Abstract
Angiomyolipoma is a benign solid renal neoplasm. A giant angiomyolipoma is more than 10cm by size, but it can grow to huge proportions. Our case appears to be the third largest angiomyolipoma and the largest among bilateral giant renal angiomyolipoma in the indexed literature. A 26-year-old man presented with large right abdominal swelling for the past three years, which was occupying his right flank and iliac region, extending beyond the midline. Computed tomography of the abdomen revealed a large well-defined mass in the right side of the abdomen, crossing the midline and measuring 35 × 20 × 12cm. The left kidney showed a similar fatty lesion of 14 × 6cm. The findings were consistent with angiomyolipoma. Further evaluation for tuberous sclerosis by magnetic resonance imaging the brain demonstrated multiple subependymal nodules. Giant renal angiomyolipoma is an uncommon tumour with bilateral giant angiomyolipoma being a rare entity. Preoperative embolisation helps in reducing size of the tumour. In case of giant and bilateral angiomyolipoma, evaluation for tuberous sclerosis should always be done.
Keywords: Angiomyolipoma, Giant, Bilateral, Tuberous sclerosis
Background
Angiomyolipoma is a benign hamartomatous solid tumour of the kidney consisting of mature adipose tissue, smooth muscle and thick-walled vessels,1 with a prevalence of 0.2–0.6% and a strong female predilection.2 It accounts for 3% of the solid renal masses.3 The term ‘giant angiomyolipoma’ is defined as a tumour greater than 10cm.4 We report a case of bilateral giant renal angiomyolipoma which occupied the patient’s right side completely and more than half of the abdomen. It appears to be the third largest angiomyolipoma and largest among bilateral giant renal angiomyolipoma in the indexed literature.
Case history
A 26-year-old male presented with a large right-sided abdominal swelling for the past three years, which was slowly increasing in size and was associated with vague abdominal pain. He had no urinary or gastrointestinal symptoms. On inspection, the abdomen was distended; the swelling was seen in the right flank and iliac region, extending beyond the midline. On palpation, it was non-tender, firm in consistency and had a smooth surface. It extended from the right subcostal to the iliac region and also beyond the midline.
His haemoglobin was 9.8 g/dl, but other laboratory investigations (including kidney function tests) were essentially normal. On ultrasound, a large right-sided retroperitoneal tumour measuring 33 × 18 × 12cm replacing the right kidney was seen, and a similar lesion was present in the left kidney measuring 12 × 6cm. Both lesions were suggestive of angiomyolipoma. Computed tomography (CT) of the abdomen revealed a large well-defined mass in the right side of the abdomen, crossing the midline and extending from D11 to the coccyx, predominantly in the retroperitoneum (Figure 1). The mass was heterogeneous, replacing and distorting the right renal parenchyma and collecting system with areas of soft tissue and fat components (Hounsfield units of −80), measuring 35 × 20 × 12cm. Intermixed within this fatty mass were areas of tissue density corresponding with smooth muscles and blood vessels. The mass was encasing the right renal vessels.
Figure 1 .
