Abstract
The pathologies and lesions affecting the sesamoid bones of the hallux are uncommon and can be easily overlooked. Among them, sesamoiditis is a relatively rare condition known to cause severe great toe pain; lack of awareness of this particular entity leads to misdiagnosis, delayed treatment, and contributes to significant morbidity. Herein, we present a chronic sesamoiditis case occurring on a medial bipartite sesamoid bone, presenting as chronic great toe pain. The main purpose of this work is to discuss the role of magnetic resonance imaging and X-rays in the diagnosis process. To the best of our knowledge, no cases of great toe sesamoiditis occurring on a bipartite bone in no-athletic patients have yet been reported.
Keywords: Bone, Sesamoid, Foot, Foot injuries, Toe
Introduction
Sesamoid bones are small, pea-shaped bones that are embedded in tendons and provide leverage and support for the foot. They can be found in a variety of locations throughout the body, but are most commonly found in the hands and feet [1]. The sesamoid bones in the foot are two small bones located beneath the first metatarsal head, called the medial (tibial) and lateral (fibular) sesamoids. Bipartite sesamoids are sesamoid bones that are divided into two parts, usually as a result of incomplete fusion during development. The medial sesamoid bone is located on the inside aspect of the foot, and is commonly bipartite [2]. Sesamoiditis is an inflammatory condition that affects the sesamoid bones, and it is often associated with repetitive stress or trauma to the affected area [3]. The aim of this work is to discuss the clinical and radiological presentation of chronic sesamoiditis occurring on a medial bipartite sesamoid bone.
Case report
A 30 years-old female patient presented with right chronic great toe pain that had been evolving for several years. Pain became more severe three weeks ago without any identifiable traumatic incident. It exacerbated when walking and wearing thin shoes, making any physical activity impossible. Patient's history did not reveal any past of medical or surgical history. She reported regular physical activity, especially running. On examination, a tender spot was identified at the base of the hallux, beneath the first metatarsophalangeal (MTP) joint. Upon inspection, there was no evidence of swelling or discoloration. The patient did not exhibit flat feet or any other deformities. The left foot examination was normal. Bilateral standard radiographs include weight-bearing anteroposterior, and oblique views, they ruled out any fracture line and revealed bipartite medial sesamoid bone. Lateral sesamoid bone was normal (Fig. 1). Magnetic Resonance imaging (MRI) in axial and sagittal views showed fragmented right medial sesamoid bone with geodes and oedema appearing as low signal T1 (Fig. 2A and B) and high signal STIR (Fig. 2C) associated with irregular and discontinuous bone contours. It also revealed an intra articular bone fragment as a direct consequence of cartilage destruction (Fig. 3). Besides, the fibular sesamoid was normal in appearance (Fig. 4A), as was the flexor hallucis longus tendon (Fig. 4B). In front of this clinical and radiological features, a chronic sesamoiditis with inflammatory changes on a medial bipartite sesamoid bone was suggested. The patient was managed conservatively with a short period of non-steroidal-anti-inflammatory-drugs (NSAIDs) prednisolone three tablets (20 mg/kg) in the morning for five days and a 3-months rest period. Low-impact activities, such as swimming, were recommended. After one-month, clinical control didn't reveal any exacerbation or reccurence of the pain, no articular infiltration or surgery were required.
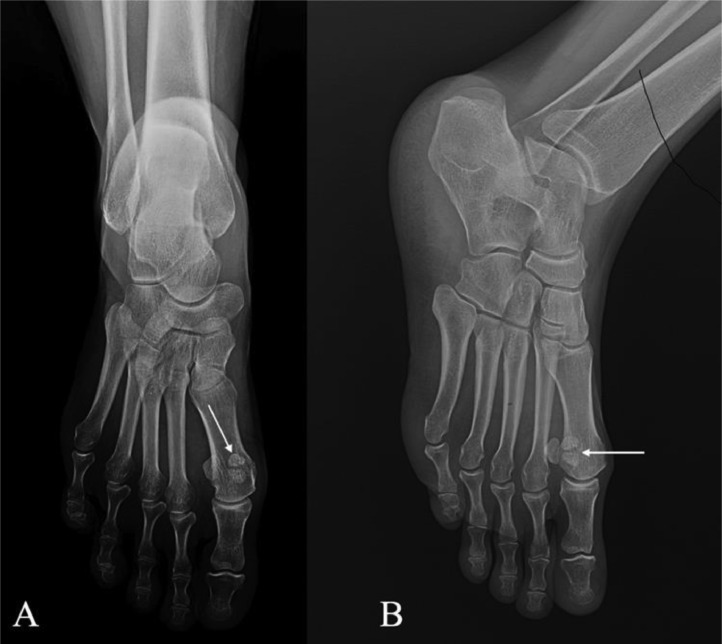
Fig. 1.
Front (A) and oblique (B) radiograph views showed a bipartite medial sesamoid bone at the base of the right great toe (white arrow).
