Key Points
Question
What factors were associated with improved operative efficiency in head and neck cancer resection and reconstruction?
Findings
In this cohort study that included 578 patients with head and neck cancer over 13 years, multiple strategies were associated with a reduced operative time. However, team-based strategies, including the use of a standardized nursing team, treatment centralization, and introduction of a fellowship program, were significantly associated with a reduction in operative time.
Meaning
The results of this cohort study suggest that in head and neck cancer resection and reconstruction, team-based strategies had a stronger association with reduced operative time than other measures, including the use of new technologies or techniques.
Abstract
Importance
Head and neck oncological resection and reconstruction is a complex process that requires multidisciplinary collaboration and prolonged operative time. Numerous factors are associated with operative time, including a surgeon’s experience, team familiarity, and the use of new technologies. It is paramount to evaluate the contribution of these factors and modalities on operative time to facilitate broad adoption of the most effective modalities and reduce complications associated with prolonged operative time.
Objective
To examine the association of head and neck cancer resection and reconstruction interventions with operative time.
Design, Setting, and Participants
This large cohort study included all patients who underwent head and neck oncologic resection and free flap–based reconstruction in Calgary (Alberta, Canada) between January 1, 2007, and March 31, 2020. Data were analyzed between November 2021 and May2022.
Interventions
The interventions that were implemented in the program were classified into team-based strategies and the introduction of new technology. Team-based strategies included introducing a standardized operative team, treatment centralization in a single institution, and introducing a microsurgery fellowship program. New technologies included use of venous coupler anastomosis and virtual surgical planning.
Main Outcomes and Measures
The primary outcome was mean operative time difference before and after the implementation of each modality. Secondary outcomes included returns to the operating room within 30 days, reasons for reoperation, returns to the emergency department or readmissions to hospital within 30 days, and 2-year and 5-year disease-specific survival. Multivariate regression analyses were performed to examine the association of each modality with operative time.
Results
A total of 578 patients (179 women [30.9%]; mean [SD] age, 60.8 [12.9] years) undergoing 590 procedures met inclusion criteria. During the study period, operative time progressively decreased and reached a 32% reduction during the final years of the study. A significant reduction was observed in mean operative time following the introduction of each intervention. However, a multivariate analysis revealed that team-based strategies, including the use of a standardized nursing team, treatment centralization, and a fellowship program, were significantly associated with a reduction in operative time.
Conclusions
The results of this cohort study suggest that among patients with head and neck cancer, use of team-based strategies was associated with significant decreases in operative time without an increase in complications.
This cohort study examines the association of head and neck cancer resection and reconstruction interventions with operative time.
Introduction
Head and neck (HN) cancer ablation and reconstruction require collaboration between specialist surgeons, anesthesiologists, and nursing teams to achieve intraoperative success. However, the complexity of these procedures makes these surgeries prone to inefficiencies and increased intraoperative time. The consequence of prolonged operative time places a burden on the patient and health care system. Prolonged surgeries are associated with increased risk for postoperative complications, including septic shock, thromboembolic events, free flap failure, and wound healing complications.1,2,3
In this patient population, the formation of a clear surgical plan4 and using virtual-surgical planning4,5,6 are known to be associated with reduced operative time. In addition, using a 2-team approach,7,8 having a dedicated nursing team,9 and the use of technology (such as venous couplers10,11,12,13 or prefabricated osteotomy guides14) have all been associated with shorter operative times. The decreased operative time associated with these interventions has not been associated with an increase in postoperative complications.
Additional factors that to our knowledge have not been widely assessed and may be associated with intraoperative time are centralization of HN procedures, surgeon’s case volume, and inclusion of learners, such as residents and fellows. Literature in digital replantation suggests that centralization was associated with more successful outcomes.15,16 Conversely, studies within autologous breast reconstruction suggest the addition of residents is associated with increased intraoperative time,17 and this has been echoed in other surgical specialties.18,19,20,21 At our center (University of Calgary; Calgary, Alberta, Canada), there have been multiple changes to the HN reconstruction program during the past 15 years. These changes have included adding dedicated nursing teams for all complex HN flap reconstruction cases, treatment centralization, introducing a fellowship program, introducing new technology (including venous couplers), and virtual surgical planning. While we have anecdotally experienced an improvement in operative efficiency, the independent contributions and interactions of each variable on operative time have yet to be quantified. In this study, we sought to evaluate the association of each modality with operative time in HN cancer resection and reconstruction. The secondary goal of this study was to determine whether these aforementioned changes were associated with the rate of complications, length of stay, or readmission rates.
