relevant tissues in vasculitis (whole blood, immune cells and arterial tissue).
Regulatory element enrichment analysis
We used GARFIELD (GWAS analysis of regulatory or functional information enrichment with linkage disequilibrium (LD) correction)22 to explore whether the set of genetic variants shared across vasculitides colocalised with tissue-specific regulatory features extracted from the Roadmap Epigenomics project. Specifically, we selected nine histone marks related to active promoters, enhancers and active (or at least accessible) genes (H2BK20ac, H3K27ac, H3K4me1, H3K4me2, H3K4me3, H3K9ac, H3K4ac, H3K79me1, H2BK15ac). Briefly, GARFIELD quantifies functional annotation enrichment for associated SNPs at various p value thresholds (p≤1E-08, p≤1E-07, p≤1E-06, p≤1E-05) while taking into account LD, minor allele frequency and distance to the nearest transcription start site. In addition, from the wide catalogue of tissues and cell types included in the Roadmap Epigenomics project, we focused on immune cells. To adjust for multiple testing correction, we used the R code Garfield-Meff-Padj.R provided by GARFIELD to calculate an enrichment p value threshold (p≤6.12E-04) adjusted on the effective number of annotations (Meff=81.66).
Drug repurposing analysis
Finally, we used the database DrugBank (V.5.0)23 to explore whether proteins encoded by the prioritised genes are targets for approved, clinical trial or experimental drugs. In order to select the most potentially promising drugs for vasculitis, we focused on the mechanism of action of the different drugs as reported in DrugBank and we also performed a manual literature search using Pubmed and ClinicalTrials.gov.
Next, to calculate if the prioritised genes obtained through functional annotation were significantly enriched in targets of drugs indicated to autoimmune diseases, we applied Fisher’s exact test. For this analysis, we used gene-products of the prioritised genes in the previous analyses and unrelated to any of the analysed diseases, drug targets indicated for autoimmune diseases and coding genes of the genome that are potentially druggable (online supplemental table 3).
Results
Cross-phenotype meta-analysis
Summary statistics data of a total of 8467 patients diagnosed with any of the 8 types of vasculitis comprised in the current study and 29 795 healthy individuals were included in the analysis.
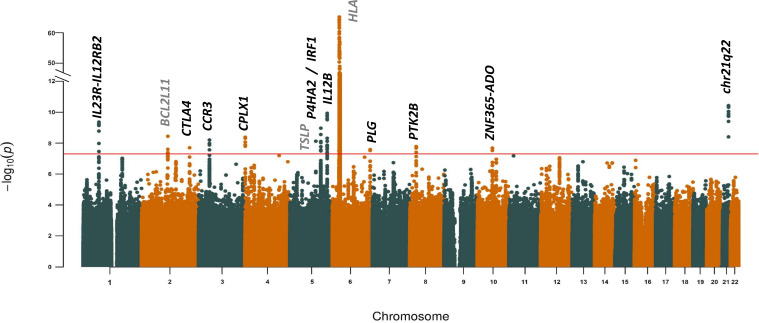
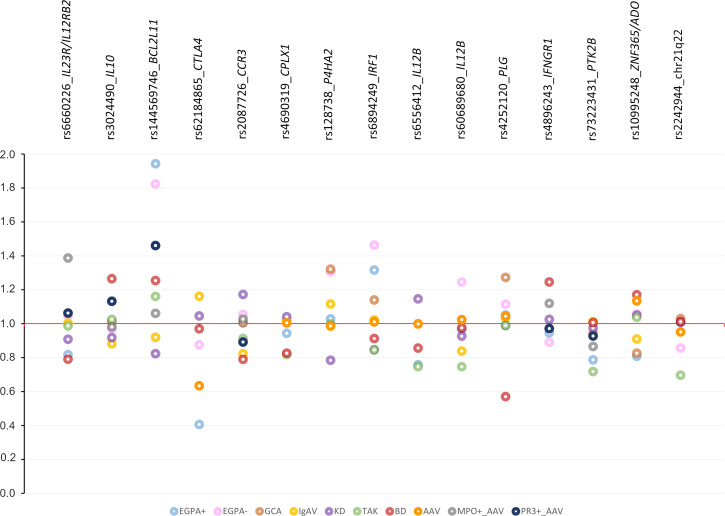
After cross-disease meta-analysis and excluding the HLA region, 85 genetic variants at 12 genomic regions were associated with two or more vasculitides at the genome-wide level of significance (figure 1). Based on LD, 14 genetic variants within these loci were independently associated (online supplemental table 4). Interestingly, 12 of these SNPs represented new associations for some of the phenotypes included in the best subset (table 1 and online supplemental table 4), 9 of them showing similar effects in all the diseases contributing to the association signal and three showing opposite effects across diseases (figure 2).
Figure 1.
Manhattan plot showing the results of the cross-phenotype meta-analysis. The −log10 of the p values are plotted against their physical chromosomal position. The red line represents the genome-wide level of significance (p<5×10−8). Loci reaching the significant threshold are annotated in the plot. Loci representing new shared risk loci in vasculitis are highlighted in bold.
Table 1.
