Abstract
It is now possible to collect large sums of health-related data which has the potential to transform healthcare. Proteomics, with its central position as downstream of genetics and epigenetic inputs and upstream of biochemical outputs and integrators of environmental signals, is well-positioned to contribute to health discoveries and management. We present our perspective on the role of proteomics and other Omics in precision health and medicine.
Keywords: proteomics, precision medicine, individualized medicine, big data, remote monitoring, mass spectrometry
Graphical Abstract
1. PRECISION HEALTH AND PRECISION MEDICINE
The concept of precision medicine is based on ensuring that the right treatment or drug is provided to the right person at the right time. This implies that (i) a precise therapy exists which can be provided to a specific individual and (ii) precise biomarkers exist that are able to determine the individual’s disease status, differentiate which therapy should be provided, and indicate when that intervention should occur. This is not yet the reality for the majority of health care needs. However, Omics-based technologies can help to ensure that the drugs or treatments target disease-causing pathways rather than more general nonspecific treatments and can help monitor outcomes. Omics-based technology can also define personalized biomarkers, which require understanding the balance between health, disease, and their modulators.
Precision medicine and precision health are often used interchangeably, but they are not the same. Precision medicine infers clinical intervention and is focused on the identification of disease and its treatment. Precision health, in our view, is focused on maintaining health and emphasizes disease prevention and early diagnosis, prior to clinical symptoms. An individual’s overall phenotype is itself a complex system centered around physiology and biochemistry of different cell types, organs and body fluids, as well as the impact of the microbiome and mental health (Figure 1). An individual’s phenotype is highly personal1 and influenced by many factors such as environment, life style, social demographic, genetics, and epigenetics. A person’s phenotype is not stable, but instead, is dynamic and can change over time (seconds, days, and decades) and in response to exposures, lifestyle and aging. Today, we are able to capture a person’s phenotype using many millions of qualitative and quantitative measures including the Omics measurements, such as genomics, epigenomics, transcriptomics, proteomics, metabolomics, and microbial measurements (Figure 1).2 The proteome occupies a central location: it (a) lies downstream of the genetic information flow, (b) responds to environmental signals and treatments, and (3) mediates the biochemical activities of a cell and organ. Proteomics has a vast chemical repertoire and broadest chemical diversity due to the extensive proteoforms arising from isoforms (arising from mRNA splicing and differential promoters and termination signals), allelic variants, and coand post-translational modifications (PTMs).3,4 As such, it is ideally positioned both as a signature of physiological phenotype and as a point of intervention for drug and health treatments. Thus, proteomic assays should be able to expand the physician’s toolbox by using an individual’s molecular proteotype as part of the clinical decision-making process. One challenge with proteomics is deciding which tissues and fluids to analyze. For practical reasons, plasma and urine are typically analyzed in healthy individuals, although biopsies are commonly analyzed in disease samples.
Figure 1.

Multifactorial influences dictate the individual’s phenotype and proteome. An individual’s phenotype can be assessed by biosensors, OMIC data and patent reported outcomes questionaries’ (PROs). It is the proteome, however, which has the broadest diversity of forms (proteoforms). That diversity is due to isoforms, single nucleotide variants (SNVs), and co- and post-translational modifications (PTMs).
2. PROTEOTYPING, DIAGNOSTICS, AND PRECISION HEALTH
The Institute of Medicine has defined that “biomarkers are tools used by doctors, scientists, and other health professionals to obtain information about a patient’s or research subject’s health status or response to interventions.5 In the same year, a broader definition came from the International Program on Chemical Safety (World Health Organization, United Nations and the International Labor Organization) as “any substance, structure, or process that can be measured in the body or its products and influence or predict the incidence of outcome or disease”.6 Biomarkers can be diagnostic, assist in risk assessment and screening, and used to predict clinical outcome (surrogate end points) or therapeutic response (effect modifiers) during and after treatment (change in disease status).7 Of emerging interests are the identification and use of biomarkers that are able to determine the health status of an individual (wellness) and those which allow us to differentiate an individual from the rest of the population.
