Abstract
The present study explored the predictive capacity of fear of COVID-19 on the intention to be vaccinated against COVID-19 and the influence in this relationship of conspiracy beliefs as a possible mediating psychological variable, in 13 Latin American countries. A total of 5779 people recruited through non-probabilistic convenience sampling participated. To collect information, we used the Fear of COVID-19 Scale, Vaccine conspiracy beliefs Scale-COVID-19 and a single item of intention to vaccinate. A full a priori Structural Equation Model was used; whereas, cross-country invariance was performed from increasingly restricted structural models. The results indicated that, fear of COVID-19 positively predicts intention to vaccinate and the presence of conspiracy beliefs about COVID-19 vaccines. The latter negatively predicted intention to vaccinate against COVID-19. Besides, conspiracy beliefs about COVID-19 vaccines had an indirect effect on the relationship between fear of COVID-19 and intention to vaccinate against COVID-19 in the 13 countries assessed. Finally, the cross-national similarities of the mediational model among the 13 participating countries are strongly supported. The study is the first to test a cross-national mediational model across variables in a large number of Latin American countries. However, further studies with other countries in other regions of the world are needed.
Keywords: COVID-19, conspiracy, beliefs, fear, vaccination
Introduction
The emergence of COVID-19 in late 2019 became the biggest public health problem of the 21st century. Its rapid spread generated increased morbidity and mortality, especially in elderly people and people with chronic diseases, leading to the establishment of quarantines and physical distancing to try to reduce the transmission of the disease. However, the restriction measures led to a worldwide economic recession (Mehta, 2020). In this sense, the negative impact of the pandemic on the health and economy of people around the world generated the imperative need to develop vaccines against COVID-19 in order to obtain collective immunity against the disease (Al-Amer et al., 2022). Having a large number of people immunized against the disease within a population will provide indirect protection to vulnerable populations (Randolph & Barreiro, 2020).
The development of COVID-19 vaccines was initiated immediately after the genetic sequence of the SARS-CoV-2 virus was known (Wong et al., 2021). This resulted in 76 COVID-19 vaccine candidates in clinical development and 182 in preclinical evaluation by March 2021. (World Health Organization, 2021a). Despite success in the development of vaccines against COVID-19, it is a great challenge to convince people to accept vaccination against the disease (World Health Organization, 2021b). There is a significant group of people in different countries of the world who hesitated to be vaccinated against COVID-19 (Aw et al., 2021; Caycho-Rodríguez et al., 2022a; Sallam, 2021; Sallam et al., 2022). A study in 175 countries reported COVID-19 vaccine uptake rates above 60% in 72 countries; whereas, 42 countries uptake rates ranged from 13% to 59%. Hesitancy to vaccinate against COVID-19 vaccine was most notable in countries in the Middle East/North Africa, Europe, Central Asia and West/Central Africa (Sallam et al., 2022). In the case of Latin America and the Caribbean, 20 countries were evaluated, where the highest rate of acceptance to be vaccinated against COVID-19 was observed in Mexico (88%) and the lowest rate in Haiti (43%) (Sallam et al., 2022). Another study involving 13 Latin American countries indicated that the highest prevalence of intention to vaccinate was observed in Brazil (96.94%), Cuba (89.59%), Chile (84.59%) and Mexico (78.33%), while the lowest prevalence was in El Salvador (54.01%), Paraguay (55.87%) and Uruguay (56.40%) (Caycho-Rodríguez et al., 2022a). Similarly, another systematic review study indicated a high prevalence of intention to be vaccinated against COVID-19 (78.0%) in the general population of Latin America (Alarcón-Braga et al., 2022). Even so, the rates of hesitancy and resistance to vaccination against COVID-19 were a problem for effective control of the spread of the virus (Fan et al., 2021). However, most of the studies on the intention to vaccinate against COVID-19 were conducted before September or October 2020, without having yet developed a vaccine (Soares et al., 2021) and, therefore, the evaluation was carried out through hypothetical questions (Fisher et al., 2020; Reiter et al., 2020). This situation could influence people’s responses and the findings reported (Lazarus et al., 2021).
Defining intention to vaccinate includes willingness to vaccinate and vaccine acceptability, as well as, desire and positive attitudes toward vaccines, in contrast to vaccine resistance and refusal to vaccinate (Al-Amer et al., 2022). There are different factors that influence the intention to be vaccinated, such as socio-demographic characteristics, beliefs, individual experiences, external or organizational factors, factors specific to vaccination, such as previous vaccination experience, religion, culture, gender and socioeconomic level, risk perception or the design of vaccination programs (Dubé et al., 2013; MacDonald, 2015). Among the different factors, it has been suggested that psychological factors may play an important role in the way individuals react to vaccination (Caci et al., 2020; Scrima et al., 2022). Therefore, the present study explored the predictive capacity of fear of COVID-19 on the intention to be vaccinated against COVID-19 and the influence in this relationship of conspiracy beliefs as a possible mediating psychological variable related to individual differences, in 13 Latin American countries. For this purpose, the following hypotheses were formulated.
First, it was hypothesized that fear of COVID-19 positively predicts intention to vaccinate against COVID-19. From the theory of protective motivation (PMT; Rogers, 1975), it has been suggested that people who perceive a greater health risk and fear of disease perform more healthy behaviors. This has been reflected in recent studies indicating that people with a greater fear of COVID-19 are more likely to be vaccinated (Detoc et al., 2020; Gagneux-Brunon et al., 2021; Head et al., 2020; Reuken et al., 2020; Yahaghi et al., 2021).
Second, the hypothesis that fear predicts the emergence of conspiracy beliefs about COVID-19 vaccines. From the dual defense process model, it has been indicated that experiencing fear can lead people to confront it in two ways. First, by eliminating the negative stimulus in a direct and rational way; and second, by activating more distant defenses, which originate the appearance of irrational and unrealistic beliefs, such as conspiracy ideas, that allow giving meaning to the fearful situation (Scrima et al., 2022). Therefore, people with the greatest fear of COVID-19 believe in conspiratorial ideas to diminish their fears and provide a justification for an uncertain situation (Stephens, 2020). The same has been suggested by other studies during the pandemic, where it has been indicated that, to counteract fear, people can share irrefutable beliefs that, although they are not directly related to a dangerous stimulus, allow them to give meaning to events or situations (Larsen et al., 2021). However, these justifications are provided without verifying the veracity of the information. Similarly, the presence of distal defenses seeks to maintain higher levels of self-esteem and strengthen people’s own cultural vision of the world. (Scrima et al., 2022). Adherence to irrefutable ideas, such as conspiracy beliefs, could strengthen people’s cultural worldviews, which would also explain the relationships between fear and conspiracy beliefs. (Newheiser et al., 2011). Likewise, it has been suggested that fear is an emotional determinant of conspiracy theories (van Prooijen & Douglas, 2018). At the Latin American level, the results on the relationship between fear of COVID-19 and conspiracy beliefs are inconclusive. One study with Latin American sample suggested a relationship between fear of COVID-19 and conspiracy beliefs (Jovančević & Milićević, 2020), while another, with the participation of four South American countries, and using the network analysis method, indicated that there is no clear relationship between conspiracy ideas about COVID-19 vaccines and symptoms of fear of the disease (Caycho-Rodríguez et al., 2022b).
