Abstract
Background:
Smoking cessation interventions are important for decreasing lung cancer mortality rate among Chinese Americans. This study aims to investigate and summarize the intervention methods focusing on smoking cessation among Chinese Americans and to compare the effects of intervention methods on the smoking cessation rates.
Methods:
A systematic review and meta-analysis design was used in this study. Keyword searching was conducted in August 2021 on PubMed, Google Scholar, PsycINFO, and CINAHL. The methodological quality of each study was assessed using the PEDro scale or The Methodological item for non-randomized studies (MINORS). The Review Manager Version 5.4 software was used to conduct the meta-analysis. Random effect model and subgroup analysis were applied in the analysis.
Results:
Twenty and 11 studies were included in the systematic review and meta-analysis, respectively. Of the 20 studies, 8 were randomized control studies, 9 were pre-post single group intervention studies, 1 was retrospective analysis for an intervention study, 1 was a baseline data analysis from a cluster randomized trial, 1 was a feasibility intervention study. Results showed that compared to the control group, the group that received interventions on smoking cessation had a significantly increased smoking cessation rate (OR, 3.76; 95% CI, 1.72-8.21; P=0.0009). Subgroup analysis showed individual-based (OR, 5.88) NRT outreach interventions (OR, 3.80) conducted in person (OR, 2.53) with smokers (OR, 6.64) seemed to be more effective to increase smoking cessation rates among Chinese Americans compared with group-based, telephone counseling, indirect remote interventions conducted among Chinese American smokers and their non-smoke family members.
Conclusions:
Individual-based NRT outreach interventions conducted in person with smokers is an effective way to increase smoking cessation rates among Chinese Americans. More culturally sensitive and effective interventions are needed to help Chinese American smokers to quit smoking.
Key Words: Chinese Americans, intervention, meta-analysis, smoking cessation, systematic review
Introduction
Lung cancer is the leading cause of cancer deaths in Chinese Americans (Gomez et al., 2015). Although studies (Jemal et al., 2009) have shown that incidence rates of lung cancer among Asian Americans have been under-reported, the incidence rates of lung cancer among Asian Americans are still disproportionately high compared with the general U.S. population (Underwood et al., 2012). Chinese Americans have the highest mortality rates of lung cancer among all Asian American subgroups (Association of Community Cancer Centers, 2016). As the second and fourth most common cancer among U.S. Chinese men and women, respectively, lung cancer accounted for approximately 30% of all cancer-related deaths in Chinese Americans (Gomez et al., 2015).
Tobacco use is the most important risk factor of lung cancer, which contributes to 80% of lung cancer death in the United States (American Cancer Society, 2019). Compared to the U.S. general population, the smoking rate among Chinese Americans was relative high, ranging from 17.4% (Yu, Chen, Kim, and Abdulrahim, 2002) to 18% (Shelley et al., 2004) and, much higher in men (29% to 34%) than in women (2% to 4%) (Shelley et al., 2004; Yu et al., 2002), whereas the smoking rate was 15.1% in U.S. adults, 17.5% among U.S. men and 13.5% among U.S. women aged 18 years and older in the United States (Jamal et al., 2016). The primary approach to prevent lung cancer is smoking cessation, which has been proved effectively decreasing the incidence rates of lung cancer among males and females (American Cancer Society, 2019). Population-based studies in Asian have revealed a sharp decrease of lung cancer risk for over 50% in the first 5 to 6 years of smoking cessation (Tse et al., 2011; Wong et al., 2010). The US Preventive Services Task Force recommends long-term smokers to quit smoking for 15 years before their risk of getting lung cancer comparable to non-smokers (U.S. Preventive Services Task Force, 2021).
Smoking cessation interventions are important for decreasing lung cancer mortality rate among Chinese Americans. Although no review study has been reported on the smoking cessation interventions in Chinese Americans, previous studies indicated a paucity of smoking cessation interventions for Asian Americans, which also included Chinese Americans (Doolan and Froelicher, 2006). While a review study conducted in 2003 showed 4 studies had reported smoking cessation interventions in Asian/Pacific Islanders from 1985 to 2001 (Lawrence et al., 2003), a review conducted in 2007 showed that only two clusters of controlled studies and one uncontrolled smoking cessation intervention study focusing on Asian Americans have been published from 1995 to 2005 (Chen et al., 2007). In addition, another review study published in 2011 showed only 3 studies had been conducted on smoking cessation treatment among Asian Americans from 1985 to 2009 (Cox et al., 2011). These studies suggest the need for continued efforts to develop and evaluate the effectiveness of smoking cessation interventions for Asian American populations including Chinese Americans (Lawrence et al., 2003). Further research relevant to the smoking cessation needs of minority populations can enable nurses and other healthcare providers to administer culturally adequate and efficacious smoking cessation interventions to these groups (Doolan and Froelicher, 2006).
The research questions aimed to be answered in this study were two-fold: (1) What intervention methods have been used for increasing smoking cessation rates among Chinese Americans in the past years? and (2) Which intervention methods are effective and how effective are they? The purpose of this systematic review and meta-analysis is to investigate and summarize the intervention methods focusing on smoking cessation among Chinese Americans and to compare the effects of intervention methods on the smoking cessation rates. This study will provide a comprehensive picture of the intervention programs which have been done on smoking cessation for Chinese Americans over the past years. It will also suggest an optimal way to increase smoking cessation rates among Chinese Americans.
Materials and Methods
Search Strategies and Selection Criteria
Keyword searching was conducted in August 2021 on PubMed, Google Scholar, PsycINFO, and CINAHL. Search strategies included [(smoking cessation) OR (quit smoking) OR (tobacco cessation) OR (tobacco quit)] AND (Chinese American*). Inclusion criteria for the studies were: 1) peer-reviewed studies, 2) intervention studies, 3) targeted at Chinese Americans or Asian Americans including data about Chinese American population; and 4) studies with relevant data about smoking cessation outcomes. Exclusion criteria for the studies were: 1) review studies; or 2) not meeting the inclusion criteria.
Guided by the PRISMA literature search process, we checked the titles of the articles first, then the abstracts of the articles were evaluated, and last the text and references of the articles were read further for inclusion and exclusion consideration. The authors of this study did the literature search separately. The initial searching results were compared and discussed among the authors to reach consent. Information on the studies’ designs, settings, samples, interventions, outcomes, and results were entered to the table of evidence by the first author and verified by the second author.
Data Synthesis and Study Quality
We organized the systematic review results into logical categories according to group consensus. The methodological quality of randomized control trial studies was assessed using the PEDro scale (www.pedro.fhs.usyd.edu.au). The methodological quality of the pre and post intervention studies was assessed using The Methodological item for non-randomized studies (MINORS). The agreement between the two assessors was evaluated with the intraclass correlation coefficient (ICC).
The PEDro scale comprises a list of 11 criteria. Each criterion is valued by either 0 (“No) or 1 (“Yes”), with only 10 of them used (item 2 to 11) to calculate the total score, yielding a maximum score of 10 points for each assessed study. The item 1 of the PEDro scale is only used for evaluating the studies’ external validity, but not used for evaluating the intervention studies’ quality, according to the recommendation from the designer of the PEDro scale (www.pedro.fhs.usyd.edu.au). Studies with a score lower than 4 are considered ‘poor’ quality, 4 to 5 are considered ‘fair’, 6 to 8 are considered ‘good’ and 9 to 10 are considered ‘excellent’ (Cashin and McAuley, 2020).
