Abstract
Objective
To report a patient who achieved complete recanalization using the parallel stent retriever (SR) technique for a refractory acute middle cerebral artery (MCA) embolism.
Case Presentation
An 86-year-old woman underwent an emergency thrombectomy for acute right MCA occlusion. Although thrombectomy has been attempted three times with the conventional technique using a single SR, no recanalization was achieved. Then, an innovative technique was used to deploy two SRs in parallel with the M1 segment of the MCA. Pulling them back simultaneously, the thrombus was retrieved, and complete recanalization was achieved.
Conclusion
The parallel SR technique is a feasible method and can be considered as one of the last treatment resorts for acute refractory embolisms at the major MCA trunk.
Keywords: mechanical thrombectomy, acute ischemic stroke, stent retriever
Introduction
Several randomized controlled trials previously demonstrated the efficacy of mechanical thrombectomy for acute ischemic stroke. Currently, this procedure is performed as an established treatment.1–5) Here, we report a case of a refractory middle cerebral artery (MCA) embolism that achieved complete recanalization using the parallel stent retriever (SR) technique by deploying two different SRs simultaneously.
Case Presentation
Case: An 86-year-old woman.
Medical history: Colorectal cancer (postoperatively).
Family history: Not contributory.
Present illness: She consulted a local clinic due to abnormal behaviors that persisted for a few days. Magnetic resonance imaging (MRI) revealed cerebral infarction, and thus, she was referred to the Department of Neurology of our hospital. However, she lost her consciousness with sudden hemiplegia while she was waiting for the consultation. She was then immediately brought to the emergency room.
Physical examination: The Japan Coma Scale score was III-100. Blood pressure and heart rate were 164/107 mmHg and 52 bpm (abnormal), respectively. Electrocardiography demonstrated atrial fibrillation. Conjugate eye deviation to the right and the left hemiplegia were observed. The National Institutes of Health Stroke Scale score was 28.