As a third hypothesis, it was indicated that the Conspiracy beliefs about COVID-19 vaccines negatively predict intention to vaccinate against COVID-19. Beliefs in conspiracy theories about infectious diseases negatively impact health behaviors associated with vaccination (Salman et al., 2022). Already since before the pandemic, it has been indicated that, the presence of conspiracy beliefs is related to a lower intention to vaccinate (Jolley & Douglas, 2014; Oliver & Wood, 2014); thus, it was expected that this would not be different for COVID-19 vaccines. Recent studies reported that beliefs in conspiracy theories showed significant negative relationships with intention to vaccinate (Bertin et al., 2020; Eberhardt & Ling, 2021; Freeman et al., 2020; Ghaddar et al., 2022; Yang et al., 2021). However, it should be considered that other studies have suggested that conspiracy beliefs had a positive impact on intentions to vaccinate against COVID-19 (Wang & Kim, 2021). A previous study, which linked conspiracy beliefs about COVID-19 vaccines and the intention to get vaccinated against the disease, found a negative relationship between the variables in these same 13 participating countries. (Caycho-Rodríguez et al., 2022c). In the previous study, unlike the present one, he only tested a structural model that related both variables without the participation of other variables.
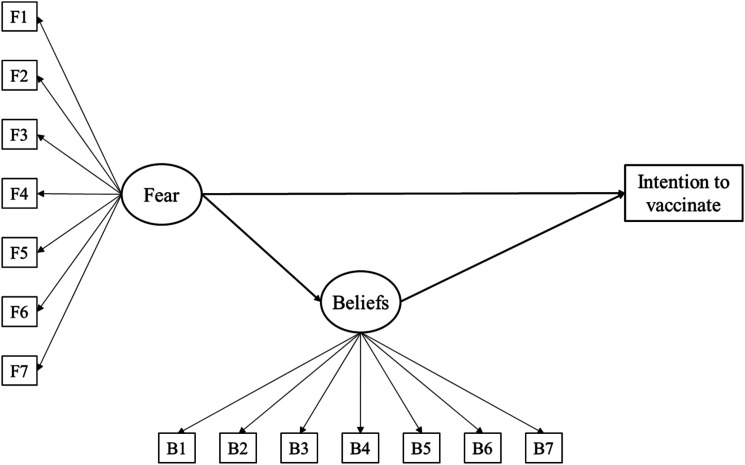
The fourth hypothesis indicates that fear of COVID-19 has an indirect effect on the intention to vaccinate against COVID-19 through Conspiracy beliefs about COVID-19 vaccines. The theoretical hypotheses already mentioned, allowed testing the mediating role of conspiracy beliefs about COVID-19 vaccines in the relationship between fear of COVID-19 and intention to be vaccinated against COVID-19. As shown in Figure 1, it is proposed that, fear of COVID-19 is a predictor of intention to vaccinate against COVID-19 (Detoc et al., 2020; Gagneux-Brunon et al., 2021; Head et al., 2020; Reuken et al., 2020; Yahaghi et al., 2021); however, this fear could generate conspiratorial ideas about COVID-19 vaccines to mitigate their impact and provide a rationale for an uncertain situation (Stephens, 2020), which would, in turn, reduce the intention to vaccinate against COVID-19 (Ghaddar et al., 2022; Yang et al., 2021). In this sense, on the one hand, there would be a direct and positive effect of fear of COVID-19 on the intention to vaccinate; while, on the other hand, there would be an indirect effect through the mediation of conspiracy beliefs about COVID-19 vaccines.
Figure 1.
A priori Structural Equation Model to predict intention to vaccinate.
Understanding the relationships between fear of COVID-19, conspiracy beliefs about COVID-19 vaccines, and intentions to vaccinate against COVID-19 is even more important in the Latin American context for several reasons. First, Latin America was one of the regions most affected by the COVID-19 pandemic and where intensive vaccination campaigns were needed to try to mitigate the impact of the pandemic (Alarcón-Braga et al., 2022). In this sense, it is important to have information on the predictors of intention to vaccinate in different countries of the region. Second, moderate levels of fear of COVID-19 have been reported in 13 Latin American countries, which was related to the presence of symptoms of anxiety and depression (Caycho-Rodríguez et al., 2021). Another study indicated that between 5.7% and 14.3% of Argentines, Peruvians and Mexicans presented high levels of fear of COVID-19 (Moya-Salazar et al., 2022). Third, a recent study indicated that people in 13 Latin American countries were, for the most part, in some degree of disagreement or indecision about conspiracy beliefs about COVID-19 vaccines (Caycho-Rodríguez et al., 2022d). Similar results were reported when assessing conspiracy beliefs about COVID-19 vaccines in the member countries of the Andean Community of Nations (CAN) (Caycho-Rodríguez et al., 2022e). However, having some degree of agreement with conspiracy beliefs could affect public health in Latin American countries (Caycho-Rodríguez et al., 2022f).
The study will provide insight into some psychological factors associated with the intention to be vaccinated against COVID-19 that may be important for designing effective awareness campaigns to promote acceptance of vaccination against COVID-19 or other similar infectious diseases at the regional level.
Method
Sample and Procedure
The participants were 5779 people residing in 13 Latin American countries (Argentina, Peru, Bolivia, Chile, Uruguay, Cuba, Ecuador, Guatemala, Mexico, Paraguay, Colombia, El Salvador, and Venezuela), who were recruited through non-probabilistic convenience sampling. The criteria for a person to be included in the study were: (1) to be of legal age according to the legislation of each participating country; (2) to reside in one of the participating countries at the time of the study; and (3) to provide informed consent. The number of participants varied among the different countries in the study (from 322 in Peru to 746 in El Salvador). Likewise, in all countries, the number of women was greater than that of men, with the former representing approximately 68% of the total number of participants in each country. Finally, the average age ranged from 26.52 years (Peru) to 44.04 years (Guatemala). Table 1 shows the sociodemographic characteristics of the participants in greater detail.
Table 1.