Methods
Patient Selection
In reporting this case series, we followed the recommendation provided by the PROCESS guidelines.22 Institutional ethics approval was granted by the health research ethics board of the Alberta Cancer Committee, which also waived consent because of the retrospective nature of our study that had minimal to no risk for participants. Data were collected retrospectively for all patients undergoing HN oncologic resection followed by immediate free-flap based reconstruction in Calgary, Alberta, Canada, between January 1, 2007, and March 31, 2020. Patients were identified and screened for study inclusion using a prospectively maintained database of patients with HN cancer. Patients were included if they underwent oncologic resection and reconstruction with 1 or more free flaps within the study period. Patients were excluded if they were younger than 18 years, did not undergo oncologic resection (eg, osteoradionecrosis), did not have a free flap–based reconstruction, or had insufficient data for subsequent analyses.
Data Collection
Data were collected from 4 databases, including Synoptec (Cancer Surgery Alberta), Sunrise Clinical Manager, OTOBASE, and Operating Room Information Systems. Information pertaining to patient demographic characteristics, tumor characteristics, surgical procedure, and postoperative complications were extracted. Patient demographic data included birth date, sex, age at time of surgery, and body mass index (calculated as weight in kilograms divided by height in meters squared) category. Data were also collected on patient smoking and alcohol history. Tumor data were collected on tumor type, tumor stage according to the American Joint Committee on Cancer at the time of surgery, and anatomic location. Surgical data included the total operative time (minutes), the tissue composition (soft tissue or bony reconstruction), flap type, number of vascular anastomoses, and vein anastomosis technique (hand-sewn or coupler use). For bony flaps, the plating technique was also collected (hand-bent intraoperatively, prebent, and custom-printed plates). For each procedure, information on the surgical teams (surgeons, specialized nursing teams, fellows present) was collected along with the hospital where the procedure was performed. Lastly, data were collected on complications, including returns to the operating room within 30 days, reasons for reoperation, returns to the emergency department or readmissions to hospital within 30 days, and 2-year and 5-year disease-specific survival. Data were stored in an encrypted password-protected database for subsequent analyses.
Factors Associated With Operative Time
Several interventions were adopted between 2007 and 2020 that can be generally classified into team-based strategies and the introduction of new technology. Team-based strategies included introducing a standardized operative team, treatment centralization in a single institution, and introducing a microsurgery fellowship program. New technologies included use of venous coupler anastomosis and virtual surgical planning.
Standardized Nursing Team
We previously reported on our early experience of using a standardized nursing team in HN cancer ablation and free flap reconstruction.9 Since May 1, 2009, an experienced nurse manager trained and managed a dedicated team of surgical nurses that would participate in every HN oncology case requiring free flap reconstruction.
Treatment Centralization
In 2012, the Calgary HN surgery clinical outcome program was established at the Foothills Medical Center (FMC), which is the largest academic teaching hospital in Alberta and serves a population of approximately 2 million people. In May 2013, all HN oncology patients within the region were referred to the FMC team for evaluation and management. Before that, 2 sites across the city were involved in HN oncology treatment.
Microsurgery Fellowship
In 2015, a microsurgical fellowship was established at the FMC in partnership with the University of Calgary. Typically, 1 microsurgery fellow joins the program every year who has already completed a plastic surgery residency. The fellow participates in every HN free flap reconstruction case along with 2 microsurgeons. Intraoperatively, the fellow assumes progressive case autonomy in flap harvest, flap inset, and microvascular anastomosis.
Introduction of New Technologies
Venous anastomosis is considered more technically challenging than arterial anastomosis. Thus, an anastomosis coupler device was developed to provide a more efficient and easier method of venous anastomosis.10 Since 2010, our group has used venous coupler devices regularly for venous anastomoses. However, we also used traditional hand-sewn techniques when vein anatomy was not suitable for coupler device (eg, end-to-side anastomosis). In this study, we examined the association of coupler device use with operative time by analyzing the difference in operative time between the coupler device and hand-sewn technique for venous anastomosis.
In addition, different plating modalities were used during the study period. Before May 2015, bone fixation was performed using the hand-bent technique, in which a reconstruction plate is bent intraoperatively based on the native mandible to achieve the best fit. After May 2015, our group adopted virtual planning systems to aid in resection and reconstruction. Initially, we used a virtual planning system to create a 3-dimensional model based on the patient’s anatomy and planned resection. This model was used to prebend the plate before the resection started. We next adopted a new plating technique with custom-made selective laser molding (SLM) plates, in which plates are printed based on preoperative imaging to match the anticipated defect after the resection has been completed.
Statistical Analysis
The statistical analyses were conducted using R, version 3.6.3 (R Foundation), using packages tidyverse23 and table 1.24 Descriptive statistics were reported to summarize demographic characteristics and tumor, surgery, site, and complication data. Continuous variables were reported using means (SDs) then compared using the mean difference and 95% CI. Changes in operative time were illustrated using process control charts in which the upper control limit (UCL) and lower control limit (LCL) were calculated using the mean and SD (UCL = mean + 3 * SD; LCL = mean − 3 * SD). Categorical variables were reported as frequencies (proportions) and compared using a χ2 or Fisher exact test when appropriate. All descriptive statistics were stratified by the pre/post variables centralization or specialized nursing team. A multivariate regression analysis was used to examine predictor variables on the continuous outcome of operative time (minutes). A variable was deemed significant if the α value was less than .05 when factored into the model.
