Abstract
Despite improvements in the safety of surgical procedures, leaving a foreign object in a patient’s body is still one of the complications of surgical procedures. The literature lacks an analysis of the effectiveness of specific diagnostic tests in detecting foreign objects. The authors present a discussion of the effectiveness of selected techniques and examples of the appearance of foreign bodies in radiological images based on the description of 10 cases. Leaving surgical haemostatic material in the abdominal or pelvic cavity is an underestimated phenomenon that poses a serious diagnostic problem. Computed tomography is the most sensitive method for detecting a foreign body, while a chest or abdominal X-ray is the simplest and most effective way to identify the surgical material. Ultrasound, although widely available, has not shown utility in diagnosing foreign bodies in our cases. Awareness of this problem is necessary to avoid unnecessary mortality in surgical patients.
Keywords: gossypiboma, textiloma, retained surgical items, computed tomography, ultrasonography
Introduction
Gossypiboma or textiloma are terms used to describe a foreign-body reaction to a cotton surgical material that was accidentally retained in a patient’s body.
The incident of leaving a foreign body in the surgical field occurs with a frequency of 0.001% to as high as 0.1% per single surgery [1,2]. The true number of cases remains underestimated, and these incidents are rarely reported because they reflect badly on the reputation of the operator and the surgical department. Soft foreign bodies, such as gauze or surgical sponges, are the items most commonly left behind (90%). It is much rarer to find so-called hard foreign bodies, i.e. instruments, needles, or drains [1,3]. Symptoms in patients with a surgical sponge left behind are nonspecific and are not the basis for making a correct diagnosis. In patients presenting with complaints, an ultrasound is typically performed, the usefulness of which in detecting a foreign body is limited. Further dia-gnostics involving computed tomography (CT) scanning should theoretically enable a definitive diagnosis to be established. However, there are sometimes difficulties in interpreting the lesions detected by CT in patients with a foreign body left behind.
Case series
The study analysed 10 cases of foreign bodies left in the abdomen and pelvis during gynaecological and surgical operations and discussed the radiological images of the left materials (Table 2). Data on hospitalizations, the imaging examinations performed, and the radiological images themselves were obtained from medical records provided to the Department of Forensic Medicine at the Pomeranian Medical University from 2008 to 2020. The types of surgical procedures, age of patients, time of detection, and symptoms presented are shown in Table 1. The aim of our study was to analyse errors made during the interpretation of imaging studies when a foreign body was left in the form of gossypiboma. This topic has been extensively described in the literature, but our goal was to verify theoretical assumptions with practical results.
Table 2.
Characteristics of foreign bodies seen in ultrasonography
| Echogenicity | Measurement (mm) | Acoustic shadow | Fluid collections | Diagnosis |
|---|---|---|---|---|
| Hyperechoic, nonhomogenous | 64 × 54 | + | – | Foreign body/tumour |
| Hyperechoic | 60 × 54 | + | + | Abscess/inflamed intestinal loop |
| Hypoechoic, nonhomogeneous | 40 × 14 | – | + | Ovarian cyst |
| Nonhomogenous with hypoechoic capsule | 67 × 44 | + | + | Haematoma |
| Homogenous, hyperechoic | 100 × 100 | + | – | Ovarian cyst |
| Hypoechoic | 85 × 0 | + | + | Abscess/haematoma |
| Nonhomogeneous | 50 × 40 | – | + | Tumour of sigmoid/abscess |
| Hyperechoic | 65 × 120 | + | – | Ovary inflammation |
| Nonhomogenous | 50 × 50 | – | + | Haematoma |
Caption: + presence of the feature, – absence of the feature
Table 1.
Characteristics of patients and type of procedures performed
| Patient | Sex | Age (years) | Primary surgery | Time elapsed from surgery to detection of foreign body (days) | Main clinical manifestation | Imaging that detected a foreign body |
|---|---|---|---|---|---|---|
| 1 | M | 71 | Prostatectomy | 177 | Mechanical obstruction | CT |
| 2 | F | 30 | Myomectomy | 139 | Abnormal discharge, diffuse abdominal pain |
CT |
| 3 | F | 68 | Abscess drainage | 211 | Lower abdominal pain, diarrhoea | CT |
| 4 | F | 48 | Unilateral adnexectomy | 117 | Fever, urinary tract infections | CT |
| 5 | F | 30 | Caesarean section | 2564 | Asymptomatic | Abdominal X-ray |
| 6 | M | 47 | Hemicolectomy | 2315 | Recurrent fevers | Excreted spontaneously |
| 7 | F | 53 | Hysterectomy with adnexectomy | 364 | Lower abdominal pain | CT |
| 8 | F | 49 | Myomectomy | 760 | Urinary incontinence | CT |
| 9 | M | 61 | Cholecystectomy | 211 | Pain in the right upper quadrant | Chest X-ray, CT |
| 10 | F | 84 | Myomectomy with adnexectomy | 84 | Abdominal shell asymmetry, diffuse abdominal pain | Abdominal X-ray |
Results
The analysis included 7 women (70%) and 3 men (30%), the average age of the patients was 50.5 ± 13.8 years (range 30 to 84), and the time from leaving the foreign body until it was detected was 694 days on average (range 84 days to 7 years and 7 days). In 9 patients, the foreign body was evacuated during a secondary laparotomy, and in one case it was excreted with faeces after previous intra-abdominal migration into the intestinal lumen. A total of 45 imaging studies were performed in the analysed patients, including 25 ultrasounds, 11 CT scans, 7 RTGs, one PET scan, and one MRI.