Sociodemographic Information of the Participants.
| Variables/Countries | Argentina | Bolivia | Chile | Colombia | Cuba | Ecuador | El Salvador | Guatemala | Mexico | Paraguay | Peru | Uruguay | Venezuela |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 363) | (n = 564) | (n = 453) | (n = 461) | (n = 334) | (n = 438) | (n = 746) | (n = 420) | (n = 484) | (n = 417) | (n = 322) | (n = 392) | (n = 385) | |
| Gender (%) | |||||||||||||
| Female | 255 (70.25) | 421 (74.65) | 314 (69.32) | 322 (69.85) | 231 (69.16) | 311 (71) | 546 (73.19) | 297 (70.71) | 331 (68.39) | 292 (70.02) | 224 (69.57) | 272 (69.39) | 276 (71.69) |
| Male | 108 (29.75) | 143 (25.35) | 139 (30.68) | 139 (30.15) | 103 (30.84) | 127 (29) | 200 (26.81) | 123 (29.29) | 153 (31.61) | 125 (29.98) | 98 (30.43) | 120 (30.61) | 109 (28.31) |
| Age | |||||||||||||
| Media (DE) | 37.95 (16.29) | 38.63 (11.55) | 35.17 (12.04) | 26.84 (11.99) | 27.63 (10.51) | 29.29 (10.81) | 32.18 (12.63) | 44.04 (13.62) | 26.66 (8.65) | 32.05 (10.29) | 26.52 (8.18) | 34.59 (11.18) | 43.75 (16.76) |
Data were collected between September and October 2021. All participating countries performed the same data collection procedure in the same time period. A Google Forms questionnaire was constructed, which contained the study objectives, informed consent, sociodemographic information, as well as the single item of intention to vaccinate, the Fear of COVID-19 Scale y la Vaccine conspiracy beliefs Scale-COVID-19. The online link to the questionnaire was distributed via social networks, such as Facebook, Instagram and LinkedIn) and email along with instructions for completing the survey. Within these instructions, participants were asked to disseminate the survey to other personal and/or professional contacts. The study received ethical approval from the Institutional Committee for the Protection of Human Subjects in Research (CIPSHI) of the University of Puerto Rico (No. 2223-006). Participation in the study was completely voluntary, requesting informed consent after reading the objectives. To submit their responses in the questionnaire, participants were required to answer all items.
Instruments
Fear of COVID-19. We used the Fear of COVID-19 Scale (FCV-19S; Ahorsu et al., 2020). The Spanish version used in different Latin American countries (Caycho-Rodríguez et al., 2022g) was used, consisting of seven items that measure symptoms of fear related to COVID-19. Each of the items was evaluated on a 5-point Likert-type scale ranging from 1 = strongly disagree to 5 = strongly agree. A total score can be obtained, from the sum of the scores of each item, ranging from 7 to 35, and where, a higher score would indicate a greater fear of the FCVID-19. The omega reliability coefficient was .94 for the FCV-19S in the present study.
Conspiracy beliefs about COVID-19 vaccines. We used the Vaccine conspiracy beliefs Scale-COVID-19 (VCBS-COVID-19, Caycho-Rodríguez et al., 2022c) validated in different Latin American countries. It is a 7-item measure that assesses the degree of agreement with conspiracy beliefs about COVID-19 vaccines. Each of the items has seven response alternatives (1 = strongly disagree to 7 = strongly agree). The sum of the scores for each of the seven items yields a total VCBS-COVID-19 score, where higher scores would indicate greater agreement with conspiracy beliefs about COVID-19 vaccines. In the present study, the omega reliability coefficient was .92 for the VCBS-COVID-19.
Intention to be vaccinated against COVID-19. A single item of intention to vaccinate against COVID-19 used in previous research was used (Caycho-Rodríguez et al., 2022a, 2022c). The single item was: How likely would you be to decide to get vaccinated against COVID-19, which had five response options (1 = Not at all likely, 2 = Unlikely, 3 = Uncertain, 4 = Somewhat likely, and 5 = Very likely). Higher scores on the single item would indicate a greater intention to vaccinate against COVID-19.
Statistical Analyses
Descriptive statistics for all the variables under study have been calculated. Additionally, internal estimates of the constructs involved in the research were estimated with coefficient omega (ω, McDonald, 1999), given that it overcomes the deficiencies of Cronbach’s alpha (Deng & Chan, 2017). Then a completely a priori full Structural Equations Model (SEM) as depicted in Figure 1. In order to assess model’s fit, the recommended indexes were employed (Tanaka, 1993): the chi-square test (χ2), the Comparative Fit Index (CFI), the Root Mean Squared Error of Approximation (RMSEA) and the Standardized Root Mean square Residual (SRMR). Cut-off criteria for the indesex according to (Hu & Bentler, 1999) are: a CFI equals or over .90 and RMSEA/SRMR equal or are under .08. Excellent fit is accomplished when CFI is at least .95 and RMSEA/SRMR estimates are .05 or less. The model was estimated with Diagonally Weighted Least Squares (DWLS) an adequate estimation method when variables are not multivariate normal and some (or all) variables are categorical (ordinal) (Kline, 2016). Additionally, a sensitivity analysis, as outlined in Harring et al. (2017), was performed. This sensitivity analyses used a phantom variable and several degrees of relations with the dependent and mediator variables varying from .25 standard deviations to .5 standard deviations to asses model sensitivity to external misspecification in the mediation effects. Finally, omega coefficients were estimated with Colwell’s calculator (Colwell, 2016).
Once the structural model was estimated in the total sample, its invariance across countries was analysed. The invariance procedure across countries consists of a series of increasingly constricted structural models and testing the significance of the differences between these models. Firstly, the model is freely estimated in all countries and (baseline) fit established. Secondly, factor loadings are constrained to equality in all countries. Thirdly, structural coefficients are constrained to equality across countries. All the models in the invariance procedure are nested, and therefore they can be compared using the statistical and the modelling approaches. The statistical approach compares models with chi-squares differences, and nonsignificant diferences point out to invariance across groups. However, the modelling rationale has been recommended (Cheung & Rensvold, 2002). This modelling approach employs practical fit indices to establish overall adequacy of models to compare. In the invariance steps, a model is retained if produces adequate levels of practical fit and a fit that is substantially similar to the fit of the less parsimonious model. Invariance is commonly assessed using CFI differences (ΔCFI), with differences of less than .01 used as the cut-off criterion to retain the parsimonious model (Cheung & Rensvold, 2002).
All statistical analyses were performed in R (R Core Team, 2021), with the structural model estimated in lavaan package (Rosseel, 2012).
Results
Descriptive statistics for all items, scales and indicators under study are presented in Table 2. Intention to vaccinate is high (4.7 on a scale ranging from a minimum of one to a maximum of five). False beliefs about COVID-19 had a mean value of 3.5, slightly below the midpoint of the scale (four). Finally, the average fear of COVID-19 stands at a 2.35 out of a maximum of 5.
Table 2.
Descriptive Statistics for the Items, the Scales and the Indicators in the Study.
