Fig. 2.
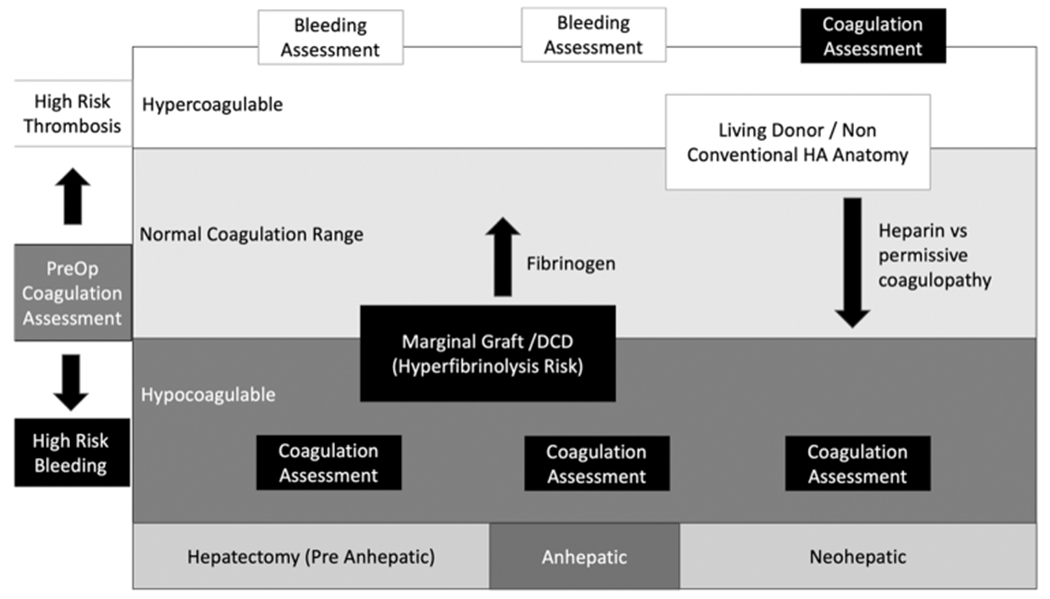
Intraoperative coagulation considerations. VET, viscoelastic testing; DCD, donation after circulatory death; HA, hepatic artery. Fig. 2 represents the dynamic changes in intraoperative coagulation assessment and treatment during the different phases of surgery. Preoperative coagulation assessment can place the patient on their trajectory toward bleeding during surgery or thrombotic complications. In those patients with preoperative hypercoagulable states, routine measurement of coagulation during the pre-anhepatic and anhepatic stage of surgery is not needed. The indication for hemostatic transfusions can be triggered by clinical assessment of bleeding. During the neohepatic phase, large changes in coagulation commonly occur and routine coagulation assessment to identify the patient’s new coagulation status can help guide a transfusion strategy. Hypocoagulable liver transplant patients on the other hand are at increased risk of major blood loss from the start of surgery. Routine coagulation assessment throughout the duration of surgery can be helpful to stay on top of coagulopathic bleeding. This is particularly relevant in LT recipients of marginal organs or DCD grafts at high risk of hyperfibrinolysis. Recipients of these grafts can benefit from preemptive fibrinogen transfusions before graft reperfusion, as there will be an anticipated dropped in fibrinogen. After reperfusion, anatomic considerations of the graft can guide resuscitation based on VET results. High-risk patients for HAT can be passively addressed with a tolerance for declining clotting indices appreciated on VET while the graft is reperfusion and transfusion triggers can be adjusted to tolerated a more hypocoagulable level in the absence of ongoing bleeding. Alternatively, this can be achieved actively with an intraoperative heparin infusion if there is a heightened concern.