The MINORS tool contains a list of 12 criteria. The first 8 items are applicable for both non-comparative and comparative studies. The last 4 items are appropriate for studies with two or more groups. Every item is scored from 0 to 2, and the total scores over 16 or 24 give an overall quality score.
Data Analysis
The Review Manager Version 5.4 software was used to conduct the meta-analysis. Random effect model and subgroup analysis were applied in the analysis. The Hedge’s g statistic was used, and sample size was weighted. Raw data (e.g., mean with standard deviation) in the studies were converted to percentage. The Tau2 statistic was used to evaluate the included studies’ heterogeneity, and I2 statistic was utilized to reveal the variance among the studies. With a I2 value between 0% and 25%, the studies were considered zero heterogeneity; 25% to 50% was low heterogeneity, 50% to 75% was moderate heterogeneity, and 75%–100% was high heterogeneity (Higgins et al., 2003). We assessed risk of bias within studies according to the PRISMA recommendation using a tool based on Agency for Healthcare Research and Quality guidance (Viswanathan et al., 2012). The first author did the data analysis and the second author reviewed and verified the results.
Results
Study characteristics
The search yielded 20 eligible articles to be included in the review. A detailed searching process could be found in Figure 1. Of the 20 articles reviewed in this study, 8 were randomized control studies (Cummins et al., 2015; Fang et al.,2006; Tong et al., 2018; Wong et al., 2008; Wu et al., 2009; Young et al., 2020; Zhao et al., 2019; Zhu et al., 2012), 9 were pre-post single group intervention studies (Burton et al., 2010; Chen et al., 2021; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Ma et al., 2005; Shelley et al., 2008; Shelley et al., 2010; Tsoh et al., 2015), 1 was retrospective analysis for an intervention study (Chang et al., 2013), 1 was a baseline data analysis from a cluster randomized trial (Daniel et al., 2021), 1 was a feasibility intervention study (Tat et al., 2016). Most of the studies were conducted in New York City. Sample size of the studies ranged from 26 (Ma et al., 2004) to 14073 (Chen et al., 2021). The publication years of the studies ranged from 2004 to 2021. More information about the study characteristics of the included studies can be found in Table 1.
Figure 1.
PRISMA Flow Chart Documenting the Study Selection Process
Table 1.
Study Characteristics of the Included Studies for the Systematic Review
| Citation | Design | Setting | Intervention | Control | Sample for intervention group | Sample for control group | Results for smoking cessation rates (Intervention vs. control) |
|---|---|---|---|---|---|---|---|
| Burton et al. (2010) | Pre-post-test | US | A minimum of 9 proactive phone counseling sessions within a 6-month period for each participant recruited at his worksite All activities were conducted in Chinese languages. |
NA | 101 Chinese Americans participated in the phone-counseling intervention in 2007-2008 75 completing the program with at least 9 counseling calls 56 completing the program at 6-month post end of intervention |
NA | Smoking cessation rate at end of intervention: 53.3% (40/75). Smoking cessation at 6-month post end of intervention: 50% (28/56). |
| Chang et al. (2013) | Retrospective analysis | A public health clinic at San Francisco | Community clinic's smoking cessation counseling program that offered acupuncture, nicotine replacement therapy (NRT) and from 2007 to 2010. Acupuncture + NRT |
Only NRT Only Acupuncture |
88 Chinese Americans | Only NRT: 54 Chinese Americans Only Acupuncture: 68 Chinese Americans |
Tobacco cessation rates at 6 months were relatively high for the acupuncture + NRT group and only acupuncture group (37.7% vs. 28.9%). |
| Chen et al. (2021) | pre-post-test quasi-experimental design | US | Asian Smokers' Quitline, August 2012 to July 2019 | NA | 14,073 nationwide Chinese-, Korean-, and Vietnamese-speaking smokers | NA | No separate data for Chinese American smokers |
| Cummins et al. (2015) | Randomized control trial | US | A multistate cessation quit line from 1/2010-7/2012 A comprehensive session to prepare for quitting and follow-up calls scheduled according to the risk of relapse (i.e., front-loaded). Experienced quit line counselors who were bilingual and bicultural provided the counseling. The self-help materials were also used from the efficacy trial Chinese speakers chose whether to receive booklets with traditional or simplified characters. |
Self-help materials-only | 2277 Chinese- (Mandarin and Cantonese), Korean-, and Vietnamese-speaking smokers . |
No separate data for Chinese American smokers | |
| Daniel et al. (2021) | Baseline data analysis from a cluster randomized trial | Northern California | Family-based healthy lifestyle intervention. Two small group education sessions about “quit Smoking for a Healthy Family” and two individual telephone calls over 2 months. |
The comparison LHWs will receive training about "Healthy Living" focusing on nutrition and physical activity education. Participants will also receive the Smoking Cessation Resource Handout. |
340 Chinese and Vietnamese American male daily smokers | No specific data about smoking cessation rates | |
| Fang et al. (2006) | Randomized control trail | Southeastern Pennsylvania | A theory-based smoking cessation intervention | General health counseling | 19 Chinese American smokers | 17 Chinese American smokers | 1week: 9/19 vs. 3/17; 1 month: 10/19 vs. 4/17; 3 months: 7/19 vs. 5/17. |
| Kwong et al. (2009) | Pre-post single-arm quasi-experimental study | New York City | A culturally and linguistically relevant, physician-led smoking cessation intervention Pharmacological treatments and brief cessation counselling, education and support by the physician and the health educator |
NA | Convenience sample of 115 Chinese American participants (94% male) | NA | Week 12 smoking cessation rates: 13.9%, Sixteen participants successfully quit smoking. |
| Lau et al. (2020) | Pre-post single-arm quasi-experimental study | New York City | A health coach-led smoking cessation program from November 2015 to January 2017 Follow-up was provided face-to-face or over-the-phone to provide support and address barriers. Free nicotine replacement treatment was provided for eligible participants. |
NA | 184 Chinese American participants | NA | 3 month smoking cessation rates: An intent-to-treat analysis found that 19% quit. |
| Citation | Design | Setting | Intervention | Control | Sample for intervention group | Sample for control group | Results for smoking cessation rates (Intervention vs. control) |
| Ma et al. (2004) | A pre-post quasi-experimental research design | Delaware Valley Region of Pennsylvania and New Jersey | A standard smoking cessation curriculum (SC) | A culturally modified program (ACT) | Chinese American male (n = 17) youth smokers, aged 14-19 years n=13 at 3-month follow-up |
Chinese American male (n = 9) youth smokers, aged 14-19 years n=9 at 3-month follow-up |
Post program smoking cessation rates: SC vs. ACT: 22.2% (n=17) vs. 0% (n=9) A 23.1% quit rate for the SC program (n=13) and an 18.2% quit rate for the ACT program (n=9) at 3-month follow-up was achieved. |
| Ma et al. (2005) | A one-group pre-post test | US | Behavioral and nicotine replacement strategies | NA | 43 Korean and Chinese smokers | NA | No separate data for Chinese American smokers. |
| Shelley et al. (2008) | Pre-post-test quasi-experimental design | Two communities in New York City | Tobacco control public policy changes and additional linguistically and culturally specific community-level tobacco control interventions from 2003 to 2005 |
Tobacco control public policy changes | 1165 adults aged 18-74 at the baseline interviews 615 participants from the original cohort completed the follow-up interview |