| Variable | Mean | SD | Min | Max |
|---|---|---|---|---|
| Intention to vaccinate | 4.70 | 0.82 | 1 | 5 |
| Information about the safety of COVID vaccines is often fabricated | 3.79 | 1.90 | 1 | 7 |
| Vaccinating children against COVID is harmful and this fact is hidden | 3.04 | 1.81 | 1 | 7 |
| Pharmaceutical companies hide the dangers of COVID vaccines | 3.63 | 1.83 | 1 | 7 |
| People are misled about the efficacy of COVID vaccines | 3.42 | 1.85 | 1 | 7 |
| Information on the efficacy of COVID vaccines is often fabricated | 3.42 | 1.81 | 1 | 7 |
| People are misled about the safety of COVID vaccines | 3.40 | 1.82 | 1 | 7 |
| Government is hiding the link between vaccines and other diseases | 3.48 | 1.85 | 1 | 7 |
| Beliefs about COVID | 3.45 | 1.47 | 1 | 7 |
| I Am very afraid of COVID. | 2.88 | 1.41 | 1 | 5 |
| It makes me uncomfortable to think about COVID. | 2.65 | 1.37 | 1 | 5 |
| My hands become clammy when I think of COVID. | 1.84 | 1.16 | 1 | 5 |
| I Am afraid of losing my life because of COVID. | 2.89 | 1.49 | 1 | 5 |
| When I see news about COVID on social media, I get nervous or anxious | 2.27 | 1.31 | 1 | 5 |
| I can’t sleep because I’m worried about having COVID. | 1.83 | 1.12 | 1 | 5 |
| My heart races when I think of contracting COVID. | 2.11 | 1.30 | 1 | 5 |
| Fear of COVID | 2.35 | 1.06 | 1 | 5 |
The completely a priori structural model in Figure 1 proposes that fear of COVID-19 may have both a direct effect on the intention to vaccinate, but also an indirect effect through the false beliefs about COVID-19. This model was first estimated controlling for age and sex in the overall model. Although this model had a good model fit (χ2(112) = 4246.21, p < .001; CFI = .977; RMSEA = .079, 90% CI [.077, .081]; SRMR = .044). Nevertheless, none of the effects of the control variables age and sex were statistically significant (p > .05), with effects sizes very low ranging in absolute values from .01 to .04. Therefore, the more simple model depicted in Figure 1, without age and sex as controls was retained, and presented a good model fit: χ2(88) = 3884.25, p < .001; CFI = .977; RMSEA = .086, 90% CI [.083, .088]; SRMR = .047.
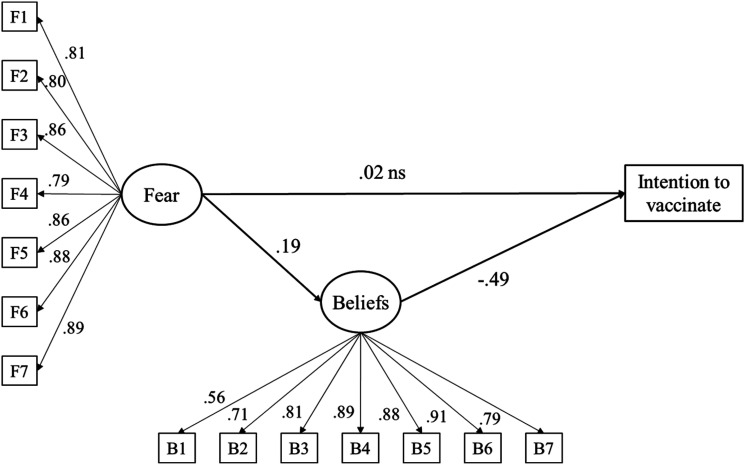
Standardized parameter estimates are presented in Figure 2. Factor loadings are all high and statistically significant. All factor loadings in the fear factor are higher than .70 indicating a clear relation to the construct. In the same vein, the lowest factor loading for the beliefs on COVID-19 indicators was already high and statistically significant (λ = .56). Regarding structural coefficients, that is the effects among the constructs of interest, the effect of fear of COVID-19 had not a significant direct effect on the intention to vaccinate (β = .02, p > .05). However, fear of COVID-19 significantly predicted false beliefs about COVID-19 (β = .19, p < .001). In turn, beliefs about COVID-19 had a significant and large negative effect on the intention to vaccinate (β = −.49, p < .001). The indirect effect of fear of COVID-19 on the intention to vaccinate was also statistically significant and negative (β = −.09, p < .001, with 95% bootstrap confidence interval from −.11 to −.08). Therefore, both beliefs and fear of COVID-19 had negative effects on the intention to vaccinate, although the effect of fear of COVID-19 was indirect. Overall a 3.9% of the variance of beliefs can be explained, while the percentage of variance explained for in intention to vaccinate was 23.1%. The additional sensitivity analysis with varying degrees of associations among the phantom variable and the mediator and the dependent variable (from .25 standard deviations to a maximum of .50) found that the effects from beliefs to intention to vaccinate remained statistically significant, and even improved (in a range from −.53 to −.69). Therefore, the significant and large negative effect on the intention to vaccinate may be considered robust.
Figure 2.
Estimates of the Structural Equation Model to predict intention to vaccinate. Note: All parameter estimates statistically significant (p < .01) but ns (p > .05).
Finally, the structural model has been tested for invariance across countries. The baseline model freely estimates the model in Figure 2 in each country. The model fit of this multigroup model is very good: This model had a very good fit to the observed data in the overall sample: χ2(1144) = 4762.6, p < .001; CFI = .980; RMSEA = .070, 90% CI [.068, .073]; SRMR = .065. Then all factor loadings are constrained to be equal across countries. This is a previous step that it is necessary before comparing structural effects therefore moderation by country. This second model, with loadings made equal across countries also fitted the data very well: χ2(1288) = 5279.9, p < .001; CFI = .978; RMSEA = .077, 90% CI [.075, .079]; SRMR = .069. Chi-square differences were statistically significant (Δχ2(144) = 300.3, p < .001), but the CFI differences were completely negligible (= .002). Therefore, it may be considered that loadings are equal in all Latin American countries analysed. Then structural effects were constrained to equality and a new multigroup model was estimated, again with excellent fit: χ2(1324) = 3734.1, p < .001; CFI = .987; RMSEA = .064, 90% CI [.061, .066]; SRMR = .085. Again, chi-square differences were statistically significant compared to the model with only loadings constrained (Δχ2(180) = 287.4, p < .001), but CFI and RMSEA values improved. In conclusion, the invariance routine allow us to stablish the model holds across all Latin American countries analysed.
Discussion
The study explored the predictive capacity of fear of COVID-19 on intention to vaccinate against COVID-19 and the influence on this relationship of conspiracy beliefs as a possible mediating psychological variable related to individual differences, in 13 Latin American countries. Overall, fear of COVID-19 had an indirect effect on intention to vaccinate against COVID-19 through conspiracy beliefs about COVID-19 vaccines.
In relation to the hypotheses posed, the results did not corroborate the first hypothesis that fear of COVID-19 positively predicts intention to vaccinate. In this sense, it was indicated that fear of COVID-19 did not have a significant direct effect on the intention to vaccinate against COVID-19. This is contrary to what was expected as reported in previous studies (Detoc, et al., 2020; Gagneux-Brunon et al., 2021; Head et al., 2020; Yahaghi et al., 2021). The findings would indicate that fear of COVID-19 alone would not significantly predict intention to vaccinate against COVI-19. This result could be explained by the fact that the study was conducted between September and October 2021, where about 29%–87% of people in the participating countries were already fully or partially vaccinated against COVID-19 (Our World in Data, 2022), which would decrease the sense of fear. Other studies have suggested that, while the threat of infection can generate fear, it is not always the threat of infection that can cause fear Ebrahimi (Ebrahimi et al., 2021), implementation of immunization programs reduces fear experience (Peng et al., 2022). Another possible explanation would indicate that the decrease in fear during the data collection period is due to people becoming accustomed to the new normal and the constant feedback from health experts (Hidaka et al., 2021).