Hematological findings: No abnormalities were observed, except a slight increase in the D-dimer level (1.2 mg/mL).
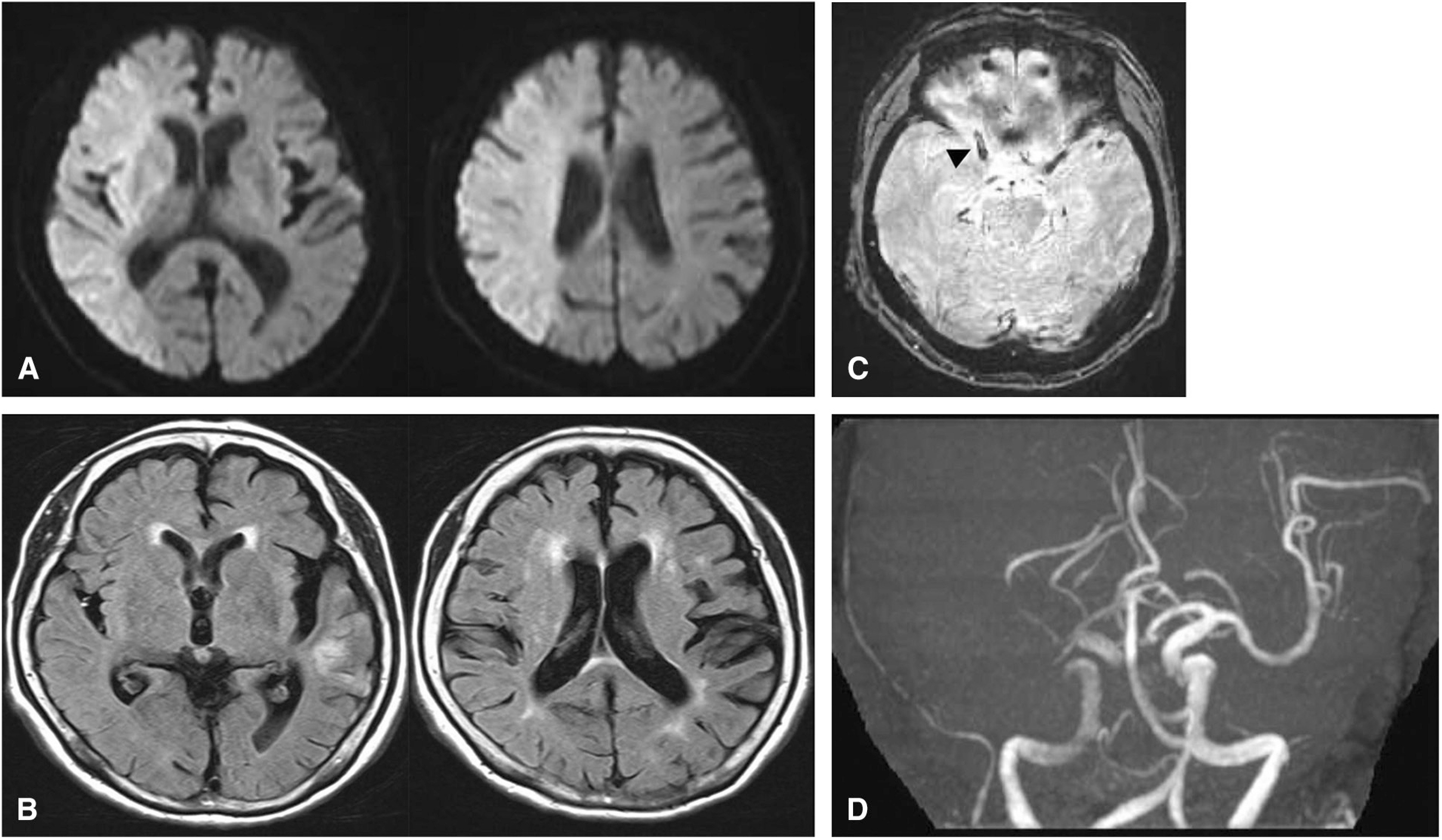
Imaging findings: On MRI-diffusion-weighted imaging (DWI) at the previous clinic, several high-signal-intensity areas were noted in the right cerebellum, left temporal lobe, and bilateral parietal lobes. DWI performed at our hospital after the deterioration revealed a slightly high signal intensity in the entire right MCA region, but fluid-attenuated inversion recovery (FLAIR) showed no signal change. Magnetic resonance angiography (MRA) demonstrated occlusion of the proximal right MCA, and a low-signal-intensity area that seems to be a thrombus was detected in the proximal M1 on T2*-weighted imaging. We diagnosed her with cardiogenic cerebral embolism (Fig. 1A–1D).
Fig. 1. MRI at onset shows acute ischemic change in the right MCA territory on DWI (A), but not on FLAIR (B). The T2*-weighted image shows a suspected thrombus in the MCA (arrowhead) (C). MRA demonstrates signal disruption in the right MCA (D). DWI: diffusion-weighted imaging; FLAIR: fluid-attenuated inversion recovery; MCA: middle cerebral artery; MRA: magnetic resonance angiography; MRI: magnetic resonance imaging.
Course: The DWI-Alberta Stroke Program Early CT Score was 0. Therefore, the patient was considered a severe case of grade C1 recommendation according to the 3rd edition of the Japanese guidelines for mechanical thrombectomy. However, we decided to perform mechanical thrombectomy due to the following reasons; an extensive DWI/FLAIR mismatch area, the interval from in-hospital onset was short, and the patient’s family strongly requested the treatment. Recombinant tissue plasminogen activator was not administered due to the preceding cerebral infarction that had developed a few days previously.
