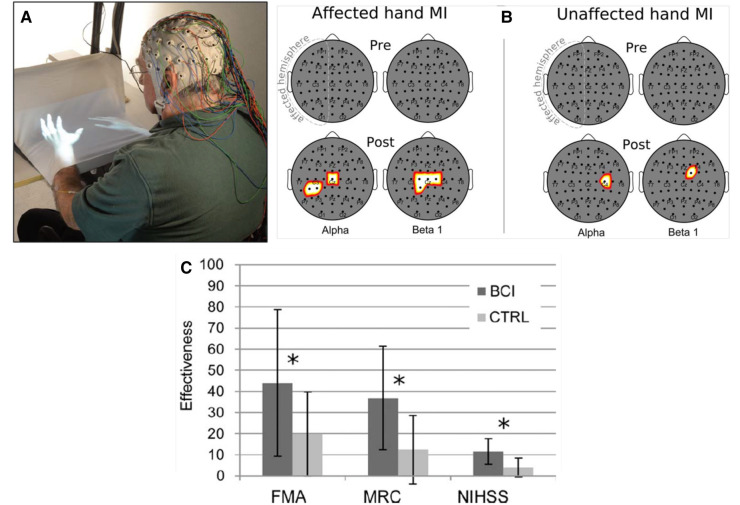
Figure 3.
Brain-computer interface (BCI)-based feedback training of motor imagery, and its effects on hand/arm function in people with chronic stroke. (A) The patient sits with hands resting on a desk and covered by a white blanket. An adjustable forearm orthosis provides support. The cue and feedback for the patient are projected on the blanket by a custom software program, providing a visual representation of the patient's hands (“virtual hands”). During each session, the therapist monitors the patient's electroencephalogram (EEG) activity continuously through immediate BCI-based feedback displayed on a screen. The amount of sensorimotor rhythm [sensorimotor rhythm (SMR) desynchronization (i.e., decrease)] at selected electrodes determines the vertical velocity of a cursor on the therapist's screen. When the cursor reaches a target in the upper part of the screen, the virtual hand performs the imagined movement (i.e., this is the feedback to the patient for a successful trial). The therapist also monitors electromyography (EMG) activity from the patient's hand and forearm muscles to assess degree of relaxation. (B) Statistical scalp maps (nose at top; stroke-affected hemisphere on the left) associated with tonic grasping movement imagery (MI) of the affected (left) and unaffected hands (right). The differences in SMR desynchronization (alpha and beta1 frequency ranges) between the brain–computer interface (BCI) and control (CTRL) patient groups in the Pre (top row) and POST (bottom row) sessions were assessed by t-test. Pixel color represents the corresponding probability value. Gray indicates nonsignificant differences; white–yellow indicates stronger desynchronization (p < 0.05, Bonferroni corrected) in the BCI group; and red denotes stronger desynchronization (p < 0.05, Bonferroni corrected) in the CTRL group. After treatment, SMR desynchronization is greater in the BCI group than in the Control group over the affected hemisphere and, to a lesser extent, over the other hemisphere. (C) Improvements in clinical outcome measures [Fugl–Meyer Assessment (FMA), Medical Research Council scale for muscle strength (MRC), National Institute of Health Stroke Scale (NIHSS)] in the BCI group and the Control (CTRL) group. *: p < 0.05 between groups by independent-samples t-test. The probability of achieving a minimal clinically important difference (MCID) for the FMA (7 points) was significantly (p = 0.01) greater in the BCI group (11/14) than in the Control group (3/14). [From (30).].