Independent genetic variants reaching genome-wide significant level in the subset-based meta-analysis and representing novel risk loci shared across vasculitides
| Region | Base pair | SNP | Gene | A1 | P value | Contributing disease | OR (95% CI) |
| 1p31.3 | 67 751 193 | rs11209039 | IL23R/IL12RB2 | G | 6.45E-10 | BD EGPA+KD | 0.81 (0.76 to 0.87) |
| 2q33.2 | 204 689 376 | rs62184865 | CTLA4 | T | 2.00E-08 | AAV EGPA+ | 1.72 (1.43 to 2.08) |
| 3p21.31 | 46 208 310 | rs2087726 | CCR3 | G | 1.04E-08 | BD IgAV | 0.81 (0.75 to 0.87) |
| 4p16.2 | 824 988 | rs4690319 | CPLX1 | A | 4.72E-09 | BD TAK | 0.82 (0.77 to 0.88) |
| 5q31.1 | 131 540 875 | rs128738 | P4HA2 | T | 2.78E-09 | EGPA- GCA | 1.32 (1.20 to 1.44) |
| 5q31.1 | 131 797 547 | rs6894249 | IRF1 | G | 7.81E-09 | EGPA+ EGPA- | BD KD TAK | 1.40 (1.21 to 1.61) | 0.85 (0.83 to 0.94) |
| 5q33.3 | 158 777 001 | rs7725339 | IL12B | T | 1.84E-10 | BD EGPA+ TAK | 1.24 (1.15 to 1.32) |
| 5q33.3 | 158 834 367 | rs60689680 | IL12B* | T | 4.62E-08 | IgAV TAK | EGPA- | 1.32 (1.19 to 1.45) | 0.80 (0.69 to 0.95) |
| 6q26 | 161 143 608 | rs4252120 | PLG | C | 2.65E-08 | EGPA- GCA | 1.28 (1.17 to 1.39) |
| 8p21.2 | 27 219 987 | rs73223431 | PTK2B | T | 1.66E-08 | EGPA+TAK | 0.73 (0.66 to 0.82) |
| 10q21.2 | 64 396 042 | rs10995248 | ZNF365/ADO | T | 2.10E-08 | AAV BD | EGPA+GCA IgAV | 1.16 (1.08 to 1.24) | 0.84 (0.77 to 0.91) |
| 21q22.2 | 40 465 178 | rs2242944 | chr21q22 | A | 1.30E-10 | EGPA- TAK | 0.75 (0.68 to 0.82) |
*Novel signals within previously known loci. Diseases included in the best subset and for which identified associations have not been previously reported are shown in bold.
A1, alternative allele used in the logistic regression; AAV, ANCA-associated vasculitis; BD, Behçet’s disease; EGPA+, ANCA-positive eosinophilic granulomatosis with polyangiitis; EGPA-, ANCA-negative eosinophilic granulomatosis with polyangiitis; GCA, giant cell arteritis; IgAV, IgA vasculitis; KD, Kawasaki’s disease; TAK, Takayasu arteritis.
Figure 2.
Novel risk loci shared across vasculitides. Effect of the independent genetic variants reaching genome-wide significant level in the subset-based meta-analysis is shown. Circles represent the analysed phenotypes of vasculitis. AAV, ANCA-associated vasculitis; BD, Behçet’s disease; EGPA, eosinophilic granulomatosis with polyangiitis; GCA, giant cell arteritis; KD, Kawasaki disease; IgAV, IgA vasculitis; TAK, Takayasu’s arteritis.
Notably, two of these SNPs, rs4690319 and rs62184865, annotated by proximity to CPLX1 and CTLA4, respectively, have not been previously associated at the genome-wide level of significance with any vasculitis, thus representing novel susceptibility loci. In addition, the remaining 10 signals have been previously associated with only 1 of the diseases included in the best subset and, therefore, they can be considered as new shared risk loci.
Moreover, our analysis also identified two independent signals within the IL12B region, a known susceptibility locus for TAK. Three diseases, BD, ANCA-positive EGPA and TAK, contributed to the association observed for the rs7725339 genetic variant, which is in complete LD with the SNP previously associated with TAK (r2=1).12 In addition, rs60689680, which is not linked to the TAK-associated variant (r2=0.007), also emerged as a common susceptibility locus. Notably, this last SNP showed opposite effects across the diseases contributing to its association, with a risk effect in TAK and IgAV and a protective effect in ANCA-negative EGPA. In addition, two independent signals (r2=0.05) were identified within the 5q31.1 region. The first one (rs128738), previously associated with GCA and annotated to the P4HA2 gene, was also associated with ANCA-negative EGPA. The second one (rs6894249), previously associated with ANCA-negative EGPA and annotated to IRF1, appeared to be a common risk locus for a high number of vasculitides but with opposite effects across them (risk to ANCA-positive and ANCA-negative EGPA and protection to BD, KD and TAK). Finally, the signal located at the 10q21.2 region also revealed opposite effects. This locus, previously associated with BD, conferred risk to BD and AAV and protection to ANCA-positive EGPA, GCA and IgAV.
In addition, while AAV (considering MPA and GPA patients as a whole) was found to contribute to only two of the newly identified shared associations (table 1), meta-analysis considering MPO-positive and PR3-positive AAV as independent phenotypes allowed identifying a specific contribution of these subgroups to three of the identified common signals (table 2 and online supplemental table 5). Specifically, MPO-positive AAV was involved in the associations observed within the 1p31.1 and 8p21.2 loci whereas PR3-positive AAV contributed to the shared association identified at 3p21.31. Moreover, this analysis also yielded three new pleiotropic loci in vasculitis, 1q32.1 and 6q23.3, previously associated with BD and annotated to IL10 and IFNGR1, for which PR3-positive AAV and MPO-positive AAV, respectively, were contributing to the association, and 2q13, previously associated with EGPA and annotated to BCL2L11, for which PR3-positive AAV was also included in the best subset (table 2, online supplemental table 5 and figure 2).
Table 2.
Shared associations across vasculitides considering MPO and PR3-autoantibody specificity in patients with ANCA-associated vasculitis
| Region | Base pair | SNP | Gene | A1 | P value | Contributing disease | OR (95% CI) |
| 1p31.3 | 67 744 601 | rs6660226 | IL23R/IL12RB2 | A | 6.78E-11 | MPO+_AAV | BD EGPA+KD | 1.39 (1.10 to 1.75) | 0.79 (0.74 to 0.85) |
| 1q32.1 | 206 945 311 | rs3024490 | IL10* | A | 1.49E-08 | PR3+_AAV BD | 1.24 (1.15 to 1.34) |
| 2q13 | 111 905 867 | rs144569746 | BCL2L11* | T | 1.11E-08 | PR3+_AAV EGPA+EGPA- | 1.68 (1.40 to 2.00) |
| 3p21.31 | 46 208 310 | rs2087726 | CCR3 | G | 4.94E-09 | PR3+_AAV BD IgAV | 0.82 (0.77 to 0.88) |
| 6q23.3 | 137 514 790 | rs4896243 | IFNGR1* | C | 1.59E-08 | MPO+_AAV BD | 1.23 (1.15 to 1.32) |
| 8p21.2 | 27 219 987 | rs73223431 | PTK2B | T | 3.23E-08 | MPO+_AAV EGPA+TAK | 0.76 (0.69 to 0.84) |
Diseases included in the best subset and for which identified associations have not been previously reported are shown in bold.