1372 adults aged 18-74 at the baseline interviews 759 participants from the original cohort completed the follow-up interview |
Baseline: 19.5% out of 1165 vs. 16.9% out of 1372 Follow up: 13.7% out of 615 vs. 13.5% out of 759 |
| Shelley et al. (2010) | Single-group trial | New York City | Tailored free nicotine patch (NRT), July 2004 and May 2005 | NA | 375 Chinese American smokers | NA | 4 months: Respondents only: 42.2% (100/237) Patch user only: 44.7% (98/219) All participants: 26.7% (100/375). |
| Tat et al. (2016) | Feasibility study collecting observational data | California | Mainly staffed by four well-trained, volunteer undergraduates, explained the risks of first- and second-hand tobacco exposure and how to access the Helpline's services. A brochure, provided in English, Chinese, Korean, and Vietnamese (the Helpline's available Asian languages), was used to guide the bicultural, bilingual students' tobacco-related discussions with shoppers. The students' repeated presence at the nine partnering Asian grocery stores served as reminders of the Helpline's availability. |
NA | NA | NA | No specific data about smoking cessation rates |
| Tong et al. (2018) | Randomized controlled trial | San Francisco, California | Moderate-intensity smoke-free-living educational intervention 2 group sessions, a laboratory report of their baseline smoke exposure, as measured by 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL), and 3 follow-up calls over 6 months |
A brief-intensity smoke-free-living educational intervention 1 group session on tobacco-cessation resources |
109 Cantonese-speaking Chinese American smoker and household nonsmoker pairs N=90 at 12 months follow up |
94 Cantonese-speaking Chinese American smoker and household nonsmoker pairs N=102 at 12 months follow up |
Baseline: moderate vs. brief 0/94 vs. 0/109 6 months: moderate vs. brief 19/92 (20.2%) vs. 19/106 (17.4%) 12 months: moderate vs. brief 23/90 (24.5%) vs. 23/102 (21.1%) |
| Tsoh et al. (2015) | Pilot single-group trial | US | Two small group education sessions and two individual telephone calls over 2 months |
NA | 96 dyads (N = 192, 75% Vietnamese) of Chinese or Vietnamese male daily smokers and their family members |
NA | No separate data for Chinese American smokers |
| Wong et al. (2008) | Randomized control trail | San Francisco Bay Area | Physician advice, in-person counseling with nicotine replacement therapy, 5 telephone calls during 2001-2007 |
Physician advice and self-help manual | 464 Chinese American smokers together, no information about the number of the participates allocated to the intervention and control groups. | Feasibility study, no data about the smoking cessation rate | |
| Citation | Design | Setting | Intervention | Control | Sample for intervention group | Sample for control group | Results for smoking cessation rates (Intervention vs. control) |
| Wu et al. (2009) | Randomized control trail | New York City |
4 individualized counselor-led MI sessions and nicotine replacement therapy [NRT] |
4 general health education sessions, self-help materials, and NRT | 60 Chinese American smokers | 62 Chinese American smokers | 1 week: 13.6% vs. 8.2% 1 month: 38.3% vs. 32.3% 3 months: 66.1% vs. 32.3% 6 months: 66.7% vs. 31.7% |
| Young et al. (2020) | Randomized control trail | San Francisco | Weekly WeChat messages for 6 weeks Follow-up surveys were administered via WeChat at 1 and 3 months |
Assessment | n=33 | n=31 | No text information, No specific data about smoking cessation rates |
| Zhao et al. (2019) | Randomized control trail | Washington DC area | Graphic, quit line group A graphic, native language text-messaging intervention Participants were randomly assigned to one of four conditions based on a between-subjects 2 (graphic plus text or text-only messages) * 2 (quit line information or quitting tips) design. The text-messaging intervention included 30 text messages in total and lasted one month. Participants completed an expired air carbon monoxide (CO) assessment and self-reported measures at both baseline and follow-up. |
Text, tips group | First-generation Chinese and Korean male immigrants Graphic =35 Quitline=34 |
First-generation Chinese and Korean male immigrants Text=36 Tips=37 |
No separate data for Chinese American smokers |
| Zhu et al. (2012) | Randomized trial | California | Telephone counseling for smoking cessation from August 2, 2004 and April 4, 2008. Telephone counseling (self-help Materials) and up to six counseling sessions |
Self-help materials only | Counseling = 359 Chinese American smokers | Self-help = 370 Chinese American smokers | 4 months: counseling vs. self-help 7-day abstinence 30.6%. vs. 14.9 7 months: counseling vs. self-help 7-day abstinence 33.4 % vs. 18.9% 6-mo prolonged abstinence: 14.8% vs. 6.0% |
In addition, sixteen of the studies are individual-based studies (Burton et al., 2010; Chang et al., 2013; Chen et al., 2021; Cummins et al., 2015; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2005; Shelley et al., 2010; Tat et al., 2016; Tong et al., 2018; Wu et al., 2009; Wong et al., 2008; Young et al., 2020; Zhao et al., 2019; Zhu et al., 2012) and 4 were group-based studies (Daniel et al., 2021; Ma et al., 2004; Shelley et al., 2008; Tsoh et al., 2015). Interventions in 13 studies were conducted in person (Chang et al., 2013; Daniel et al., 2021; Fang et al.,2006; Kwong et al., 2009; Ma et al., 2004; Ma et al., 2005; Shelley et al., 2008; Shelley et al., 2010; Tat et al., 2016; Tong et al., 2018; Tsoh et al., 2015; Wong et al., 2008; Wu et al., 2009), in 6 studies (Burton et al., 2010; Chen et al., 2021; Cummins et al., 2015; Young et al., 2020; Zhao et al., 2019; Zhu et al., 2012) were conducted in indirect remote methods, and in 1 study (Lau et al., 2020) was conducted either in person or phone counselling methods, depending on participants’ preference. Sixteen studies were smokers-based studies (Burton et al., 2010; Chang et al., 2013; Chen et al., 2021; Cummins et al., 2015; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Ma et al., 2005; Shelley et al., 2010; Tat et al., 2016; Wong et al., 2008; Wu et al., 2009; Young et al., 2020; Zhao et al., 2019; Zhu et al., 2012), 3 were smokers and non-smoke family member dyads-based studies (Daniel et al., 2021; Tong et al., 2018; Tsoh et al., 2015), and 1 was Smokers and physicians-based study (Shelley et al., 2008).
Of the 20 studies, NRT outreach (Burton et al., 2010; Chang et al., 2013; Chen et al., 2021; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2005; Shelley et al., 2008; Shelley et al., 2010; Wu et al., 2009) and the telephone counselling (Burton et al., 2010; Chen et al., 2021; Cummins et al., 2015; Daniel et al., 2021; Lau et al., 2020; Tong et al., 2018; Tsoh et al., 2015; Zhu et al., 2012) methods were the most frequently used interventions. Furthermore, offering health education workshops (Daniel et al., 2021; Shelley et al., 2008; Tat et al., 2016 Tong et al., 2018; Tsoh et al., 2015) and patient counselling (Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Wong et al., 2008; Wu et al., 2009), distributing self-help materials (Cummins et al., 2015; Wu et al., 2009; Zhu et al., 2012), and using patient education curriculum (Ma et al., 2004; Shelley et al., 2008), flip chart (Tsoh et al., 2015), video/audiotapes (Wong et al., 2008) , behavior skill training (Wong et al., 2008), patient navigation (Ma et al., 2005), wechat message (Young et al., 2020), acupuncture (Chang et al., 2013), text-messaging (Zhao et al., 2019), pharmacotherapy (Shelley et al., 2008), and holding quit and win contest (Shelley et al., 2008) were conducted in the studies. More information about the intervention characteristics of the included studies can be found in Table 2.