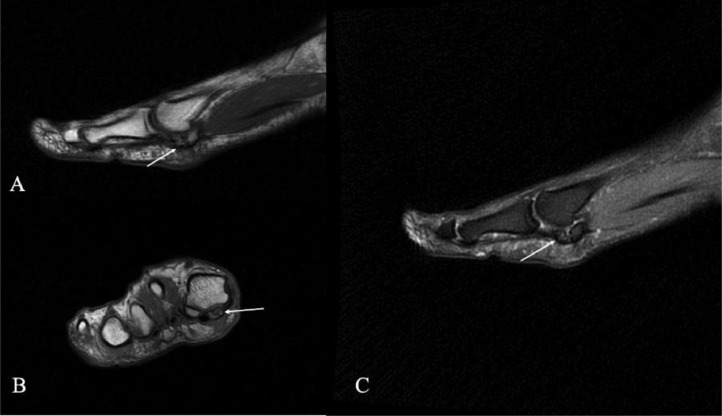
Fig. 2.
Sagittal and axial T1-W MRI section (A and B) and sagittal T2-W section (C) revealing fragmented right medial sesamoid bone with geodes and oedema appearing in low signal T1 and high signal STIR, associated with irregular and discontinuous bone contours.
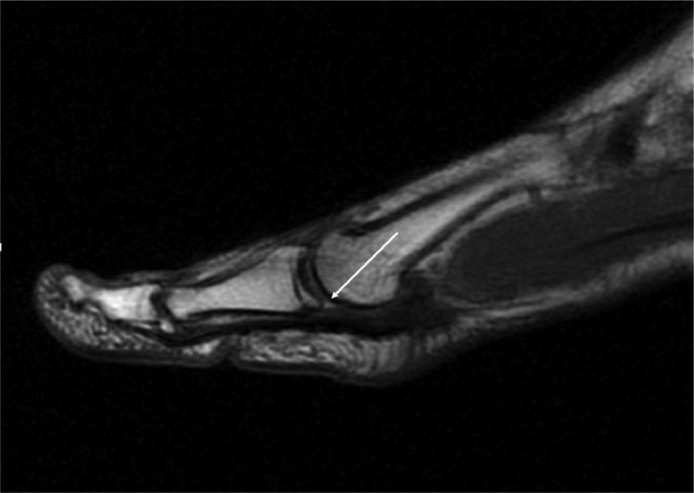
Fig. 3.
Sagittal T1-W MRI section revealing an intra-articular fragment of cartilage.
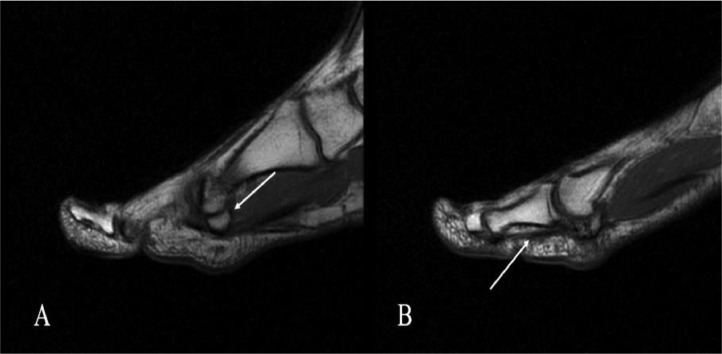
Fig. 4.
Sagittal T1-W MRI sections showing normal appearance of the fibular sesamoid (Figure A) and the flexor hallucis longus tendon (Figure B).
Discussion
Foot pain is a frequently reported issue among patients, with an estimated occurrence rate in adults ranging from 13% to 36% [4]. Nevertheless, sesamoids are usually asymptomatic. Their disorders account for less than 9% of foot injuries [5]. It can be affected by either inflammation, fracture, osteonecrosis, infection and degeneration [6]. Bipartite sesamoids are a common anatomical variant. Their incidence is between 7% and 30% [2]. To the best of our knowledge, no case of hallucal sesamoiditis occurring on a bipartite bone in no-athletic patient has yet been reported. It consists on an inflammatory condition that affects a fragmented sesamoid bone, and is often associated with repetitive stress or trauma to the affected area [3]. Several elements have been reported as predisposing factors [7,8]. Chang et al. found that female sex, younger age, higher BMI (body mass index), foot deformities, and athletic activities were significant risk factors for hallux sesamoiditis [9]. This affection is more common in athletes who engage in activities that involve a lot of running and jumping, but can also occur in non-athletes. Due to the increased weight distribution on the medial sesamoid, some anatomical differences and its greater mobility, it is more prone to injury and disease [10]. Sesamoiditis can have both acute and chronic presentations [4]. Chronic sesamoiditis is often attributed to repetitive training or prolonged use of high-heeled shoes. It can be described as an overuse injury [10]. Patients typically report a gradual onset of pain that worsens with weight bearing, walking, running, and wearing thin shoes [4,5].
Diagnosis of sesamoiditis on a medial bipartite sesamoid bone may involve a meticulous physical examination, X-rays, and MRI [4,10].
The main purpose of X-rays is to rule out a fracture. The identification of fractures can be difficult due to the common occurrence of a bipartite sesamoid. Therefore, in the diagnosis of an acute fracture, it is essential to observe any irregular discontinuity of the sesamoid bone with serrated margins, along with the occurrence of callus formation visible on repeated radiographic imaging [10].