Results
A total of 578 patients undergoing 590 procedures met the inclusion criteria for this study. The mean (SD) age of patients was 60.8 (12.9) years, and 399 (69.1%) were male (Table 1). Most patients had a smoking (370 [65.2%]) and alcohol use history (466 [67.6%]; Table 1). Most tumors were stage 3 or 4 (390 [66.1%]) and located in the oral cavity (419 [71%]) (eTable 1 in Supplement 1).
Table 1. Patient Demographic Characteristics.
| Characteristic | Overall, No. (%) (n = 578)a |
|---|---|
| Sex | |
| Female | 179 (30.9) |
| Male | 399 (69.1) |
| Age, y | |
| Mean (SD) | 60.8 (12.9) |
| Median (range) | 62.0 (19.0-89.0) |
| Smokingb | |
| Current | 172 (30.3) |
| Ex-smoker | 198 (34.9) |
| Never | 147 (25.0) |
| Alcohol intakeb | |
| Heavy | 123 (21.7) |
| Moderate | 33 (5.8) |
| Light | 157 (27.6) |
| Previous | 71 (12.5) |
| Never | 112 (19.7) |
| BMIb | |
| Normal | 148 (26.1) |
| Overweight | 120 (21.1) |
| Obesity | 84 (14.8) |
| Underweight | 24 (4.2) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
A total of 578 patients underwent a total of 590 procedures. Twelve patients underwent a second procedure.
Indicates some missing data: smoking (51 [9%]), alcohol intake (72 [12.7%]), and BMI (192 [33%]).
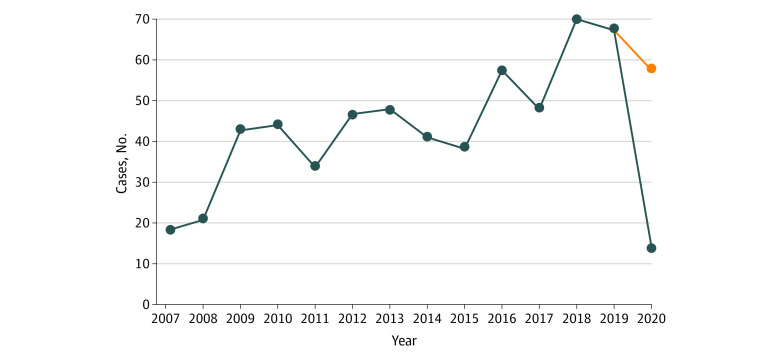
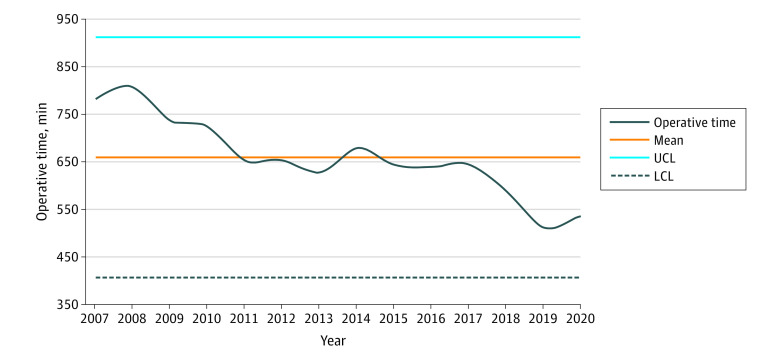
Number of Cases and Operative Time
During the study period, there was an increase of the total number in HN free flap oncologic resections and reconstructions per year, from 18 patients in 2007 to 67 patients in 2019 (Figure 1). In addition, the mean (SD) operative time decreased from nearly 13 hours (780 [133] minutes) in 2007 to less than 9 hours (534 [201] minutes) in 2020 (difference, 246 minutes; 95% CI, 146-346) (Figure 2).
Figure 1. Total Number of Cases per Year.
The orange line represents the projected number of cases in 2020.
Figure 2. Mean Operative Time per Year.
LCL indicates lower control limit; UCL, upper control limit.
Factors Associated With Operative Time
Standardized Nursing Team
Fifty-three patients (9.2%) underwent HN reconstruction before the introduction of a standardized nursing team compared with 537 patients (90.8%) after standardization. There were no statistically significant differences in age, sex, smoking and alcohol history, and tumor factors between groups (eTable 2 in Supplement 1). The mean (SD) operative time decreased after the introduction of a standardized nursing team, from nearly 13 hours (771 [120] minutes) prestandardization to 10.5 hours (630 [120] minutes) poststandardization (difference, 141 minutes; 95% CI, 107-175).
