Abstract
Rates of electronic nicotine delivery systems (ENDS) use are exponentially increasing in youth and young adults within the United States, including Asian American, Native Hawaiian, and Pacific Islander (AANHPI) youth in Hawai‘i. Disproportionately high ENDS use rates for AANHPI youth point to the need to understand the empirical literature in this area. A systematic literature review is a prerequisite for programs effectively curbing AANHPI youths’ elevated use of ENDS. This systematic literature review examines empirical studies published between 2010-2020 on ENDS and their use as it applies to AANHPI youth. A total of 11 articles were identified using specific inclusionary and exclusionary criteria in a literature search. Studies described individual and interpersonal correlates to ENDS use. Notably, there were no published ENDS intervention studies detailed to AANHPI youth. Implications of these studies for prevention and social welfare interventions are discussed.
Keywords: vaping, electronic nicotine delivery systems, e-cigarettes, smoking, youth
Introduction
Electronic nicotine delivery systems (ENDS) products can be considered an entry nicotine product for youth that may lead to future use of more harmful tobacco products. ENDS use is considered a risk factor for future combustible cigarette (CC) use1-4 and other substances (eg, marijuana, cocaine).5,6 Over the past decade, youth use of ENDS has grown exponentially. Compared with other tobacco products, which have shown relatively unchanged or decreasing trajectories of use over the past decade, youth e-cigarette use has rapidly accelerated,7 particularly for Asian Americans (AAs), Native Hawaiians (NHs), and Pacific Islanders (PIs).8 These disproportionate rates point to the emerging need for health practitioners to address ENDS use within schools due to increased exposure from peers and communities with large Asian American, Native Hawaiian, and Pacific Islander (AANHPI) populations.8
Therefore, this study aims to systematically review the published scientific literature related to ENDS use within AANHPI adolescent and young adult populations. It is necessary to understand this existing literature to identify research gaps and guide the development of relevant prevention and cessation programs. This study used a set of inclusionary and exclusionary criteria to identify relevant studies focused on the determinants of ENDS use and ENDS-use interventions for AANHPI youth and young adults. As a new generation of smokers emerges and significant health implications associated with them, healthcare providers must be aware of ENDS use correlates to provide relevant interventions.
Definition and History of Youth ENDS Use
ENDS are non-combustible tobacco products that include a diverse group of reusable or disposable devices that use an “e-liquid”. E-liquids can contain nicotine, tetrahydrocannabinol (THC), cannabidiol (CBD), flavoring, and other chemicals that are converted to an aerosol through pod or mod systems.7,9-11 These products come in scents and flavors, such as lychee, taro, and passion fruit, that target and are attractive to AANHPI preferences.
Studies from the early 2000s found tobacco use to be a substantial problem in many AANHPI populations.12 In 2000, one-third of AA high school seniors were smokers, and more than 25% of female PI middle school youth had smoked within the past month.12,13 After 2000, health researchers began focusing on tobacco use prevalence, though these efforts predated the introduction of ENDS.10,12,14 The surge of ENDS use in the US around 2011 brought forth national ENDS surveillance efforts; however, ENDS research targeting AANHPI populations remained limited. This disparity is a significant problem since AANHPI populations represent one of the fastest-growing demographics (5.6% nationally and 14.9% in California) yet they are underrepresented in health and tobacco use research.15 Due to these gaps in the literature, it is crucial to understand and identify correlates associated with ENDS use onset to aid in establishing culturally competent programs.