Endovascular treatment
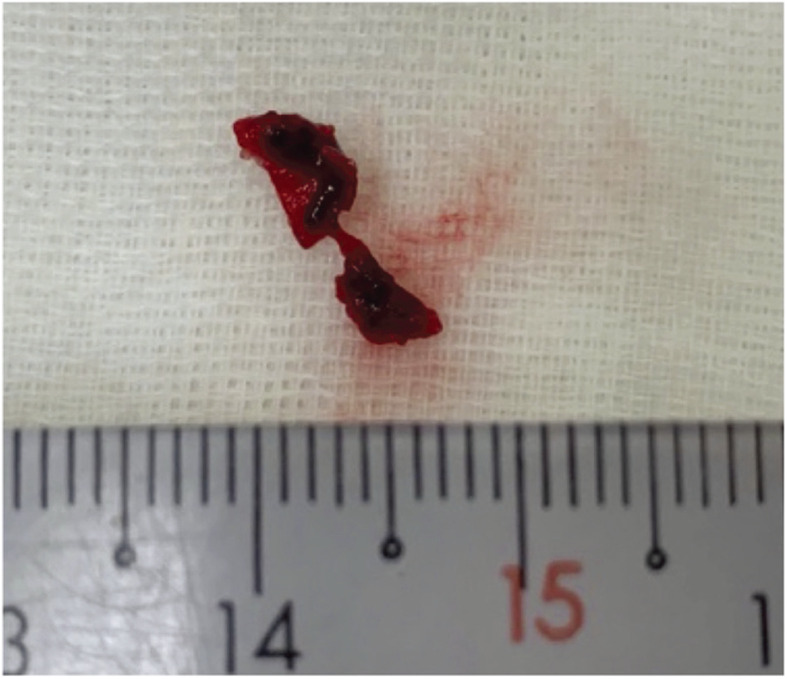
Under local anesthesia, a 9-F 25-cm sheath was carefully inserted into the left femoral artery. We attempted to advance a 9-F Optimo balloon guiding catheter (Tokai Medical Products, Aichi, Japan) into the right internal carotid artery coaxially with a 4-F catheter, but it was extremely difficult because the aortic arch was type 3 and the origin of the common carotid artery (CCA) was markedly tortuous (Fig. 2A). The inner catheter and guidewire were exchanged several times, but guiding was impossible. Therefore, the Optimo was grasped using a 10-mm Gooseneck Snare (Medtronic, Minneapolis, MN, USA) inserted through the right brachial artery, and successfully pulled up to the origin of the right CCA. However, it was impossible to advance the catheter more distally, and mechanical thrombectomy was performed from this position (Fig. 2B). Common carotid angiography confirmed occlusion of the proximal right MCA. First, we decided to perform thrombectomy with a SR alone because the position of Optimo was too far and an aspiration catheter could not reach the lesion. A Marksman (Medtronic) was crossed over the lesion and a Solitaire Platinum 