*New shared associations identified in the meta-analysis considering MPO-positive and PR3-positive AAV as independent phenotypes.
A1, alternative allele used in the logistic regression; AAV, ANCA-associated vasculitis; BD, Behçet’s disease; EGPA+, ANCA-positive eosinophilic granulomatosis with polyangiitis; EGPA-, ANCA-negative eosinophilic granulomatosis with polyangiitis; IgAV, IgA vasculitis; KD, Kawasaki’s disease; TAK, Takayasu arteritis.
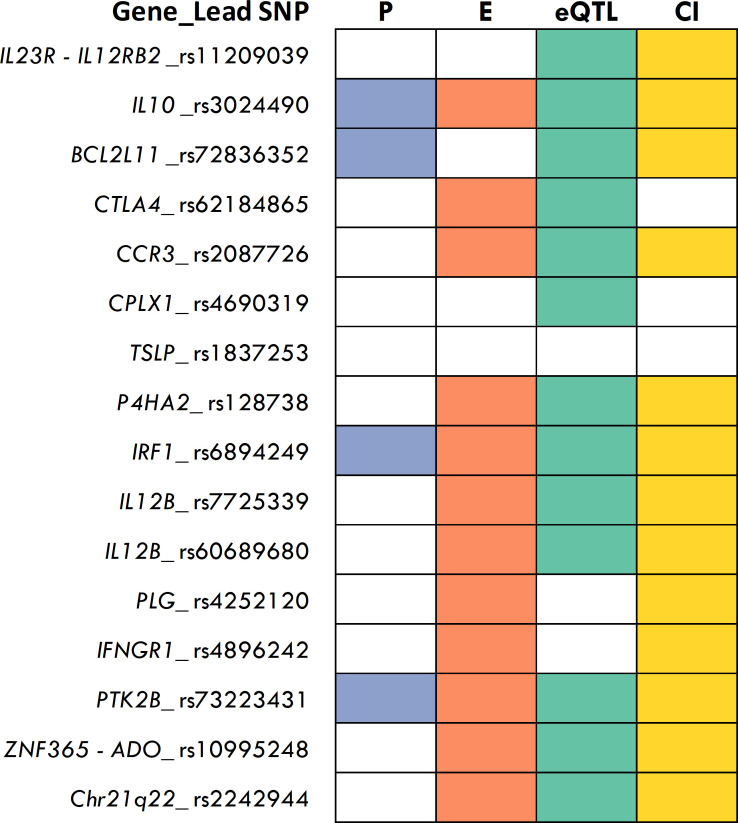
Functional annotation of pleiotropic variants
FUMA annotation of the shared genetic variants showed that none of the lead SNPs were coding, whereas five of their proxies (r2 ≥0.6) were exonic, including three non-synonymous variants, mapping at BCL2L11, IL3 and PLG, and two synonymous variants, mapping at PLG. Of these missense variants, only the SNP at BCL2L11 was annotated as possibly damaging according to SIFT and Polyphen scores (online supplemental table 6).
Since all the lead SNPs, and most of their proxies, were located in non-coding regions, we annotated them using FUMA to determine their overlap with functional regulatory elements as well as to prioritise their most probable target genes. Notably, all but one of the shared genetic variants overlapped with predicted regulatory regions in immune cells, whole blood and/or arterial tissue, whereas 69% overlap with at least three functional annotations (figure 3). Remarkably, 14 out of the 16 shared SNPs, or their proxies, appeared to act as eQTLs affecting gene expression levels (figure 3 and online supplemental table 7). Based on this annotation, FUMA prioritised 182 genes, of which 159 were protein-coding, as potential causal genes in vasculitis (table 3).
Figure 3.
Functional annotation of the identified pleiotropic variants. Colours indicate both lead and proxy polymorphisms overlapping with the different regulatory elements analysed. CI (yellow), chromatin interactions; E (orange), enhancers; P (blue), promoters; eQTL (green), expression quantitative trait loci.
Table 3.
Prioritised causal genes for the pleiotropic loci based on functional annotation by FUMA
| Region | Gene | Lead SNP | Nominated genes by proximity | Nominated genes by eQTL | Nominated genes by sQTL | Nominated genes by CI | Nominated genes by eQTL+CI | Nominated genes by eQTL+promoter |
| 1p31.3 | IL23R/IL12RB2 | rs11209039 | IL12RB2 | IL23R, MIER1, SLC35D1 | C1orf141 | |||
| 1q32.1 | IL10 | rs3024490 | IL10 | IL10, IL19, IL24, FAIM3 | IL19, FCMR, PIGR, FCAMR, C1orf116, YOD1, PFKB2, CR1, CR2, MAPKAPK2 | IL19 | YOD1, PFKB2, CR1, CR2, MAPKAPK2 | |
| 2q13 | BCL2L11 | rs72836352 | ACOXL, BCL2L11 | BCL11A, BCL2L11, C3AR1, CPVL, CSFR1, FAM46A, LARGE, MS4A14, MS4A7, MTSS1, PEA15, TNFRSF8 | ACOXL | BCL2L11 | ||
| 2q33.2 | CTLA4 | rs62184865 | CTLA4 | CTLA4 | ||||
| 3p21.31 | CCR3 | rs2087726 | CCR1, CCR3 | ABCB1, AGAP1, AUTS2, CAMTA1, CCR1, CCR2, CCR3, CCR5, CCR9, CCRL2, CFH, COLQ, CXCR6, CYP2E1, CYTH3, DPP4, ELOVL4, FYCO1, GZMK, IL7R, KDSR, KLRB1, LTK, LZTFL1, NCALD, RORA, RORC, SACM1L, SLAMF1, SMAD3, SYTL2, TDGF1, XCR1 | LZTFL1, FYCO1, CCR3 | CCR1, CCR2, CCR5, CCR9, CCRL2, CXCR6, FYCO1, LZTFL1, SACM1L, XCR1 | CCR1, CCR2, CCR5, CCR9, CCRL2, CXCR6, FYCO1, LZTFL1, SACM1L, XCR1 | |
| 4p16.2 | CPLX1 | rs4690319 | CPLX1 | CPLX1, CRIPAK, DGKQ, GAK, IDUA, MFSD7, MYL5, PCGF3, TMEM175, UVSSA | ||||
| 5q22.1 | TSLP | rs1837253 | TSLP | |||||
| 5q31.1 | P4HA2 | rs128738 | C5orf56, CSF2, IL3, P4HA2 | ACSL6, C5orf56, CDC42SE2, FNIP1, HINT1, LYRM7, P4HA2, RAD50, RAPGEF6, SLC224A, SLC22A5 | P4HA2, CDC42SE2, HINT | C5orf56, PDLIM4, RAD50, RAPGEF6, SLC22A5 | C5orf56, RAD50, RAPGEF6, SLC22A5 | |
