Abstract
Background
The care ability of caregivers markedly impacts the patient’ s quality of life and such ability may be influenced by various factors. This study aimed to explore the factors affected the care ability of caregivers for hemodialysis patients.
Material/Methods
This cross-sectional study involved 271 caregivers of hemodialysis patients. Various basic sociodemographic data of patients and caregivers were collected using questionnaires. The care abilities of caregivers were evaluated by the Caregiver Task Inventory (CTI). Univariate and multivariate linear regression analyses were used to identify the independent factors associated with the care ability of caregiver. The independent samples t test was used to further explore the impact of the independent factors on caregiver’s care ability.
Results
The mean age was 54.88±10.73 years for the patients and 44.68±15.22 years for the caregivers. Among the 271 hemodialysis patients, 59.04% were male. Multivariate regression analysis showed that female caregivers (standardized β=−0.140, P=0.002), lived with patients (standardized β=−0.381, P<0.001), high annual income of caregivers (standardized β=−0.281, P<0.001), receiving caregiving training (standardized β=−0.183, P<0.001), and patients without other chronic diseases (standardized β=0.200, P<0.001) were associated with better care abilities of caregivers.
Conclusions
The gender and annual income of caregivers, receiving caregiving training, cohabitation with patient, and other concurrent chronic diseases of patients were the independent influencing factors for the care ability of caregivers for hemodialysis patients. Our study emphasized the necessity of implementing comprehensive socioeconomic and educational support to improve the care ability of caregivers.
Keywords: Caregivers, Patient Acceptance of Health Care, Renal Dialysis
Background
A caregiver is anyone who provides assistance and support to an individual in need due to chronic illness, disability, or age-related conditions [1,2]. Caregivers can be family members, friends, or trained professionals [3]. They provide essential support to patients, including administering medication, providing emotional support, managing dietary restrictions, and coordinating medical appointments [4], and thus play critical roles in managing the health and well-being of patients.
End-stage kidney disease (ESKD) is a terminal illness requiring prolonged treatment to support the body’s needs [5,6]. Hemodialysis is the most common treatment for ESKD, chosen by almost 90% of patients [7,8]. Previous studies showed that hemodialysis patients face a wide range of challenges and experience physical, psychological, and social burdens [9–11]. The common complications of hemodialysis are fatigue, malnutrition, nausea, sleep disturbances, renal anemia, and muscle cramps [12,13]. Moreover, frequent hemodialysis and restrictive dietary diet may alter the lifestyles of patients and have a severe impact on daily life [14]. Hemodialysis is time-consuming; patients have to spend a long time in the hospital or treatment center, which limits participation in social activities [15]. Hemodialysis patients may also have psychological issues like anxiety and depression [9]. Because of these difficulties, almost all hemodialysis patients require assistance from caregivers to manage their daily life [16]. As a consequence, the care abilities of caregivers significantly impact the patients’ quality of life [17,18]. Although the caregivers play vital roles for patients undergoing hemodialysis, few studies have investigated the factors affecting the care ability of caregivers.
Previous studies revealed that the overwhelming stress caused by long-term care of stroke patients hindered the ability of family caregivers [19,20]. Providing interventional educational programs to the caregiver for patients may improve their caregiving abilities. However, there has been little research on factors associated with the ability of caregivers of hemodialysis patient. Identifying possible factors associated with the care ability of caregivers could improve integrated healthcare strategies for the illness [21]. Unfortunately, there is no consensus on this, especially those caring for patients undergoing hemodialysis. Therefore, we focused on the caregivers of hemodialysis patients in this study. The primary aim was to explore which factors affected the care ability of caregivers. This will provide a foundation for improving the comprehensive care abilities of caregivers and the patients’ quality of life.
Material and Methods
Study Participants
This study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital and was performed in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The study objective and data confidentiality were communicated to patients and their caregivers. Written informed consent was obtained from patients and their primary caregivers prior to enrollment.
This cross-sectional study investigated 271 primary caregivers who provided care for patients undergoing hemodialysis. All patients received regular hemodialysis in Guangdong Provincial People’s Hospital between February 2021 and February 2023. The included patients were diagnosed as having end-stage kidney disease (ESKD) with glomerular filtration rate (GFR) less than 15 ml/(min·1.73 m2) and were aged more than 18 years. Patients were excluded from the study if they had psychiatric disorders or cognitive illnesses, or if they only received temporary hemodialysis.