Our second hypothesis indicated that fear predicts the emergence of conspiracy beliefs about COVID-19 vaccines. The results confirm this hypothesis, which is in agreement with previous reports (Jovančević & Milićević, 2020). This could be explained from the model of the dual defense process, where it has been indicated that experiencing fear can lead people to face it in two ways. First, by eliminating the negative stimulus in a direct and rational way; and second, by activating more distant defenses, which originate the appearance of irrational and unrealistic beliefs, such as conspiracy ideas, that allow giving meaning to the fearful situation (Scrima et al., 2022). Therefore, people who are most afraid of COVID-19 tend to believe in conspiratorial ideas to diminish their fears and give a justification to an uncertain situation (Stephens, 2020). However, these justifications are provided without verifying the veracity of the information. Likewise, the relationship between both variables is explained by the fact that fear is an emotional determinant of conspiracy theories (van Prooijen & Douglas, 2018). Nevertheless, it should be noted that another study indicated that the relationship between fear of COVID-19 and conspiracy beliefs about COVID-19 vaccines is not entirely clear (Caycho-Rodríguez et al., 2022b). This would lead to further research for more and better information on the relationship between the study variables.
The results also suggest that conspiracy beliefs about COVID-19 vaccines negatively predict intention to vaccinate against COVID-19 in the 13 participating countries, which has also been observed in previous studies (Bertin et al., 2020; Eberhardt & Ling, 2021; Freeman et al., 2020; Ghaddar et al., 2022; Yang, et al., 2021). It has been suggested that this relationship could be explained by the foreign origin of the pandemic and distrust of multinational institutions such as pharmaceutical companies (Bertin et al., 2020). Others explain the relationship in terms of a cost–benefit analysis (Wirawan et al., 2021). In this sense, the lower intention to vaccinate could be explained by the greater perception of the dangers related to conspiracy beliefs about vaccines, which outweigh the perceived benefits (Jolley & Douglas, 2014). On the other hand, it is possible that the relationship between conspiracy beliefs about COVID-19 vaccines and intention to vaccinate is due to the general psychological tendency to believe in conspiracies (Lewandowsky et al., 2013). It has been suggested that belief in conspiracy ideas linked to man’s landing on the moon was associated with a negative attitude towards vaccines (Lewandowsky et al., 2013). Also, the presence of a general conspiratorial mindset predicted a lower intention to vaccinate against COVID-19 (Bertin et al., 2020). The former needs to be further investigated, as it has also been suggested that, only beliefs in vaccine-related conspiracy theories negatively impacted intentions to vaccinate; whereas, believing in general pandemic conspiracy theories did not negatively impact intentions to vaccinate (Yang et al., 2021).
Finally, the fourth hypothesis suggested a mediating effect of conspiracy beliefs about COVID-19 vaccines on the relationship between fear of COVID-19 and intention to vaccinate against COVID-19. The findings of the present study confirmed a mediating effect that is related to that proposed in the dual-process model of defense (Pyszczynski et al., 1999). Furthermore, the model is invariant and, therefore, the relationships between the variables would have comparable meanings among the participants from the different Latin American countries. This model indicates that, despite the cultural and socioeconomic differences among the 13 countries, when experiencing fear, people may confront it with more proximal, direct and rational defense mechanisms that eliminate dangerous stimuli. However, fear may activate more distal defenses that generate irrational beliefs, such as conspiracy theories, and give meaning to their fear and, at the same time, negatively affect the occurrence of protective health behaviors, such as the intention to get vaccinated. The evidence that the relationships among the variables were not different among the 13 countries is of utmost importance for cross-cultural research. This is because the results of comparisons of variables between different cultures and/or countries would not be valid without evidence of measurement invariance (Milfont & Fischer, 2010). Similarly, the findings on the invariance of the relationships between the variables can inform the formulation of health policies for adherence to immunization programs at the regional level.
The strength of this study was the inclusion of a large number of participants from 13 Latin American countries. Previous studies have shown that different countries and regions have been underrepresented (see, for example, Lin et al., 2021; Sawicki et al., 2022; Varma et al., 2021), thus, the present study sought to overcome this problem by having participants from different Latin American countries. Likewise, the large number of participants allowed for a more statistically powerful analysis. Similarly, conducting a mediation allowed for a more detailed analysis of the relationships between fear of COVID-19, conspiracy beliefs about COVID-19 vaccines, and intention to vaccinate. Finally, the instruments used to measure fear of COVID-19 and conspiracy beliefs about COVID-19 vaccines were validated in different Latin American countries; whereas, the single item to measure intention to vaccinate has also been used in different countries of this region.
Despite the above, it is important to note the presence of some limitations in the study. First, the use of non-probability snowball sampling meant that the samples in each country were not representative and the findings cannot be generalized to all populations. Second, the use of an online questionnaire may generate a selection bias, as it does not take into account groups that have limited access to the Internet. However, social distancing regulations imposed during the pandemic did not allow face-to-face data collection. In addition, it should be noted that, the use of online questionnaires allows information to be obtained from larger samples during COVID-19. A third limitation was to assess intention to vaccinate against COVID-19 with a single item. Although it is common to use a single item to measure intention to vaccinate, the importance of this variable for public health makes it necessary to assess it in depth using standardized questionnaires (Ogilvie et al., 2021). Fourth, the implications of confinement were not controlled for due to differences in social constraints in each of the participating countries; however, as mentioned above, the survey was conducted in all countries at the same time. Fifth, data collection was done using self-report measures; therefore, the information could be susceptible to social desirability biases. However, the strong psychometric evidence from the self-report measures would indicate that the data are adequately valid and reliable. Sixth, the study design was cross-sectional, which limits cause and effect relationships between variables. Indeed, the same concept of mediation is causal in nature and therefore requires temporal precedence, an assumption that cannot be tested using cross-sectional data, which may bias the results compared to longitudinal data. That is, not all indirect effects in SEM models are mediational. In this case, the effect between fear and belief could be reciprocal, with increased belief in conspiracy theories about COVID-19 vaccines increasing fear. In this sense, other studies have suggested that conspiracy beliefs, spread through false news without scientific support, have created global panic, which has caused people to live in fear and anxiety (Allington et al., 2021; Naveed et al., 2021). Unfortunately, a model with this effect would fit the data exactly the same as the proposed model, and therefore our proposal of indirect effect is based on theoretical considerations and can only be considered tentative until longitudinal data are gathered and analyzed. All these limitations would lead to the fact that the findings should be interpreted with caution.
Conclusion
This study is, to our knowledge of the current scientific literature, the first to test a cross-national mediational model to assess the relationships between intentions to vaccinate against COVID-19, conspiracy beliefs about COVID-19 vaccines, and COVID-19 fear symptoms. It is concluded that, fear of COVID-19 positively predicts intention to vaccinate and the presence of conspiracy beliefs about COVID-19 vaccines. The latter, moreover, negatively predicted intention to vaccinate against COVID-19. Furthermore, conspiracy beliefs about COVID-19 vaccines had a mediating effect on the relationship between fear of COVID-19 and intention to vaccinate against COVID-19 in the 13 countries assessed. Finally, the cross-national similarities of the mediational model among the 13 participating countries are strongly supported.