| 5q31.1 | IRF1 | rs6894249 | C5orf56, IRF1, P4HA2 | ACSL6, AFF4, ALDH1A1, APBA2, C1QA, C1QB, C5orf56, CACNA2D3, CTSL, CYP2S1, CYP4F22, DDX58, EPB41L3, FAM26E, IL15, IL5, IRF1, KCNMA1, LAP3, LGALS3BP, MYOF, P4HA2, PDE7B, RAD50, SLC22A4, SLC22A5, STAT1, TCN2, TRANK1, TSPAN2, VAMP5, WARS | P4HA2, RAD50, IRF1, SLC22A4 | AFF4, C5orf56, CCNI2, GDF9, HSPA4, IL13, IL4, IL5, IRF1, KIF3A, LEAP2, PDL1M4, RAD50, SEPT8, SHROOM1, SLC22A5, SOWAHA, UQCRO, ZCCHC10 | AFF4, C5orf56, IL5, IRF1, RAD50, SLC22A5 | IL5, IRF1 |
| 5q33.3 | IL12B | rs7725339 | IL12B | NSMCE1, RNF145 | RNF145, UBLCP1 | RNF145 | ||
| 5q33.3 | IL12B | rs60689680 | RNF145 | ADRA1B, C5orf54, RNF145, TTC1, UBLCP1 | RNF145 | |||
| 6q26 | PLG | rs4252120 | PLG | AGPAT4, MAP3K4, PLG | ||||
| 6q23.3 | IFNGR1 | rs4896243 | IFNGR1, IL22RA2 | IFNGR1 | IFNGR1, TNFAIP3, IL20RA | IFNGR1 | IFNGR1 | |
| 8p21.2 | PTK2B | rs73223431 | PTK2B | CHRNA2, CTNNA1, EPHX2, PTK2B, TRIM35 | PTK2B | CLU, PTK2B, TRIM35 | PTK2B, TRIM35 | PTK2B, TRIM35 |
| 10q21.2 | ZNF365/ADO | rs10995248 | ZNF365 | ADO, EGR2, RTKN2 | ADO, ARID5B, EGR2, JMJD1C, NRBF2 | ADO, EGR2 | ||
| 21q22.2 | chr21q22 | rs2242944 | ETS2, HMGN1, LCA5L, WRB | ETS2 | ETS2 |
Genes nominated by eQTL + promoter and also with CI are highlighted in bold
CI, chromatin interaction; eQTL, expression quantitative trait loci; sQTL, splicing quantitative trait loci.
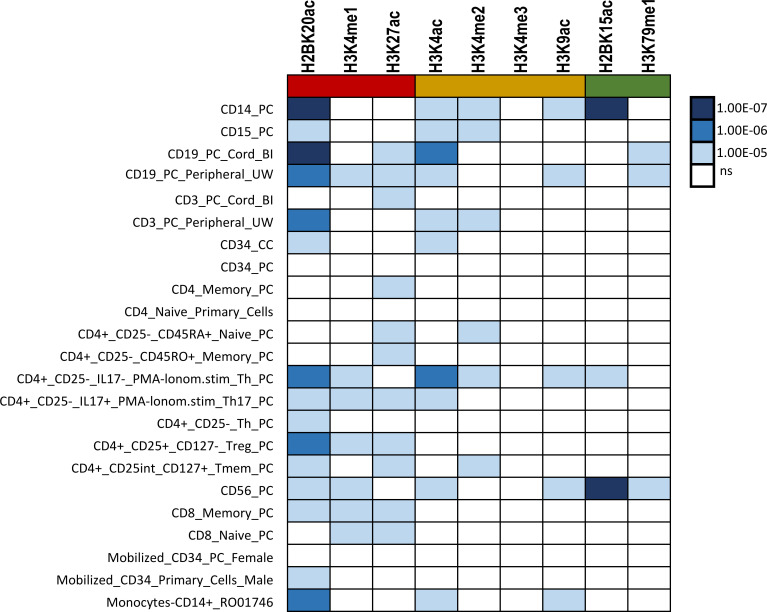
Regulatory element enrichment
Considering that most of the shared genetic variants overlapped with regulatory regions, we applied GARFIELD to determine whether the set of pleiotropic polymorphisms was enriched in tissue-specific histone modifications. We detected a total of 60 significant enrichments (p≤6.12E-04) in all the analysed immune cell types (figure 4). The most significant enrichments were found for H2BK15ac (mapping accessible genes), in NK cells (p=1.07E-07) and monocytes (p=9.37E-07); H2BK20ac (mapping enhancer regions), in monocytes (p=1.46E-07), B cells (p=7.98E-07) and CD4+T cells (p=2.72E-06); and H3K4ac (mapping promoter regions), in B cells (p=1.55E-06) and CD4+T cells (p=2.11E-06). Specific enrichment in these cell types was found for at least five of the nine analysed histone marks.
Figure 4.
Results of the histone mark enrichment analysis of the set of pleiotropic variants. First column shows the analysed cell-types. The remaining columns denote the analysed histone modifications, including histone marks associated with enhancers (red colour), promoters (orange colour) and accessible genes (green). Results of the enrichment analysis are represented in a scale-based colour gradient depending on the p value. Blue indicates enrichment and white indicates no statistical significance.
Similar results were found when enrichment analysis was performed based on the results of the meta-analysis considering MPO-positive and PR3-positive AAV as independent phenotypes (online supplemental table 8).
Drug-repurposing candidates in vasculitis
Finally, we performed a drug repurposing analysis with the aim of identifying new potential therapies for the analysed vasculitides. Proteins encoded by 33 of the 159 prioritised coding-genes were targets of both pharmacologically active drugs indicated for any disease and drugs with unknown mechanisms of action but currently indicated for immune-mediated diseases (online supplemental table 9). In total, we identified 103 drugs that could be potentially repurposed in vasculitis (online supplemental table 9), 13 of which are currently indicated for immune-mediated disorders (table 4).