Proteomics is involved in the identification of new candidate biomarkers via untargeted profiling of proteins and proteoforms in a wide range of diseases. Chronic and complex diseases such as autism and type 2 diabetes are highly heterogeneous and likely to classify into multiple different diseases. Indeed, it has recently been shown type 2 diabetes may have as many as five different subtypes.8 This number is likely to increase with additional profiling. Proteomics and mass spectrometry (MS) may also provide alternative or complementary diagnostic platforms to existing ELISA assays. This is already evident from the test for thyroglobulin, a current clinical chemistry analyte that is used to detect follicular cell-derived thyroid carcinoma, and less frequently to differentiate early phase silent thyroiditis from Graves’ disease; in this case, the ELISA assay has to contend with interference from antithyroglobulin autoantibodies or heterophile antibodies, which is not an issue with the immuno-MS assay.9 In addition, MS is effective for analysis of protein panels such as the ratio of apolipoprotein B to apolipoprotein A1, which is diagnostically equal to or better than the classical lipid panel that is used extensively in cardiovascular disease management.10–12
The concept of personalized medicine is to carry out robust quantitative assays on large numbers (hundreds) of blood, plasma or urine proteins on 100s or 1000s of individuals. MS and quantitative analysis using high-throughput capture reagents are ideal platforms for making tens to hundreds of targeted measurements with relatively low percent coefficient variance (%CV, indicates inter- and intra-assay reproducibility). At the same time, it is important that the protein assay is accurate, precise (reproducible), sensitive, and specific for the analyte. Specificity arises from having multiple independent measurement for each protein. MS and sandwich ELISAs, most commonly used in clinical chemistry tests, are rapid, thereby enabling multiple measurements.
Proteomics pipelines for analysis of blood and plasma have improved significantly over the past decade. These improvements, which include automated MS-sample preparation to produce tryptic peptides (unless intact proteins are being used),13–15 improved sensitivity of mass spectrometers, and accurate software and algorithms for quantifying and interpreting MS peptide-spectra, have resulted in a leap in the breath of candidate biomarkers with many more likely to be uncovered. However, it is a long journey from a candidate biomarker to determining its clinical utility. There are many technical challenges in the validation/verification process and the clinical trials required to set reference ranges and assay performance; these include automation and scaling of proteomic pipeline and decisions to use MS and/or ELISA methodology but also cohort selection as it will ultimately determine if, when and how the assay can be used clinical.
Thus, it is important to test the candidate biomarker(s) on the numerous and appropriate clinical cohorts as this will establish clinical utility. It is essential that when a biomarker(s) is deployed clinically, it can not only distinguish between healthy and disease, but distinguish among diseases that cause the same “phenotype”. For example, when a patient arrives at the emergency room with chest pain, it could be due to myocardial infarction, pulmonary embolism, aortic aneurysm or a host of other causes (e.g., esophageal spasm, GI symptoms, etc.). Distinguishing these are essential as it alters treatment and, in some cases, such as the first three, the treatment for each is counter indicated for the others.
Many candidate biomarkers uncovered in academia are pursued in the private sector. High standards are required for clinical validation and implementation, and these often require substantial resources. In order to attract commercial interest, it is usually important to perform some level of validation of a candidate biomarker in an additional independent cohort. However, having an academic center which has the capacity to run a large number of samples to establish clinical utility and convert to a clinical assay for implementation in a CLIA certified clinical laboratory could enable this need without relying exclusively on the commercial sector. Converting a candidate biomarker into a clinical marker requires establishment of a robust assay with high reproducibility (i.e., low % CV), a high sensitivity, and a low false positive rate. The latter is particularly important because most individuals do not carry a specific disease marker and thus even a modest fraction of false positives will yield many false positives over true positives. Commercial entities have robust protocols and practices in place to develop candidate markers into clinical test.
In order to make more accurate diagnoses in the future, most tests will combine multiple sources of information and, therefore, be multianalyte. As a simple form of this, low-density lipoprotein (LDL) levels are associated with heart failure, but LDL plus high-density lipoprotein (HDL) levels are more informative. This clinical parameter can be substituted by quantifying the ratio of ApoB to ApoA1 proteins (which represent the atherogenic particles and antiatherogenic particles, respectively), which can be measured in a MS multiplex (i.e., 10–12, review 16). Adding additional markers such as C-reactive protein (CRP), an indication of inflammation may be more informative in a subgroup of individuals with acute coronary syndromes (e.g., compare17 versus 18). It is expected in the future that multiple analytes will be used for prediction of most major complex diseases and will be important for disease classification, prognosis and treatment. Indeed, using CPTAC data as an example, multiple proteomics markers have been shown to be valuable for ovarian cancer prognosis.19 Multiple markers can be selected and combined in a fashion that increases both sensitivity and specificity but, excess markers can increase false positives impacting clinical usefulness.