Table 2.
Intervention Characteristics of the Included Studies for the Systematic Review
| Citation | Intervention methods | Intervention delivery objects | Intervention contact | Intervention types | Intervention focus |
|---|---|---|---|---|---|
| Burton et al., 2010 | Proactive phone-counseling intervention: a minimum of 9 proactive phone counseling sessions within a 6-month period for each participant recruited at his worksite. All activities were conducted in Chinese languages. comparing baseline smoking with smoking 6 months after the intervention ended. Smoking-cessation products (Chinese quit-smoking tea; ginger candy; NRT patch) were free and delivered in person to participants for whom they had been recommended. |
Individual | Indirect remote | Telephone counseling + NRT outreach | Smokers-based |
| Chang et al., 2013 | The intervention consisted of one individual office counseling session, and two group class sessions with options offered for acupuncture treatments and NRT. The self-selected treatment groups were categorized as (a) only acupuncture, (b) only NRT, and (c) acupuncture + NRT. The individual counseling, including in the group class sessions, was conducted by the bilingual, bicultural health education staff. Acupuncture was provided by a Chinese physician with medical acupuncturist training and a licensed acupuncturist. Up to six needles were used in each area, most commonly elbows, knees, and earlobes. For participants who declined acupuncture therapy or were waiting for needle placement, counselors helped them set up a quit plan and strategies for reduction and cessation. All needles were in place within the first 30 minutes; those who received acupuncture first had therapy the longest, but all had therapy for at least 15 minutes. Prescriptions for nicotine patches were offered, and patients were responsible for picking up the medications from their pharmacies. Medication costs were covered by Medi-Cal or the county insurance, which also has a program that provides coverage to uninsured residents. Acupuncture was provided free of charge. |
Individual | In person | Office counseling + acupuncture + NRT outreach | Smokers-based |
| Chen et al., 2021 | Participants received behavioral telephone counseling from counselors fluent in Chinese, Korean, or Vietnamese. Participants also received 2 weeks’ worth of nicotine patches mailed directly to their homes. |
Individual | Indirect remote | Telephone + NRT outreach | Smokers-based |
| Cummins et al., 2015 | Toll-free Asian-language quit line service. The multistate service also used the self-help materials from the efficacy trial, which were designed to motivate smokers to make quit attempts and to teach the skills needed to avoid relapse. Chinese speakers chose whether to receive booklets with traditional or simplified characters. |
Individual | Indirect remote | Telephone counseling + self-help materials | Smokers-based |
| Daniel et al., 2021 | Randomization in one of two family-based educational interventions. Family-based healthy lifestyle intervention: two small group education sessions and two individual telephone calls over 2 months on topic of “Quit Smoking for a Healthy Family”. |
Group | In person | Health education + telephone call follow-up | Smokers and non-smoke family member- dyads based |
| Fang et al.,2006 | A theory-based smoking cessation intervention vs. general health counseling +nicotine replacement therapy one in-person session lasting approximately 90–120 min and targeted cognitive–affective reactions to smoking and cessation. Cultural values and culturally appropriate quitting strategies, such as the importance of familial support, concerns relating to children's health, and having a healthy Asian diet, were employed to assist and encourage participants during their quit attempts. Follow-up assessments were conducted by telephone at one-week, one- month, and three-month post-counseling and assessed health beliefs and smoking status. All study procedures and assessments were conducted in the participant's native language (Korean, Cantonese, or Mandarin). |
Individual | In person | Patient counseling + NRT outreach | Smokers-based |
| Kwong et al., 2009 | A culturally and linguistically relevant, physician-led smoking cessation intervention. Pharmacological treatments and brief cessation counselling, education and support by the physician and the health educator. |
Individual | In person | Office counseling+ NRT outreach | Smokers-based |
| Lau et al., 2020 | A health coach-led smoking cessation program. Follow-up was provided face-to-face or over-the-phone to provide support and address barriers. Free nicotine replacement treatment was provided for eligible participants. |
Individual | In person+ indirect remote | Office counseling/ Telephone + NRT outreach | Smokers-based |
| Ma et al., 2004 | The American Lung Association’s Not on Tobacco (N-O-T) curriculum was selected as the generic curriculum. The study was conducted over a period of 6 weeks during the summer of 2001 and used a pre-post quasi-experimental research design using two related samples. A buddy system was developed, and participants received more monetary rewards if they brought their respective buddies and additional incentives (t-shirts, gift certificates) if they continued to attend the sessions. |
Group | In person | Patient education curriculum | Smokers-based |
| Citation | Intervention methods | Intervention delivery objects | Intervention contact | Intervention types | Intervention focus |
| Ma et al., 2005 | During the intervention, a counselor met with each participant individually for approximately two hours. At the beginning of the session, participants were asked to complete a baseline smoking behavior questionnaire. The intervention was in accordance with current nicotine addiction treatment guidelines. The program was designed to be time-, labor-, and cost-effective, without compromising its efficacy; it entailed smoking cessation advice along with nicotine replacement therapy (NRT). Participants who were interested in the use of NRT were screened for eligibility for nicotine patch use and were provided usage instructions and free patches. These programmatic features were designed especially for underserved and hard-to-reach minority populations. |
Individual | In person | Patient navigation + NRT outreach | Smokers-based |
| Shelley et al., 2008 | Physician education and detailing which included 1) the distribution of “Tool Kits” to 99 physicians in 42 practices; 2) distribution of 305 six-week courses of free nicotine patches through ACS and AAFE; 3) implementation of three free Chinese-language smoking cessation programs that included free pharmacotherapy (one hospital-based and two located in community-based health centers); 4) a quit and win contest (50 participants) and; 5) 13 smoking cessation workshops conducted by ACS (122 attendees). The launch of city-wide tobacco control initiatives sponsored by the NYCDOH. These included a cigarette tax increase of $1.50 per pack, that when combined with the NY State excise tax raised cigarette taxes to $3.00 per pack, and the enactment of the Smoke Free Air Act. NYCDOH also launched a citywide media campaign in English and Spanish, however, they did not distribute a Chinese-language educational campaign during the intervention period. |
Group | In person | NRT outreach + patient education curriculum + pharmacotherapy + quit and win contest + health education | Smokers and physicians-based |
| Shelley et al., 2010 | A 6-week course of the nicotine patch Kits contained a 2-week supply each of generic 21, 14, and 7 mg patches, instruction sheets and a self-help smoking cessation guide. All written materials were provided in Chinese and English. |
Individual | In person | NRT outreach | smokers-based |
| Tat et al., 2016 | The new module, mainly staffed by four well-trained, volunteer undergraduates, explained the risks of first- and second-hand tobacco exposure and how to access the Helpline’s services. A brochure, provided in English, Chinese, Korean, and Vietnamese (the Helpline’s available Asian languages), was used to guide the bi-cultural, bi-lingual students’ tobacco-related discussions with shoppers. The students’ repeated presence at the nine partnering Asian grocery stores served as reminders of the Helpline’s availability. |