Ultrasound
Ultrasound was the most frequently performed imaging among the cases analysed while showing the lowest sensitivity in detecting a foreign body, at 4%. Out of 25 exa-minations performed, the suspicion of a foreign body was raised only once. On examination, the gossypiboma in the patient’s body was most often described as a heterogeneous, well-demarcated structure with a hypoechoic capsule giving a strong acoustic shadow. The average dimensions of the described foreign body were 66.8 × 49 mm (range from 40 × 14 mm to 100 × 120 mm). In most cases gossypiboma was distinguished as a fluid reservoir, the most common diagnoses being haematoma, abscess, or cyst in the case of bodies left in the lower quadrants of the abdomen. Nearly half of the doctors performing the examination saw an inflammatory infiltrate near the foreign body, describing inflammation and thickening of the wall of structures such as the fallopian tube or large intestine. About 15% of the exami-nations performed described a small amount of free fluid in the abdominal cavity. In 4 cases a suspicion of a tumour was raised, recognizing the dressing material as a solid lesion. None of the studies performed described vascular flows in the mass of the observed tumour – this symptom can be considered the most typical for a foreign body.
Computed tomography
Computed tomography was the second most frequently performed examination. Out of 11 performed scans, the diagnosis of a foreign body was made in 8 cases, which gives a sensitivity of 73%. The gossypiboma was most often described as a spherical structure of low density and heterogeneous structure located close to the anterior abdominal wall. The average size of the described structure was 83 × 89 × 80 mm. The most distinctive feature was the presence of a radiopaque marker inside the retained surgical item (Figures 3-5), visible as a hyperintense metallic foreign body forming circular folds. The presence of the radiopaque marker was described in 7 cases, it was unnoticed in one case, and in 3 it was not visible in the CT scan. The second most frequent observation was gas bubbles trapped in a folded material forming a characteristic spongiform pattern (Figures 3 and 4); for gossypiboma, it was noted in 8 out of 10 examinations. Only the connective tissue capsule surrounding the foreign body was contrast enhanced. In 5 cases, calcifications were described on the outer part of the mass. The characteristics of the foreign body in CT are presented in Table 3.
Figure 3.

Axial CT scan reveals inhomogenous mass with characteristic spongiform pattern
Figure 5.

Axial abdominal CT scan. A round mass next to left iliac bone with air bubbles is visible. High density whirling structure corresponds to radiopaque marker
Figure 4.

Axial CT scan. Visible gossypiboma with preserved parts of radiopaque marker
Table 3.
Characteristics of foreign bodies seen in computed tomography
| Homogenic structure | Measurements AP, RL, CC (mm) | Contrast capsule enhancement | Presence of air bubbles (spongiform pattern) | Presence of radiopaque marker |
Suspicion of a foreign body |
|---|---|---|---|---|---|
| – | 30 × 100 × 30 | + | + | + | + |
| + | 110 × 90 × 70 | – | + | – | – |
| – | 69 × 104 × 73 | + | + | + | + |
| – | 122 × 94 × 163 | + | + | – | – |
| – | 60 × 60 × 60 | – | + | + | + |
| 0 | 67 × 77 × 77 | – | + | + | + |
| + | 0 | + | – | + | + |
| 0 | 90 × 90 × 90 | – | + | – | – |
| – | 40 × 90 × 50 | + | – | + | + |
| – | 78 × 54 × 65 | – | + | + | + |
X-ray
Retrospective analysis showed that 8 X-rays were taken in the described patients. In 3 cases, the radiologist describing the radiograph correctly suggested the presence of a foreign body in the abdominal cavity. Gossypiboma was not correctly diagnosed in 2 cases. The other 3 imaging scans did not cover the area with the foreign body. The feature that directed the radiologists describing the examination to the diagnosis was a delicate, threadlike shadow with metallic saturation (Figures 1 and 2). Two foreign bodies developed calcifications within the foreign body, creating characteristic shading. An additional observation was the dilatation of the intestinal tract proximal to the foreign body, which may suggest partial mechanical obstruction caused by pressure on the intestinal wall.