Acknowledgments
None.
Footnotes
Author Contributions: TC-R and JMT provided initial conception, organization, and main writing of the text. JMT analyzed the data and prepared all figures and tables. PDV, CC-L, LWV, JV-L, RP-A, GC-L, WLAG, RR-C, MR-B, MD-C, MG, CR-J, RP-C, MC, PM, MEL-R, RM-H, DAPS, AS-P, ABF, DXP-C, AC, JT, JAMB, PG, VS-C, OP-R, IEC-R, RC, WYMR, DF-B, PC-V, AM-dC-T, JP, CB-V, AMEFL, IV, DV, MN-G, MKS and NAB-A were involved in data collection and acted as consultants and contributors to research design, data analysis, and text writing. The first draft of the manuscript was written by TC-R, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The study received ethical approval from the Institutional Committee for the Protection of Human Subjects in Research (CIPSHI) of the University of Puerto Rico (No. 2223-006).
Informed Consent: Informed consent was provided by all participants.
ORCID iD
Tomas Caycho-Rodriguez https://orcid.org/0000-0002-5349-7570
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
References
- Ahorsu D. K., Lin C. Y., Imani V., Saffari M., Griffiths M. D., Pakpour A. H. (2022). The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 20(3), 1537–1545. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Amer R., Maneze D., Everett B., Montayre J., Villarosa A. R., Dwekat E., Salamonson Y. (2022). COVID‐19 vaccination intention in the first year of the pandemic: A systematic review. Journal of Clinical Nursing, 31(1–2), 62–86. 10.1111/jocn.15951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alarcón-Braga E. A., Hernandez-Bustamante E. A., Salazar-Valdivia F. E., Valdez-Cornejo V. A., Mosquera-Rojas M. D., Ulloque-Badaracco J. R., Rondon-Saldaña J. C., Zafra-Tanaka J. H. (2022). Acceptance towards Covid-19 vaccination in Latin America and the Caribbean: A systematic review and meta-analysis. Travel Medicine and Infectious Disease, 49, 102369. 10.1016/j.tmaid.2022.102369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allington D., Duffy B., Wessely S., Dhavan N., Rubin J. (2021). Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychological medicine, 51(10), 1763–1769. 10.1017/S003329172000224X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aw J., Seng J. J. B., Seah S. S. Y., Low L. L. (2021). COVID-19 vaccine hesitancy. A scoping review of literature in high-income countries. Vaccines, 9(8), 900. 10.3390/vaccines9080900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertin P., Nera K., Delouvée S. (2020). Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: A conceptual replication-extension in the COVID-19 pandemic context. Frontiers in Psychology, 11, 565128. 10.3389/fpsyg.2020.565128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caci B., Miceli S., Scrima F., Cardaci M. (2020). Neuroticism and fear of COVID-19. The interplay between boredom, fantasy engagement, and perceived control over time. Frontiers in Psychology, 11, 574393. 10.3389/fpsyg.2020.574393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Tomás J. M., Vilca L. W., Carbajal-León C., Cervigni M., Gallegos M., Martino P., Barés I., Calandra M., Anacona C. A. R., López-Calle C., Moreta-Herrera R., Chacón-Andrade E. R., Lobos-Rivera M. E., Del Carpio P., Quintero Y., Robles E., Lombardo M. P., Recalde O. G., Figares A. B., White M., Videla C. B. (2021). Socio-demographic variables, fear of COVID-19, anxiety, and depression: Prevalence, relationships and explanatory model in the general population of seven Latin American countries. Frontiers in Psychology, 12, 695989. 10.3389/fpsyg.2021.695989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Valencia P. D., Vilca L. W., Carbajal-León C., Vivanco-Vidal A., Saroli-Araníbar D., Reyes-Bossio M., White M., Rojas-Jara C., Polanco-Carrasco R., Gallegos M., Cervigni M., Martino P., Palacios D. A., Moreta-Herrera R., Samaniego-Pinho A., Lobos Rivera M. E., Ferrari I. F., Flores-Mendoza C., Intimayta-Escalante C. (2022. a). Prevalence and predictors of intention to be vaccinated against COVID-19 in thirteen Latin American and Caribbean countries. Trends in Psychology, 1–25. 10.1007/s43076-022-00170-x [DOI] [Google Scholar]
- Caycho-Rodríguez T., Ventura-León J., Valencia P. D., Vilca L. W., Carbajal-León C., Reyes-Bossio M., Delgado-Campusano M., Rojas-Jara C., Polanco-Carrasco R., Gallegos M., Cervigni M., Martino P., Palacios D. A., Moreta-Herrera R., Samaniego-Pinho A., Elías Lobos Rivera M., Figares A. B., Puerta-Cortés D. X., Corrales-Reyes I. E., Petzold O. (2022. b). Network analysis of the relationships between conspiracy beliefs towards COVID-19 vaccine and symptoms of fear of COVID-19 in a sample of Latin american countries. Current Psychology, 1–16. 10.1007/s12144-022-03622-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Valencia P. D., Ventura-León J., Vilca L. W., Carbajal-León C., Reyes-Bossio M., White M., Rojas-Jara C., Polanco-Carrasco R., Gallegos M., Cervigni M., Martino P., Palacios D. A., Moreta-Herrera R., Samaniego-Pinho A., Lobos-Rivera M. E., Figares A. B., Puerta-Cortés D. X., Corrales-Reyes I. E., Petzold O. (2022. c). Design and cross-cultural invariance of the COVID-19 vaccine conspiracy beliefs scale (COVID-VCBS) in 13 Latin American countries. Frontiers in Public Health, 10, 908720. 10.3389/fpubh.2022.908720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Ventura-León J., Valencia P. D., Vilca L. W., Carbajal-León C., Reyes-Bossio M., White M., Rojas-Jara C., Polanco-Carrasco R., Gallegos M., Cervigni M., Martino P., Palacios D. A., Moreta-Herrera R., Samaniego-Pinho A., Lobos Rivera M. E., Buschiazzo Figares A., Puerta-Cortés D. X., Corrales-Reyes I. E., Petzold O. (2022. d). What is the support for conspiracy beliefs about COVID-19 vaccines in Latin America? A Prospective exploratory study in 13 countries. Frontiers in Psychology, 13, 855713. 10.3389/fpsyg.2022.855713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Gallegos M., Valencia P. D., Vilca L. W., Moreta-Herrera R., Puerta-Cortés D. X., Pinto Tapia B. (2022. e). Creencias en teorías conspirativas sobre vacunas COVID-19 en la Comunidad Andina de Naciones. Boletín de Malariología y Salud Ambiental, 62(2), 123–128. [Google Scholar]
- Caycho-Rodríguez T., Gallegos M., Valencia P. D., Vilca L. W. (2022. f) ¿Cuánto apoyan los peruanos las creencias de conspiración sobre las vacunas contra la COVID-19? Atención Primaria, 54(5), 102318. 10.1016/j.aprim.2022.102318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caycho-Rodríguez T., Valencia P. D., Vilca L. W., Cervigni M., Gallegos M., Martino P., Barés I., Calandra M., Rey Anacona C. A., López-Calle C., Moreta-Herrera R., Chacón-Andrade E. R., Lobos-Rivera M. E., Del Carpio P., Quintero Y., Robles E., Panza Lombardo M., Gamarra Recalde O., Buschiazzo Figares A., Burgos Videla C. (2022. g). Cross-cultural measurement invariance of the fear of COVID-19 scale in seven Latin American countries. Death Studies, 46(8), 2003–2017. 10.1080/07481187.2021.1879318 [DOI] [PubMed] [Google Scholar]