Treatment Centralization
A total of 221 patients (38.2%) underwent HN reconstruction before the introduction of HN care centralization compared with 369 patients (61.8%) after centralization. There were no statistically significant differences in patient characteristics and tumor profiles between groups (eTable 3 in Supplement 1). The mean (SD) operative time decreased after the introduction of HN care centralization, from nearly 12 hours (707 [124] minutes) precentralization to 10 hours (604 [124] minutes) postcentralization (difference, 103 minutes; 95% CI, 82-124).
Microsurgery Fellowship
Following the introduction of the microsurgery fellowship in 2015, fellows participated in 267 procedures during the study period. The mean (SD) operative time with fellow participation was much shorter than procedures without fellow participation (589 [129] minutes vs 687 [120] minutes; difference, 98 minutes; 95% CI, 78-118).
Introduction of New Technologies
Venous Coupler Devices
A total of 331 venous anastomoses (65.1%) were performed using a coupler device; 167 venous anastomoses (28.3%) were performed using a hand-sewn technique. The mean (SD) operative time was significantly shorter when a venous coupler device was used compared with a hand-sewn anastomosis (620 [165] minutes vs 670 [117] minutes; difference, 50 minutes; 95% CI, 22-78).
Plate Fixation Modalities
The analysis of plating modalities showed a trend toward a shorter operative time with the introduction of each new techniques. The use of SLM plates was associated with a reduction in operative time compared with hand-bent (mean difference, −133 minutes; 95% CI, −188 to −80) and prebent techniques (mean difference, −72 minutes; 95% CI, −129 to −15) (eTable 4 in Supplement 1).
Multivariate Analysis of Factors Associated With Operative Time
A multivariate regression model was used to identify factors associated with decreased operative time (Table 2). These factors included treatment centralization, a standardized nursing team, introduction of a fellowship program, coupler use, and the number of free flaps per case. Treatment centralization (−39.75 minutes; 95% CI, −68.07 to −47.97), standardized nursing team (−84.05 minutes; 95% CI, −119.13 to −48.97), and introduction of the fellowship program (−53.95 minutes; 95% CI, −79.44 to −28.47) were associated with large reductions in operative time. Coupler devices were associated with small reductions in operative time (−9.58 minutes; 95% CI, −29.55 to 10.39). In addition, a multivariate regression analysis of the plating technique showed a large reduction in operative time for the use of SLM (−44.23 minutes) and small reductions with use of prebent (−16.69 minutes) plates compared with the older hand-bent technique; however, wide confidence intervals prevented us from making any definitive conclusions (Table 3).
Table 2. Multivariant Analysis of Factors Associated With Operative Time for All Flaps.
| Factor | Estimates, min (95% CI) |
|---|---|
| Treatment centralization | −39.75 (−68.07 to −11.43) |
| Specialized nursing team | −84.05 (−119.13 to −48.97) |
| Fellow participation | −53.95 (−79.44 to −28.47) |
| Coupler use | −9.58 (−29.55 to 10.39) |
| Multiple free flaps | 178.31 (139.44 to 217.19) |
Table 3. Multivariant Analysis of Factors Associated With Operative Time for Osseous or Osteocutaneous Flaps.
| Factor | Estimates, min (95% CI) |
|---|---|
| Treatment centralization | −49.70 (−116.23 to 16.82) |
| Specialized nursing team | −115.29 (−147.19 to −56.39) |
| Fellow participation | −18.60 (−71.44 to 34.24) |
| Coupler use | 11.49 (−30.17 to 53.15) |
| Multiple free flaps | 139.58 (96.20 to 182.96) |
| 3-Dimensional printed plates | −44.23 (−120.99 to 32.53)a |
| Prebend technique | −16.69 (−79.98 to 46.59)a |
Compared with hand-bend technique.
Length of Stay, Return to the Emergency Department, Readmission Rates, and Survival
The mean (SD) length of stay for the cohort throughout the study period was 16.3 (21.7) days. However, the mean (SD) length of stay was shorter after treatment centralization and use of standardized nursing team, averaging 13.9 (12.4) days (mean difference, 6.4 days; 95% CI, 2.8-9.9) and 15.5 (18.6) days (mean difference, 8.1 days; 95% CI, 2.7-13.4), respectively (eTables 5 and 6 in Supplement1). Readmission rates and return to the emergency department within 30 days remained low and stable during the study period and did not differ after the introduction of centralization or a standardized nursing team (eTables 6 and 7 in Supplement 1).
There was no meaningful difference in 2-year (χ2 = 15.011; P = .13) and 5-year (χ2 = 12.739; P = .08) survival for each year between 2009 and 2019 (2-year) and 2009 and 2016 (5-year) (eTable 7 in Supplement 1).