Patients were asked to identify their primary caregiver. The inclusion criteria for the caregiver were: (1) age ≥18 years, (2) maintained frequent contact with the patient; (3) present with the patient during the whole hemodialysis process; (4) provided care for the patient’s daily life; and (5) provided significant financial support to the patient. The exclusion criteria for the caregiver were: (1) psychiatric disorders or cognitive illnesses; (2) unable to complete the study questionnaires; or (3) hearing or visual impairment.
Measures
The basic sociodemographic data of patients and caregivers were collected using questionnaires in Chinese. We collected information on hemodialysis patients, including age, gender, frequency of hemodialysis sessions per week, and comorbidity with other chronic diseases. The caregivers were also asked to provide information on their age, gender, marital status, educational level, occupation, annual income, employment relationship, duration as caregivers, relationship with patients, whether cohabitating with the patients, and whether they received caregiver training that aims to educate and support caregivers of patients who undergo hemodialysis. Some of the caregivers reported that they received health education and skills training before providing care for patients.
To comprehensively evaluate the care ability of caregivers, the Chinese version of the Caregiver Task Inventory (CTI) was used in this study. A previous study found that the Chinese version of the CTI had satisfactory psychometric properties and was a relevant and culturally appropriate research instrument for measuring the needs of Chinese family caregivers [22]. This scale is a 25-item questionnaire with 5 sub-scales. These sub-scales evaluate the care ability of caregiver from multiple dimensions, including: ‘learning to cope with a new role’, ‘providing care according to care-receiver’s needs’, ‘managing own emotional needs’, ‘appraising supportive resources’, and ‘balancing caregiving needs and one’s own needs’. The caregivers were asked to indicate their perceptions for the difficulty of caregiving tasks using a 3-point Likert scoring method: 0 points means not difficult, 1 point means difficult, and 2 points means extremely difficult. The total score of this scale is 50 points. A higher score reflects more difficulty and worse care ability.
Procedures
Two researchers were responsible for the data collection. A face-to-face interview between the researchers and patients and their caregivers was conducted before hemodialysis procedures in the hospital. At the time of participant enrollment, the researchers explained the purpose and significance of the investigation. The researchers also verified beforehand that the procedure was not too onerous and the surveys could be finished in 10–15 min. The questionnaires were given after obtaining the cooperation of participants. Then, another 2 researchers checked the completeness and authenticity of the questionnaires and eliminated invalid questionnaires.
Statistical Analysis
All statistical analyses were performed using SPSS software version 25.0 (IBM Corporation; United States). The scores of the Caregiver Task Inventory (CTI) were continuous variables approximately normally distributed, which were described using means and standard deviation (SD). Descriptive statistics for categorical variables were presented using frequencies and percentages. The relationships between sociodemographic factors and CTI scores of caregivers were evaluated by univariate linear regression analyses. Variables with the value of P<0.05 were accepted as candidates for multivariate linear regression analysis to identify the independent factors associated with the care ability of caregivers. The independent samples t test was used to compare the CTI scores in different groups. We considered P<0.05 to be statistically significant.
Results
General Characteristics
This study included a total of 271 hemodialysis patients and their primary caregivers, selected based on the pre-determined inclusion and exclusion criteria. The CTI scores for these caregivers were 36.63±6.48. Table 1 shows the sociodemographic characteristics of these study participants. The mean age was 54.88±10.73 years for the patients and 44.68±15.22 years for the caregivers. Among the 271 hemodialysis patients, 59.04% were male. Apart from ESKD, 60.15% of patients had another chronic disease, such as hypertension and diabetes mellitus. Most of them underwent hemodialysis 3 times per week (73.80%). Of the caregivers, 54.24% were male. The relationships between caregivers and patients were as follows: 31.37% were partners, 33.94% were children, and 34.69% were identified as ‘other’. We found that 75.65% of caregivers provided care without remuneration and 46.86% lived with patients. Most (68.27%) caregivers had a high school education level or below, and 57.20% of them did not undergo formal caregiving training. Of the caregivers, about half were employed. Only 7.75% earned an annual income over 200 000 Chinese yuan (CNY), 17.71% earned 100 000 to 200 000 CNY, 35.42% earned 50 000 to 100 000 CNY, and the remaining 39.12% earned less than 50 000 CNY annually. The frequency of hemodialysis in patients with ESKD was determined by their physicians according to several factors, including residual kidney function, comorbidities, nutritional status, quality of life, and preferences. Most (73.80%) underwent hemodialysis 3 times a week and the rest (26.20%) underwent hemodialysis twice a week.
Table 1.