- Cheung G. W., Rensvold R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9(2), 235–255. 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Colwell S. R. (2016). The composite reliability calculator. Technical Report. 10.13140/RG.2.1.4298.088 [DOI] [Google Scholar]
- Deng L., Chan W. (2017). Testing the difference between reliability coefficients alpha and omega. Educational and Psychological Measurement, 77(1), 185–203. 10.1177/0013164416658325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. (2020). Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine, 38(45), 7002–7006. 10.1016/j.vaccine.2020.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. A. (2013). Vaccine hesitancy: An overview. Human Vaccines & Immunotherapeutics, 9(8), 1763–1773. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhardt J., Ling J. (2021). Predicting COVID-19 vaccination intention using protection motivation theory and conspiracy beliefs. Vaccine, 39(42), 6269–6275. 10.1016/j.vaccine.2021.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahimi O. V., Hoffart A., Johnson S. U. (2021). Physical distancing and mental health during the COVID-19 pandemic: Factors associated with psychological symptoms and adherence to pandemic mitigation strategies. Clinical Psychological Science, 9(3), 489–506. 10.1177/2167702621994545 [DOI] [Google Scholar]
- Fan C. W., Chen I. H., Ko N. Y., Yen C. F., Lin C. Y., Griffiths M. D., Pakpour A. H. (2021). Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Human Vaccines & Immunotherapeutics, 17(10), 3413–3420. 10.1080/21645515.2021.1933687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher K. A., Bloomstone S. J., Walder J., Crawford S., Fouayzi H., Mazor K. M. (2020). Attitudes toward a potential SARS-CoV-2 vaccine: A survey of US adults. Annals of Internal Medicine, 173(12), 964–973. 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D., Loe B. S., Chadwick A., Vaccari C., Waite F., Rosebrock L., Jenner L., Petit A., Lewandowsky S., Vanderslott S., Innocenti S., Larkin M., Giubilini A., Yu L. M., McShane H., Pollard A. J., Lambe S. (2020). COVID-19 vaccine hesitancy in the UK: The oxford coronavirus explanations, attitudes, and narratives survey (oceans) II. Psychological Medicine, 52(14), 3127–3141. 10.1017/S0033291720005188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., Botelho-Nevers E. (2021). Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross-sectional survey. Journal of Hospital Infection, 108, 168–173. 10.1016/j.jhin.2020.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaddar A., Khandaqji S., Awad Z., Kansoun R. (2022). Conspiracy beliefs and vaccination intent for COVID-19 in an infodemic. PloS One, 17(1), e0261559. 10.1371/journal.pone.0261559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harring J. R., McNeish D. M., Hancock G. R. (2017). Using phantom variables in structural equation modeling to assess model sensitivity to external misspecification. Psychological Methods, 22(4), 616–631. PMID: 29265846. 10.1037/met0000103 [DOI] [PubMed] [Google Scholar]
- Head K. J., Kasting M. L., Sturm L. A., Hartsock J. A., Zimet G. D. (2020). A national survey assessing SARS-CoV-2 vaccination intentions: Implications for future public health communication efforts. Science Communication, 42(5), 698–723. 10.1177/1075547020960463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidaka Y., Sasaki N., Imamura K., Tsuno K., Kuroda R., Kawakami N. (2021). Changes in fears and worries related to COVID-19 during the pandemic among current employees in Japan: A 5-month longitudinal study. Public Health, 198, 69–74. 10.1016/j.puhe.2021.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Bentler P. M. (1999). Cut-off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modelling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jolley D., Douglas K. M. (2014). The effects of anti-vaccine conspiracy theories on vaccination intentions. PloS One, 9(2), e89177. 10.1371/journal.pone.0089177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovančević A., Milićević N. (2020). Optimism-pessimism, conspiracy theories and general trust as factors contributing to COVID-19 related behavior–A cross-cultural study. Personality and Individual Differences, 167, 110216. 10.1016/j.paid.2020.110216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (2016). Principles and practice of structural equation modeling .The Guilford Press. [Google Scholar]
- Larsen E. M., Donaldson K. R., Liew M., Mohanty A. (2021). Conspiratorial thinking during COVID-19: The roles of paranoia, delusion-proneness, and intolerance of uncertainty. Frontiers in Psychiatry, 12, 698147. 10.3389/fpsyt.2021.698147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J. V., Ratzan S. C., Palayew A., Gostin L. O., Larson H. J., Rabin K., Kimball S., El-Mohandes A. (2021). A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine, 27(2), 225–228. 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowsky S., Gignac G. E., Oberauer K. (2013). The role of conspiracist ideation and worldviews in predicting rejection of science. PloS One, 8(10), e75637. 10.1371/journal.pone.0075637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C. Y., Hou W. L., Mamun M. A., Aparecido da Silva J., Broche‐Pérez Y., Ullah I., Masuyama A., Wakashima K., Mailliez M., Carre A., Chen Y. P., Chang K. C., Kuo Y. J., Soraci P., Scarf D., Broström A., Griffiths M. D., Pakpour A. H. (2021). Fear of COVID‐19 Scale (FCV‐19S) across countries: Measurement invariance issues. Nursing Open, 8(4), 1892–1908. 10.1002/nop2.855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N. E. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- McDonald R. P. (1999). Test theory: A unified treatment .Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Mehta V. (2020). The new proxemics: COVID-19, social distancing, and sociable space. Journal of Urban Design, 25(6), 669–674. 10.1080/13574809.2020.17852 [DOI] [Google Scholar]
- Milfont T. L., Fischer R. (2010). Testing measurement invariance across groups: Applications in cross-cultural research. International Journal of Psychological Research, 3(1), 111–130. 10.21500/20112084.857 [DOI] [Google Scholar]
- Moya-Salazar J., Cañari B., Contreras-Pulache H. (2022). How much fear of COVID-19 is there in Latin America? A Prospective exploratory study in six countries. Electronic Journal of General Medicine, 19(1), em339. 10.29333/ejgm/11401 [DOI] [Google Scholar]
- Naveed M. A., Malik A., Mahmood K. (2021). Impact of conspiracy beliefs on Covid-19 fear and health protective behavior: a case of university students. Library Hi Tech, 39(3), 761–775. 10.1108/LHT-12-2020-0322 [DOI] [Google Scholar]
- Newheiser A. K., Farias M., Tausch N. (2011). The functional nature of conspiracy beliefs: Examining the underpinnings of belief in the Da Vinci Code conspiracy. Personality and Individual Differences, 51(8), 1007–1011. 10.1016/j.paid.2011.08.011 [DOI] [Google Scholar]