Discussion
The results of this cohort study suggest that the improvement of efficiency and decrease in operative time for HN reconstruction followed the adoption of multiple team-based strategies and introduction of new operative technologies. However, the reduction in operative time varied with each adopted strategy and/or technology. Specifically, team-based strategies, including treatment centralization, introduction of specialized nursing team, and fellow participation, had a greater association with operative time compared with the adoption of new technologies.
Treatment centralization for high-risk surgical care has been associated with reduced postoperative morbidity and improved survival.25,26,27 High-volume institutions are associated with improved outcomes through a better understating of surgical indications, procedures, and postoperative care.28,29 In HN oncology, improved outcomes are seen after treatment is performed at high-volume institutions.30,31,32,33 However, the association of treatment centralization with operative time is less clear. In the present study, the total number of cases performed annually increased steadily after centralization. Despite the increase in volume, we observed a yearly reduction in mean operative time of approximately 1 hour and 43 minutes.
We previously reported on our early experience following the use of a standardized nursing team.9 In this earlier study, operative time decreased by an average of 47 minutes following team standardization. We have replicated these findings in the current study and have shown an improvement in operative efficiency since the initial study. Specifically, the average reduction in operative time following nursing team standardization in the current cohort was 141 minutes, nearly a 100-minute improvement since data were last collected in 2010.
The reduction in operative time associated with use of a standardized nursing team and treatment centralization, despite the increase operative volume, can be explained by the adage “practice makes perfect.” Educational psychologists have shown that many years of intense involvement and 10 000 hours of practice is required to achieve an elite level of performance.34,35 Ericsson and colleagues35 showed that these principles extend to various domains, including music, chess, and sports.36 Ericsson et al35 also demonstrated that the acquisition of superior performance in medicine is closely associated with deliberate practice and continuous feedback.36 High case volumes are also associated with significant improvements in health outcomes, including operative time.37 Therefore, if the rate of improvement is procedure-specific and outcome-specific, then deliberate practice (eg, higher volumes), feedback, and constant measurement of outcomes are paramount for improved performance.
We believe that improvement in task performance also extends to the nursing team. As the number of HN cases increased, the nursing team became more familiar with the typical operative events, and this allowed the nurses to anticipate future steps, eliminate unnecessary searches for instruments, and avoid disruptions during the procedure. Recently, Sawaf et al38 examined the association of team familiarity with reducing operative time in HN free flap reconstruction. The authors found that a consistent nursing team (circulating nurse and/or surgical technologist) was associated with a significant reduction in operative time. Team familiarity is known to be associated with improved operative time in other surgical specialties, including breast surgery39 and orthopedic surgery,40 and reduced cardiopulmonary bypass and cross clamp time in cardiac surgery.41
It is commonly acknowledged in the surgical literature that learner participation is associated with increased operative time compared with an attending surgeon alone. This has been validated across multiple specialties for selected procedures.18,19,20,21 Operative time tends to decrease as level of training increases, indicating that learners become more efficient as they gain more experience. Surprisingly, fellow participation in the current study was associated with a shorter operative time. Our fellowship program consists of 1 year of intense training in microsurgery. Fellows have already completed a plastic surgery residency and fulfilled the competency requirements for flap harvest and reconstruction. As expected, we have observed fellows who typically start slowly and become more efficient as they progress and gain experience during the fellowship year. Typically, 2 attending microsurgeons are involved during flap harvest and inset and provide additional direction and assistance to the fellow. Therefore, the addition of 2 surgical attendings may also explain the reduction in operative time despite fellow participation.
New technologies have been used in multiple surgical fields to improve operative efficiency and treatment outcomes. In microsurgical reconstruction, introducing venous couplers was associated with reductions in anastomosis time compared with hand-sewn techniques.10 However, the reduction in anastomosis time does not always translate to a reduction in operative time. For example, Heidekrueger and colleagues42 found that improvement in anastomosis time did not translate into reduction in total operative time in free flap breast reconstruction. Similar to this, the regression analyses in the current study regarding the use of venous coupler devices were not associated with a significant reduction in operative time when accounting for other variables. This finding may suggest the actual microvascular anastomosis component of the reconstructive procedure carries a lesser association with the overall operative time.
Another adopted technology into the HN cases in this study was virtual surgical planning (VSP) for maxillary and mandibular reconstruction, which allows for precise osteotomies and accurate reconstruction for osseous flaps.43,44 Several studies have shown that the use of VSP is associated with significantly reduced operative time in HN reconstruction.5,44 This study’s regression analysis did not show a significant reduction in operative time with the introduction of VSP. Since we implemented the VSP technology later in the study timeline, we hypothesize that the improvement in operative time associated with the use of VSP may have been masked by the improvement in operative time that was secondary to other factors.