In addition to well-known tobacco-linked health issues (eg, lung cancer, lipoid pneumonia, asthma), the rise in ENDS products has introduced new nicotine-related lung injuries and illnesses, such as bronchiolitis obliterans (reported in 18.8% of adolescent ENDS users), primary spontaneous pneumothorax, injuries due to exploding vape pens, and e-cigarette or vaping product use-associated lung injury (EVALI).7,9,16,17 King et al reported 2602 EVALI cases across the US and 57 confirmed deaths.7 The median age of patients diagnosed with EVALI was 24 years, and 62% of patients were 18–34 years old.7 Not only are the effects of long-term ENDS use unclear, but recent studies have shown that ENDS use is associated with severe respiratory disorders, such as COVID-19 and asthma.18-20 There is also evidence that ENDS use onset alters youth brain reward systems, leading to a higher likelihood of future tobacco and other drug use.5,15,21-23
Recent surveillance data indicates the need to understand AANHPI youth use of ENDS. For example, 30.6% of all middle school youth in Hawai‘i reported lifetime use of an ENDS product, ranking first nationally among all states collecting middle school data.10 Of these youth, 45.4% were NH or other Pacific Islanders (OPI), and 24.2% were Asian, representing the highest ENDS use among major ethnic groups in Hawai‘i. When assessed as a single group, AANHPI youth expressed higher usage rates than all other racial/ethnic groups.24 However, AANHPI subgroups have differing reasons for ENDS smoking onset and prolonged usage, such as the availability of e-liquid flavors targeted towards Asian cultures, nicotine highs, and as a quit-aid for CCs.24,25
A current understanding of ENDS use patterns in AANHPI youth populations will lead to more effective, culturally relevant intervention programs for these youth. Thus, this study aims to examine the literature related to ENDS use within AANHPI youth and young adult populations residing in the US and the US-Affiliated Pacific Islands (USAPI). Using established procedures for systematic literature reviews (ie, Preferred Reporting Items for Systematic Reviews and Meta-Analyses, or PRISMA26; see Figure 1), this peer-reviewed literature review focuses on the correlates of ENDS use, interventions to reduce its use, and implications for AANHPI communities.
Figure 1.
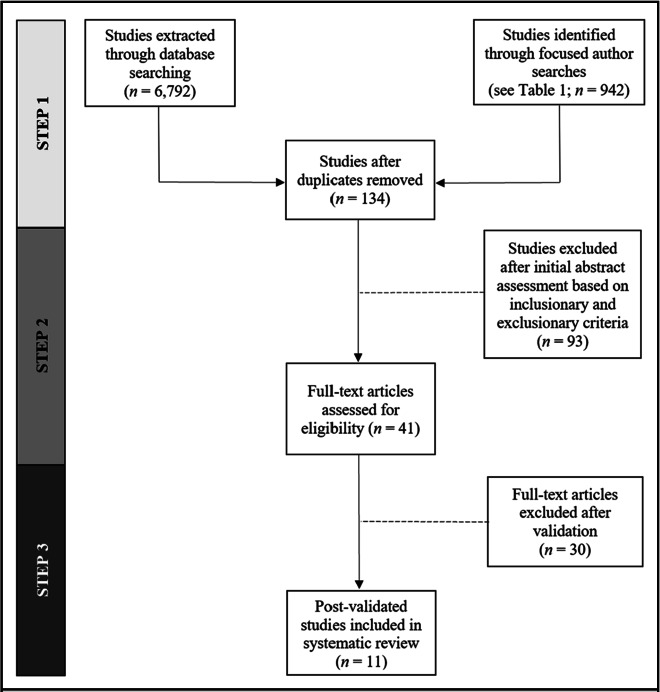
PRISMA Diagram of Study Identification and Selection
Method
Figure 1 illustrates the literature search and review process for identifying articles for this review. In Step 1, a systematic search was conducted using 2 primary methods: (1) a computerized database search using keywords, and (2) a focused author search. For the computerized database search, the databases that were included were PubMed, PsycNet (which includes PsycArticles and PsycInfo), and a focused author search through Hawai‘i Pacific University’s search engine, which pulls from a multitude of databases. All databases used were searched using key terms; “smoking”, “e-cigarette”, “Pacific Islander”, “Asian American”, “youth”, and “young adult”. The term “smoking” was used in the primary search, due to its broad inclusion of studies with both CCs and ENDS. Additionally, the articles were filtered to include publication dates from 2010-2020, which coincides with the national increase in ENDS usage among youth. To expand the search perimeter, smoking and e-cigarette derivatives were included as search terms (eg, “ENDS”, “vaping”, “vape”). For the focused author search, the names of 15 known AANHPI tobacco researchers were used: Kevin Cassel, Trenette Clark, Richard Hofstette, Jimi Huh, Seo-Ryung Kim, Adam Leventhal, Annette Maxwell, Sung See Moon, Pallav Pokhrel, Christopher Rogers, Andrew Subica, Sora Park Tanjasiri, Jennifer Unger, Thomas Wills, and Shu-Hong Zhu. This list was derived in collaboration with 3 senior co-authors who were established, federally funded tobacco and e-cigarette researchers.