Table 4.
Drugs indicated for immune-mediated disorders that could be potentially repurposed in systemic vasculitis
| Associated genomic region | Target gene | Drug | Type | Indication | Potential clinical application |
| 2q33.2 | CTLA4 | Abatacept | Fusion proteins | RA, PsA, JIA | AAV EGPA+ |
| 3p21.31 | LTK | Fostamatinib | Small molecule | Chronic immune thrombocytopenia | BD IgAV |
| 4p16.2 | GAK | Fostamatinib | Small molecule | Chronic immune thrombocytopenia | BD TAK |
| IDUA | Chondroitin sulfate | Small molecule | Primary osteoarthritis | ||
| 5q31.1 | C1QA/C1QB | Daclizumab | mAb | MS | EGPA+EGPA BD KD TAK |
| CTSL | Fostamatinib | Small molecule | Chronic immune thrombocytopenia | ||
| IL13 | Tralokinumab | mAb | Atopic dermatitis | ||
| IL5 | Mepolizumab | mAb | EGPA, Asthma, Hypereosinophilic syndrome | ||
| Reslizumab | mAb | Asthma | |||
| 5q33.3 | IL12B | Ustekinumab | mAb | Ps, PsA, CD, UC | BD EGPA+TAK |
| Tildrakizumab | mAb | Ps | |||
| Risankizumab | mAb | Ps, PsA, CD | |||
| 6q26 | MAP3K4 | Fostamatinib | Small molecule | Chronic immune thrombocytopenia | EGPA- GCA |
| 6q23.3 | TNFAIP3 | Mesalazine | Small molecule | UC | MPO-AAV BD |
| Sulfasalazine | Small molecule | UC, RA | |||
| 8p21.2 | PTK2B | Leflunomide | Small molecule | RA | EGPA+TAK |
| Fostamatinib | Small molecule | Chronic immune thrombocytopenia |
AAV, ANCA-associated vasculitis; BD, Behçet’s Disease; CD, Crohn’s disease; EGPA+, ANCA-positive EGPA; EGPA-, ANCA-negative EGPA; EGPA, eosinophilic granulomatosis with polyangiitis; GCA, giant cell arteritis; IgAV, IgA vasculitis; JIA, juvenile idiopathic arthritis; KD, Kawasaki’s disease; MS, multiple sclerosis; Ps, psoriasis; PsA, psoriatic arthritis; RA, rheumatoid arthritis; TAK, Takayasu’s arteritis; UC, ulcerative Colitis.
Interestingly, drug enrichment analysis revealed that the set of prioritised coding-genes was significantly enriched in pharmacological active drug targets currently used in the treatment of autoimmune diseases (OR=2.19 (95% CI 1.10 to 3.97); Fisher’s exact test p=1.57E-02) (online supplemental table 3).
Discussion
In this study, we performed a comprehensive analysis of the genetic overlap across the major forms of systemic vasculitis. The results greatly improve our knowledge regarding the genetic architecture of these conditions. We identified 15 new shared risk loci, most of which appear to affect disease by regulating gene expression levels, and prioritised potential causal genes based on functional annotation of pleiotropic polymorphisms.
Although all the lead pleiotropic SNPs, and most of their proxies, were located in non-coding regions, functional annotation also showed some non-synonymous variants, located at BCL2L11 (2q13) and PLG (6q26), in almost complete LD with the most associated polymorphisms. Considering their potential direct effect on protein function, they could be considered as the most probable causal variants within these loci, thus supporting the role of PLG, involved in vascular remodelling and angiogenesis, and BCL2L11, encoding a Bcl2 family member involved in apoptosis and immune homeostasis, as causal genes in vasculitis.
In addition, this strategy allowed us to identify two shared loci that have not been previously associated with any vasculitis at the genome-wide significance level. For one of these loci (lead SNP rs62184865), functional annotation prioritised CTLA4, a common genetic risk locus in autoimmunity involved in the negative regulation of T cell activation, as the most probable causal gene. Specifically, AAV (including MPA and GPA) and ANCA-positive EGPA contributed to this association signal in our cross-disease meta-analysis. This is in line with the results of previous GWAS suggesting a role of CTLA4 in the susceptibility to MPA and GPA11 24; however, no genomic association was found in these studies. Therefore, our findings provide for the first time genomic evidence of association between this locus and AAV, adding ANCA-positive EGPA to the list of diseases in which this locus plays a pleiotropic role. Regarding the other new vasculitis-associated locus (lead SNP rs4690319), 10 genes were prioritised (CPLX1, CRIPAK, DGKQ, GAK, IDUA, MFSD7, MYL5, PCGF3, TMEM175, UVSSA) based on eQTL overlap. However, no obvious role in the immune response or any process directly related with the pathogenesis of vasculitis has been described for these genes, to date. Further studies are warranted to fully understand how this locus might be affecting the pathophysiology of the associated vasculitides. It should be noted that this locus has not been associated with any immune-mediated disease so far, which suggests a specific role in vasculitis susceptibility. This is also the case of the associations at the P4HA2, PLG, IL10 and IFNGR1 loci, which have been previously reported in a single disease, the first two in GCA9 and the last two in BD.13 14 Our results now indicate that these risk factors are common to GCA and ANCA-negative EGPA, in the case of P4HA2 and PLG, and shared between BD and PR3-positive AAV, in the case of IL10, and between BD and MPO-positive AAV, in the case of IFNGR1. Interestingly, the P4HA2 variant has also been associated with eosinophil count,25 a crucial cell type in the pathophysiology of EGPA, which would explain its role in the susceptibility to this vasculitis.