Limitations
This study was not without limitations. The retrospective nature of this study carried inherited risk of recall and sampling biases. In addition, the effects of previous experiences of surgeons, the learning curve of the surgeon(s), and the effect of having surgeons responsible for either the resection or reconstruction were not fully evaluated in this study. However, given that the data represent multiple surgeons and that all surgeons on the HN team were practicing several years before the start of the study, we believe these risks to the integrity of the study to be negligible. Despite these limitations, to our knowledge this is the first large-scale study to examine the association of multiple factors with operative efficiency that is specific to HN reconstruction. The possibility of confounding factors was minimized via use of a multivariate regression analysis. Finally, throughout the length of the study, there was a consistent group of HN surgeons responsible for resection and reconstruction. Therefore, the effects demonstrated can be attributed to the specific factor investigated and not due to individual surgeon variability.
Conclusions
The results of this cohort study suggest that team-based strategies have a stronger association than the adoption of new surgical technologies with reduced operative time in HN cancer ablation and free flap reconstruction. Most importantly, the adoption of new operative strategies and decreased operative time was not associated with an increase in complications. We encourage HN operative teams to emphasize team building and proper use of existing resources to significantly improve operating time and operating room efficiency.
eTable 1. Tumor characteristics
eTable 2. Patients characteristics before and after implementation of standardized nursing team
eTable 3. Patients characteristics before and after implementation of treatment centralization
eTable 4. The effect of plating techniques on operative time (OR)
eTable 5. Secondary outcomes; length of stay (LOS), return to ED within 30 days, readmission rate
eTable 6. Effect of treatment centralization and standardized nursing team on length of stay LOS, return to ED within 30 days and readmission rate
eTable 7. 2 years and 5 years disease specific survival 2007-2020
eFigure. Secondary outcomes (30 days readmission rate, 30 days return to ER) and mean length of stay
Data sharing statement
References
- 1.Eskander A, Kang S, Tweel B, et al. Predictors of complications in patients receiving head and neck free flap reconstructive procedures. Otolaryngol Head Neck Surg. 2018;158(5):839-847. doi: 10.1177/0194599818757949 [DOI] [PubMed] [Google Scholar]
- 2.Lindeborg MM, Sethi RKV, Puram SV, et al. Predicting length of stay in head and neck patients who undergo free flap reconstruction. Laryngoscope Investig Otolaryngol. 2020;5(3):461-467. doi: 10.1002/lio2.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh B, Cordeiro PG, Santamaria E, Shaha AR, Pfister DG, Shah JP. Factors associated with complications in microvascular reconstruction of head and neck defects. Plast Reconstr Surg. 1999;103(2):403-411. doi: 10.1097/00006534-199902000-00007 [DOI] [PubMed] [Google Scholar]
- 4.Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope. 2013;123(3):597-604. doi: 10.1002/lary.23717 [DOI] [PubMed] [Google Scholar]
- 5.Tang NSJ, Ahmadi I, Ramakrishnan A. Virtual surgical planning in fibula free flap head and neck reconstruction: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2019;72(9):1465-1477. doi: 10.1016/j.bjps.2019.06.013 [DOI] [PubMed] [Google Scholar]
- 6.Toto JM, Chang EI, Agag R, Devarajan K, Patel SA, Topham NS. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck. 2015;37(11):1660-1664. doi: 10.1002/hed.23815 [DOI] [PubMed] [Google Scholar]
- 7.Torabi SJ, Chouairi F, Dinis J, Alperovich M. Head and neck reconstructive surgery: characterization of the one-team and two-team approaches. J Oral Maxillofac Surg. 2020;78(2):295-304. doi: 10.1016/j.joms.2019.09.011 [DOI] [PubMed] [Google Scholar]
- 8.Ghazizadeh S, Kuan EC, Mallen-St Clair J, et al. It takes two: one resects, one reconstructs. Otolaryngol Clin North Am. 2017;50(4):747-753. doi: 10.1016/j.otc.2017.03.010 [DOI] [PubMed] [Google Scholar]
- 9.Doherty C, Nakoneshny SC, Harrop AR, et al. A standardized operative team for major head and neck cancer ablation and reconstruction. Plast Reconstr Surg. 2012;130(1):82-88. doi: 10.1097/PRS.0b013e3182547e22 [DOI] [PubMed] [Google Scholar]