After overlapping articles from the database searches were eliminated, in Step 2, the remaining articles were reviewed and evaluated based on the inclusionary and exclusionary criteria for this study. Articles were included in this review if the following criteria were met: (1) at least 50% of the study sample included AAs and/or PIs residing in the US or US territories (eg, Guam); (2) the study participants were between the ages of 12-29 years and/or had a mean age under 29 years; (3) the article exclusively focused on ENDS products, correlates to their use, (eg, social context, such as peer influences), and/or interventions; and (4) the article was a data-based empirical study published between 2010 and 2020. Articles were excluded from this review if: (1) the article focused on ENDS use with other substances but did not individually examine ENDS-use correlates; (2) the article was non-empirical (eg, descriptive or theoretical); or (3) the article was not peer-reviewed. This assessment excluded 93 articles, reducing the possible inclusions to 41 articles. In Step 3, the 3 primary authors screened the full text of the remaining 41 articles using the inclusionary and exclusionary criteria stated above.
Discussion
This study systematically reviewed the empirical literature focused on AANHPI ENDS use. The findings indicate that multiple individual-level and interpersonal factors affect AANHPI youth and young adult ENDS use. In particular, interpersonal factors highlight how ENDS use is influenced by significant relationships for AANHPI youth and young adults. Additional studies also examined ENDS onset for low-risk AANHPI youth and found ENDS as a gateway towards CC use for adolescents who would otherwise have been considered low-risk.1,2,28
Regarding youth ENDS interventions, the Substance Abuse and Mental Health Services Administration29 described 6 universal ENDS-focused prevention interventions for youth that were exclusively educational.29 However, these studies focused on something other than school or community-based ENDS interventions for AANHPI youth. Based on the current programs available and the emphasis placed on family and community within AANHPI groups, balanced, multi-level interventions targeting different ecosystemic levels (eg, the Social-Ecological model consisting of the individual, family, and community levels) is a promising approach to reduce ENDS use among AANHPI youth and young adult populations. Based on the interpersonal correlates described in this study’s findings, these interventions should also reflect the relational context for AANHPI youth, including offers to use ENDS from family and peer influences. There is a disparity in ENDS research targeting AANHPI populations and a substantial gap in substance use and tobacco interventions for these groups. A recent systematic literature review found only 2 tobacco prevention interventions for NHPI youth published between 2010-2020, neither of which included ENDS use.30 Studies of ENDS interventions have included AANHPI youth in their samples; however, due to the relatively small AANHPI sample sizes and lack of analysis specific to AANHPI culture when developing the interventions, it is unclear if these universal interventions will be effective in curbing ENDS use for AANHPI youth populations.31,32
PI youth, not including NH youth, are still one of the most underrepresented groups in empirical studies examining ENDS use. Of the ENDS studies that included PI youth in their samples, the number of participants were often so low that researchers were unable to draw definitive conclusions regarding youth ENDS and tobacco use. From the studies included in this review, 50% evaluated NHs separately from AAs. However, they also grouped specific PI populations with AAs or in the broader category of “other Pacific Islanders”. Historically, researchers have combined AAs and PIs in their sample demographics and data analyses, obscuring rates of physical disorders and mental health issues.33 Notably, AAs, PIs, and NHs all belong to distinct cultural groups that vary greatly in regards to their within-group cultural, linguistic, and socioeconomic differences, as well as their interaction with their environments.33 Data and information specific to distinct AA, PI, and NH subgroups are necessary to guide the development of culturally relevant interventions for different AA, PI, and NH communities.