Moreover, two independent signals at the 5q33.3 locus were also identified, one of them (lead SNP rs7725339) previously associated with TAK and annotated to IL12B,12 and now also associated with BD and ANCA-positive EGPA, and another one (lead SNP rs60689680) that represents a novel signal in vasculitis and appeared to confer risk to TAK and IgAV and protection to ANCA-negative EGPA. Surprisingly, functional annotation of both signals pointed to RNF145, encoding an E3 ubiquitin ligase, as the most likely causal gene. This gene was recently shown to activate the NF-κB signalling pathway and to promote the transcription of IL-8, a chemotactic factor that attracts neutrophils to the site of inflammation and that is involved in angiogenesis.26 Interestingly, increased levels of this chemokine have been reported in all the vasculitides contributing to the association signals, EGPA,27 IgAV,28 TAK29 and BD.30 Nevertheless, prioritisation based on positional mapping also nominated IL12B as the target gene of the signal originally associated with TAK. This gene encodes the p40 subunit common to IL-12 and IL-23, two cytokines that are crucial in Th1 and Th17 responses, respectively. Therefore, given the relevant role of this gene in inflammation and the proven usefulness of prioritisation based on physical proximity,31 it could be possible that this variant influences vasculitis by affecting both RNF145 and IL12B.
Genetic variants at nine additional loci, previously associated with a single vasculitis, emerged as new shared associations. Although several of these pleiotropic loci included multiple prioritised genes, two or less genes showed the strongest evidence of causality in five of these loci, 5q31.1, 6q23.3, 8p21.2, 10q21.2 and 21q22.2. These highly probable causal genes included IL5, IRF1, IFNGR1, PTK2B, TRIM35, ADO, EGR2 and ETS2. Both IL5 and IRF1 were linked to the association signal at 5q31.1 (lead SNP rs6894249), which conferred risk to ANCA-positive and ANCA-negative EGPA and protection to BD, KD and TAK. Notably, IL5 encodes a Th2 cytokine involved in the regulation of growth, activation, recruitment and survival of eosinophils,32 whereas IRF1 encodes a transcription factor that promotes transcription of genes involved in both innate and acquired immune responses.33 Considering this, the opposite effect observed across vasculitides could be due to the different biological consequences of the shared genetic variant in different cell types. Indeed, the lead SNP (rs6894249) affects IL5 expression levels in Th1/17 cells and IRF1 levels in monocytes (online supplemental table 7). Therefore, it could be hypothesised that this signal influences EGPA pathogenesis by regulating IL5 in one cell type, but affects BD, KD and TAK by regulating IRF1 in another.
Along with the 5q31.1 locus, 10q21.2 was also found associated with multiple vasculitides, including the already known association with BD,13 but also with AAV, to which it confers risk, and GCA, IgAV and ANCA-positive EGPA, in which has a protective effect. This locus was also mapped to two different genes, ADO, encoding a dioxygenase involved in amino acid metabolism and EGR2, which plays a crucial role in regulating inflammation in different cell types and has been involved in autoimmunity.34–36 Indeed, a recent study has described a role of EGR2 in the impaired frequency and function of type 1 regulatory T (Tr1) cells detected in IgAV, one of the vasculitides contributing to this association.37 Therefore, EGR2 seems to be a more plausible candidate to be involved in vasculitis pathogenesis. Regarding the 8p21.2 locus, two genes with a role in the immune response, PTK2B and TRIM35, were prioritised. The protein encoded by PTK2B is involved in promoting T and B cell adhesion and migration,38 39 whereas TRIM35 plays a role in the innate immune response.40 The association at the 6q23.3 region was detected when analysing AAV patients according to autoantibody specificity. Two phenotypes contributed to this signal, BD, previously associated with this locus13 and MPO-positive AAV. The IFNGR1 gene, which plays a crucial role in inflammation, emerged as a highly probable causal gene within this region. Finally, and supporting previous results, a single gene, ETS2, was linked to the 21q22.2 locus,12 which was associated with TAK and ANCA-negative EGPA according to our results. It has been described that this transcription factor has anti-inflammatory functions, however, ETS2 is also involved in the differentiation, activation and survival of macrophages,41 and in promoting angiogenesis.42
It should be noted that our study did not replicate the association between the KDM4C polymorphism rs16925200 and several vasculitides (GCA, TAK, IgAV and AAV) previously reported in a meta-Immunochip study.8 Although several of these diseases contributed to this signal in our study, namely IgAV and AAV, this association did not reached genome-wide significance (p=0.036). Taking into account, these contradictory results, further studies are needed to clarify the role of KDM4C as a common risk locus for vasculitis.
Enrichment analysis of shared genetic risk variants in histone marks related with active gene transcription evidenced a specific regulatory role of these polymorphisms in monocytes and NK, B and CD4+T cells, thus suggesting that these cell types are especially relevant for the common pathogenic mechanisms influencing vasculitis. It is worth highlighting that NK cells showed the strongest enrichment signal. These results support previous knowledge about the pathogenesis of vasculitis and suggest that special attention should be paid to NK cells, whose role in vasculitis is less well understood.
It has become increasingly evident that GWAS findings are useful in identifying opportunities for repurposing existing drugs.43 In this regard, based on the results of our cross-phenotype analysis, we identified several drugs that could be potentially repositioned for vasculitis, some of which are especially promising, since they are already indicated for the treatment of other immune-mediated disorders. Indeed, two of these drugs, abatacept, a fusion protein consisting of the Fc region of IgG1 and the extracellular domain of CTLA4 that inhibits T cell costimulation, and ustekinumab, a monoclonal antibody against the p40 subunit encoded by IL12B, are currently in clinical trials in some of the vasculitides contributing to these associations, GPA (NCT02108860), TAK (NCT04882072) and BD (NCT02648581). It is also interesting that several of the prioritised genes were target for the same drug, Fostamatinib, a tyrosine kinase inhibitor, which would support the potential clinical utility of this drug in the treatment of the different vasculitides contributing to these associations.
Despite the large number of individuals analysed in this study, the fact of meta-analysing data from different studies and that were, therefore, genotyped with different platforms, imputed using different reference panels and filtered based on slightly different quality criteria, may affect the overlap of variants, thus decreasing the statistical power of the analysis. Therefore, the existence of additional shared associations in vasculitis that were not detected here cannot be ruled out. In addition, through in silico functional annotation, we have been able to prioritise several genes as potentially causal; however, experimental validation of these results is essential to confirm the role of these loci in vasculitis susceptibility.
In conclusion, through the largest and most comprehensive cross-phenotype study performed to date in vasculitis, we provided new insights into the shared genetic component across vasculitides, revealing common biological mechanisms and new therapeutic options that could be explored for the treatment of these diseases.