Computed tomography (coronal section) showing giant right angiomyolipoma occupying more than 50% of the abdomen and going into the pelvis
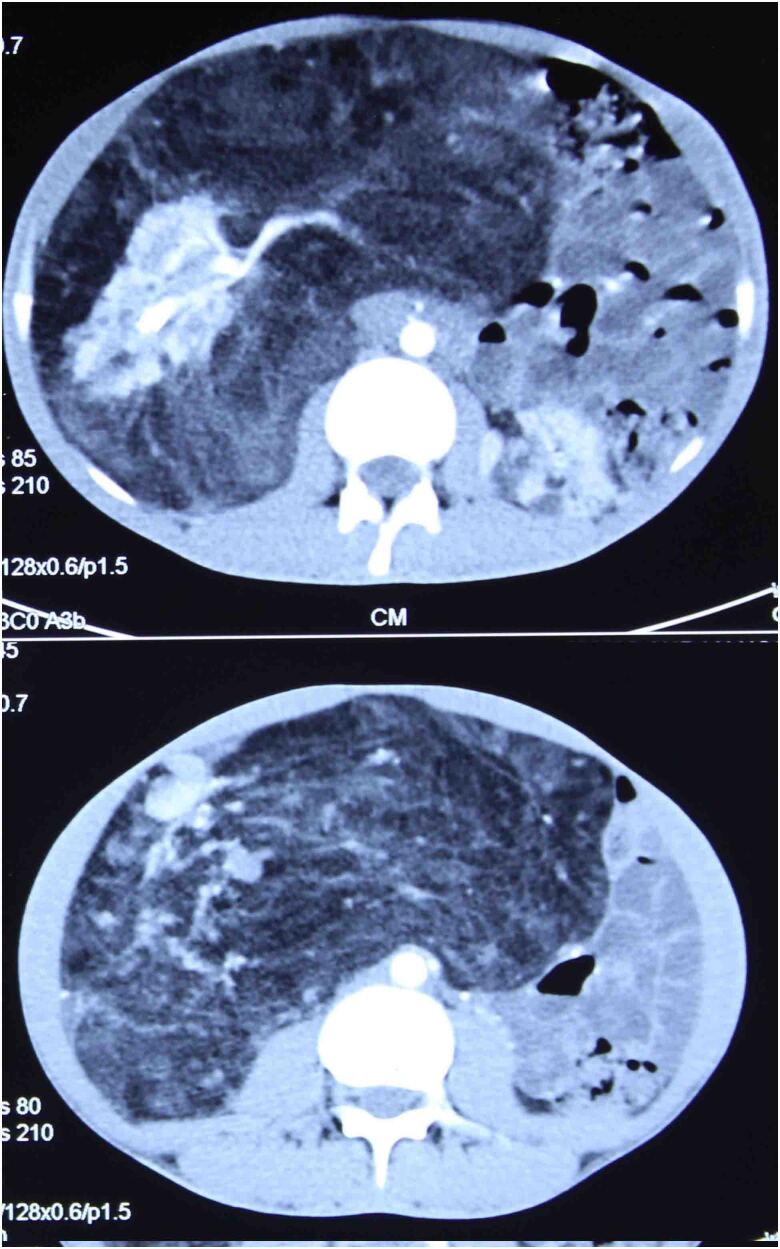
The left kidney showed a similar fatty lesion of size 14 × 6cm. Findings were consistent with angiomyolipoma (Figures 2, 3). The patient was re-evaluated for the possibility of tuberous sclerosis. There was no history of mental restriction, epilepsy or adenoma sebaceum and no dermatological lesions. However, a magnetic resonance image (MRI) of the patient’s brain demonstrated multiple small subependymal nodules, which indicated tuberous sclerosis (Figure 4). Immunotesting for HMB45 was not available in our hospital. The patient was prepared for preoperative embolisation followed by surgery. However, because of an emergency in the family, the patient left hospital before surgery. He was contacted by telephone for about 10 months, but he refused any treatment and is lost to follow-up.
Figure 2 .
Computed tomography: axial section (left) showing bilateral renal angiomyolipoma; coronal section (right)
Figure 3 .
Computed tomography (axial section) showing right side totally occupied by the tumour and bowel loops pushed towards the left side
Figure 4 .