Implications for Practice and Future Research
The primary purpose of this study was to systematically review the published scientific literature related to ENDS use within AANHPI adolescent and young adult populations. Additionally, this work provides insight into what has been published in the area and identifies correlates within the resulting literature. In the process of finding relevant articles on this subject, a significant gap in published works was discovered concerning research interventions for these groups. This study also points to the need for further research and culturally relevant, evidence-based interventions or prevention programs focused on ENDS use for AANHPI youth populations. Culturally relevant drug prevention programs for AANHPI youth that draw upon evidence-based principles and practices have shown significant effects on curbing alcohol, tobacco and other drug use.34,35 However, not enough research has been conducted specifically on ENDS use across a broader cross-section of AANHPIs,36 which may limit the ability to develop effective, culturally relevant ENDS interventions for AANHPI youth.
Understanding cultural and ethnic differences in correlates and determinants of ENDS use in AANHPI youth is an essential component to the development of successful interventions and culturally competent practice in a variety of settings (eg, schools, community agencies, policy settings, and case management). The findings from this study indicate the need for further research in the field of prevention and the development of research-based methods to intervene successfully with ethnically diverse populations. Future research should also address ENDS use, ENDS determinants, and ENDS uses as an entry for other illicit substances.
Although there are large gaps in intervention research on AANHPI youth ENDS use, there are promising research projects in the very early stages of development and evaluation. For example, 1 project specifically targeting PI youth is funded through the National Cancer Institute. Entitled Adolescent Tobacco and Areca Nut Use Prevention in Guam (U54CA143727), this project (referred to as the Guam Study) aims to develop a culturally grounded, evidence-based CC, ENDS, and betel nut prevention program that can be utilized in schools across the USAPI.3 Culturally grounded ENDS prevention focused on Marshallese and Chamorro youth populations in the Guam Study can be used to identify core prevention components that can be adapted to other PI subgroups and implemented by school social workers or psychologists in the Pacific region. Overall, more ENDS research is indicated for AANHPI youth populations, including studies using a multi-level approach to intervene at the individual, familial, and societal levels to address AANHPI youth ENDS use.
Limitations
Findings were limited in this literature review to the most recent decade (2010-2020), to coincide with the emergence of youth ENDS use. This may have left out other relevant studies prior to 2010, articles in their early (pre-publication) stages, and any unpublished manuscripts. With the exception of 1 study, all took place in either California or Hawai‘i, which have the highest concentrations of AANHPIs. Generalizations of the findings with this population may not apply to other US regions. Many studies in this review combined AAs, PIs, and NHs in their study samples, which can be misleading due to the subgroup differences in culture, values, and beliefs. Finally, we employed a stringent criterion for inclusion of studies in our review (ie, study samples of 50% or more AANHPIs), in order to ensure that study findings were focused on and relevant to AANHPI youth. This criterion may have eliminated broader surveillance studies with secondary or supplemental findings relevant to AANHPI youth.
Conclusions
Evidence concerning the association between ENDS use and individual or interpersonal correlates among AANHPI adolescents and young adults is growing, but still limited. Eleven empirical articles on a range of correlates to AANHPI ENDS use were identified in this systematic review. Of these 11 studies, social and familial influences were highly correlated with ENDS product use. ENDS use remains the most prevalent form of smoking in early adolescence in the US, including within Hawai‘i,10 and disproportionately impacts AANHPI communities.8,36 Developing empirically informed ENDS interventions focused on AANHPI youth populations will address ENDS use disparities.
Table 1.