6 × 40 mm (Medtronic) was deployed. However, effective flow restoration was not confirmed (Fig. 3A), possibly because of the hard thrombus. The SR was retrieved while manually aspirating the blood through the Optimo; however, recanalization was not achieved. The same procedure was performed three times, exceeding the upper limit of the proper frequency of Solitaire use; however, recanalization was still not achieved. Although thrombectomy seemed to be difficult due to the hard thrombus, we attempted to deploy two different SRs in parallel as the last strategy. A Marksman and Excelsior XT-27 (Stryker, Kalamazoo, MI, USA) were advanced in parallel into the MCA and crossed over the lesion. A 6 × 40 mm Solitaire and 6 × 25 mm Trevo XP Provue retriever (Stryker) were simultaneously inserted into the M1 segment through the Marksman and Excelsior XT-27, respectively. Angiography immediately after deployment confirmed favorable flow restoration (Fig. 3B–3D). The two SRs were simultaneously pulled back, and the thrombus was successfully retrieved with sandwiched between them (Fig. 4). Complete recanalization was confirmed (thrombolysis in cerebral infarction (TICI) grade 3) (Fig. 3E).
Fig. 2. (A) Angiography shows the strong tortuosity in the CCA. (B) A goose neck snare via the right brachial artery is holding a 9Fr balloon guiding catheter. CCA: common carotid artery.
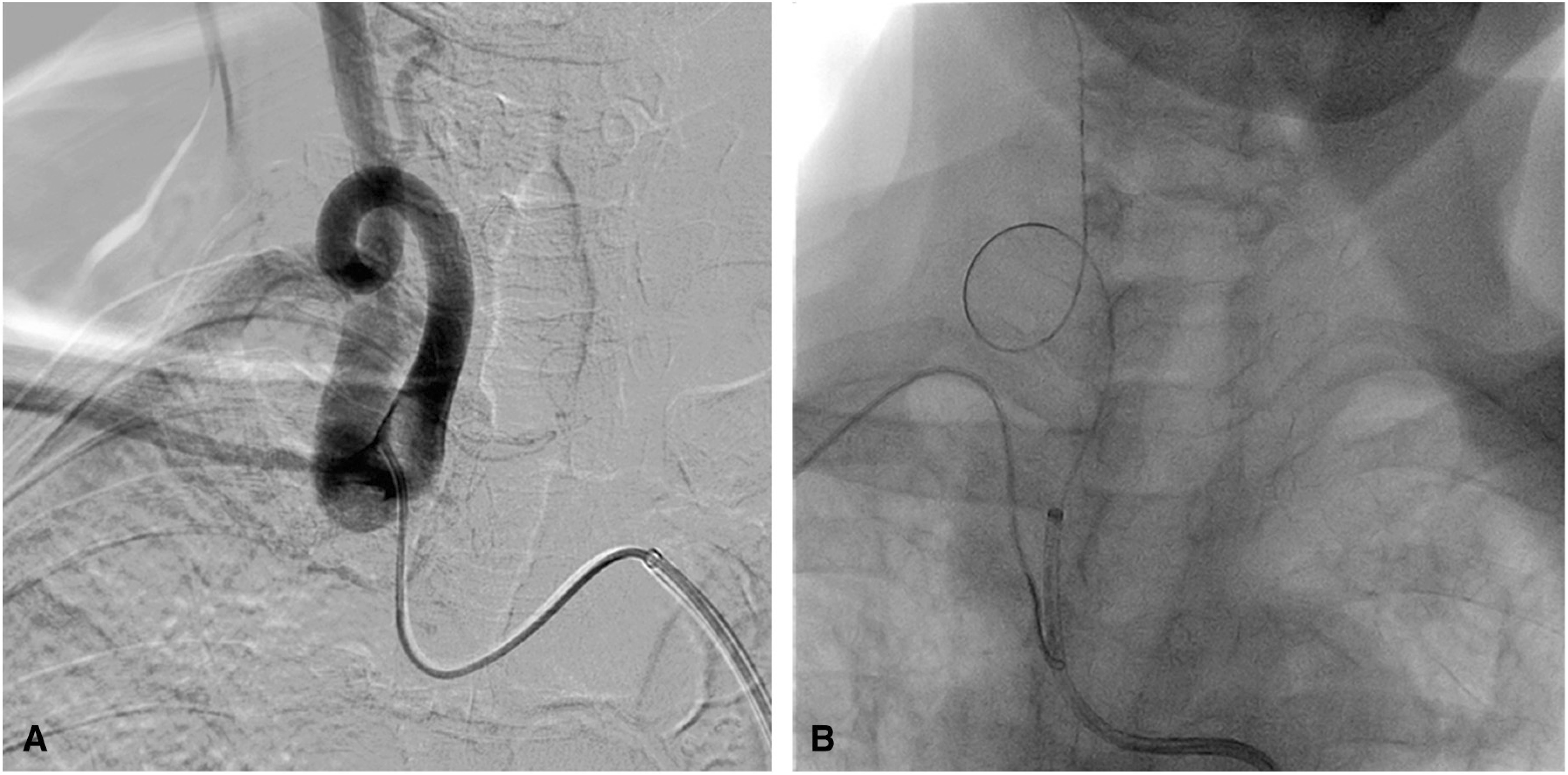
Fig. 3. Angiography during thrombectomy. A single SR is deployed in the right M1; however, no flow restoration was observed (A). Two microcatheters are navigated into the right M1 (B) and two SRs are deployed simultaneously (C). Immediate flow restoration is confirmed (D) and complete recanalization was achieved (E). SR: stent retrievers.
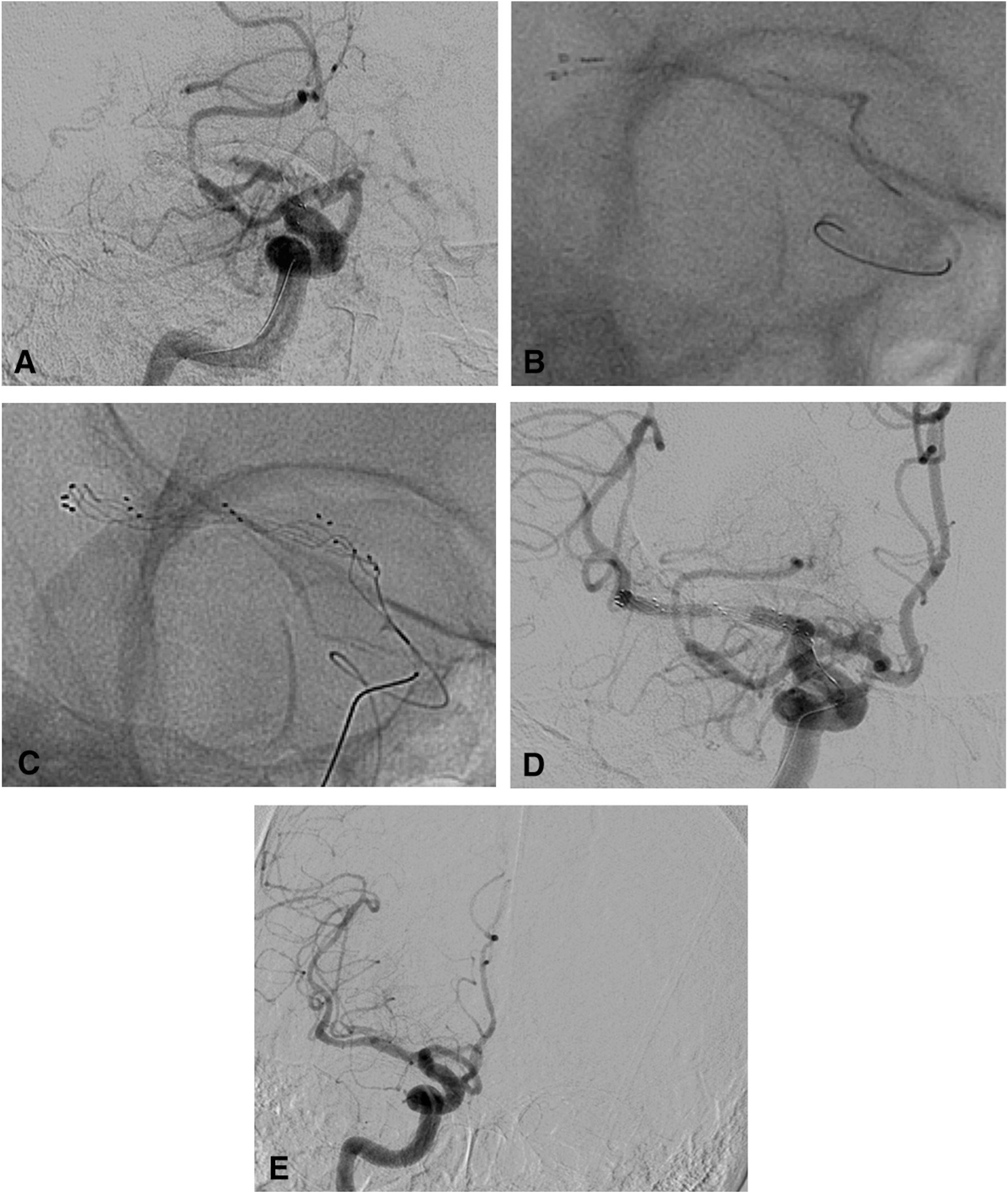
Fig. 4. Removal of partially white thrombus.
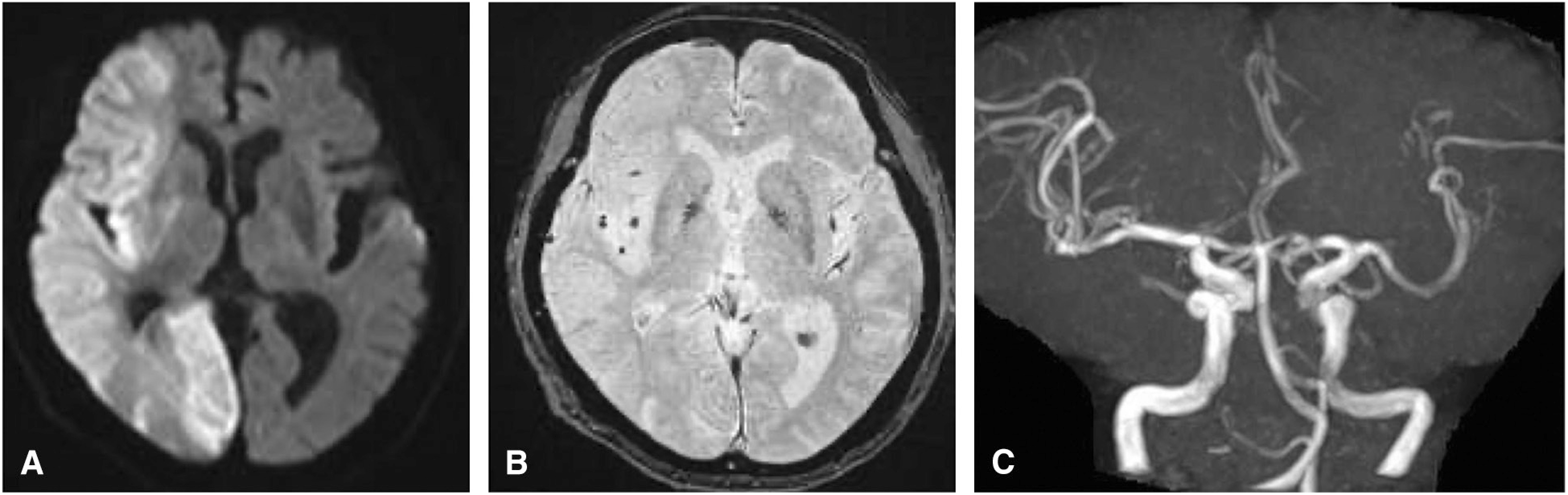
Postoperative course: The patient’s consciousness level slightly improved; however, other neurological symptoms remained unimproved. DWI on the following day demonstrated a high signal intensity in the same area as before the thrombectomy. However, no intracranial hemorrhage occurred related to the procedure. On MRA, the right MCA was well visualized, and neither vasospasm nor dissection was observed in the M1 segment (Fig. 5A–5C). On the 9th postoperative day, the patient was discharged with a modified Rankin Scale (mRS) score of 5.