(Left) Magnetic resonance image of the brain (axial section) showing subependymal nodules in lateral ventricles. (Right) Susceptibility weighted image showing calcified subependymal nodules
Discussion
Renal angiomyolipoma is a benign neoplasm arising from mesenchymal tissues.5 It is typically a solid triphasic tumour composed of varying amounts of three elements: dysmorphic blood vessels, smooth muscle components and mature adipose tissue.6 It usually presents in middle-aged women and accounts for 3% of the solid renal masses.3 Some 80% of renal angiomyolipomas are sporadic and remaining 20% are associated with tuberous sclerosis complex.7 Tuberous sclerosis is an autosomal dominant disease with incomplete penetrance. Its prevalence in the literature varies from 1/6,000 to 1/12,000 individuals.8 Of those patients with tuberous sclerosis, 55–75% may have renal angiomyolipoma.9,10 Other renal manifestations of tuberous sclerosis complex are renal cysts and, rarely, renal cell carcinomas. In contrast to the sporadic form of angiomyolipoma, hereditary lesions of angiomyolipoma affect both men and women equally and manifest in the second or third decade.11 They are usually large, multiple and bilateral, and are prone to grow more aggressively,12 up to 30cm in diameter.13,14
Renal angiomyolipoma is largely an incidental radiological finding; most patients are asymptomatic when they receive the diagnosis.2 Symptomatic presentation is most frequently related to spontaneous retroperitoneal haemorrhage due to a haemorrhagic aneurysm, although this is seen in less than 15% of cases.2 It leads to one-third of the patients presenting with shock, and thus the risk of haemorrhagic shock is the main clinical concern in a patient with angiomyolipoma. Other symptoms include a palpable mass, flank pain, haematuria, anaemia, urinary tract infection or renal failure.15
About 50 cases of giant renal angiomyolipoma have been reported to date in the indexed literature, Most of which were unilateral. The literature was searched using PubMed and the Cochrane Library for the keywords ‘giant angiomyolipoma’ and ‘bilateral angiomyolipoma’ for the period 1979–2019. The search on PubMed yielded 23 results, while MEDLINE and the Cochrane Library did not produce any results. Our case appears to be the third largest angiomyolipoma and the largest among bilateral giant renal angiomyolipomas in the indexed literature (Table 1).
Table 1 .
Giant renal angiomyolipoma in the indexed literature, by size
| Study | Year | Size (cm) | Side | Tuberous sclerosis | Bilateral |
|---|---|---|---|---|---|
| Katz et al29 | 1997 | 45 × 20 × 12 | Left | Yes | No |
| Taneja et al30 | 2013 | 39 × 25 × 9 | Left | No | No |
| Current case | 2020 | 35 × 20 × 12 (R) and 14 × 6 (L) | Both | Yes | Yes |
| Hussain et al31 | 2013 | 32 × 16 × 12 (R) and 27 × 21 × 16 (L) | Both | Yes | Yes |
| Barbará et al32 | 2004 | 31 × 19 × 10 (L) and 14 × 5.5 (R) | Both | Yes | Yes |
| Castillo et al13 | 1987 | 30 × 25 × 20 | Left | No | No |
| Alshehri et al14 | 2020 | 30 × 22 × 20 | Right | No | No |
| Tong et al33 | 1980 | 30 | No | No | |
| Zhou et al34 | 2015 | 28 × 20 × 14 (R) and 12 × 9 × 6 (L) | Both | No | Yes |
| Eason et al35 | 1979 | 28 × 16 × 9 | Left | No | No |
| Hsu et al36 | 2002 | 24 × 17 × 10 | Right | No | No |
| Cichocki et al37 | 2014 | 22.5 × 9.5 × 10.4 | Left | No | No |
Imaging plays a major role in the diagnosis and management of renal angiomyolipomas. The detection of adipose tissue is the fundamental diagnostic criterion of a classic angiomyolipoma.2 On ultrasound, a classic angiomyolipoma is markedly hyperechoic to renal parenchyma, owing to the presence of fat.16 The image-based detection of fat is aided by CT,17 which correctly diagnosed angiomyolipoma in 75–86% of cases.18 The presence of fat, which is highly suggested by attenuation less than −10 HU, is diagnostic of renal angiomyolipoma.19,20 MRI can determine the amount of intravoxel fat, which helps in the diagnosis of angiomyolipoma.21 The ‘Indian ink artefact’, which refers to the loss of signal at the border of the mass and renal parenchyma, is indicative of an angiomyolipoma.22
Although the diagnosis of angiomyolipoma can usually be established by imaging alone, percutaneous biopsy is sometimes advocated when uncertainty persists after radiographic imaging. Needle biopsy is not widely used for diagnosing renal masses because biopsy results often do not affect the subsequent management of renal masses, including angiomyolipoma, since negative biopsy does not exclude possible malignancy in giant angiomyolipomas.3 Positive immunoreactivity for HMB45, a monoclonal antibody raised against a melanoma-associated antigen, is characteristic for angiomyolipoma and can be used to differentiate this tumour from sarcoma and other tumours.23
Giant renal angiomyolipomas are usually slow growing tumours, usually at the rate of 5% per year or 0.19cm/year.24 They can rarely reach a large size but, in our patient, it was of enormous proportions, occupying the right side completely, together with more than half of the abdomen, pushing the bowel loops to the left side.