Acknowledgments
We thank all the patients and control donors who participated in this study and Sofia Vargas and Gema Robledo for their excellent technical assistance. We would like to acknowledge the support and help by the late Dr Justin C. Mason. This research is part of the doctoral degree awarded by E.G.C, within the Biomedicine program from the University de Granada entitled 'Estudio de las bases moleculares de la arteritis de células gigantes mediante el análisis e integración de datos –ómicos'. This work was supported by the use of study data downloaded from the dbGaP web site (accession number: phs000272.v1.p1).
Footnotes
Handling editor: Josef S Smolen
EGC and MK contributed equally.
Contributors: LO-F, MK, EGC and AM: data analysis and interpretation of the results. LO-F and AM: manuscript drafting. PL, FDC, RLM, CCK, PCG, ET, LJ, JM, HD, GS-D, AWM, PAM, DB, AHS, KGCS, MAG-G: sample and data collection. AM and JM: study design and guarantors of the study. All authors revised critically the manuscript draft. All authors read and approved the manuscript.
Funding: This work was supported by the HELICAL Innovative Training Network, a European Commission funded project under the Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 813545, the Cooperative Research Thematic Network programme (RD16/0012/0013), Redes de Investigación Cooperativa Orientadas a Resultados en Salud (RICORS) (RD21/0002/0039) and by grant PI18/00040 funded by Instituto de Salud Carlos III. LO-F was supported by Juan de la Cierva Incorporación fellowship (IJC2019-040746-I) funded by MCIN/AEI /10.13039/501100011033. AHS is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health grant number R01 AR070148. DB is supported by a National Health and Medical Research Council (Australia) Investigator Grant (GTN1175744). Research at Murdoch Children’s Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. The Vasculitis Clinical Research Consortium (VCRC) received funding as part of the Rare Diseases Clinical Research Network (RDCRN), an initiative of the Office of Rare Diseases Research (ORDR), National Center for Advancing Translational Science (NCATS) and received funds from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), U54 AR057319) and the National Center for Research Resources (U54 RR019497).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the CSIC Ethic Committee and the Ethic Committee of Research of the Granada Province (CEIM/CEI). These organisations do not provide a reference number. Participants gave informed consent to participate in the study before taking part.
References
- 1. Jennette JC, Falk RJ, Bacon PA. Overview of the 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Clin Exp Nephrol 2013;17:603–6. 10.1007/s10157-013-0869-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grayson PC, Cuthbertson D, Carette S, et al. New features of disease after diagnosis in 6 forms of systemic vasculitis. J Rheumatol 2013;40:1905–12. 10.3899/jrheum.121473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Katsuyama T, Sada KE, Makino H. Current concept and epidemiology of systemic vasculitides. Allergol Int 2014;63:505–13. 10.2332/allergolint.14-RAI-0778 [DOI] [PubMed] [Google Scholar]
- 4. Saadoun D, Vautier M, Cacoub P. Medium- and large-vessel vasculitis. Circulation 2021;143:267–82. 10.1161/CIRCULATIONAHA.120.046657 [DOI] [PubMed] [Google Scholar]
- 5. Acosta-Herrera M, González-Gay MA, Martín J, et al. Leveraging genetic findings for precision medicine in vasculitis. Front Immunol 2019;10:1796. 10.3389/fimmu.2019.01796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carmona EG, García-Giménez JA, López-Mejías R, et al. Identification of a shared genetic risk locus for Kawasaki disease and immunoglobulin A vasculitis by a cross-phenotype meta-analysis. Rheumatology (Oxford) 2022;61:1204–10. 10.1093/rheumatology/keab443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carmona FD, Coit P, Saruhan-Direskeneli G, et al. Analysis of the common genetic component of large-vessel vasculitides through a meta-immunochip strategy. Sci Rep 2017;7:43953. 10.1038/srep43953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ortiz-Fernández L, Carmona FD, López-Mejías R, et al. Cross-phenotype analysis of immunochip data identifies KDM4C as a relevant locus for the development of systemic vasculitis. Ann Rheum Dis 2018;77:589–95. 10.1136/annrheumdis-2017-212372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carmona FD, Vaglio A, Mackie SL, et al. A genome-wide association study identifies risk alleles in plasminogen and P4HA2 associated with giant cell arteritis. Am J Hum Genet 2017;100:64–74. 10.1016/j.ajhg.2016.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lyons PA, Peters JE, Alberici F, et al. Genome-wide association study of eosinophilic granulomatosis with polyangiitis reveals genomic loci stratified by ANCA status. Nat Commun 2019;10:5120. 10.1038/s41467-019-12515-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lyons PA, Rayner TF, Trivedi S, et al. Genetically distinct subsets within ANCA-associated vasculitis. N Engl J Med 2012;367:214–23. 10.1056/NEJMoa1108735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ortiz-Fernández L, Saruhan-Direskeneli G, Alibaz-Oner F, et al. Identification of susceptibility loci for takayasu arteritis through a large multi-ancestral genome-wide association study. Am J Hum Genet 2021;108:84–99. 10.1016/j.ajhg.2020.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ortiz Fernández L, Coit P, Yilmaz V, et al. Genetic association of a gain-of-function IFNGR1 polymorphism and the intergenic region LNCAROD/DKK1 with Behçet’s disease. Arthritis Rheumatol 2021;73:1244–52. 10.1002/art.41637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Remmers EF, Cosan F, Kirino Y, et al. Genome-Wide association study identifies variants in the MHC class I, IL10, and IL23R-IL12RB2 regions associated with Behçet’s disease. Nat Genet 2010;42:698–702. 10.1038/ng.625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chang CC, Chow CC, Tellier LC, et al. Second-Generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 2015;4:7. 10.1186/s13742-015-0047-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Das S, Forer L, Schönherr S, et al. Next-Generation genotype imputation service and methods. Nat Genet 2016;48:1284–7. 10.1038/ng.3656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang J, Lee SH, Goddard ME, et al. GCTA: a tool for genome-wide complex trait analysis. Am J Hum Genet 2011;88:76–82. 