Individual | In person | Health-education | Smokers-based |
| Tong et al., 2018 | The moderate-intensity group pairs received two 90-minute educational sessions over 3 months, individual laboratory reports of baseline tobacco exposure, a bilingual booklet that summarized the educational materials and included self-reflection questions, and 3 individual follow-up calls (<15 minutes) over 6 months. The brief-intensity group pairs received 1 hour of education. The educational sessions primarily consisted of PowerPoint presentations and group discussions delivered by the CPHC health educator. All participants received a project magnet with scheduling information. |
Individual | In person | Health education +telephone call | Smokers and household nonsmokers- dyads based |
| Tsoh et al., 2015 | The 2-month SNFF intervention involved LHW outreach to both smokers and families through two small group education sessions with smoker-family dyads (90 minutes each) and two LHW-delivered individual telephone calls (10–15 minutes each) to reinforce progress and provide support. The size of each small group ranged from 2 to 4 dyads. Education sessions involved engaging participants sharing their personal stories, teaching with a flip chart, and setting individual goals using a “Health Family Action Plan.” The flip chart was made of hard laminated cardboard and able to stand on its own base. Bulleted speaking points for the LHW in English, Chinese, and Vietnamese were on one side of each page while the other side had a headline, brief explanatory text, and culturally appropriate graphics. |
Group | In person | Health education + flip chart + telephone call | Smokers and family member dyads-based |
| Wong et al., 2008 | Participants assigned to the minimal intervention group received (a) a strong message to quit smoking from their primary care physician and/or the research nurse, (b) a self-help manual with information on pharmaco-therapies, and (c) a list of smoking cessation programs available in the San Francisco Bay Area. Smokers in the intensive group also received 45-minutes of cognitive behavioral counseling as well as the smoking cessation video and the relaxation audiotapes to view or listen on their own. For those patients who reported less than 75% confidence on the self-efficacy scale to resist smoking during high-risk situations, behavioral skill training was provided. |
Individual | In person | Patient counseling + video/audiotapes +behavior skill training | Smokers-based |
| Citation | Intervention methods | Intervention delivery objects | Intervention contact | Intervention types | Intervention focus |
| Wu et al., 2009 | Adapted MI counseling + self-help smoking cessation materials vs. health education sessions + general health self-help information Intervention consisted of four 60-min in-person sessions of Adapted MI counseling and a packet of self-help smoking cessation materials. The deleterious effects of tobacco use, secondhand smoke, as well as participants’ experiences with smoking were discussed within various cultural contexts as, for example, hosting friends or in business transactions. Additionally, participants were counseled about the addictive nature of nicotine, encouraged to conduct a decisional balance exercise to examine the pros and cons of smoking, and encouraged to contemplate quitting behavior. Participants were provided NRT packs and counseled on their use. |
Individual | In person | Patient counseling + self-help materials + NRT outreach | Smokers-based |
| Young et al., 2020 | WeChat participants received weekly culturally sensitive smoking cessation WeChat messages for 6 weeks. Follow-up surveys were administered via WeChat at 1 and 3 months. This study reports user engagement, satisfaction, knowledge gain and quit attempts at 1- and 3-month follow-up. |
Individual | Indirect remote | Wechat message | Smokers-based |
| Zhao et al., 2019 | The study consisted of a baseline survey and biochemical assessment, a one-month text-messaging intervention and a follow-up survey and another biochemical assessment. Participants received either graphic plus text or text-only health messages depicting the physical and social harms of smoking. They also received either information about an Asian-language Quitline or culturally tailored tips for quitting adapted from an existing smoking cessation text-messaging program, SmokeFreeTXT and its application in China. |
Individual | Indirect remote | Text-messaging | Smokers-based |
| Zhu et al., 2012 | Smokers in the counseling group received telephone counseling in addition to the self-help materials. | Individual | Indirect remote | Telephone counseling + self-help materials | Smokers-based |
Study Quality
Of the 20 eligible papers, 11 studies were included in the meta-analysis. Among the 4 studies evaluated by PEDro scale, two were good quality trials (Tong et al., 2018; Zhu et al., 2012), and two were fair quality trials (Fang et al., 2006; Wu et al., 2009). Among the 7 studies evaluated by MINORS, the scores for the quality evaluation ranged from 12 (Burton et al., 2010; Kwong et al., 2009; Lau et al., 2020; Shelley et al., 2008; Shelley et al., 2010) to 20 (Chang et al., 2003) with one study (Ma et al., 2004) having a score of 14. The score of each individual study’s quality constituted the average value of the scores given by the two assessors. The ICC was 0.88 (95% CI: 0.47–0.99). Details about the study quality evaluation was shown in Tables 3 and 4.
Table 3.
Methodological Quality Measurement of the Included RCT Studies (PEDro Scale)
| PEDro items | No. Studies | References |
|---|---|---|
| Random allocation | 4 | Fang et al., 2006; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012 |
| Concealed allocation | 2 | Tong et al., 2018; Zhu et al., 2012 |
| Baseline comparability | 4 | Fang et al., 2006; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012 |
| Blinding of participants | 0 | 0 |
| Blinding of therapists | 0 | 0 |
| Blinding of assessors | 0 | 0 |
| Adequate follow-up (> 85%) | 3 | Fang et al., 2006; Tong et al., 2018; Wu et al., 2009 |
| Intention-to-treat analysis | 2 | Tong et al., 2018; Zhu et al., 2012 |
| Between-group statistical comparisons | 4 | Fang et al., 2006; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012 |
| Reporting of point measures and measures of variability | 4 | Fang et al., 2006; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012 |
Table 4.
Methodological Quality Measurement of the Included Pre and Post Intervention Studies
| MINORS items | Reported and adequate |
|---|---|
| A clearly stated aim | Burton et al., 2010; Chang et al., 2003; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Inclusion of consecutive patients | Burton et al., 2010; Chang et al., 2003; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Prospective collection of data | Burton et al., 2010; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Endpoints appropriate to the aim of the study | Burton et al., 2010; Chang et al., 2003; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Unbiased assessment of the study endpoint | Burton et al., 2010; Chang et al., 2003; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Follow-up period appropriate to the aim of the study | Burton et al., 2010; Chang et al., 2003; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010 |
| Loss to follow up less than 5% | Chang et al., 2003; Ma et al., 2004 |
| Prospective calculation of the study size | 0 |
| An adequate control group* | Chang et al., 2003 |
| Contemporary groups* | Chang et al., 2003 |
| Baseline equivalence of groups* | Chang et al., 2003 |
| Adequate statistical analyses* | Chang et al., 2003 |
*Only applicable to the quasi-experimental study with a control group.
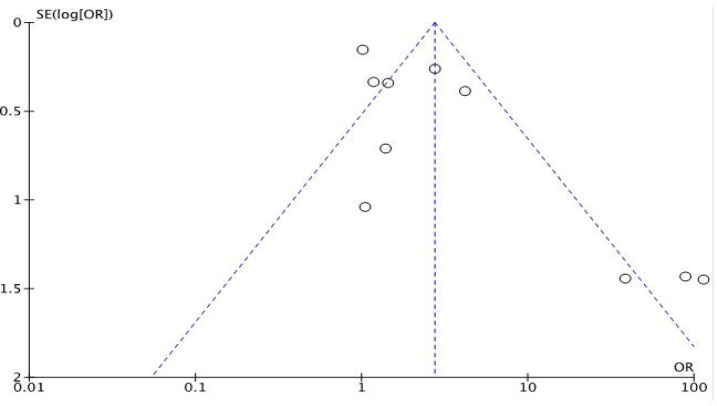
Publication Bias
For the outcome of interest, funnel plot (Figure 2) was generated for evaluation of publication bias. The distribution of data points provided limited evidence for small study publication bias.
Figure 2.