The management of angiomyolipomas has been correlative with symptoms. Primary indications for intervention are symptoms such as pain or haemorrhage, or the suspicion of malignancy.3 The risk of haemorrhage and the frequency of symptoms increases with the size of the angiomyolipoma.25 Thus, selective arterial embolisation is the first line of treatment for patients with larger-sized tumours.26 In selected high-risk patients, such as patients with whom regular follow-up is difficult, prophylactic embolisation (asymptomatic tumour of 4cm or larger) is recommended.16 The size of the tumour usually decreases by two-thirds.4 The principle indications of surgical intervention are persistent haemorrhage, suspicion of malignancy or failed embolisation.4 The benign nature of renal angiomyolipoma favours nephron-sparing surgery.3 In cases of bilateral lesions, as seen in tuberous sclerosis, nephron-sparing surgery should be performed.27 Total nephrectomy should be reserved for patients with life-threatening haemorrhage and near total replacement of renal tissue.28
Conclusion
Giant renal angiomyolipoma is an uncommon tumour, with bilateral giant angiomyolipoma being a rare entity. It is rare for angiomyolipoma to occupy the right side completely and more than half of the abdomen. CT is diagnostic tool identification of classic angiomyolipoma. Preoperative embolisation helps in reducing size of the tumour. In cases of giant and bilateral angiomyolipoma, evaluation for tuberous sclerosis should always be done.
References
- 1.Jinzaki M, Silverman SG, Akita Het al. Renal angiomyolipoma: a radiological classification and update on recent developments in diagnosis and management. Abdom Imaging 2014; 39: 588–604. 10.1007/s00261-014-0083-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fittschen A, Wendlik I, Oeztuerk Set al. Prevalence of sporadic renal angiomyolipoma: a retrospective analysis of 61,389 in-and out-patients. Abdom Imaging 2014; 39: 1009–1013. 10.1007/s00261-014-0129-6 [DOI] [PubMed] [Google Scholar]
- 3.Nelson CP, Sanda MG. Contemporary diagnosis and management of renal angiomyolipoma. J Urol 2002; 168: 1315–1325. 10.1016/S0022-5347(05)64440-0 [DOI] [PubMed] [Google Scholar]
- 4.Chronopoulos PN, Kaisidis GN, Vaiopoulos CKet al. Spontaneous rupture of a giant renal angiomyolipoma: Wunderlich’s syndrome: report of a case. Int J Surg Case Rep 2016; 19: 140–143. 10.1016/j.ijscr.2015.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan GS, Straumfjord JV, Hall EJ. Angiomyolip of the kidney. J Urol 1951; 65: 525–527. 10.1016/S0022-5347(17)68515-X [DOI] [PubMed] [Google Scholar]
- 6.Eble JN, Togashi P, Pisani P.. Renal cell carcinoma. In: Eble JN, Sauter G, Epstein JI, Sesterhenn IA, eds. Pathology and Genetics of Tumours of the Urinary and Male Genital Organs. Lyon: IARC Press. 2004. pp. 12–14. [Google Scholar]
- 7.Flum AS, Hamoui N, Said MAet al. Update on the diagnosis and management of renal angiomyolipoma. J Urol 2016; 195: 834–846. 10.1016/j.juro.2015.07.126 [DOI] [PubMed] [Google Scholar]
- 8.O'Callaghan FJ, Noakes MJ, Martyn CN, Osborne JP. An epidemiological study of renal pathology in tuberous sclerosis complex. BJU Int 2004; 94: 853–857. 10.1111/j.1464-410X.2004.05046.x [DOI] [PubMed] [Google Scholar]