Sociodemographic characteristics and CTI scores.
| Variables | n | % | CTI scores mean±SD |
|---|---|---|---|
| Age of caregiver (y) | 271 | 100.00 | 44.68±15.22 |
| Age of patient (y) | 271 | 100.00 | 54.88±10.73 |
| Gender of caregiver | |||
| Male | 147 | 54.24 | 38.41±5.73 |
| Female | 124 | 45.76 | 34.52±6.71 |
| Gender of patient | |||
| Male | 160 | 59.04 | 36.13±6.81 |
| Female | 111 | 40.96 | 37.37±5.93 |
| Relation between caregiver and patient | |||
| Partner | 85 | 31.37 | 35.95±5.83 |
| Child | 92 | 33.94 | 36.18±6.20 |
| Other | 94 | 34.69 | 37.69±7.21 |
| Employment relationship | |||
| No | 205 | 75.65 | 36.46±6.12 |
| Yes | 66 | 24.35 | 37.17±7.52 |
| Marital status of caregiver | |||
| Unmarried | 49 | 18.08 | 38.04±6.67 |
| Married | 135 | 49.82 | 36.45±5.95 |
| Other | 87 | 32.10 | 36.13±7.11 |
| Cohabitation with patient | |||
| No | 144 | 53.14 | 39.98±5.04 |
| Yes | 127 | 46.86 | 32.84±5.83 |
| Time as a caregiver (y) | |||
| <1 | 75 | 27.68 | 36.79±7.40 |
| 1~3 | 80 | 29.52 | 36.63±6.59 |
| >3 | 116 | 42.80 | 36.54±5.80 |
| Educational level of caregiver | |||
| High school or lower | 185 | 68.27 | 37.20±5.93 |
| University degree or higher | 86 | 31.73 | 35.42±7.43 |
| Occupation of caregiver | |||
| No | 136 | 50.18 | 36.07±6.91 |
| Yes | 135 | 49.82 | 37.20±5.99 |
| Annual income of caregiver (CNY) | |||
| Less than 50k | 106 | 39.12 | 39.29±5.35 |
| 50k~100k | 96 | 35.42 | 37.33±5.08 |
| 100k~200k | 48 | 17.71 | 31.73±6.06 |
| More than 200k | 21 | 7.75 | 31.24±8.95 |
| Received caregiving training | |||
| No | 155 | 57.20 | 38.77±5.46 |
| Yes | 116 | 42.80 | 33.78±6.66 |
| Times of hemodialysis per week for patient | |||
| Twice | 71 | 26.20 | 36.49±6.76 |
| Thrice | 200 | 73.80 | 36.69±6.40 |
| Patient has other concurrent chronic diseases | |||
| No | 108 | 39.85 | 34.19±7.05 |
| Yes | 163 | 60.15 | 38.26±5.52 |
Univariate Regression Analyses of Factors Associated with Care Ability
Based on the results of univariate linear regression analysis (Table 2), no correlations were found between the care ability of caregiver and various factors, including patient age (P=0.068) and caregiver age (P=0.478), patient gender (P=0.120), relationship between caregiver and patient (P=0.069), employment relationship (P=0.444), marital status of caregiver (P=0.127), the duration as caregiver (P=0.803), occupation of caregiver (P=0.153), and frequency of hemodialysis per week for patients (P=0.831). However, associations were found between the care ability of caregiver and caregiver gender (β=−3.891, P<0.001), educational level (β=−1.781, P=0.035), annual income (β=−3.138, P<0.001), cohabitation with patient (β=−7.137 P<0.001), receipt of caregiving training (β=−4.998, P<0.001), and presence of concurrent chronic diseases in the patient (β=4.088, P<0.001).
Table 2.
Univariate linear regression analysis of factors and CTI scores of caregivers.
| Variables | β | Standard error | Standardized β | t | P value |
|---|---|---|---|---|---|
| Age of caregiver (y) | −0.018 | 0.026 | −0.043 | −0.710 | 0.478 |
| Age of patient (y) | −0.067 | 0.037 | −0.111 | −1.833 | 0.068 |
| Gender of caregiver | −3.891 | 0.756 | −0.300 | −5.149 | <0.001 |
| Gender of patient | 1.244 | 0.799 | 0.095 | 1.558 | 0.120 |
| Relation between caregiver and patient | 0.880 | 0.483 | 0.110 | 1.923 | 0.069 |
| Employment relationship | 0.703 | 0.918 | 0.047 | 0.766 | 0.444 |
| Marital status of caregiver | −0.866 | 0.566 | −0.093 | −1.53 | 0.127 |
| Cohabitation with patient | −7.137 | 0.660 | −0.550 | −10.810 | <0.001 |
| Time as a caregiver (y) | −0.119 | 0.478 | −0.015 | −0.249 | 0.803 |
| Educational level of caregiver | −1.781 | 0.841 | −0.128 | −2.119 | 0.035 |
| Occupation of caregiver | 1.126 | 0.786 | 0.087 | 1.433 | 0.153 |
| Annual income of caregiver (Yuan) | −3.138 | 0.376 | −0.454 | −8.346 | <0.001 |
| Receive caregiving training | −4.998 | 0.737 | −0.382 | −6.783 | <0.001 |
| Hemodialysis sessions per week for patient | 0.192 | 0.897 | 0.013 | 0.214 | 0.831 |
| Patient has other concurrent chronic diseases | 4.088 | 0.766 | 0.309 | 5.334 | <0.001 |
β – regression coefficients; Standardized β – standardized regression coefficients.