Fig. 5. MRI on postoperative day 1. (A) DWI shows extensive high-signal-intensity areas in the right hemisphere. (B) There is no hemorrhagic lesion on the T2*-weighted image. (C) MRA shows good recanalization and no vasospasm in the right MCA. DWI: diffusion-weighted imaging; MCA: middle cerebral artery; MRA: magnetic resonance angiography.
Discussion
Several randomized controlled trials published after 2014 demonstrated the efficacy of thrombectomy for large vessel occlusion. This procedure has become the standard treatment.1–5) In addition, based on the DAWN/DEFUSE 3 trial results in 2018, this procedure has been increasingly indicated.6,7) Due to development of devices and increasing experience, the effective recanalization (TICI grade 2b-3) rate after mechanical thrombectomy has reached 58.7%–88%,1–4) contributing to an improved outcome. However, recanalization fails in about 20% of patients. The main causes include the nature of the thrombus and anatomical access limitations.8,9) Machi et al.8) reported that SR did not effectively expand the white thrombus as compared to the red thrombus, analyzing the results of in vitro thrombectomies. In particular, >6 mm white thrombus affected the SR expansion, reducing the thrombus retrieval rate. Furthermore, they emphasized that radial forces of most SRs decreased during the retrieval, leading to a reduced recanalization rate. Concerning the access, especially in elderly patients, reaching the lesion may be impossible due to anatomical limitations, such as vascular tortuosity, and the treatment may have to be abandoned. Furthermore, the inability to perform conventional methods may reduce the effectiveness of devices. Ribo et al. reported that access was difficult in 67% of patients aged >75 years and that the recanalization rate was significantly lower in these patients, leading to a poor outcome.9)
This patient aged 86 years, and the access route was severely tortuous; thus, a guiding catheter cannot be advanced beyond the CCA origin. Therefore, we considered that a thrombus aspiration catheter may not reach the lesion and attempted thrombectomy using an SR alone. However, recanalization was not achieved. Since the thrombus was too hard to be grasped with a single SR, we considered to give up the treatment but tried to retrieve using two different SRs as the last resort. As a result, the thrombus was successfully retrieved and captured between the two SRs, and finally complete recanalization was obtained.
Several thrombectomy techniques using multiple SRs have been performed in patients with difficult recanalization.10–15) Klisch et al.10) reported 10 patients who underwent double Solitaire mechanical thrombectomy for a thrombus at the MC bifurcation. Of 10 patients, Y-configured stents (Y-stents) were used in 9 and parallel stents were used in 1. In 8 of 10 patients, TICI 2b-3 recanalization was achieved. In 50% of patients, the outcome was favorable (mRS score ≤2). Aydin et al. also adopted the Y-stent technique for 10 patients in whom it was difficult to achieve recanalization using conventional techniques and reported favorable recanalization (TICI 2b-3) in 80% of patients. In addition, the Y-stent technique achieved favorable recanalization in all patients during the first pass.15) Several case reports also confirmed the efficacy of the Y-stent technique.1–13) In the present case, the thrombus was present in the M1 segment, and the retrieval force was improved by simultaneously deploying two different SRs in parallel in the M1 segment, leading to recanalization. When two microcatheters take different thrombus routes, grasping the thrombus may be possible with two SRs. Indeed, in the present case, the thrombus was caught between the two SRs. This effect cannot be obtained using conventional techniques. Thus, this technique should be considered as the “last strategy” for patients with difficulty achieving recanalization using the conventional techniques alone.