Figure 1.

Chest X-ray. Thin metallic shadow is visible in left subcostal space
Figure 2.
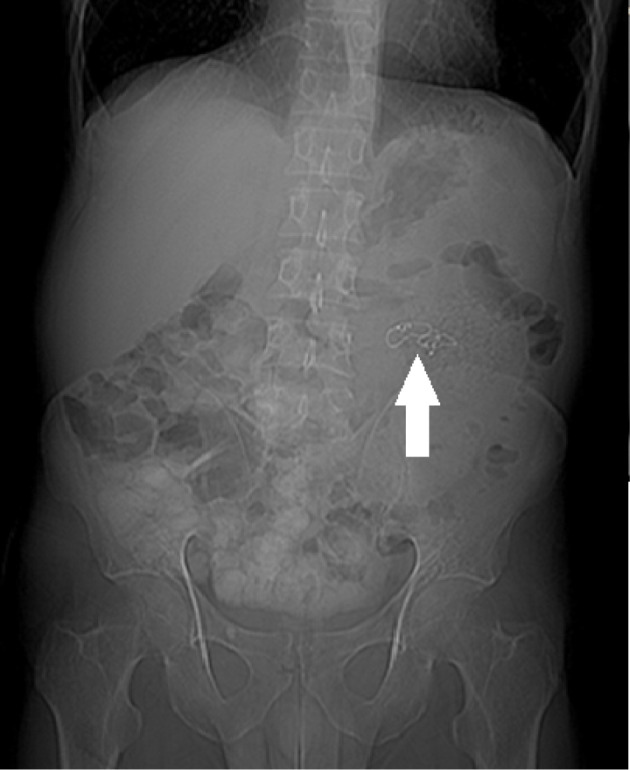
Scout scan, raqiopaque marker visible that corresponds to the foreign body
MRI/PET
MRI was performed once in the analysed cases. A welldefined, heterogeneous, cystic structure has been described. The capsule was enhanced after contrast administration. In the T1/T2 images, a protein-rich fluid was visible inside the lesion. A haemolyzed haematoma or abscess was suspected. In the PET examination, the person describing the images noticed a foreign body but considered it to be a deliberately left clip or a mechanical suture. Increased fludeoxyglucose uptake was described in the vicinity of the surgical material, which was consistent with the inflammation process.
Discussion
Leaving surgical material in the form of a towel or gauze pad is a rare but potentially fatal complication of surgery. The actual scale of the phenomenon remains underestimated due to the low reporting rate of this incident and low detectability due to the lack of symptoms in some patients.
An overlooked foreign body during surgery is referred to in medicine as a never event – a serious incident that is entirely preventable because guidance or safety recommendations providing strong systemic protective barriers are available at a national level and should have been implemented by all healthcare providers [4]. Missing retained surgical items in imaging studies despite obvious indications is classified in the same way – as a medical error. As obvious indications, we can include the image of a characteristic metallic shadow in the case of X-ray imaging, and in the case of computed tomography we can distinguish the appearance of a spongiform or a radiopaque marker, specific for a foreign body. As a matter of fact, these events will continue to occur, and healthcare professionals should be familiar with their recognition and management. The key to patient safety is a quick dia-gnosis and surgery to remove the retained surgical item. Incorrect preoperative diagnosis may lead to unnecessary invasive diagnostic procedures and operations [5]. Unfortunately, a prolonged diagnostic process is associated with a higher risk of complications and an increase in mortality, which can be as high as 35% according to retrospective studies [3,6].
This complication can affect any cavity in the body and all types of procedures. Surgical materials are most often found in the abdominal cavity and pelvis (> 50%), as well as in the chest, spinal canal, or skull [7].