Multivariate Regression Analysis of the Factors Associated with Care Ability
The results of multivariate regression analysis are shown in Table 3. Caregiver gender (standardized β=−0.140, P=0.002), cohabitation with patient (standardized β=−0.381, P<0.001), annual income (standardized β=−0.281, P<0.001), receipt of caregiving training (standardized β=−0.183, P<0.001), and the presence of concurrent chronic diseases in the patient (standardized β=0.200, P<0.001) were independent factors associated with the care ability of caregivers. The adjusted coefficient of determination R2 for this multivariate regression analysis was 0.506.
Table 3.
Multiple linear regression analysis of factors and CTI scores of caregivers.
| Variables | β | Standard error | Standardized β | t | P value |
|---|---|---|---|---|---|
| Gender of caregiver | −1.823 | 0.573 | −0.140 | −3.181 | 0.002 |
| Cohabitation with patient | −4.936 | 0.597 | −0.381 | −8.273 | <0.001 |
| Educational level of caregiver | −0.689 | 0.602 | −0.050 | −1.144 | 0.254 |
| Annual income of caregiver (Yuan) | −1.942 | 0.311 | −0.281 | −6.241 | <0.001 |
| Received caregiving training | −2.397 | 0.590 | −0.183 | −4.061 | <0.001 |
| Patient has other concurrent chronic diseases | 2.639 | 0.580 | 0.200 | 4.553 | <0.001 |
β – regression coefficients; Standardized β – standardized regression coefficients; Adjusted coefficient of determination R2=0.506; Fishers F test F=47.085; P<0.001.
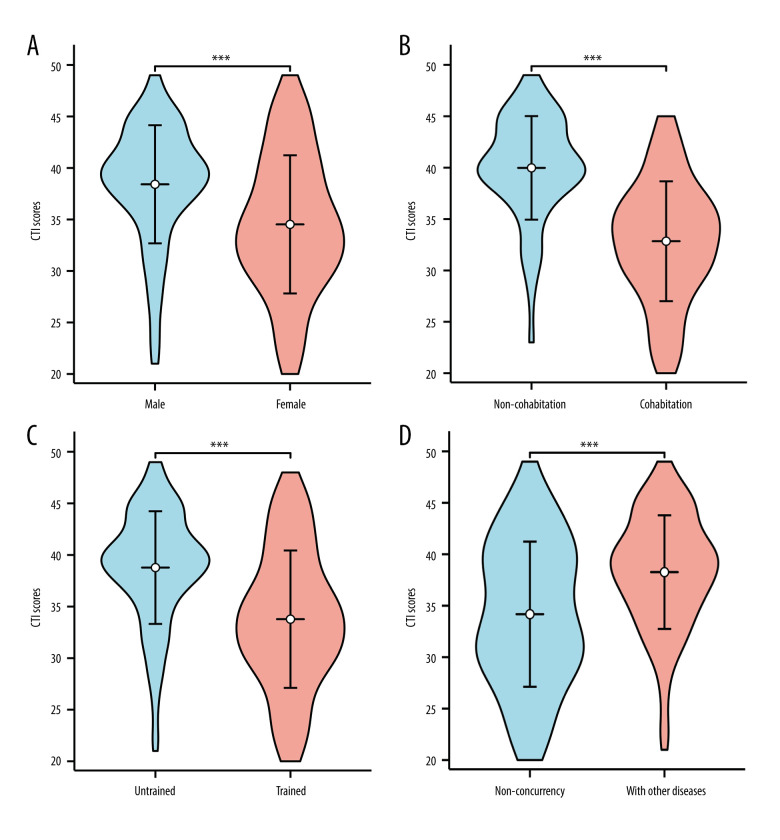
The Comparison of Care Ability in Different Groups
We further investigated the impact of different influencing factors on the caregivers’ care ability. As shown in Figure 1, the CTI scores of female caregivers were lower than for males (P<0.001). The caregivers who lived with patients and received caregiving training had lower CTI scores than those who did not live with patients and did not receive training, respectively (both P<0.001). Caregivers who cared for patients without other chronic diseases had lower CTI scores (P<0.001). CTI scores of the caregivers with annual incomes over 100 000 CNY were lower than those who earned less than 100 000 CNY per year, regardless of whether they were employed or not (both P<0.001) (Figure 2). To sum up, caregivers who were female, lived with patients, earned higher annual income, received caregiving training, and cared for patients without other chronic diseases had better care ability.