As regards the disadvantages of this technique, dissection, vasospasm, or hemorrhagic complications may occur. When two SRs are simultaneously deployed in the same artery, their radial forces against the arterial wall may increase, which may also increase the ability to capture a thrombus, but may also increase stress on the arterial wall. According to Klisch et al.,10) symptomatic hemorrhage was noted in 1 of 10 patients and mild asymptomatic vasospasm was noted in 7. Aydin et al.15) reported asymptomatic hemorrhage in 2 of 10 patients and mild asymptomatic vasospasm in 5. Conversely, in a single SR technique, the incidence of procedure-related hemorrhagic complications ranged from 4.5% to 7% and that of vasospasm ranged from 6.4% to 22.5%.16–18) Although the number of patients was small, vascular wall stress may increase in two SR technique. For this reason, this technique should be considered as the “last strategy” only for patients encountering recanalization difficulty with conventional techniques.
Conclusion
We experienced a case of the refractory MCA thrombus in which complete recanalization was achieved by deploying two SRs in parallel and retrieving them simultaneously. This technique may be an effective alternative for patients in whom recanalization is difficult.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1).Berkhemer OA, Fransen PS, Beumer D, et al. : A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 2).Campbell BC, Mitchell PJ, Kleinig TJ, et al. : Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 3).Goyal M, Demchuk AM, Menon BK, et al. : Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 4).Saver JL, Goyal M, Bonafe A, et al. : Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 5).Jovin TG, Chamorro A, Cobo E, et al. : Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 6).Nogueira RG, Jadhav AP, Haussen DC, et al. : Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018; 378: 11–21. [DOI] [PubMed] [Google Scholar]
- 7).Albers GW, Marks MP, Kemp S, et al. : Thrombectomy for Stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018; 378: 708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Machi P, Jourdan F, Ambard D, et al. : Experimental evaluation of stent retrievers’ mechanical properties and effectiveness. J Neurointerv Surg 2017; 9: 257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Ribo M, Flores A, Rubiera M, et al. : Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J Neurointerv Surg 2013; 5: i70–i73. [DOI] [PubMed] [Google Scholar]
- 10).Klisch J, Sychra V, Strasilla C, et al. : Double solitaire mechanical thrombectomy in acute stroke: effective rescue strategy for refractory artery occlusions? AJNR Am J Neuroradiol 2015; 36: 552–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Asadi H, Brennan P, Martin A, et al. : Double stent-retriever technique in endovascular treatment of middle cerebral artery saddle embolus. J Stroke Cereberovasc Dis 2016; 25: e9–11. [DOI] [PubMed] [Google Scholar]
- 12).Okada H, Matsuda Y, Chung J, et al. : Utility of a Y-configured stentriever technique as a rescue method of thrombectomy for an intractable rooted thrombus located on the middle cerebral artery bifurcation: technical note. Neurosurg Focus 2017; 42: E17. [DOI] [PubMed] [Google Scholar]
- 13).Peker A, Akgoz A, Arsava EM, et al. : Dual mechanical thrombectomy for recanalization of a resistant acute posterior circulation stroke. J Cerebrovasc Endovasc Neurosurg 2017; 19: 96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Crosa R, Spiotta AM, Negrotto M, et al. : “Y-stent retriever”: a new rescue technique for refractory large-vessel occlusions? J Neurosurg 2018; 128: 1349–1353. [DOI] [PubMed] [Google Scholar]
- 15).Aydin K, Barburoglu M, Cakmak OO, et al. : Crossing Y-Solitaire thrombectomy as a rescue treatment for refractory acute occlusion of the middle cerebral artery. J Neurointerv Surg 2019; 11: 246–250. [DOI] [PubMed] [Google Scholar]
- 16).Akins PT, Amar AP, Pakbaz RS, et al. : Complications of endovascular treatment for acute stroke in the SWIFT trial with solitaire and Merci devices. AJNR Am J Neuroradiol 2014; 35: 524–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Lapergue B, Blanc R, Gory B, et al. : Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: The ASTER randomized clinical trial. JAMA 2017; 318: 443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Turk AS, Siddiqui A, Fifi JT, et al. : Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019; 393: 998–1008. [DOI] [PubMed] [Google Scholar]