Symptoms presented by patients remain unspecific; most often they include fever, nausea, vomiting, weight loss, and abdominal pain [8,9]. The type and severity of the presented symptoms depend on the body’s reaction to the textile foreign body in the patient’s body. Two possible reactions are known. The most common of them consists of a persistent, moderately intensified inflammatory process during which fibrosis occurs and the formation of granulation tissue together with a connective tissue capsule around the surgical material. In such cases, the symptoms are less severe and result from the presence of a mass in the abdominal cavity; a foreign body in this form can be felt through the abdominal wall as a tumour. Contamination of the material and the formation of an abscess around the dressing material occur less frequently. In this case, the patient will report intermittent fevers more often and inflammatory parameters will be elevated. With this type of inflammatory reaction, the formation of fistulas also occurs, and the time of detection of such a body – due to the rich clinical manifestation – will be faster. One of the rarer complications of leaving the surgical cavity in the patient’s abdominal cavity is spontaneous migration into the intestinal lumen and subsequent partial or complete mechanical obstruction [10,11]. If the gauze enters the intestine above the ileocaecal valve, it is likely to cause obstruction, and if it migrates downstream, it is likely to be excreted spontaneously in the faeces.
Our analysis showed that in most cases the structure of the foreign body was visualized but not correctly identified. Gossypiboma is a rare complication and therefore not included in the standard differential diagnosis. In the case of ultrasound, this difficulty arises from the unfamiliarity with the appearance of the textiloma in this type of imaging. Difficulty also results from the non-specific appearance of the foreign body in the US, its spherical shape, the presence of fluid reservoirs, and the inflammatory infiltration which may suggest a haematoma or tumour. Misdiagnosed X-ray images resulted from incorrect interpretation of the metallic shadows corresponding to the radiopaque marker – they were described as fragments of a surgical anastomosis or sutures. Radiolucent materials also cause diagnostic difficulties in X-ray-based images. Radiologists are often the first physicians to diagnose patients with an unrecognized foreign body.
The specialist in imaging diagnostics must be familiar not only with the appearance of the gossypiboma in individual imaging but also with the risk factors for leaving the surgery material in the patient’s body. Analyses covering large groups of patients have shown that gynaecological operations – in particular caesarean section and hysterectomy – are procedures with a high risk of leaving a foreign body [5]. Other factors predisposing to leave a towel in the abdominal cavity include the occurrence of an unforeseen event during the procedure, emergency surgery, and high BMI of the patient [11,12].
The radiograph should be the basic method of imaging left-over soft foreign bodies. Nowadays all surgical materials must be marked with a radiopaque fragment. In the case of a marker clearly visible on the X-ray (Figures 1 and 2), the diagnosis seems to be certain if the physician describing the examination knows its appearance. Diagnosis becomes more difficult if part of the marker sponge is folded or torn, which happens if the foreign body remains undetected for a long time [13]. The authors point out that vigilance should also be exercised in X-ray examinations with the use of contrast, such as urography, ascending pyelography, or intestinal transit examination. Ultrasonography was the least sensitive in our analysis, but it was the most frequently performed test. The difficulty in recognizing a foreign body in ultrasound is due to the different appearance of the foreign body in this type of imaging. This picture depends on the type of inflammatory reaction and changes with the time spent in the patient’s body. The common features of their appearance in USG is the presence of a strong acoustic shadow, which may be caused by calcifications or gas inside the dressing material. The heterogeneous structure and lack of vascular flows inside the foreign body mass are also characteristic of the US image [8]. Some authors indicate a characteristic zigzag shape inside the described structure, which may correspond to the folds of the material [14,15]. Computed tomography is the best tool to diagnose left foreign bodies and possible complications [16]. It is most often described as a heterogeneous, hypodense mass with a capsule of increased density. The marker takes on the appearance of a metallic body inside the gauze, usually arranged in circular structures. The authors in most cases described the appearance of the sponge as a characteristic spongy pattern caused by the presence of air bubbles [16]. Another observation is the presence of calcifications and contrast enhancement of only the capsule of the described lesion. The material left behind was most often mistaken for an abscess, haematoma, or solid tumour [16,17]. Magnetic resonance imaging is of limited use in diagnosing residual foreign bodies. The main limitation is the inability to see the radiological marker because the radiopaque fragment is not magnetic or paramagnetic. The surgical material was most often described as a soft-tissue oval mass of low density with a thick, reinforcing capsule. In the T1-weighted images, a signal of reduced intensity was described; in the T2-weighted images the foreign body was seen as a hyperintense area [18]. The authors note that the characteristic hypointense bands seen in T2WI corresponding to gauze fibres may only be present in the presence of a foreign body [19].
Study limitations
The collected group of analysed patients is relatively small in relation to the prevalence of the phenomenon. It should be noted that we took into account only the cases of patients who were received by the forensic medicine department of one clinical centre. We believe that further analysis and research are necessary to gain a full picture of this phenomenon.
Conclusions
Postoperative abdominal complaints require detailed diagnostics to exclude the presence of a foreign body.
Ultrasound examination is not sensitive enough in detecting a foreign body.