It is expected that by harnessing the chemical diversity of proteins (by measuring specific proteoforms), we will increase our ability to differentiate between individuals and different disease states. For examples, differences in apolipidprotein L1 geneotypes (SNVs) have been linked to chronic kidney disease in African Americans, yet differences in the circulating concentration of these protein variants (each can be quantified by mass spectrometry)20 may not correlate with CKD outcome.21 However, it is the protein that provides protection against Trypanosoma brucei rhodesiense22 and the two CKD-variants may confer different, and potentially even opposing, dominant associations with human African trypanosomiasis susceptibility,23 which forms can be measured directly in blood/plasma. Other proteoisoforms involved in heart disease (i.e., 3, 24, 25) and cancer (i.e., 26) have changes in their abundance, which is evidently relevant to healthy tissue or potentially during metastasis.
3. LONGITUDINALLY PROTEOMIC PROFILING OF INDIVIDUALS
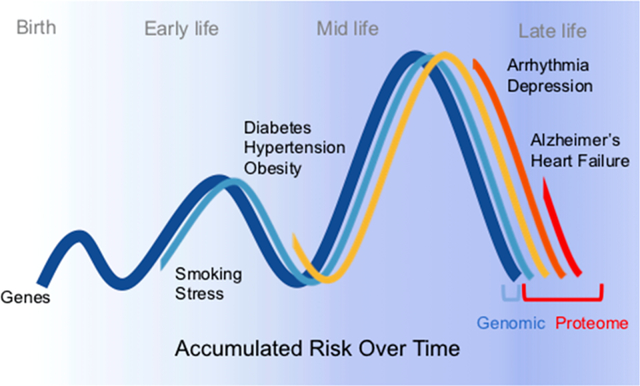
Individuals can have tremendous variability in their biochemical and physiological health baselines (e.g., 1). Moreover, personal accumulated risk will change over the course of their lives. As schematically illustrated in Figure 2, genome, epigenome and proteome contribution due to smoking, stress, obesity, etc., can contribute to increased disease risk with age (top panel). Conceptually, we suggest that frequent assessment of an individual’s proteotypic measures may enable monitoring and insights into individual health, and changes in these measures will enable early detection of disease. This in turn will enable earlier intervention and improve clinical outcomes and possibly increase cost efficiency of the health care system.
Figure 2.

Accumulative risk with aging can be continuously assessed with biomarkers. Top panel, graphically illustrates the effect of genes (dark blue line) over lifetime versus changes induce by various risk factors which can affect the proteomic contribution (light blue, yellow, orange and red) to overall risk burden. Bottom panel, illustrates the conceptual difference between a static versus continuous biomarker monitoring as a means to assign risk over a lifetime.
Moving from a single, static measurement to multiple measurements over time is a cornerstone for the precision proteotyping (Figure 2, lower panel). Today there is only a handful of markers which are monitored over time and there are a few biomarkers that have sex and/or age cut offs established. Rather for many biomarkers, at the individual level, we do know yet know what to expect. The ability to have easy access to dynamic measurements during illness and treatment will enable monitoring of chronic disease progression and an individual’s therapeutic responsiveness. Furthermore, inexpensive remote sampling devices can be deployed in areas where there is limited access to clinical chemistry grade biochemical assays, including underserved areas in cities or in remote regions of the world. These types of devices will allow observational studies of human disease and determine the natural history of diseases. Certainly, remote sampling devices, if deployed in epidemiological and population studies, could dramatically increase the speed, scale and cost saving of sampling. The devices hold great promise, yet today we do not know which biomarkers to use or how often they should be measured.