Studies Included in the Systematic Literature Review of Electronic Nicotine Delivery Systems Among AANHPI Youth
| Study | Age Range (M age) | Race/Ethnicity | Study Design (N) | ENDS Type(s) | Correlate(s) | Description | Major Finding(s) |
|---|---|---|---|---|---|---|---|
| Maglalang et al. (2016) | 18–25 (21.0) | FIL, CHI, VIE, MAAPI, OAAPI | QUAN (501) | VP, EH | Awareness of ENDS from various sources, perceived ENDS harm, demographics, flavors | Study explored associations between ENDS use and awareness and perceived risks | ENDS use was associated with awareness of ENDS through peers, low perceived risk, and particular ethnic backgrounds. |
| Maglalang et al. (2019) | 19–34 (25) | CHI, FIL, THA, VIE, MAR | QUAL (12) | E-CIG | Perceived ENDS harm, cultural, familial, and peer acceptance | Study examined ENDS usage, health perception, and culture | Five major themes emerged: perceived health benefits, perceived as less harmful, de-stigmatization among family and peers, variety of options and familiarity with e-juice flavors, and popularity of cloud-chasing. |
| Pokhrel et al. (2014) | 18–40 (23.5) | AA, AFA, FIL, HIS, NHPI, WHI | QUAN (307) | E-CIG | Outcome expectancies, race/ethnicity, age | Examined participant characteristics, and E-CIG susceptibility, outcome expectancies, and use | Current and past 30-day CC smoking was positively associated with positive expectancies while inverse relationships were found with negative expectancies. Older age and Filipino background were associated with E-CIG use. |
| Pokhrel,… Fagen (2015) | 18–35 (25.1) | AA, AFA, FIL, HIS, NHPI, WHI | QUAL (62) | E-CIG | Reasons for liking and not liking E-CIGs | Explored the reasons ENDS users liked and disliked E-CIGs | Four major themes emerged: perceptions that E-CIGs are safer than CCs, benefits related to vaping, flavor advantages, and use for recreational purposes. |
| Pokhrel,… Regmi, & Fagen (2015) | 18–35 (25.1) | AA, AFA, FIL, HIS, NHPI, WHI | QUAL (62) | E - C I G , CC | Contexts when CCs and E-CIGs are used | Explored the contexts surrounding CC and E-CIG use in dual users | CCs and E-CIGs were used during select activities (eg, before/after a meal). CCs were used for craving or stimulation, in certain locations (eg, being outdoors), and with other substances. E-CIGs were used when CCs were unavailable or unable to be used. |
| Subica et al. (2020) | 18–30 (23.6) | SAM, MAR | QUAN (143) | E - C I G , CC | Outcome expectancies, gender, race/ethnicity | Explored risk factors associated with E-CIG use | Positive outcome, but not negative, expectancies, were associated with current E-CIG use. Men were more likely to report CC use and SAMs were more likely to report ever using E-CIGs and reported higher positive and negative expectancies. |
| Schweitzer et al. (2017) | N/A (15.8) | AI, AN, AFA, FIL, NH, OPI, JAP, OA, WHI | QUAN (6089) | E - C I G , CC, MJ | E-CIG use, age, gender, ethnicity, weight (body mass index) | Examined the relationship between E-CIG use and asthma | Those who reported having asthma (ever or current) was associated significantly with E-CIG, CC, and MJ use. |
