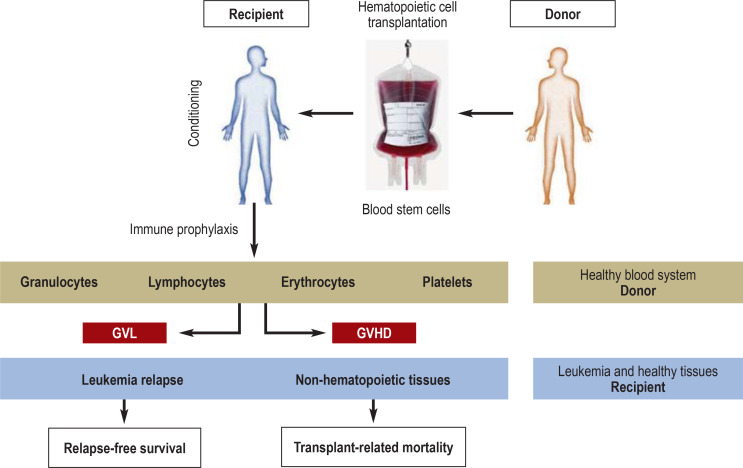
Figure 2.
The principle of allogeneic hematopoietic cell transplantation. The procedure aims at eradicating the underlying hematologic malignancy along with replacement of the patient‘s (blue) hematopoietic system by that of a healthy, genetically different donor (brown). The transplanted hematopoietic system therefore carries the genetic traits of the donor, while all other tissues (non-hematopoietic tissues and any residual leukemia cells) carry the genetic characteristics of the recipient. The recipient undergoes so-called pretransplant conditioning by chemotherapy with or without total-body irradiation, followed by pharmacological immune prophylaxis for days or weeks after transplantation. Donor immune cells, in particular T lymphocytes, can recognize patient-specific major and/or minor histocompatibility antigens, thereby mediating an anti-tumor effect (graft versus leukemia, GvL) and/or damage to healthy tissues, in particular skin, liver, or gut (graft versus host disease, GvHD). The balance between GvL and GvHD is crucial for relapse-free survival and transplant-related mortality.