Funnel Plots of Interventions’ Effect on Participants’ Smoking Cessation Rates. OR, Odds ratio, SE, standard error; log, logarithm
Meta-Analysis of the Smoking Cessation Interventions
Total effect
Of the 20 studies which tested the effects of interventions on participants’ smoking cessation rates, nine studies (Chen et al., 2021; Cummins et al., 2015; Daniel et al., 2021; Ma et al., 2005; Tat et al., 2016; Tsoh et al., 2015; Wong et al., 2008; Young et al., 2020; Zhao et al., 2019) were not included in the meta-analysis due to lacking data on the smoking cessation rate among Chinese American participants. Results showed that compared to the control group, the group that received interventions on smoking cessation had a significantly increased smoking cessation rate. The pooled summary effect of the interventions included was 3.76 times higher in comparison to the control (OR, 3.76; 95% CI, 1.72-8.21; P=0.0009). However, a high heterogeneity was noticed across the study results (Tau2=1.16, ChI2=77.85, df =10, P<0.00001, I2 = 87%) (Figure 3).
Figure 3.
Forest Plot of the Interventions’ Effect on Participants’ Smoking Cessation Rates
Subgroup Analysis
Individual- vs. group- based interventions
Of the 11 included studies which tested effects of the interventions on Chinese American participants’ smoking cessation rates (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012), nine studies were individual-based intervention studies (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012) and two studies were group-based intervention studies (Ma et al., 2004; Shelley et al., 2008). Results showed that compared to the control group, the individual-based interventions significantly increased participants’ smoking cessation rates. The pooled summary effect of the included individual-based interventions was 5.88 times higher compared to the control (OR, 5.88; 95% CI, 2.20-15.74; P=0.0004); the same effect was noticed on the group-based interventions; however, the increase was not significant (OR, 1.02; 95% CI, 0.75-1.39; P=0.90). With subgroup analysis, the heterogeneity across the studies decreased both among individual-based studies (Tau2=1.57, ChI2=58.87, df = 8, p<0.00001, I2 = 86%) and group-based studies (Tau2=0.00, ChI2=0.00, df = 1, p=0.98, I2 = 0%) (Figure 4).
Figure 4.
Forest Plot of the Interventions’ Effects on Participants’ Smoking Cessation Rates Individual-based vs. Group-based Interventions
NRT outreach vs. telephone counselling interventions
Of the 11 included studies which tested effects of the interventions on Chinese American participants’ smoking cessation rates (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012), six studies were NRT outreach-based intervention studies (Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Shelley et al., 2008; Shelley et al., 2010; Wu et al., 2009) and two studies were telephone counseling-based intervention studies (Tong et al., 2018; Zhu et al., 2012). Results showed that compared to the control group, the NRT outreach-based interventions significantly increased participants’ smoking cessation rates. The pooled summary effect of the included NRT outreach-based interventions was 3.80 times higher compared to the control (OR, 3.80; 95% CI, 1.19-12.10; P=0.02); the same effect was noticed on the telephone counseling-based interventions; however, the increase was not significant (OR, 1.84; 95% CI, 0.81-4.21; P=0.15). Although with subgroup analysis, the heterogeneity slightly increased across the NRT outreach-based studies (Tau2=1.56, ChI2=49.15, df = 5, p<0.00001, I2 = 90%), the heterogeneity decreased across the telephone counseling-based studies (Tau2=0.26, ChI2=3.85, df =1, p=0.05, I2 = 74%) (Figure 5).
Figure 5.
Forest Plot of the Interventions’ Effects on Participants’ Smoking Cessation Rates NRT Outreach vs. Telephone Counselling Interventions
In person vs. indirect remote interventions
Of the 11 included studies which tested effects of the interventions on Chinese American participants’ smoking cessation rates (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012), eight studies were in person-based intervention studies (Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009] and two studies were indirect remote-based intervention studies (Burton et al., 2010; Zhu et al., 2012). Results showed that compared to the control group, the in person-based interventions significantly increased participants’ smoking cessation rates. The pooled summary effect of the included in person-based interventions was 2.53 times higher compared to the control (OR, 2.53; 95% CI, 1.09-5.88; P=0.03); the same effect was noticed on the group-based interventions; however, the increase was not significant (OR, 14.08; 95% CI, 0.26-764.39; P=0.19). Although with subgroup analysis, the heterogeneity slightly increased across the indirect remote-based studies (Tau2=7.35, ChI2=7.81, df = 1, p=0.005, I2 = 87%), the heterogeneity didn’t change across the in person-based studies (Tau2=1.01, ChI2=48.47, df = 7, p<0.00001, I2 = 86%) (Figure 6).
Figure 6.
Forest Plot of the Interventions’ Effects on Participants’ Smoking Cessation Rates in Person vs. Indirect Remote Interventions
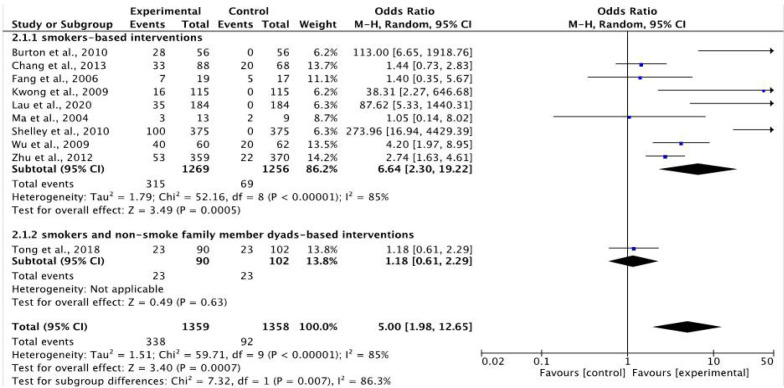
Smokers based vs. smokers and non-smoke family member dyads-based interventions
Of the 11 included studies which tested effects of the interventions on Chinese American participants’ smoking cessation rates (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2008; Shelley et al., 2010; Tong et al., 2018; Wu et al., 2009; Zhu et al., 2012), nine studies were smokers-based intervention studies (Burton et al., 2010; Chang et al., 2013; Fang et al.,2006; Kwong et al., 2009; Lau et al., 2020; Ma et al., 2004; Shelley et al., 2010; Wu et al., 2009; Zhu et al., 2012) and one studies was smokers and non-smoke family member dyads-based intervention studie (Tong et al., 2018). Results showed that compared to the control group, the smokers-based interventions on smoking cessation significantly increased participants’ smoking cessation rates. The pooled summary effect of the included smokers-based interventions was 6.64 times higher compared to the control (OR, 6.64; 95% CI, 2.30-19.22; P=0.0005); the same effect was noticed on the smokers and non-smoke family member dyads-based interventions; however, the increase was not significant (OR, 1.18; 95% CI, 0.61-2.29; P=0.63). With subgroup analysis, the heterogeneity slightly decreased across the smokers-based studies (Tau2=1.79, ChI2=52.16, df = 8, p<0.00001, I2 = 85%) (Figure 7).
Figure 7.