Figure 1. Comparison of CTI scores for caregivers in different groups.
(A) Gender of caregivers; (B) Cohabitation with patients; (C) Receive caregiving training or not; (D) Patient concurrent with other chronic diseases or not. *** <0.001. (The figure was created using R software, Version 4.2.3).
Figure 2. The comparison of CTI scores for employed and non-employed caregivers with different annual incomes.
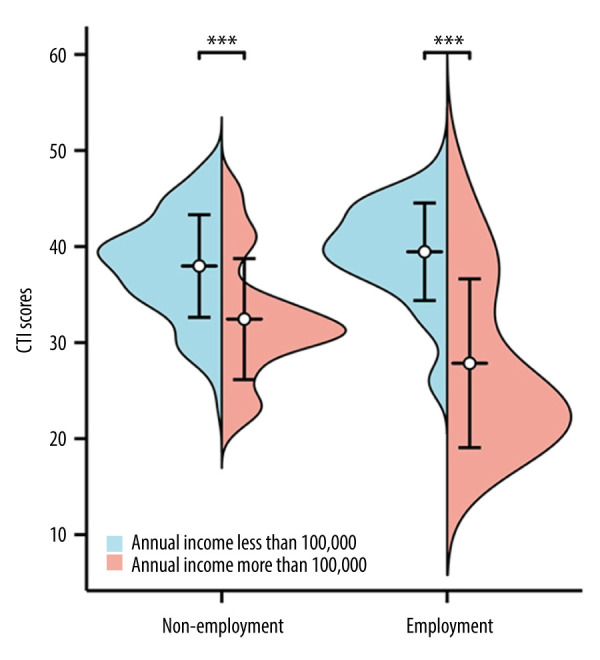
*** <0.001. (The figure was created using R software, Version 4.2.3).
Discussion
Due to the rising incidence of chronic diseases such as diabetes, hypertension, and cardiovascular disease, the population of patients undergoing hemodialysis has been constantly increasing internationally [23]. In China, the incidence of kidney disease requiring dialysis treatment has increased from 2013 to 2017 and is expected to continue rising until 2025 [24]. There are over 500 000 patients receiving hemodialysis in the United States currently. Worldwide, it is projected to reach 5.4 million by 2030 [25].
The global incidence of hemodialysis was 223 per million population in 2017, with the highest rates in Taiwan, Japan, and the United States [26]. According to a study of lifetime and age-conditional risk estimates of ESKD in Japan, the lifetime risk of ESKD requiring dialysis was 3.4% for men and 2.2% for women at age 40 years, and 2.6% for men and 1.6% for women at age 60 years [27]. Patients with ESKD heavily depend on their caregivers because of the effects of long-term hemodialysis [28]. Hence, the care ability of caregivers largely determines the patients’ quality of life. Therefore, it is crucial to explore the factors associated with the care ability of caregivers.
In this cross-sectional study, we found that female caregivers had better care abilities than males. One reason for this is that women have historically and traditionally been expected to take on the caregiver roles, such as caring for children, elderly parents, and sick family members [29], and they may develop better caregiving skills and accumulate experience over time [30]. Additionally, female caregivers may be more considerate and more likely to communicate with patients, so they could provide better physical and emotional support [31]. This helps to provide better care for patients. Moreover, the result of multivariate regression analysis showed that cohabitating with patients was beneficial to improve the care ability of caregivers. This finding was consistent with the conclusion of a nationwide study investigating 44 480 cancer patients in Denmark [32]. They confirmed that cohabitation between caregivers and patients with advanced cancer helped to improve the quality and continuity of care. Cohabitating with patients, the caregivers could provide care around the clock and communicate with patients in a timely manner [33]. This ensured a better understanding of the patient’s needs and improved the quality of care [34].