The decisive test in diagnosing abdominal postoperative complaints should be CT, which also enables the diagnosis of a foreign body and its complications.
Abdominal and thoracic plain X-rays are an underestimated but useful way of detecting a foreign body.
Conflict of interest
The authors report no conflict of interest.
References
- 1.Judson TJ, Howell MD, Guglielmi C, et al. Miscount incidents: a novel approach to exploring risk factors for unintentionally retained surgical items. Jt Comm J Qual Patient Saf 2013; 39: 468-474. [DOI] [PubMed] [Google Scholar]
- 2.Dieng M, Sanoussi Y, Toure AO, et al. Retained surgical sponge after laparotomy: discussion about 8 cases. Surg Chron 2012; 17: 79-82. [Google Scholar]
- 3.Sozutek A, Colak T, Reyhan E, et al. Intra-abdominal gossypiboma revisited: various clinical presentations and treatments of this potential complication. Indian J Surg 2015; 77 (Suppl 3): 1295-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Austin JM, Pronovost PJ. “Never events” and the quest to reduce preventable harm. Jt Comm J Qual Patient Saf 2015; 41: 279-288. [DOI] [PubMed] [Google Scholar]
- 5.Biswas RS, Ganguly S, Saha ML, et al. Gossypiboma and surgeon-current medicolegal aspect–a review. Indian J Surg 2012; 74: 318-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lauwers PR, Van Hee RH. Intraperitoneal gossypibomas: the need to count sponges. World J Surg 2000; 24: 521-527. [DOI] [PubMed] [Google Scholar]
- 7.Gawande AA, Studdert DM, Orav EJ, et al. Risk factors for retained instruments and sponges after surgery. N Engl J Med 2003; 348: 229-235. [DOI] [PubMed] [Google Scholar]
- 8.Birolini DV, Rasslan S, Utiyama EM. Unintentionally retained foreign bodies after surgical procedures. Analysis of 4547 cases. Rev Col Bras Cir 2016; 43: 12-17. [DOI] [PubMed] [Google Scholar]
- 9.Manzella A, Filho PB, Albuquerque E, et al. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol 2009; 193 (6 Suppl): S94-S101. doi: 10.2214/AJR.07.7132. [DOI] [PubMed] [Google Scholar]
- 10.Choi JW, Lee CH, Kim KA, et al. Transmural migration of surgical sponge evacuated by defecation: mimicking an intraperitoneal gossypiboma. Korean J Radiol 2006; 7: 212-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godara R, Marwah S, Karwasra RK, et al. Spontaneous transmural migration of surgical sponges. Asian J Surg 2006; 29: 44-45. [DOI] [PubMed] [Google Scholar]
- 12.Moffatt-Bruce SD, Cook CH, Steinberg SM, Stawicki SP. Risk factors for retained surgical items: a meta-analysis and proposed risk stratification system. J Surg Res 2014; 190: 429-436. [DOI] [PubMed] [Google Scholar]
- 13.Yildirim S, Tarim A, Nursal TZ, et al. Retained surgical sponge (gossypiboma) after intraabdominal or retroperitoneal surgery: 10 cases treated at a single center. Langenbecks Arch Surg 2006; 391: 390-395. [DOI] [PubMed] [Google Scholar]
- 14.Li QY, Wang LX, An NY, Xu H. Sonographic appearances of retained surgical sponges in the abdomen and pelvis. J Clin Ultrasound 2020; 48: 156-159. [DOI] [PubMed] [Google Scholar]
- 15.Mathew RP, Thomas B, Basti RS, Suresh HB. Gossypibomas, a surgeon’s nightmare-patient demographics, risk factors, imaging and how we can prevent it. Br J Radiol 2017; 90: 20160761. doi: 10.1259/bjr.20160761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kokubo T, Itai Y, Ohtomo K, et al. Retained surgical sponges: CT and US appearance. Radiology 1987; 165: 415-418. [DOI] [PubMed] [Google Scholar]
- 17.Cheng TC, Chou AS, Jeng CM, et al. Computed tomography findings of gossypiboma. J Chin Med Assoc 2007; 70: 565-569. [DOI] [PubMed] [Google Scholar]
- 18.Kim CK, Park BK, Ha H. Gossypiboma in abdomen and pelvis: MRI findings in four patients. AJR Am J Roentgenol 2007; 189: 814-817. [DOI] [PubMed] [Google Scholar]
- 19.Lo CP, Hsu CC, Chang TH. Gossypiboma of the leg: MR imaging characteristics. A case report. Korean J Radiol 2003; 4: 191-193. [DOI] [PMC free article] [PubMed] [Google Scholar]