- 9.Dabora SL, Jozwiak S, Franz DNet al. Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared with TSC1, disease in multiple organs. Am J Hum Genet 2001; 68: 64–80. 10.1086/316951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ewalt DH, Sheffield E, Sparagana SPet al. Renal lesion growth in children with tuberous sclerosis complex. J Urol 1998; 160: 141–145. 10.1016/S0022-5347(01)63072-6 [DOI] [PubMed] [Google Scholar]
- 11.Seyam RM, Bissada NK, Kattan SAet al. Changing trends in presentation, diagnosis and management of renal angiomyolipoma: comparison of sporadic and tuberous sclerosis complex-associated forms. Urology 2008; 72: 1077–1082. 10.1016/j.urology.2008.07.049 [DOI] [PubMed] [Google Scholar]
- 12.Von Ranke FM, Faria IM, Zanetti Get al. Imaging of tuberous sclerosis complex: a pictorial review. Radiol Bras 2017; 50: 48–54 10.1590/0100-3984.2016.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Castillo M, Casillas J. CT appearance of giant renal angiomyolipoma. Comput Radiol 1987; 11: 49–52. 10.1016/0730-4862(87)90029-1 [DOI] [PubMed] [Google Scholar]
- 14.Alshehri M, Hakami B, Aljameel Net al. Sporadic giant renal angiomyolipoma: A case report and literature review of clinical presentation, diagnosis, and treatment options. Urol Ann 2020; 12: 167–171. 10.4103/UA.UA_26_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Logue LG, Acker RE, Sienko AE. Best cases from the AFIP: angiomyolipomas in tuberous sclerosis. Radiographic 2003; 23: 241–246. 10.1148/rg.231025109 [DOI] [PubMed] [Google Scholar]
- 16.Siegel CL, Middleton WD, Teefey SA, McClennan BL. Angiomyolipoma and renal cell carcinoma: US differentiation. Radiology 1996; 198: 789–793. 10.1148/radiology.198.3.8628873 [DOI] [PubMed] [Google Scholar]
- 17.Bosniak MA. Angiomyolipoma (hamartoma) of the kidney: a preoperative diagnosis is possible in virtually every case. Urol Radiol 1981; 3: 135–142. 10.1007/BF02938781 [DOI] [PubMed] [Google Scholar]
- 18.Blute ML, Malek RS, Segura JW. Angiomyolipoma: clinical metamorphosis and concepts for management. J Urol 1988; 139: 20–24. 10.1016/S0022-5347(17)42276-2 [DOI] [PubMed] [Google Scholar]
- 19.Bosniak MA, Megibow A, Hulnick DHet al. CT diagnosis of renal angiomyolipoma: the importance of detecting small amounts of fat. AJR Am J Roentgenol 1988; 151: 497–501. 10.2214/ajr.151.3.497 [DOI] [PubMed] [Google Scholar]
- 20.Totty WG, McClennan BL, Melson GL, Patel R. Relative value of computed tomography and ultrasonography in the assessment of renal angiomyolipoma. J Comput Assist Tomogr 1981; 5: 173–178. 10.1097/00004728-198104000-00006 [DOI] [PubMed] [Google Scholar]
- 21.Lemaitre L, Claudon M, Dubrulle F, Mazeman E. Imaging of angiomyolipomas. Semin Ultrasound CT MR 1997; 18: 100–114. 10.1016/S0887-2171(97)90054-8 [DOI] [PubMed] [Google Scholar]
- 22.Israel GM, Hindman N, Hecht E, Krinsky G. The use of opposed-phase chemical shift MRI in the diagnosis of renal angiomyolipomas. AJR Am J Roentgenol 2005; 184: 1868–1872. 10.2214/ajr.184.6.01841868 [DOI] [PubMed] [Google Scholar]