Our study also showed that the annual income of caregiver was an independent influence factor of the care ability. The CTI scores of those caregivers with annual incomes over 100 000 CNY were lower than those earned less than 100 000 CNY per year, regardless of whether they were employed or not. Lower CTI score indicates better care ability. Our finding suggested that the caregivers with higher annual incomes had better care abilities. For caregivers who have formal employment relationships with patients, higher annual incomes are indicative of greater experience in providing care. It is indisputable that caregivers with higher annual incomes possess better care abilities. Those unemployed caregivers, such as the partners or children of patients, may have better care abilities because they are supported by higher incomes that provide more financial resources. To be specific, higher incomes may allow those caregivers to afford better health care, nutrition, education, and other resources that can improve their own health and well-being, as well as the health and well-being of the patients. These resources enabled them to better meet the needs of patients under their care [35]. Hemodialysis is a long-term treatment and is required several times per week. The cost of hemodialysis and transportation increases the economic burden of the patients and their families [36]. Additionally, hemodialysis patients usually have various comorbidities, which adds to the cost of healthcare [37]. To provide better safeguards and care to patients undergoing hemodialysis and ease their economic burden, the government should strengthen medical insurance and its coverage [38]. Reducing the costs of hemodialysis treatment though improving the effectiveness and quality is also critical [8].
Another factor associated with the care ability indicated in our study is whether the caregivers had received caregiving training or not. In addition to daily activities, caregivers also need to help manage the complications and chronic diseases of hemodialysis patients [39]. To provide better care, caregivers must have relevant medical knowledge about hemodialysis and nursing care. Receiving caregiving training can help patients and their caregivers better understand the disease and remember medical advice at various stages of the illness and management, which helps to improve a patient’s self-management capacity and the caregiver’s care ability [40]. Moreover, it also can exert intervention effects on the self-efficacy and preparedness of caregivers to fulfill their roles and release their depression, anxiety, and burdens [41]. Therefore, it may be beneficial to offer pertinent training to those caring for hemodialysis patients.
Our study stands out from others by specifically targeting caregivers of hemodialysis patients and being the first to investigate the factors associated with their caregiving abilities. However, a few limitations cannot be ignored. Firstly, his was a cross-sectional study, and further longitudinal study is needed to investigate the cause and effect of various factors and the care ability of caregivers. Secondly, we recruited all participants from a single hospital, which may have affected the representativeness and universality of the samples. A multicenter study with larger sample size is needed to verify the reliability of our conclusions. Some of our patients underwent hemodialysis twice a week. The frequency was determined by their nephrologists according to the patient’s residual kidney function, comorbidities, nutritional status, quality of life, and preferences. Patients receiving hemodialysis twice a week may have personal preferences or logistical constraints that make it difficult to attend 3 dialysis sessions per week.
Conclusions
In conclusion, the care ability of caregiver for hemodialysis patient was independently associated with the co-occurrence of other chronic diseases, caregiver annual income, and whether the caregiver lived with the patient and had received caregiving training. These findings may help to develop better medical insurance and nursing interventions for these vulnerable patients, which could markedly alleviate caregiver burden and enhance patient quality of life.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Ethics Approval and Consent to Participate
Ethics approval was granted from the Ethics Committee of Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences (China). The approval number was KY-N-2021-008-02. Written informed consent was obtained from each patient prior to participating in this study.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: This research was funded by Nursing Scientific Research Foundation of Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, grant number DFJH2021015
References