- 10.Maruccia M, Fatigato G, Elia R, et al. Microvascular coupler device versus hand-sewn venous anastomosis: a systematic review of the literature and data meta-analysis. Microsurgery. 2020;40(5):608-617. doi: 10.1002/micr.30585 [DOI] [PubMed] [Google Scholar]
- 11.Head L, McKay D. Economic comparison of hand-sutured and coupler-assisted microvascular anastomoses. J Reconstr Microsurg. 2018;34(1):71-76. doi: 10.1055/s-0037-1606540 [DOI] [PubMed] [Google Scholar]
- 12.Vernier-Mosca M, Feuvrier D, Obert L, Mauvais O, Loisel F, Pluvy I. Utilisation du coupleur pour les anastomoses veineuses en reconstruction cervico-faciale. Étude rétrospective sur 51 lambeaux libres. Ann Chir Plast Esthet. 2020;65(3):236-243. doi: 10.1016/j.anplas.2019.06.011 [DOI] [PubMed] [Google Scholar]
- 13.Dimitropoulos G, Efanov JI, Paek L, Bou-Merhi J, Danino MA. Comparison of venous couplers versus hand-sewn technique in free flap breast reconstruction. Ann Chir Plast Esthet. 2019;64(2):150-156. doi: 10.1016/j.anplas.2018.10.002 [DOI] [PubMed] [Google Scholar]
- 14.Chang EI, Jenkins MP, Patel SA, Topham NS. Long-term operative outcomes of preoperative computed tomography-guided virtual surgical planning for osteocutaneous free flap mandible reconstruction. Plast Reconstr Surg. 2016;137(2):619-623. doi: 10.1097/01.prs.0000475796.61855.a7 [DOI] [PubMed] [Google Scholar]
- 15.Brown M, Lu Y, Chung KC, Mahmoudi E. Annual hospital volume and success of digital replantation. Plast Reconstr Surg. 2017;139(3):672-680. doi: 10.1097/PRS.0000000000003087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hustedt JW, Bohl DD, Champagne L. The detrimental effect of decentralization in digital replantation in the United States: 15 years of evidence from the National Inpatient Sample. J Hand Surg Am. 2016;41(5):593-601. doi: 10.1016/j.jhsa.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 17.Wu WW, Medin C, Bucknor A, Kamali P, Lee BT, Lin SJ. Evaluating the impact of resident participation and the July effect on outcomes in autologous breast reconstruction. Ann Plast Surg. 2018;81(2):156-162. doi: 10.1097/SAP.0000000000001518 [DOI] [PubMed] [Google Scholar]
- 18.Pollei TR, Barrs DM, Hinni ML, Bansberg SF, Walter LC. Operative time and cost of resident surgical experience: effect of instituting an otolaryngology residency program. Otolaryngol Head Neck Surg. 2013;148(6):912-918. doi: 10.1177/0194599813482291 [DOI] [PubMed] [Google Scholar]
- 19.Lee SL, Sydorak RM, Applebaum H. Training general surgery residents in pediatric surgery: educational value vs time and cost. J Pediatr Surg. 2009;44(1):164-168. doi: 10.1016/j.jpedsurg.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 20.Farnworth LR, Lemay DE, Wooldridge T, et al. A comparison of operative times in arthroscopic ACL reconstruction between orthopaedic faculty and residents: the financial impact of orthopaedic surgical training in the operating room. Iowa Orthop J. 2001;21:31-35. [PMC free article] [PubMed] [Google Scholar]
- 21.Sasor SE, Flores RL, Wooden WA, Tholpady S. The cost of intraoperative plastic surgery education. J Surg Educ. 70(5):655-659. doi: 10.1016/j.jsurg.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 22.Mathew G, Agha R; STROCSS Group . STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Ann Med Surg (Lond). 2021;72:103026. doi: 10.1016/j.amsu.2021.103026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wickham H, Averick M, Bryan J, et al. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686. doi: 10.21105/joss.01686 [DOI] [Google Scholar]
- 24.Rich B. Tables of descriptive statistics in HTML. Accessed November 1, 2021. https://CRAN.R-project.org/package=table1
- 25.Williams SB, Ray-Zack MD, Hudgins HK, et al. Impact of centralizing care for genitourinary malignancies to high-volume providers: a systematic review. Eur Urol Oncol. 2019;2(3):265-273. doi: 10.1016/j.euo.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grilli R, Violi F, Bassi MC, Marino M. The effects of centralizing cancer surgery on postoperative mortality: a systematic review and meta-analysis. J Health Serv Res Policy. 2021;26(4):289-301. doi: 10.1177/13558196211008942 [DOI] [PubMed] [Google Scholar]
- 27.van Putten M, Nelen SD, Lemmens VEPP, et al. Overall survival before and after centralization of gastric cancer surgery in the Netherlands. Br J Surg. 2018;105(13):1807-1815. doi: 10.1002/bjs.10931 [DOI] [PubMed] [Google Scholar]