- 23.Eble JN. Angiomyolipoma of kidney. Semin Diagn Pathol 1998; 15: 21–40. [PubMed] [Google Scholar]
- 24.Lemaitre L, Robert Y, Dubrulle Fet al. Renal angiomyolipoma: growth followed up with CT and/or US. Radiology 1995; 197: 598–602. 10.1148/radiology.197.3.7480725 [DOI] [PubMed] [Google Scholar]
- 25.Luca D, Rossetti R. Management of renal angiomyolipoma: a report of 53 cases. BJU Int 1999; 83: 215–218. 10.1046/j.1464-410x.1999.00932.x [DOI] [PubMed] [Google Scholar]
- 26.Bora A, Soni A, Sainani N, Patkar D. Emergency embolisation of a bleeding renal angiomyolipoma using polyvinyl alcohol particles. Diagn Interv Radiol 2007; 13: 213–216. [PubMed] [Google Scholar]
- 27.Faddegon S, So A. Treatment of angiomyolipoma at a tertiary care centre: the decision between surgery and angioembolisation. Can Urol Assoc J 2011; 5: E138–E141. 10.5489/cuaj.10028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Granata A, Basile A, Figuera Met al. Spontaneous retroperitoneal hemorrhage due to massive rupture of renal angiomyolipoma treated with nephrectomy: an unusual onset of tuberous sclerosis complex. Clin Nephrol 2009; 71: 441–444. 10.5414/CNP71441 [DOI] [PubMed] [Google Scholar]
- 29.Katz DS, Poster RB. Massive renal angiomyolipoma in tuberous sclerosis. Clin Imaging 1997; 21: 200–202. 10.1016/S0899-7071(96)00019-8 [DOI] [PubMed] [Google Scholar]
- 30.Taneja R, Singh DV. Giant renal angiomyolipoma: unusual cause of huge abdominal mass. J Clin Imaging Sci 2013; 3: 56. 10.4103/2156-7514.122326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hussain M, Mubarak M, Sultan Get al. Renal transplant in a tuberous sclerosis patient with bilateral giant renal angiomyolipomas and concurrent renal carcinoma. Saudi J Kidney Dis Transpl 2013; 24: 318–321. 10.4103/1319-2442.109591 [DOI] [PubMed] [Google Scholar]
- 32.Barbará MR, Malleu AM, Llul MR, Armada JC. Giant renal angiomyolipoma disclosed by mild lumbar trauma and treated with nephrectomy: report of a case. Actas Urol Esp 2004; 28: 133–137. 10.1016/S0210-4806(04)73052-1 [DOI] [PubMed] [Google Scholar]
- 33.Tong YC, Chieng PU, Tsai TC, Lin SM. Renal angiomyolipoma: report of 24 cases. Br J Urol 1990; 66: 585–589. 10.1111/j.1464-410X.1990.tb07187.x [DOI] [PubMed] [Google Scholar]
- 34.Zhou Y, Tang Y, Tang Jet al. Total nephrectomy with nephron-sparing surgery for a giant bilateral renal angiomyolipoma: A case report. Oncol Lett 2015; 10: 2450–2452. 10.3892/ol.2015.3538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eason AA, Cattolica EV, Mcgrath TW. Massive renal angiomyolipoma: preoperative infarction by balloon catheter. J Urol 1979; 121: 360–361. 10.1016/S0022-5347(17)56786-5 [DOI] [PubMed] [Google Scholar]
- 36.Hsu TH, O’Hara J, Mehta Aet al. Nephron-sparing nephrectomy for giant renal angiomyolipoma associated with lymphangioleiomyomatosis. Urology 2002; 59: 138. 10.1016/S0090-4295(01)01505-9 [DOI] [PubMed] [Google Scholar]
- 37.Cichocki M, Sosnowski M, Jablonowski Z. A giant renal angiomyolipoma (angiomyolipoma) in a patient with septo-optic dysplasia (SOD). Eur J Med Res 2014; 19: 46. 10.1186/s40001-014-0046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]