Forest Plot of the Interventions’ Effects on Participants’ Smoking Cessation Rates Smokers based vs. Smokers and Non-Smoke Family Member Dyads-based Interventions
Discussion
This study examined the effects of smoking cessation Interventions for Chinese American smokers to quit smoking. Results showed that compared to the control group, the group that received interventions on smoking cessation had a significantly increased smoking cessation rate (OR, 3.76; 95% CI, 1.72-8.21; P=0.0009). Furthermore, subgroup analysis showed individual-based (OR, 5.88) NRT outreach interventions (OR, 3.80) conducted in person (OR, 2.53) with smokers (OR, 6.64) seemed to be more effective to increase smoking cessation rates among Chinese Americans compared with group-based, telephone counseling, indirect remote interventions conducted among Chinese American smokers and their non-smoke family members. This is the first study testing smoking cessation interventions’ effects on Chinese American smokers quit smoking rate. Findings from this study could help to inform the design of efficient approaches to increase smoking cessation rates among Chinese American smokers.
Utilizing appropriate intervention methods to increase smoking cessation rates among Chinese American smokers is necessary. First, an individual-based smoking cessation intervention can help to bring personal-targeted culturally sensitive intervention content to individual Chinese American smoker. It can help them to overcome the barriers which they face during their smoking cessation process. Based on the individual targeted interventions, approaches such as individual motivational interview, personal counseling with smoking cessation experts, and one-on-one smoking cessation collaborator could be used to help Chinese American smokers to quit smoking. Second, NRT outreach can help to provide necessary tobacco substitutes to addicted Chinese American smokers, which can help them to suffer less from the withdraw effect of quit smoking. In recent years, using NRT outreach as the main method to help smokers to quit smoking and assisting with the telephone counseling to facilitate the usage of NRT products is the trend to be used in smoking cessation projects (Fu et al., 2016). Third, in person interventions could help to build a close rapport between smokers and interveners. In person interventions which happen face to face can help smokers get familiar with the interveners easier and faster. Also, interactions between smokers and interveners could be facilitated through various methods conducted in person, such as role play intervention games, counseling with paper-based materials’ assistance, introduction of a smoking cessation buddy, etc.
Last, smokers-based interventions seemed more effective for smokers to quit smoking than interventions focusing on both smokers and their non-smoke family members. This finding answered the concern which raised by Hubbard et al., (2016) in their systematic review study, which stated that most studies did not assess the influence of family involvement in the interventions on smoking behavior, because there was no direct study comparing a family-based smoking cessation intervention with an individual-based smoking cessation intervention. In our study, results showed the family involvement in the smoking cessation interventions was not effective as it would be. In addition, compared with interventions focusing on family-based smoking cessation interventions, results in this study showed that interventions focusing on smokers were more effective for them to quit smoking, however, previous studies showed that no differences existed between smokers-based and family-based smoking cessation interventions. In the study conducted by McBride et al., (2004), the intent-to-treat analyses showed no significant difference was found at any follow-up time among the three female smoker groups (usual care, female smokers only, or partner-assisted groups) regarding the reports of abstinence. McIntyre-Kingsolver et al., (1986) also found that no significant differences between spouse involved intervention and smoker-based intervention on the smoking cessation rates due to spouse training at any assessment point. Same result was found in Nyborg and Nevid’s (1986) study, which showed that although abstinence posttreatment was more frequent among couples in therapist-administered treatment, no significant differences were noticed between couples and individual training approaches.
Possible reasons for family-based smoking cessation interventions not being effective as smokers-based interventions may derive from: 1) more difficulties existing in the family-based training, and 2) challenges to get mutual support during the smoking cessation maintenance period. First, compared with smokers-based interventions, family-based interventions required more work to be done to be effective. Intervention plans which are specifically designed for smokers’ non-smoke family members are needed to increase family support. Accordingly, extra staff support and cost related to the non-smoker family members interventions are required. Second, although interventions are implemented aiming to increase family support for Chinese American smokers to quit smoking, sometimes, it may turn out to be ineffective and unhelpful for them to quit smoking. For example, knowing the harm of secondhand smoking, Chinese American smokers’ family members may blame the smokers for smoking instead of supporting them to quit. Thus, techniques directed at enhancing social support during the maintenance period need to be explored in working with smoking family members (Nyborg and Nevid, 1986).
As a systematic review and meta-analysis study, this research has some limitations. First, as noticed in the funnel plot, outliners are distributed at the bottom of the plot, this may indicate some systematic bias related to the publication bias. Like it was mentioned in other research (Murad et al., 2018), studies with significant results, published in English language, published quickly, and cited frequently are more likely to be found in the data search process. Accordingly, they are more likely to be included in the systematic review and meta-analysis. This may lead to the publication bias which further impacts the data analysis results. Second, some studies included in this study had a not sufficient PEDro score or MINORS score, which means the quality of the studies are fair. This may impact the meta-analysis result. However, since few studies had been conducted on Chinese American smokers’ smoking cessation, and a small sample size was noticed in the subgroup analysis, excluding those studies could result in sample bias in the analysis. Thus, the insufficient strength of evidence included in this review should not be interpreted as evidence that the interventions are not effective but, rather, as encouragement for additional research before effectiveness can be established.
In conclusions, this study examined the effects of smoking cessation interventions on Chinese American smokers quit smoking rates. Results showed that compared to the control group, the group that received interventions on smoking cessation had a significantly increased smoking cessation rate. Furthermore, subgroup analysis showed individual-based, NRT outreach interventions conducted in person with smokers seemed to be effective. This study provided evidence for health care providers to design appropriate and effective smoking cessation interventions to be used in Chinese American smokers. More culturally sensitive and effective interventions are needed to help Chinese American smokers to quit smoking.
Author Contribution Statement
Fang Lei, Conceptualization, methodology, writing-original draft preparation; Ying Zheng, methodology, writing-review and editing.
Acknowledgements
Ethics approval
This systematic review and meta-analysis study was waived ethics approval by the IRB.
Availability of data
All data are available on PubMed, Google Scholar, PsycINFO, and CINAHL
Conflict of interest
The authors declare no conflict of interest.
References
- American Cancer Society. Lung Cancer Risk Factors. 2019. Retrieved January 08, 2022, from https://www.cancer.org/cancer/lung-cancer/causes-risks-prevention/risk-factors.html.
- Association of Community Cancer Centers. Understanding and Improving Lung Cancer Treatment in Asian Americans and Pacific Islanders in the Community Setting. Rockville, MD: Association of Community Cancer Centers. 2016. Retrieved January 08, 2022, from: https://www.accc-cancer.org/docs/projects/resources/pdf/LungCancerTools/aapi-whitepaper.