10.1016/j.ajhg.2010.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Loh P-R, Bhatia G, Gusev A, et al. Contrasting genetic architectures of schizophrenia and other complex diseases using fast variance-components analysis. Nat Genet 2015;47:1385–92. 10.1038/ng.3431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Han B, Eskin E. Random-effects model aimed at discovering associations in meta-analysis of genome-wide association studies. Am J Hum Genet 2011;88:586–98. 10.1016/j.ajhg.2011.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bhattacharjee S, Rajaraman P, Jacobs KB, et al. A subset-based approach improves power and interpretation for the combined analysis of genetic association studies of heterogeneous traits. Am J Hum Genet 2012;90:821–35. 10.1016/j.ajhg.2012.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Watanabe K, Taskesen E, van Bochoven A, et al. Functional mapping and annotation of genetic associations with FUMA. Nat Commun 2017;8:1826. 10.1038/s41467-017-01261-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Iotchkova V, Ritchie GRS, Geihs M, et al. Garfield classifies disease-relevant genomic features through integration of functional annotations with association signals. Nat Genet 2019;51:343–53. 10.1038/s41588-018-0322-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wishart DS, Feunang YD, Guo AC, et al. DrugBank 5.0: a major update to the drugbank database for 2018. Nucleic Acids Res 2018;46:D1074–82. 10.1093/nar/gkx1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Xie G, Roshandel D, Sherva R, et al. Association of granulomatosis with polyangiitis (Wegener’s) with HLA-DPB1*04 and SEMA6A gene variants: evidence from genome-wide analysis. Arthritis Rheum 2013;65:2457–68. 10.1002/art.38036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kachuri L, Jeon S, DeWan AT, et al. Genetic determinants of blood-cell traits influence susceptibility to childhood acute lymphoblastic leukemia. Am J Hum Genet 2021;108:1823–35. 10.1016/j.ajhg.2021.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rong L, Chen B, Liu K, et al. CircZDBF2 up-regulates RNF145 by cerna model and recruits CEBPB to accelerate oral squamous cell carcinoma progression via NFκB signaling pathway. J Transl Med 2022;20:148. 10.1186/s12967-022-03347-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Khoury P, Zagallo P, Talar-Williams C, et al. Serum biomarkers are similar in Churg-Strauss syndrome and hypereosinophilic syndrome. Allergy 2012;67:1149–56. 10.1111/j.1398-9995.2012.02873.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang YH, Lai HJ, Huang CM, et al. Sera from children with active Henoch-Schönlein purpura can enhance the production of interleukin 8 by human umbilical venous endothelial cells. Ann Rheum Dis 2004;63:1511–3. 10.1136/ard.2003.016196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Alibaz-Oner F, Yentür SP, Saruhan-Direskeneli G, et al. Serum cytokine profiles in Takayasu’s arteritis: search for biomarkers. Clin Exp Rheumatol 2015;33(2 Suppl 89):S–32 [PubMed] [Google Scholar]
- 30. Novak T, Hamedi M, Bergmeier LA, et al. Saliva and serum cytokine profiles during oral ulceration in behçet’s disease. Front Immunol 2021;12:724900. 10.3389/fimmu.2021.724900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mountjoy E, Schmidt EM, Carmona M, et al. An open approach to systematically prioritize causal variants and genes at all published human GWAS trait-associated loci. Nat Genet 2021;53:1527–33. 10.1038/s41588-021-00945-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosenberg HF, Dyer KD, Foster PS. Eosinophils: changing perspectives in health and disease. Nat Rev Immunol 2013;13:9–22. 10.1038/nri3341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol 2014;14:36–49. 10.1038/nri3581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Veremeyko T, Yung AWY, Anthony DC, et al. Early growth response gene-2 is essential for M1 and M2 macrophage activation and plasticity by modulation of the transcription factor cebpβ. Front Immunol 2018;9:2515. 10.3389/fimmu.2018.02515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Okamura T, Yamamoto K, Fujio K. Early growth response gene 2-expressing CD4+LAG3+ regulatory T cells: the therapeutic potential for treating autoimmune diseases. Front Immunol 2018;9:340. 10.3389/fimmu.2018.00340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Morita K, Okamura T, Sumitomo S, et al. Emerging roles of EGR2 and EGR3 in the control of systemic autoimmunity. Rheumatology (Oxford) 2016;55(suppl 2):ii76–81. 10.1093/rheumatology/kew342 [DOI] [PubMed] [Google Scholar]
- 37. Pan L, Wang J, Liu J, et al. Deficiency in the frequency and function of tR1 cells in igav and the possible role of IL-27. Rheumatology (Oxford) 2021;60:3432–42. 10.1093/rheumatology/keaa752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hamoudi C, Muheidli A, Aoudjit F. Β1 integrin induces adhesion and migration of human Th17 cells via Pyk2-dependent activation of P2X4 receptor. Immunology 2023;168:83–95. 10.1111/imm.13563 [DOI] [PubMed] [Google Scholar]
- 39. Tse KWK, Lin KBL, Dang-Lawson M, et al. Small molecule inhibitors of the Pyk2 and FAK kinases modulate chemoattractant-induced migration, adhesion and Akt activation in follicular and marginal zone B cells. Cell Immunol 2012;275:47–54. 10.1016/j.cellimm.2012.03.002 [DOI] [PubMed] [Google Scholar]
- 40. Sun N, Jiang L, Ye M, et al. TRIM35 mediates protection against influenza infection by activating TRAF3 and degrading viral PB2. Protein Cell 2020;11:894–914. 10.1007/s13238-020-00734-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sevilla L, Zaldumbide A, Carlotti F, et al. Bcl-Xl expression correlates with primary macrophage differentiation, activation of functional competence, and survival and results from synergistic transcriptional activation by Ets2 and PU.1. J Biol Chem 2001;276:17800–7. 10.1074/jbc.M008270200 [DOI] [PubMed] [Google Scholar]
- 42. Cheng C, Tempel D, Den Dekker WK, et al. Ets2 determines the inflammatory state of endothelial cells in advanced atherosclerotic lesions. Circ Res 2011;109:382–95. 10.1161/CIRCRESAHA.111.243444 [DOI] [PubMed] [Google Scholar]
- 43. Reay WR, Cairns MJ. Advancing the use of genome-wide association studies for drug repurposing. Nat Rev Genet 2021;22:658–71. 10.1038/s41576-021-00387-z [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ard-2022-223697supp001.xlsx (391.2KB, xlsx)
Data Availability Statement
Data are available on reasonable request.