| Wills et al. (2015) | N/A (14.6) | CHI, JAP, KA, FIL, WHI, NH, SAM, TONG, AFA, HIS | QUAN (1941) | E - C I G, CC | Psychosocial risk and protective variables (eg, parental support, peer smoking, sensation seeking) | Examined E-CIG and CC use to determine risk factors for discriminate user categories | Dual users (17% of sample) and CC users (12%) had the highest risk status (elevated on risk factors and lower on protective factors). E-CIG users were higher on risk status than nonusers but lower than dual users. E-cigarette and dual users perceived E-CIGs as healthier than CCs compared to non-users. |
| Wills, Sargent, Gibbons, et al. (2016) | N/A (14.7) | CHI, JAP, KA, FIL, NH, OPI, WHI, OTH | QUAN (1136) | E - C I G, CC | E-CIG use, rebelliousness, parental support, and willingness to smoke, ethnicity | Studied whether E-CIG use onset differs for youth who are at low- vs. high-risk of smoking | Findings suggested that E-CIG use was a risk factor for future CC use among those who had never smoked previously. WHI populations, FILs, NHs, and those from other backgrounds were more likely to begin smoking than AA’s. |
| Wills, Sargent, Knight, et al. (2016) | N/A (14.7) | CHI, JAP, KA, FIL, NH, OPI, WHI, OTH | QUAN (2309) | E - C I G, CC | Age, ethnicity, parent support/ monitoring, parent-adolescent conflict, rebelliousness, willingness to use CC, smoking expectancies, peer smoking | Examined the relation between E-CIG use, willingness to smoke CCs, and social-cognitive factors that predict smoking CCs | Those who had used E-CIGs had a greater willingness to use CCs. This relation was partly mediated through positive expectancies about smoking. Parent-adolescent conflict and parental monitoring also predicted willingness to smoke CC. Willingness was associated with future CC onset. |
| Wills et al. (2017) | 14–16 (14.7) | CHI, JAP, KA, FIL, NH, OPI, WHI, OTH | QUAN (2338) | E - C I G, CC | CC smoking onset, gender, ethnicity, age, rebelliousness, sensation seeking, parental support and monitoring, parental education | Examined relationship between E-CIG use and future CC smoking, as well as predictors of future E-CIG uptake | E-CIG use was a risk factor for future CC use. WHI populations and NHs were at higher risk for E-CIG uptake. |
Table 1. Note: Race/Ethnicity: AA = Asian American, AI = American Indian, AN = Alaskan Native, AFA = African American, PI = Pacific Islander, AFA = African American, WHI = White, HIS = Hispanic, KA = Korean American, FIL = Filipino, CHI = Chinese, VIE = Vietnamese, THA = Thai, JAP = Japanese, CHU = Chuukese, SAM = Samoan, TONG = Tongan, MAR = Marshallese, NH = Native Hawaiian, NHPI = Native Hawaiian/Pacific Islander, NH = Native Hawaiian, MAAPI = Mixed Asian American Pacific Islander, OAAPI = Other Asian American Pacific Islander, OA = Other Asian, OPI = Other Pacific Islander, MPI = Mixed Pacific Islander, MR = Mixed Race, OTH = Other.
Study Design: QUAL = Qualitative, QUAN = Quantitative
Tobacco Type: E-CIG = Electronic Cigarette, CC = Combustible Cigarette, VP = Vape pen, EH = E-hookah, MJ = Marijuana
Other: N/A = not available
Acknowledgement
This study was supported by funding from the National Institutes of Health/National Institute on Drug Abuse (R34 DA046735, R01 DA054215; PIs: Okamoto), National Institutes of Health/National Institute on General Medical Sciences (U01 GM138435; MPIs: Horgen and Okamoto), and the National Institutes of Health/National Cancer Institute (R01 CA228905, R01 CA202277; PIs: Pokhrel).