The collection of remote samples for precision health has challenges. In addition to determining what to measure, important considerations include the type of lance, sample volume, dried or liquid blood or plasma, test location, and stability of the analytes (e.g., ref 27). Dealing with compliance, the usability of blood/plasma collection device, ease of delivering to the lab (if the assay is not done on site), and patient feedback all remain to be solved before this approach can be employed clinically. Equally important is establishing the appropriate menu for each clinical use. As stated above, this will require, establishing clinical utility through appropriate sized and powered cohorts composed of large number of individuals tracked over time. In the meantime, as studies are carried out to build the foundation of evidence and knowledge there will be much that we will learn about disease and biological heterogeneity.
Today, our understanding of disease and health is broad, and we recognize that health is impacted not just from genetic and biochemical factors, but also from behavioral, sociodemographic, and psychological determinants which can have a genetic and biochemical basis (Figure 1). Physiological and other signatures of health and disease which can be obtained from wearable biosensors that provide information, for example, of heart rate, activity, sleep, step count, skin temperature, caloric expenditure, and/or patient reported outcome are used to obtain health related questions from the patient (i.e., refs 28 and 29). Patient reported outcome data and questionnaires can be used to attempt to define psychological and behavioral status. However, biochemistry provides important insights into health and disease, in part due to vast amounts of data that can be measured which reflects that person’s phenotype. An excellent example is continuous glucose monitoring that provides important information into not only glucose levels, but also postprandial levels after meals that can be used to guide health management.30 From the proteomics perspective, physiological parameters impact the proteome and thus should be reflective and measurable in the proteome while conversely, measurements of the proteome should provide insight into human physiology. Furthermore, being able to integrate lifestyle, diet, and societies impact on the biochemical markers will be a particularly important part of understanding the connections between phenotype, genetics, environment, and the biochemistry. However, there needs to be thoughtful and well powered studies to set up the foundation for establishing clinical implication. The understanding of how precision medicine approaches are to be most effectively applied will be crucial for managing the environmental impact on personal wellness, disease progression, and response.
4. MULTIOMICS, BIG DATA VERSUS SMART DATA
It is now possible to collect large amounts of quantitative data on individuals, not just from proteomics, but also from a wide array of other Omics-based and wearable devices. These efforts are likely to uncover novel molecules and pathways important for human health and disease as well as identify biomarkers for diagnostics and prognostics. However, big data is not necessarily smart data, at least for clinical application. It will be important to define the exact data types that are valuable for each purpose. For example, interpretable genomics and epigenomics data will be valuable for disease risk prediction and drug efficacy, response, and side effects. Proteomics and other Omics are expected to be valuable for early diagnosis, treatment and prognosis, and monitoring outcome. Although today combining proteomic data with other data types and in different formats is challenging, such studies are occurring.1,2 The challenge ahead will be to extract which biomarker or combination are best suited for which disease and applications.31 Equally important will be to apply this in an individual fashion at a scale so that implementation on a personal level is possible.
Two advances will likely drive success in this area. First, machine learning methods to extract useful information associated with disease risk, disease detection, and prognosis will be essential. Second, large sums of data are required through aggregation of clinical information, Omics information, and outcome data. In this fashion, matching of treatment with Omics information and outcome data will be essential for the realization of personalized medicine. It is expected that Omics information that closely relates to the clinical phenotype (e.g., proteoisoforms and also metabolomes) will provide the most informative markers for diagnostics, treatment, and prognostics.
5. FUTURE STEPS
The potential to measure large numbers of biomarkers frequently has the potential to revolutionize human healthcare. Sensitive assays can be used to monitor health, detect early signs of disease, and continuously monitor physiology, guide treatments, and follow outcome. However, there are still many challenges. An important consideration for longitudinal profiling of precision health is what to measure and how often, and to do so at an affordable cost. Measures of acute illness and reactions are best suited for frequent and continuous mentoring so that instant feedback can be provided to the individual and physician. Other markers of slow progression might only require sampling annually. The frequency of measurements and types of measurements can be guided by weighing convenience, cost, and value of the measurement and their impact on health. For example, convenient physiological measuring wearables and at home tests at low cost will enable continuous and frequent measurements. Those associated with slow disease progression or are expensive might be performed less frequently. Importantly, since prediction of risk for specific disease will vary from among individuals and will progress to specific chronic diseases, it will be important to develop personal models for health management and treatments. For example, individuals with type 2 diabetes should be measured frequently for neuropathy and kidney markers, whereas those at risk for heart failure should be measure closely for cardiac markers. The construction of a personal, longitudinal health dashboard that is available to both the individual and physician will facilitate precision healthcare in the future. Such information may not only facilitate personal health management, but also provide fundamental insights into human biology and disease.