- 1.Loo YX, Yan S, Low LL. Caregiver burden and its prevalence, measurement scales, predictive fa ctors and impact: A review with an Asian perspective. Singapore Med J. 2022;63(10):593–603. doi: 10.11622/smedj.2021033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Utz RL, Warner EL. Caregiver burden among diverse caregivers. Cancer. 2022;128(10):1904–6. doi: 10.1002/cncr.34171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griva K, Goh CS, Kang WCA, et al. Quality of life and emotional distress in patients and burden in caregivers: A comparison between assisted peritoneal dialysis and self-care peritoneal dialysis. Quality of life research: An international journal of quality of life aspects of treatment, care and rehabilitation. 2016;25(2):373–84. doi: 10.1007/s11136-015-1074-8. [DOI] [PubMed] [Google Scholar]
- 4.Sun V, Raz DJ, Kim JY. Caring for the informal cancer caregiver. Curr Opin Suppor Palliat Care. 2019;13(3):238–42. doi: 10.1097/SPC.0000000000000438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaitonde DY, Cook DL, Rivera IM. Chronic kidney disease: Detection and evaluation. Am Fam Physician. 2017;96(12):776–83. [PubMed] [Google Scholar]
- 6.Wouk N. End-stage renal disease: Medical management. Am Fam Physician. 2021;104(5):493–99. [PubMed] [Google Scholar]
- 7.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2019 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis. 2020 Jan;75(1 Suppl 1):A6–A7. doi: 10.1053/j.ajkd.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Liyanage T, Ninomiya T, Jha V, et al. Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet. 2015;385(9981):1975–82. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 9.Ma SJ, Wang WJ, Tang M, et al. Mental health status and quality of life in patients with end-stage renal disease undergoing maintenance hemodialysis. Ann Palliat Med. 2021;10(6):6112–21. doi: 10.21037/apm-20-2211. [DOI] [PubMed] [Google Scholar]
- 10.Hong Z, Zhuang Y, Lu J, et al. Economic evaluation of three dialysis methods in patients with end-stage renal disease in China. Int Urol Nephrol. 2022;55(5):1247–54. doi: 10.1007/s11255-022-03402-2. [DOI] [PubMed] [Google Scholar]
- 11.Hiramatsu T, Okumura S, Asano Y, et al. Quality of life and emotional distress in peritoneal dialysis and hemodialysis patients. Therapeutic apheresis and dialysis: Official peer-reviewed journal of the International Society for Apheresis, the Japanese Society for Apheresis, the Japanese Society for Dialysis Therapy. 2020;24(4):366–72. doi: 10.1111/1744-9987.13450. [DOI] [PubMed] [Google Scholar]
- 12.Himmelfarb J, Ikizler TA. Hemodialysis. N Engl J Med. 2010;363(19):1833–45. doi: 10.1056/NEJMra0902710. [DOI] [PubMed] [Google Scholar]
- 13.Hargrove N, El Tobgy N, Zhou O, et al. Effect of aerobic exercise on dialysis-related symptoms in individuals undergoing maintenance hemodialysis: A systematic review and meta-analysis of clinical trials. Clin J Am Soc Nephrol. 2021;16(4):560–74. doi: 10.2215/CJN.15080920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zazzeroni L, Pasquinelli G, Nanni E, et al. Comparison of quality of life in patients undergoing hemodialysis and peritoneal dialysis: A systematic review and meta-analysis. Kidney Blood Press Res. 2017;42(4):717–27. doi: 10.1159/000484115. [DOI] [PubMed] [Google Scholar]
- 15.Bossola M, Pepe G, Antocicco M, et al. Interdialytic weight gain and educational/cognitive, counseling/behavioral and psychological/affective interventions in patients on chronic hemodialysis: A systematic review and meta-analysis. J Nephrol. 2022;35(8):1973–83. doi: 10.1007/s40620-022-01450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hejazi SS, Hosseini M, Ebadi A, et al. Components of quality of life in hemodialysis patients from family caregivers’ perspective: a qualitative study. BMC Nephrol. 2021;22(1):379. doi: 10.1186/s12882-021-02584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walker RC, Hanson CS, Palmer SC, et al. Patient and caregiver perspectives on home hemodialysis: A systematic review. Am J Kidney Dis. 2015;65(3):451–63. doi: 10.1053/j.ajkd.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Gilbertson EL, Krishnasamy R, Foote C, et al. Burden of care and quality of life among caregivers for adults receiving maintenance dialysis: A systematic review. Am J Kidney Dis. 2019;73(3):332–43. doi: 10.1053/j.ajkd.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Cheng HY, Chair SY, Chau JPC. Effectiveness of a strength-oriented psychoeducation on caregiving competence, problem-solving abilities, psychosocial outcomes and physical health among family caregiver of stroke survivors: A randomised controlled trial. Int J Nurs Stud. 2018;87:84–93. doi: 10.1016/j.ijnurstu.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Bayly M, Morgan D, Elliot V, et al. Does early-stage intervention improve caregiver well-being or their ability to provide care to persons with mild dementia or mild cognitive impairment? A systematic review and meta-analysis. Psychol Aging. 2021;36(7):834–54. doi: 10.1037/pag0000642. [DOI] [PubMed] [Google Scholar]