Abbreviations and Acronyms
- AA
Asian American
- AANHPI
Asian American, Native Hawaiian, and Pacific Islander
- CBD
cannabidiol
- CC
combustible cigarettes
- ENDS
electronic nicotine delivery systems
- NH
Native Hawaiian
- PI
Pacific Islander
- THC
tetrahydrocannabinol
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2016;26((1)):34–39. doi: 10.1136/tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wills TA, Sargent JD, Knight R, Pagano I, Gibbons FX. E-cigarette use and willingness to smoke: A sample of adolescent non-smokers. Tob Control. 2015;25((e1)):e52–59. doi: 10.1136/tobaccocontrol-2015-052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wills TA, Sargent JD, Gibbons FX, Pagano I, Schweitzer R. E-cigarette use is differentially related to smoking onset among lower risk adolescents. Tob Control. 2016;26((5)):534–539. doi: 10.1136/tobaccocontrol-2016-053116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pokhrel P, Little MA, Fagan P, Muranaka N, Herzog TA. Electronic cigarette use outcome expectancies among college students. Addict Behav. 2014;39((6)):1062–1065. doi: 10.1016/j.addbeh.2014.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pokhrel P, Fagan P, Kawamoto CT, Okamoto SK, Herzog TA. Predictors of marijuana vaping onset and escalation among young adults. Drug Alcohol Depend. 2020;216:108320. doi: 10.1016/j.drugalcdep.2020.108320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Subica AM, Guerrero E, Wu L-T, Aitaoto N, Iwamoto D, Moss HB. Electronic cigarette use and associated risk factors in U.S.-dwelling pacific islander young adults. Subst Use Misuse. 2020;55((10)):1702–1708. doi: 10.1080/10826084.2020.1756855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King BA, Jones CM, Baldwin GT, Briss PA. The EVALI and youth vaping epidemics — implications for public health. N Engl J Med. 2020;382((8)):689–691. doi: 10.1056/nejmp1916171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson AM, Unger JA, Sorensen G. E-cigarette use among Asian American, Native Hawaiian, and Pacific Islander youth in the United States. J Adolesc Health. 2019;67((3)):416–420. doi: 10.1016/j.jadohealth.2019.07.019. [DOI] [Google Scholar]
- 9.United States Food and Drug Administration Tips to help avoid “vape” battery explosions. Accessed September 9, 2020. https://www.fda.gov/tobacco-products/products-ingredients-components/tips-help-avoid-vape-battery-explosions.
- 10.Center for Disease Control and Prevention . GA: U.S. Department of Health & Human Services; 1995-2019 Middle school youth risk behavior survey data Atlanta. Accessed September 9, 2020. http://nccd.cdc.gov/youthonline/. [Google Scholar]
- 11.U.S. Department of Health and Human Services E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2016. Accessed September 9, 2020. https://www.ncbi.nlm.nih.gov/books/NBK538680/
- 12.Lew R, Tanjasiri SP. Slowing the epidemic of tobacco use among Asian Americans and Pacific Islanders. Am J Public Health. 2003;93((5)):764–768. doi: 10.2105/ajph.93.5.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Appleyard J, Messeri P, Haviland ML. Smoking among Asian American and Hawaiian/Pacific Islander youth: Data from the 2000 national youth tobacco survey. Asian Am Pac Isl J Health. 2001;9((1):):5–14. [PubMed] [Google Scholar]
- 14.Kim SS, Ziedonis D, Chen K. Tobacco use and dependence in Asian American and Pacific Islander adolescents: A review of the literature. J Ethn Subst Abuse. 2007;6((3)):113–142. doi: 10.1300/J233v06n03_05. [DOI] [PubMed] [Google Scholar]
- 15.Romero DR, Pulvers K. Cigarette smoking among Asian American and Pacific Islander college students. Health Promot Pract. 2013;14((5 Suppl)):61S–9S. doi: 10.1177/1524839913482923. [DOI] [PubMed] [Google Scholar]
- 16.Broderick SR. What does vaping do to your lungs? Johns Hopkins Medicine. 2021. Accessed September 9, 2020. https://www.hopkinsmedicine.org/health/wellness-and-prevention/what-does-vaping-do-to-your-lungs.