ACKNOWLEDGMENTS
The work was funded by NIH 5R01DK11018602 (MS), 5R01DK11018602 (MPS), PHIND (MPS), 1R01HL132075-01A (J.E.V.E.); DOD 16W81XWH-16-1-0592 (J.E.V.E.), American Heart Association Challenge Grant (J.E.V.E.), and the Erika J. Glazer chair in Women’s Heart Health (J.E.V.E.); the Barbra Streisand Women’s Heart Center (J.E.V.E.); the Advanced Clinical Biosystems Institute (J.E.V.E.). We thank Irene van den Broek and Nicole Tolan for concept and help on figures and Casey Johnson for edits.
ABBREVIATIONS
- CRP
C-reactive protein
- HDL
high density lipoprotein
- LDL
low density lipoprotein
- MS
mass spectrometry
- PTM
post-translational modification
- %CV
percent coefficient of variance
- PROs
patent reported outcomes
- SNVs
single nucleotide variants
Footnotes
The authors declare the following competing financial interest(s): M.P.S. is a cofounder and scientific advisor for Personalis, SensOmics, and Qbio.J.V.E. is on scientific advisor for Neoteryx.
REFERENCES
- (1).Piening BD; Zhou W; Contrepois K; Röst H; Gu Urban GJ; Mishra T; Hanson BM; Bautista EJ; Leopold S; Yeh CY; Spakowicz D; Banerjee I; Chen C; Kukurba K; Perelman D; Craig C; Colbert E; Salins D; Rego S; Lee S; Zhang C; Wheeler J; Sailani MR; Liang L; Abbott C; Gerstein M; Mardinoglu A; Smith U; Rubin DL; Pitteri S; Sodergren E; McLaughlin TL; Weinstock GM; Snyder MP Integrative Personal Omics Profiles during Periods of Weight Gain and Loss. Cell Syst. 2018, 6, 157–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Chen R; Mias GI; Li-Pook-Than J; Jiang L; Lam HY; Chen R; Miriami E; Karczewski KJ; Hariharan M; Dewey FE; Cheng Y; Clark MJ; Im H; Habegger L; Balasubramanian S; O’Huallachain M; Dudley JT; Hillenmeyer S; Haraksingh R; Sharon D; Euskirchen G; Lacroute P; Bettinger K; Boyle AP; Kasowski M; Grubert F; Seki S; Garcia M; Whirl-Carrillo M; Gallardo M; Blasco MA; Greenberg PL; Snyder P; Klein TE; Altman RB; Butte AJ; Ashley EA; Gerstein M; Nadeau KC; Tang H; Snyder M Personal omics profiling reveals dynamic molecular and medical phenotypes. Cell 2012, 148, 1293–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Aebersold R; Agar JN; Amster IJ; Baker MS; Bertozzi CR; Boja ES; Costello CE; Cravatt BF; Fenselau C; Garcia BA; Ge Y; Gunawardena J; Hendrickson RC; Hergenrother PJ; Huber CG; Ivanov AR; Jensen ON; Jewett MC; Kelleher NL; Kiessling LL; Krogan NJ; Larsen MR; Loo JA; Ogorzalek Loo RR; Lundberg E; MacCoss MJ; Mallick P; Mootha VK; Mrksich M; Muir TW; Patrie SM; Pesavento JJ; Pitteri SJ; Rodriguez H; Saghatelian A; Sandoval W; Schlüter H; Sechi S; Slavoff SA; Smith LM; Snyder MP; Thomas PM; Uhlén M; Van Eyk JE; Vidal M; Walt DR; White FM; Williams ER; Wohlschlager T; Wysocki VH; Yates NA; Young NL; Zhang B How many human proteoforms are there? Nat. Chem. Biol. 2018, 14, 206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Fert-Bober J; Murray CI; Parker SJ; Van Eyk JE Precision Profiling of the Cardiovascular Post-Translationally Modified Proteome: Where There Is a Will, There’s a Way. Circ. Res. 2018, 122, 1221–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Evaluation of Biomarkers and Surrogate Endpoints in Chronic Disease Institute of Medicine (US) Committee on Qualification of Biomarkers and Surrogate Endpoints in Chronic Disease; Micheel CM, Ball JR, Eds.; National Academies Press, 2010. [PubMed] [Google Scholar]
- (6).WHO International Programme on Chemical Safety Biomarkers in Risk Assessment: Validity and Validation. 2001. Retrieved from http://www.inchem.org/documents/ehc/ehc/ehc222.htm.