MRI can be useful in the diagnosis process by showing inflammation in the bones, soft tissues, and in the flexor hallucis longus tendon. MRI findings for sesamoiditis may show bone marrow oedema, which appears as low signal T1 and high signal STIR areas. Additionally, there may be soft tissue oedema surrounding the sesamoid bones, appearing as an area of increased fluid. Sesamoid sclerosis or fragmentation may be present, indicating degenerative changes of the sesamoid bones. In some instances, flexor hallucis longus tenosynovitis may also be visualized. Fracture line seen on sagittal view as low intensity on T1. Ischemia was variable more commonly involving the fibular sesamoid as low signal on T1 and high T2 and STIR images in variable intensities. In this particular case of sesamoiditis, the bone marrow oedema was localized in the medial sesamoid bone with intra-articular cartilage fragment. Normal aspect of the fibular sesamoid bone. No tenosynovitis was found.
Sesamoiditis treatment typically involves rest, and immobilization by orthotic management to off-loading the hallux metatarsal phalangeal complex. The NSAIDs medication can reduce pain and inflammation on the affected area [11,12]. Intra-articular corticoid infiltration can also facilitate the healing process, but repeated injections are not recommended. Rarely, surgical intervention may be considered if severe instability or lesion of ligaments of the plantar plate complex was suspected [12].
Conclusion
Sesamoiditis of the great toe is an infrequent occurrence, especially on a bipartite bone. The diagnosis is suggested by the location and nature of the pain, with imaging playing an important role in confirmation. This particular entity should be kept in mind in the face of chronic big toe pain, especially in young athletes. MRI, by showing inflammation of the sesamoid bones, of the surrounding soft tissues, flexor hallucis longus tenosynovitis, and some signs of degeneration, can help to confirm the diagnosis and to quickly implement an appropriate treatment. Conservative treatment should be attempted initially, with surgery rarely indicated. Early diagnosis and appropriate treatment can help relieve symptoms and prevent further damage to the affected area.
Patient consent
The corresponding author confirms that patient consent has been obtained.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Yeung AY, Arbor TC, Garg R. Anatomy, Sesamoid Bones. [Updated 2023 Apr 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK578171/ [PubMed]
- 2.Sims AL, Kurup HV. Painful sesamoid of the great toe. World J Orthoped. 2014;5(2):146–150. doi: 10.5312/wjo.v5.i2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma P, Singh H, Agarwal KK, Sudhir KS, Khangembam BC, Bal C., et al. Utility of (99m)Tc-MDP SPECT-CT for the diagnosis of sesamoiditis as cause of metatarsalgia. Indian J Nucl Med: IJNM. 2012;27(1):45–47. doi: 10.4103/0972-3919.108865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrews NA, Ray J, Dib A, Harrelson WM, Khurana A, Singh MS, et al. Diagnosis and conservative management of great toe pathologies: a review. Postgrad Med. 2021;133(4):409–420. doi: 10.1080/00325481.2021.1895587. [DOI] [PubMed] [Google Scholar]
- 5.Boike A, Schnirring-Judge M, McMillin S. Sesamoid disorders of the first metatarsophalangeal joint. Clin Podiatr Med Surg. 2011;28(2) doi: 10.1016/j.cpm.2011.03.006. 269–vii. [DOI] [PubMed] [Google Scholar]
- 6.Atiya S, Quah C, Pillai A. Sesamoiditis of the metatarsophalangeal joint. OA Orthopaed. 2013;1:19. [Google Scholar]
- 7.Lee KT, Park YU, Jegal H, Yoon TR. Radiographic factors associated with sesamoid arthritis in patients with hallux valgus. J Foot Ankle Surg. 2019;58(1):5–9. doi: 10.1053/j.jfas.2018.08.009. Epub 2018 Nov 8. [DOI] [Google Scholar]
- 8.Van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Sesamoiditis: etiology, imaging, and treatment. J Am Podiatr Med Assoc. 2014;104(6):583–593. doi: 10.7547/13-033.1. [DOI] [Google Scholar]
- 9.Chang YC, Tsai WC, Wang CL, Hsu HH, Lin CJ, Wu CH. Risk factors for hallux sesamoiditis: a case-control study. Foot Ankle Int. 2015;36(10):1174–1179. doi: 10.1177/1071100715585465. [DOI] [Google Scholar]
- 10.Marques JP, Pinheiro J-P, Cordeiro A, Rodineau J. Fracture de fatigue du sésamoïde médial de l’hallux chez un footballeur : à propos d’un cas. J Traumatol Sport. 2017;34(3):185–187. doi: 10.1016/j.jts.2017.07.003. ISSN 0762-915X. [DOI] [Google Scholar]
- 11.Cohen BE. Hallux sesamoid disorders. Foot Ankle Clin. 2009;14(1):91–104. doi: 10.1016/j.fcl.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 12.York PJ, Wydra FB, Hunt KJ. Injuries to the great toe. Curr Rev Musculoskeletal Med. 2017;10(1):104–112. doi: 10.1007/s12178-017-9390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]