- Ogilvie G. S., Gordon S., Smith L. W., Albert A., Racey C. S., Booth A., Gottschlich A., Goldfarb D., Murray M. C. M., Sadarangani M. (2021). Intention to receive a COVID-19 vaccine: Results from a population-based survey in Canada. BMC Public Health, 21(1), 1–14. 10.1186/s12889-021-11098-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver J. E., Wood T. (2014). Medical conspiracy theories and health behaviors in the United States. JAMA Internal Medicine, 174(5), 817–818. 10.1001/jamainternmed.2014.190 [DOI] [PubMed] [Google Scholar]
- Our World in Data . (2022). Monkeypox. Our World in Data. https://ourworldindata.org/monkeypox [Google Scholar]
- Peng X., Liu L., Liang S., Chen J., Zhao J. (2022). Longitudinal changes in fear and anxiety among Chinese college students during the COVID-19 pandemic: A one-year follow-up study. Current Psychology, 26, 1–10. 10.1007/s12144-022-03487-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyszczynski T., Greenberg J., Solomon S. (1999). A dual-process model of defense against conscious and unconscious death-related thoughts: An extension of terror management theory. Psychological Review, 106(4), 835–845. 10.1037/0033-295X.106.4.835 [DOI] [PubMed] [Google Scholar]
- R Core Team (2021). R: A language and environment for statistical computing .R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Randolph H. E., Barreiro L. B. (2020). Herd immunity: Understanding COVID-19. Immunity, 52(5), 737–741. 10.1016/j.immuni.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiter P. L., Pennell M. L., Katz M. L. (2020). Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine, 38(42), 6500–6507. 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuken P. A., Rauchfuss F., Albers S., Settmacher U., Trautwein C., Bruns T., Stallmach A. (2020). Between fear and courage: Attitudes, beliefs, and behavior of liver transplantation recipients and waiting list candidates during the COVID‐19 pandemic. American Journal of Transplantation, 20(11), 3042–3050. 10.1111/ajt.16118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R. W. (1975). A protection motivation theory of fear appeals and attitude change1. The Journal of Psychology, 91(1), 93–114. 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- Rosseel Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Sallam M. (2021). COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 160. 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam M., Al-Sanafi M., Sallam M. (2022). A global map of COVID-19 vaccine acceptance rates per country: An updated concise narrative review. Journal of Multidisciplinary Healthcare, 15, 21–45. 10.2147/JMDH.S347669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salman M., Mallhi T. H., Tanveer N., Shehzadi N., Khan H. M., Ul Mustafa Z., Khan T. M., Hussain K., Mohamed M. S., Maqbool F., Aftab R. A., Butt M. H., Panda D. S., Alotaibi N. H., Khedr A. I. M., Alanazi A. S., Alatawi A. D., Alzarea A. I., Sulatana K., Khan Y. H. (2022). Evaluation of conspiracy beliefs, vaccine hesitancy, and willingness to Pay towards COVID-19 vaccines in six countries from Asian and African regions: A large multinational analysis. Vaccines, 10(11), 1866. 10.3390/vaccines10111866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawicki A. J., Żemojtel-Piotrowska M., Balcerowska J. M., Sawicka M. J., Piotrowski J., Sedikides C., Jonason P. K., Maltby J., Adamovic M., Agada A. M. D., Ahmed O., Al-Shawaf L., Appiah S. C. Y., Ardi R., Babakr Z. H., Bălţătescu S., Bonato M., Cowden R. G., Chobthamkit P., Zand S. (2022). The fear of COVID-19 scale: Its structure and measurement invariance across 48 countries. Psychological Assessment, 34(3), 294–310. 10.1037/pas0001102 [DOI] [PubMed] [Google Scholar]
- Scrima F., Miceli S., Caci B., Cardaci M. (2022). The relationship between fear of COVID-19 and intention to get vaccinated. The serial mediation roles of existential anxiety and conspiracy beliefs. Personality and Individual Differences, 184, 111188. 10.1016/j.paid.2021.111188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares P., Rocha J. V., Moniz M., Gama A., Laires P. A., Pedro A. R., Dias S., Leite A., Nunes C. (2021). Factors associated with COVID-19 vaccine hesitancy. Vaccines, 9(3), 300. 10.3390/vaccines9030300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens M. (2020). A geospatial infodemic: Mapping Twitter conspiracy theories of COVID-19. Dialogues in Human Geography, 10(2), 276–281. 10.1177/2043820620935683 [DOI] [Google Scholar]
- Tanaka J. S. (1993). Multifaceted conceptions of fit in structural equation models. In Bollen K. A., Long J. S. (Ed.), Testing structural equation models (pp. 10–39). Sage. [Google Scholar]
- van Prooijen J. W., Douglas K. M. (2018). Belief in conspiracy theories: Basic principles of an emerging research domain. European Journal of Social Psychology, 48(7), 897–908. 10.1002/ejsp.2530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma P., Junge M., Meaklim H., Jackson M. L. (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 109, 110236. 10.1016/j.pnpbp.2020.110236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Kim S. (2021). The paradox of conspiracy theory: The positive impact of beliefs in conspiracy theories on preventive actions and vaccination intentions during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(22), 11825. 10.3390/ijerph182211825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirawan G. B. S., Mahardani P. N. T. Y., Cahyani M. R. K., Laksmi N. L. P. S. P., Januraga P. P. (2021). Conspiracy beliefs and trust as determinants of COVID-19 vaccine acceptance in Bali, Indonesia: Cross-sectional study. Personality and Individual Differences, 180, 110995. 10.1016/j.paid.2021.110995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L. P., Alias H., Danaee M., Ahmed J., Lachyan A., Cai C. Z., Lin Y., Hu Z., Tan S. Y., Lu Y., Cai G., Nguyen D. K., Seheli F. N., Alhammadi F., Madhale M. D., Atapattu M., Quazi-Bodhanya T., Mohajer S., Zimet G. D., Zhao Q. (2021). COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: A global survey of 17 countries. Infectious Diseases of Poverty, 10(1), 1–14. 10.1186/s40249-021-00900-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2021. a). Draft landscape and tracker of COVID-19 candidate vaccines. World Health Organization. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines [Google Scholar]
- World Health Organization . (2021. b). Ten threats to global health in 2019. World Health Organization. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 [Google Scholar]
- Yahaghi R., Ahmadizade S., Fotuhi R., Taherkhani E., Ranjbaran M., Buchali Z., Jafari R., Zamani N., Shahbazkhania A., Simiari H., Rahmani J., Yazdi N., Alijani H., Poorzolfaghar L., Rajabi F., Lin C. Y., Broström A., Griffiths M. D., Pakpour A. H. (2021). Fear of COVID-19 and perceived COVID-19 infectability supplement theory of planned behavior to explain Iranians’ intention to get COVID-19 vaccinated. Vaccines, 9(7), 684. 10.3390/vaccines9070684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Luo X., Jia H. (2021). Is it all a conspiracy? Conspiracy theories and people’s attitude to COVID-19 vaccination. Vaccines, 9(10), 1051. 10.3390/vaccines9101051 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.