- 17.Galderisi A, Ferraro VA, Caserotti M, Quareni L, Perilongo G, Baraldi E. Protecting youth from the vaping epidemic. Pediatr Allergy and Immunol. 2020;31((S26)):66–68. doi: 10.1111/pai.13348. [DOI] [PubMed] [Google Scholar]
- 18.Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67((4)):519–523. doi: 10.1016/j.jadohealth.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wills TA, Pagano I, Williams RJ, Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend. 2019;194:363–370. doi: 10.1016/j.drugalcdep.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schweitzer RJ, Wills TA, Tam E, Pagano I, Choi K. E-cigarette use and asthma in a multiethnic sample of adolescents. Prev Med. 2017;105:226–231. doi: 10.1016/j.ypmed.2017.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhalerao A, Sivandzade F, Archie SR, Cucullo L. Public health policies on e-cigarettes. Current Cardiology Reports. 2019;21((10)):111. doi: 10.1007/s11886-019-1204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCausland K, Maycock B, Leaver T, Jancey J. The messages presented in electronic cigarette-related social media promotions and discussion: Scoping review. J Med Internet Res. 2019;21((2)) doi: 10.2196/11953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: A qualitative study. Psychol Health. 2015;30((12)):1450–1469. doi: 10.1080/08870446.2015.1061129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maglalang DD, Brown-Johnson C, Prochaska JJ. Associations with e-cigarette use among Asian American and pacific islander young adults in California. Prev Med Rep. 2016;4:29–32. doi: 10.1016/j.pmedr.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maglalang DD, Le M-N, Yoo GJ, Del Mundo GO. Personal motivations of Asian Americans who use ENDS: A qualitative study. Am J Health Behav. 2019;43((4)):680–690. doi: 10.5993/ajhb.43.4.3. [DOI] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, et al. The Prisma 2020 statement: An updated guideline for reporting systematic reviews. The BMJ. 2021 doi: 10.1136/bmj.n71.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pokhrel P, Herzog TA, Muranaka N, Regmi S, Fagan P. Contexts of cigarette and e-cigarette use among dual users: A qualitative study. BMC Public Health. 2015;15:859. doi: 10.1186/s12889-015-2198-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatr. 2015;135((1)):e43–e51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Substance Abuse and Mental Health Services Administration Reducing vaping among youth and young adults. 2020. Accessed September 7, 2020. https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-06-01-003_508_0.pdf. 2020.
- 30.Rosario MH, Johnson DL, Manglallan KS, Phillips KT, Pokhrel P, Okamoto SK. Tobacco use among native Hawaiian and Pacific Islander youth in the U.S. and USAPI: A systematic review of the literature [published online ahead of print, 2021 Aug 23] J Ethn Subst Abuse. 2021:1–16. doi: 10.1080/15332640.2021.1965934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen AB. Disaggregating Asian American and Native Hawaiian and Other Pacific Islander (AANHOPI) adult tobacco use: Findings from Wave 1 of the population assessment of tobacco and Health (PATH) study, 2013-2014. J Racial Ethn Health Disparities. 2019;6((2)):356–363. doi: 10.1007/s40615-018-00532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen AB, Henrie J, Slavit WI, Kaufman AR. Beliefs about FDA tobacco regulation, modifiability of cancer risk, and tobacco product comparative harm perceptions: Findings from the hints-FDA 2015. Prev Med. 2018;110:1–8. doi: 10.1016/j.ypmed.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaholokula JK, Okamoto SK, Yee BW. Special issue introduction: Advancing Native Hawaiian and other Pacific Islander health. Asian Am J Psychol. 2019;10((3)):197–205. doi: 10.1037/aap0000167. [DOI] [Google Scholar]
- 34.Okamoto SK, Kulis S, Helm S, Lauricella M, Valdez JK. An evaluation of the Ho’ouna Pono curriculum: A pilot study of culturally grounded substance abuse prevention for rural Hawaiian youth. J Health Care Poor Underserved. 2016;27((2)):815–833. doi: 10.1353/hpu.2016.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okamoto SK, Kulis SS, Helm S, Chin SK, Hata J, Hata E, Lee A. An efficacy trial of the Ho‘ouna Pono drug prevention curriculum: An evaluation of a culturally grounded substance abuse prevention program in rural Hawai‘i. Asian Am J Psychol. 2019;10((3)):239–248. doi: 10.1037/aap0000164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phillips KT, Okamoto SK, Johnson DL, Rosario MH, Manglallan KS, Pokhrel P. Correlates of tobacco use among Asian and Pacific Islander Youth and young adults in the U.S.: A systematic review of the literature. Exp Clin Psychopharmacol. 2021;29((5)):440–455. doi: 10.1037/pha0000511. [DOI] [PMC free article] [PubMed] [Google Scholar]