- (7).Committee on the Review of Omics-Based Tests for Predicting Patient Outcomes in Clinical Trials; Board on Health Care Services; Board on Health Sciences Policy; Institute of Medicine. Evolution of Translational Omics: Lessons Learned and the Path Forward, Micheel CM, Nass SJ, Omenn GS, Eds.; National Academies Press, 2012. [PubMed] [Google Scholar]
- (8).Ahlqvist E; Storm P; Karäjämäki A; Martinell M; Dorkhan M; Carlsson A; Vikman P; Prasad RB; Aly DM; Almgren P; Wessman Y; Shaat N; Spégel P; Mulder H; Lindholm E; Melander O; Hansson O; Malmqvis U; Lernmark A; Lahti K; Forsén T; Tuomi T; Rosengren AH; Groop L Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysi of six variables. Lancet Diabetes Endocrinol. 2018, 6, 361–369. [DOI] [PubMed] [Google Scholar]
- (9).Hoofnagle AN; Roth MY Improving the Measurement of Serum Thyroglobulin With Mass Spectrometry. J. Clin. Endocrinol. Metab. 2013, 9, 1343–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).van den Broek I; Romijn FP; Nouta J; van der Laarse A; Drijfhout JW; Smit NP; van der Burgt YE; Cobbaert CM Automated Multiplex LC-MS/MS Assay for Quantifying Serum Apolipoproteins A-I, B, C-I, C-II, C-III, and E with Qualitative Apolipoprotein E Phenotyping. Clin. Chem. 2016, 6, 188–97. [DOI] [PubMed] [Google Scholar]
- (11).van den Broek I; Nouta J; Razavi M; Yip R; Bladergroen MR; Romijn FP; Smit NP; Drews O; Paape R; Suckau D; Deelder AM; van der Burgt YE; Pearson TW; Anderson NL; Cobbaert CM Quantification of serum apolipoproteins A-I and B-100 in clinical samples using an automated SISCAPA-MALDI-TOFMS workflow. Methods 2015, 81, 74–85. [DOI] [PubMed] [Google Scholar]
- (12).Agger SA; Marney LC; Hoofnagle A Simultaneous Quantification of Apolipoprotein A-I and Apolipoprotein B by Liquid-Chromatography–Multiple-Reaction–Monitoring Mass Spectrometry. Clin. Chem. 2010, 56, 1804–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Dayon L; Núñez Galindo A; Corthésy J; Cominetti O; Kussmann M Comprehensive and Scalable Highly Automated MS-Based Proteomic Workflow for Clinical Biomarker Discovery in Human Plasma. J. Proteome Res. 2014, 13, 3837–3845. [DOI] [PubMed] [Google Scholar]
- (14).Fu Q; Kowalski MP; Mastali M; Parker SJ; Sobhani K; van den Broek I; Hunter CL; Van Eyk JE Highly Reproducible Automated Proteomics Sample Preparation Workflow for Quantitative Mass Spectrometry. J. Proteome Res. 2018, 17, 420–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Jeffrey R; Lei Zhao W; Anderson L; Paulovich AG An Automated and Multiplexed Method for High Throughput Peptide Immunoaffinity Enrichment and Multiple Reaction Monitoring Mass Spectrometry-based Quantification of Protein Biomarkers. Mol. Cell. Proteomics 2010, 9, 184–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).van den Broek I; Sobhani K; Van Eyk JE Advances in quantifying apolipoproteins using LC-MS/MS technology: implications for the clinic. Expert Rev. Proteomics 2017, 14, 869–880. [DOI] [PubMed] [Google Scholar]
- (17).Ray KK; Cannon CP; Cairns R; Morrow DA; Ridker PM; Braunwald E Prognostic utility of apoB/AI, total cholesterol/HDL, non-HDL cholesterol, or hs-CRP as predictors of clinical risk in patients receiving statin therapy after acute coronary syndromes: results from PROVE IT-TIMI. Arterioscler., Thromb., Vasc. Biol. 2009, 29, 424–30. [DOI] [PubMed] [Google Scholar]