- 28.Nguyen YL, Wallace DJ, Yordanov Y, et al. The volume-outcome relationship in critical care: a systematic review and meta-analysis. Chest. 2015;148(1):79-92. doi: 10.1378/chest.14-2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mesman R, Westert GP, Berden BJMM, Faber MJ. Why do high-volume hospitals achieve better outcomes? a systematic review about intermediate factors in volume-outcome relationships. Health Policy. 2015;119(8):1055-1067. doi: 10.1016/j.healthpol.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 30.Cheung MC, Koniaris LG, Perez EA, Molina MA, Goodwin WJ, Salloum RM. Impact of hospital volume on surgical outcome for head and neck cancer. Ann Surg Oncol. 2009;16(4):1001-1009. doi: 10.1245/s10434-008-0191-9 [DOI] [PubMed] [Google Scholar]
- 31.Chen AY, Pavluck A, Halpern M, Ward E. Impact of treating facilities’ volume on survival for early-stage laryngeal cancer. Head Neck. 2009;31(9):1137-1143. doi: 10.1002/hed.21072 [DOI] [PubMed] [Google Scholar]
- 32.Gourin CG, Frick KD. National trends in laryngeal cancer surgery and the effect of surgeon and hospital volume on short-term outcomes and cost of care. Laryngoscope. 2012;122(1):88-94. doi: 10.1002/lary.22409 [DOI] [PubMed] [Google Scholar]
- 33.Gourin CG, Frick KD. National trends in oropharyngeal cancer surgery and the effect of surgeon and hospital volume on short-term outcomes and cost of care. Laryngoscope. 2012;122(3):543-551. doi: 10.1002/lary.22447 [DOI] [PubMed] [Google Scholar]
- 34.Gladwell M. Outliers: The Story of Success. Little, Brown, and Company. 2008. [Google Scholar]
- 35.Ericsson KA, Hoffman RR, Kozbelt A, Williams AM. Cambridge Handbook of Expertise and Expert Performance. Cambridge University Press; 2018. [Google Scholar]
- 36.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10)(suppl):S70-S81. doi: 10.1097/00001888-200410001-00022 [DOI] [PubMed] [Google Scholar]
- 37.Maruthappu M, Gilbert BJ, El-Harasis MA, et al. The influence of volume and experience on individual surgical performance: a systematic review. Ann Surg. 2015;261(4):642-647. doi: 10.1097/SLA.0000000000000852 [DOI] [PubMed] [Google Scholar]
- 38.Sawaf T, Renslo B, Virgen C, et al. Team consistency in reducing operative time in head and neck surgery with microvascular free flap reconstruction. Laryngoscope. Published online January 5, 2023. doi: 10.1002/lary.30542 [DOI] [PubMed] [Google Scholar]
- 39.Xu R, Carty MJ, Orgill DP, Lipsitz SR, Duclos A. The teaming curve: a longitudinal study of the influence of surgical team familiarity on operative time. Ann Surg. 2013;258(6):953-957. doi: 10.1097/SLA.0b013e3182864ffe [DOI] [PubMed] [Google Scholar]
- 40.Maruthappu M, Duclos A, Zhou CD, et al. The impact of team familiarity and surgical experience on operative efficiency: a retrospective analysis. J R Soc Med. 2016;109(4):147-153. doi: 10.1177/0141076816634317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elbardissi AW, Duclos A, Rawn JD, Orgill DP, Carty MJ. Cumulative team experience matters more than individual surgeon experience in cardiac surgery. J Thorac Cardiovasc Surg. 2013;145(2):328-333. doi: 10.1016/j.jtcvs.2012.09.022 [DOI] [PubMed] [Google Scholar]
- 42.Heidekrueger P, von Fritschen U, Moellhoff N, et al. Comparison of venous couplers versus hand-sewn technique in 4577 cases of DIEP-flap breast reconstructions—a multicenter study. Microsurgery. 2022;42(1):5-12. doi: 10.1002/micr.30686 [DOI] [PubMed] [Google Scholar]
- 43.Witjes MJH, Schepers RH, Kraeima J. Impact of 3D virtual planning on reconstruction of mandibular and maxillary surgical defects in head and neck oncology. Curr Opin Otolaryngol Head Neck Surg. 2018;26(2):108-114. doi: 10.1097/MOO.0000000000000437 [DOI] [PubMed] [Google Scholar]
- 44.Padilla PL, Mericli AF, Largo RD, Garvey PB. Computer-aided design and manufacturing versus conventional surgical planning for head and neck reconstruction: a systematic review and meta-analysis. Plast Reconstr Surg. 2021;148(1):183-192. doi: 10.1097/PRS.0000000000008085 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Tumor characteristics
eTable 2. Patients characteristics before and after implementation of standardized nursing team
eTable 3. Patients characteristics before and after implementation of treatment centralization
eTable 4. The effect of plating techniques on operative time (OR)
eTable 5. Secondary outcomes; length of stay (LOS), return to ED within 30 days, readmission rate
eTable 6. Effect of treatment centralization and standardized nursing team on length of stay LOS, return to ED within 30 days and readmission rate
eTable 7. 2 years and 5 years disease specific survival 2007-2020
eFigure. Secondary outcomes (30 days readmission rate, 30 days return to ER) and mean length of stay
Data sharing statement