- Burton D, Zeng XX, Chiu CH, et al. A phone-counseling smoking-cessation intervention for male Chinese restaurant workers. J Community Health. 2010;35:579–85. doi: 10.1007/s10900-010-9244-7. [DOI] [PubMed] [Google Scholar]
- Cashin AG, McAuley, JH Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother. 2020;66:59. doi: 10.1016/j.jphys.2019.08.005. [DOI] [PubMed] [Google Scholar]
- Chang E, Fung LC, Li CS, et al. Offering acupuncture as an adjunct for tobacco cessation: a community clinic experience. Health Promot Pract. 2013;14:80–7. doi: 10.1177/1524839913485756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Anderson CM, Babb SD, et al. Evaluation of the Asian Smokers’ Quitline: A Centralized Service for a Dispersed Population. Am J Prev Med. 2021;60:154–62. doi: 10.1016/j.amepre.2020.01.033. [DOI] [PubMed] [Google Scholar]
- Chen MS, Tang H. Review of smoking cessation research among Asian Americans: The state of the research. N TR. 2007;9:485–93. doi: 10.1080/14622200701587052. [DOI] [PubMed] [Google Scholar]
- Cox LS, Okuyemi K, Choi WS, Ahluwalia JS. A review of tobacco use treatments in U S ethnic minority populations. Am J Health Promot. 2011;25:11–30. doi: 10.4278/ajhp.100610-LIT-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins SE, Wong S, Bonnevie E, et al. A Multistate Asian-Language Tobacco Quitline: Addressing a Disparity in Access to Care. Am J Public Health. 2015;105:2150–5. doi: 10.2105/AJPH.2014.302418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel JA, Kim-Mozeleski JE, Poudel KC, et al. Family support and readiness to consider smoking cessation among Chinese and Vietnamese American male smokers. J Smok Cessat. 2021:6678219. doi: 10.1155/2021/6678219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doolan DM, Froelicher ES. Efficacy of smoking cessation intervention among special populations: review of the literature from 2000 to 2005. Nurs Res. 2006;55:29–37. doi: 10.1097/00006199-200607001-00005. [DOI] [PubMed] [Google Scholar]
- Fang CY, Ma GX, Miller SM, et al. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43:321–4. doi: 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Ferketich AK, Wewers ME, Shek A, et al. Development and Evaluation of a Physician- led Smoking Cessation Intervention for Low-income Chinese Americans. J Smok Cessat. 2009;4:92–8. [Google Scholar]
- Fu SS, van Ryn M, Nelson D, et al. Proactive tobacco treatment offering free nicotine replacement therapy and telephone counselling for socioeconomically disadvantaged smokers: a randomized clinical trial. Thorax. 2016;71:446–53. doi: 10.1136/thoraxjnl-2015-207904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez SL, Yang J, Lin SW, et al. Incidence trends of lung cancer by immigration status among Chinese Americans. Cancer Epidemiol Biomarkers Prev. 2015;24:1157–64. doi: 10.1158/1055-9965.EPI-15-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta- analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard G, Gorely T, Ozakinci G, Polson R, Forbat L. A systematic review and narrative summary of family-based smoking cessation interventions to help adults quit smoking. BMC Fam Pract. 2016;17:73. doi: 10.1186/s12875-016-0457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Phillips E, Gentzke AS, et al. Current Cigarette Smoking Among Adults – United States, 2016. MMWR. 2018;67:53–9. doi: 10.15585/mmwr.mm6702a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–49. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- Lau J, Feldman N, Lee R, Xu A, Oster A. A health coach-led smoking cessation program for Chinese Americans at a community health center in New York City. J Smok Cessat. 2020;15:128–35. [Google Scholar]
- Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in U racial/ethnic minority populations: an assessment of the literature. Prev Med. 2003;36:204–16. doi: 10.1016/s0091-7435(02)00023-3. [DOI] [PubMed] [Google Scholar]
- Ma GX, Fang C, Steven SE, et al. A Culturally Enhanced Smoking Cessation Study among Chinese and Korean Smokers. Int Electron J Health Educ. 2005;v8:1–10. [Google Scholar]
- Ma GX, Shive SE, Tan Y, Thomas P, Man VL. Development of a culturally appropriate smoking cessation program for Chinese American youth. J Adolesc Health. 2004;35:206–16. doi: 10.1016/j.jadohealth.2003.09.013. [DOI] [PubMed] [Google Scholar]
- McBride CM, Baucom DH, Peterson BL, et al. Prenatal and postpartum smoking abstinence a partner-assisted approach. Am J Prev Med. 2004;27:232–8. doi: 10.1016/j.amepre.2004.06.005. [DOI] [PubMed] [Google Scholar]
- McIntyre-Kingsolver K, Lichtenstein E, Mermelstein RJ. Spouse training in a multicomponent smoking-cessation program. Behav Ther. 1986;17:67–74. [Google Scholar]
- Murad MH, Chu H, Lin L, Wang Z. The effect of publication bias magnitude and direction on the certainty in evidence. BMJ Evid based Med. 2018;23:84–6. doi: 10.1136/bmjebm-2018-110891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyborg KF, Nevid JS. Couples who smoke: A comparison of couples training versus individual training for smoking cessation. Behav Ther. 1986;17:620–5. [Google Scholar]
- Shelley D, Fahs M, Scheinmann R, et al. Acculturation and Tobacco Use Among Chinese Americans. Am J Public Health. 2004;94:300–7. doi: 10.2105/ajph.94.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelley D, Fahs M, Yerneni R, et al. Effectiveness of tobacco control among Chinese Americans: a comparative analysis of policy approaches versus community-based programs. Prev Med. 2008;47:530–6. doi: 10.1016/j.ypmed.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelley D, Nguyen N, Peng CH, et al. Increasing access to evidence-based smoking cessation treatment: effectiveness of a free nicotine patch program among Chinese immigrants. J Immigr Minor Health. 2010;12:198–205. doi: 10.1007/s10903-008-9194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tat J, Nguy M, Tong EK, et al. Disseminating tobacco control information to Asians and Pacific Islanders. J Cancer Educ. 2015;30:26–30. doi: 10.1007/s13187-014-0695-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong EK, Saw A, Fung LC, at al. Impact of a smoke-free-living educational intervention for smokers and household nonsmokers: A randomized trial of Chinese American pairs. Cancer. 2018;124:1590–8. doi: 10.1002/cncr.31115. [DOI] [PubMed] [Google Scholar]
- Tse LA, Yu IT, Qiu H, at al. Lung cancer decreased sharply in first 5 years after smoking cessation in Chinese men. J Thorac Oncol. 2011;6:1670–6. doi: 10.1097/JTO.0b013e3182217bd4. [DOI] [PubMed] [Google Scholar]
- Tsoh JY, Burke NJ, Gildengorin G, et al. A Social Network Family-Focused Intervention to Promote Smoking Cessation in Chinese and Vietnamese American Male Smokers: A Feasibility Study. N TR. 2015;17:1029–38. doi: 10.1093/ntr/ntv088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood JM, Townsend JS, Tai E, et al. Racial and regional disparities in lung cancer incidence. Cancer. 2012;118:1910–8. doi: 10.1002/cncr.26479. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Lung Cancer: Screening. 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening .
- Wong CC, Tsoh JY, Tong EKH, et al. The Chinese community smoking cessation project: a community sensitive intervention trial. J Community Health. 2008;33:363–73. doi: 10.1007/s10900-008-9114-8. [DOI] [PubMed] [Google Scholar]
- Wong KY, Seow A, Koh WP, et al. Smoking cessation and lung cancer risk in an Asian population: findings from the Singapore Chinese Health Study. Br J Cancer. 2010;103:1093–6. doi: 10.1038/sj.bjc.6605782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu D, Ma GX, Zhou K, et al. The effect of a culturally tailored smoking cessation for Chinese American smokers. N TR. 2009;11:1448–57. doi: 10.1093/ntr/ntp159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu ES, Chen EH, Kim KK, Abdulrahim S. Smoking among Chinese Americans: behavior, knowledge, and beliefs. Am J Public Health. 2002;92:1007–12. doi: 10.2105/ajph.92.6.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao XQ, Peterson EB, Oh KM, Cai XM. Using graphic text-messaging to promote smoking cessation among first-generation Chinese and Korean male immigrants. Health Educ Res. 2019;34:332–44. doi: 10.1093/her/cyz006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu SH, Cummins SE, Wong S, et al. The effects of a multilingual telephone quitline for Asian smokers: a randomized controlled trial. J Natl Cancer Inst. 2012;104:299–310. doi: 10.1093/jnci/djr530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available on PubMed, Google Scholar, PsycINFO, and CINAHL