- 21.Leykum LK, Penney LS, Dang S, et al. Recommendations to improve health outcomes through recognizing and supporting caregivers. J Gen Intern Med. 2022;37(5):1265–69. doi: 10.1007/s11606-021-07247-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee RLT, Mok ESB. Evaluation of the psychometric properties of a modified Chinese versio n of the Caregiver Task Inventory – refinement and psychometric testing of the Chinese Caregiver Task Inventory: A confirmatory factor analys is. J Clin Nurs. 2011;20(23–24):3452–62. doi: 10.1111/j.1365-2702.2011.03729.x. [DOI] [PubMed] [Google Scholar]
- 23.Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: Global dimension and perspectives. Lancet. 2013;382(9888):260–72. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 24.Yang C, Yang Z, Wang J, et al. Estimation of prevalence of kidney disease treated with dialysis in China: A study of insurance claims data. Am J Kidney Dis. 2021;77(6):889–897e1. doi: 10.1053/j.ajkd.2020.11.021. [DOI] [PubMed] [Google Scholar]
- 25.Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709–33. doi: 10.1016/S0140-6736(20)30045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bello AK, Okpechi IG, Osman MA, et al. Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. 2022;18(6):378–95. doi: 10.1038/s41581-022-00542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wakasugi M, Narita I. Lifetime and age-conditional risk estimates of end-stage kidney disease requiring maintenance dialysis in Japan. Clin Exp Nephrol. 2020;24(6):518–25. doi: 10.1007/s10157-020-01860-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown EA, Zhao J, McCullough K, et al. Burden of kidney disease, health-related quality of life, and employment among patients receiving peritoneal dialysis and in-center hemodialysis: Findings from the DOPPS program. Am J Kidney Dis. 2021;78(4):489–500e1. doi: 10.1053/j.ajkd.2021.02.327. [DOI] [PubMed] [Google Scholar]
- 29.DePasquale N, Polenick CA, Davis KD, et al. The psychosocial implications of managing work and family caregiving roles: Gender differences among information technology professionals. J Fam Issues. 2017;38(11):1495–519. doi: 10.1177/0192513X15584680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pilarz AR. Mothers’ work schedule inflexibility and children’s behavior problems. J Fam Issues. 2021;42(6):1258–84. doi: 10.1177/0192513x20940761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ryvicker M, Barrón Y, Shah S, et al. Clinical and demographic profiles of home care patients with Alzheimer’s disease and related dementias: Implications for information transfer across care settings. J Appl Gerontol. 2022;41(2):534–44. doi: 10.1177/0733464821999225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adsersen M, Thygesen LC, Neergaard MA, et al. Cohabitation status influenced admittance to specialized palliative care for cancer patients: A nationwide study from the Danish Palliative Care Database. J Palliat Med. 2019;22(2):164–72. doi: 10.1089/jpm.2018.0201. [DOI] [PubMed] [Google Scholar]
- 33.Humber MB, Yefimova M, Lessios AS, et al. “It Isn’t the Same”: Experiences of informal caregivers of older adults enrolled in a home-based senior care program during COVID-19. J Gerontol Nurs. 2023;49(3):19–26. doi: 10.3928/00989134-20230209-04. [DOI] [PubMed] [Google Scholar]
- 34.Aranda MP, Kremer IN, Hinton L, et al. Impact of dementia: Health disparities, population trends, care interventions, and economic costs. J Am Geriatr Soc. 2021;69(7):1774–83. doi: 10.1111/jgs.17345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Panruti RV, Liebig PS, Duvvuru J. Gerontology in India. Gerontologist. 2015;55(6):894–900. doi: 10.1093/geront/gnv022. [DOI] [PubMed] [Google Scholar]
- 36.Kassa DA, Mekonnen S, Kebede A, Haile TG. Cost of hemodialysis treatment and associated factors among end-stage renal disease patients at the tertiary hospitals of Addis Ababa City and Amhara Region, Ethiopia. Clinicoecon Outcomes Res. 2020;12:399–409. doi: 10.2147/CEOR.S256947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morfin JA, Fluck RJ, Weinhandl ED, et al. Intensive hemodialysis and treatment complications and tolerability. Am J Kdney Dis. 2016 Nov;68(5s1):S43–S50. doi: 10.1053/j.ajkd.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 38.Ranasinghe P, Perera YS, Makarim MF, et al. The costs in provision of haemodialysis in a developing country: A multi-centered study. BMC Nephrol. 2011;12:42. doi: 10.1186/1471-2369-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pépin M, Ferreira AC, Arici M, et al. Cognitive disorders in patients with chronic kidney disease: specificities of clinical assessment. Nephrol Dial Transplant. 2021;37(Suppl 2):ii23–ii32. doi: 10.1093/ndt/gfab262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Figueiredo AE, Bernardini J, Bowes E, et al. A syllabus for teaching peritoneal dialysis to patients and caregivers. Perit Dial Int. 2016;36(6):592–605. doi: 10.3747/pdi.2015.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hendrix CC, Bailey DE, Jr, Steinhauser KE, et al. Effects of enhanced caregiver training program on cancer caregiver’s self-efficacy, preparedness, and psychological well-being. Support Care Cancer. 2016;24(1):327–36. doi: 10.1007/s00520-015-2797-3. [DOI] [PMC free article] [PubMed] [Google Scholar]