- (18).Graversen P; Abildstrom SZ; Jespersen L; Borglykke A; Prescott E Cardiovascular risk prediction: Can Systematic Coronary Risk Evaluation (SCORE) be improved by adding simple risk markers? Results from the Copenhagen City Heart Study. Eur. J. Prev Cardiol. 2016, 23, 1546–56. [DOI] [PubMed] [Google Scholar]
- (19).Yu KH; Levine DA; Zhang H; Chan DW; Zhang Z; Snyder M Predicting Ovarian Cancer Patients’ Clinical Response to Platinum-Based Chemotherapy by Their Tumor Proteomic Signatures. J. Proteome Res. 2016, 15, 2455–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Zhou H; Hoek M; Yi P; Rohm RH; Mahsut A; Brown P; Sanders J; Chmielowski RA; Ren N; Shuster D; Southwick K; Ayanoglu G; Laface D; Santino D; Conway J; Liu Z; Cully D; Cleary M; Roddy TP; Blom D Rapid detection and quantification of apolipoprotein L1 genetic variants and total levels in plasma by ultra-performance liquid chromatography/tandem mass spectrometry. Rapid Commun. Mass Spectrom. 2013, 27, 2639–47. [DOI] [PubMed] [Google Scholar]
- (21).Kozlitina J; Zhou H; Brown PN; Rohn RJ; Pan Y; Ayanoglu G; Du X; Rimmer E; Reilly DF; Roddy RJ; Cully DF; Vogt TF; Blom D; Hoek M Plasma Levels of Risk-Variant APOL1 Do Not Associate with Renal Disease in a Population-Based Cohort. J. Am. Soc. Nephrol. 2016, 27, 3204–3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Limou S; Nelson GW; Kopp JB; Winkler CA APOL1 Kidney Risk Alleles: Population Genetics and Disease Associations. Adv. Chronic Kidney Dis. 2014, 21, 426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Cooper A; Ilboudo H; Alibu VP; Ravel S; Enyaru J; Weir W; Noyes H; Capewell P; Camara M; Milet J; Jamonneau V; Camara O; Matovu E; Bucheton B; MacLeod A APOL1 renal risk variants have contrasting resistance and susceptibility associations with African trypanosomiasis. eLife 2017, 6, e25461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Smith LE; White MY The role of post-translational modifications in acute and chronic cardiovascular disease. Proteomics: Clin. Appl. 2014, 8, 506–21. [DOI] [PubMed] [Google Scholar]
- (25).Cai W; Tucholski TM; Gregorich ZR; Ge Y Top-down Proteomics: Technology Advancements and Applications to Heart Diseases. Expert Rev. Proteomics 2016, 13, 717–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Menon R; Im H; Zhang EY; Wu SL; Chen R; Snyder M; Hancock WS; Omenn GS Distinct splice variants and pathway enrichment in the cell-line models of aggressive human breast cancer subtypes. J. Proteome Res. 2014, 13, 212–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).van den Broek I; Fu Q; Kushon S; Kowalski MP; Millis K; Percy A; Holewinski RJ; Venkatraman V; Van Eyk JE Application of volumetric absorptive microsampling for robust, high-throughput mass spectrometric quantification of circulating protein biomarkers. Journal of Clinical Mass Spectrometry 2017, 4–5, 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Li X; Dunn J; Salins D; Zhou G; Zhou W; Schüssler-Fiorenza Rose SM; Perelman D; Colbert E; Runge R; Rego S; Sonecha R; Datta S; McLaughlin T; Snyder, MP Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol. 2017, 15, e2001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Speier W; Dzubur E; Zide M; Shufelt C; Joung S; Van Eyk JE; Bairey Merz CN; Lopez M; Spiegel B; Arnold C Evaluating utility and compliance in a patient-based eHealth study using continuous-time heart rate and activity trackers. J. Am. Med. Inform Assoc. 2018, 25, 1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Hall H; Perelman D; Breschi A; PaLimcaoco P; Kellogg R; McLaughlin T; Snyder M Glucotypes Reveal New Patterns of Glucose Dysregulation. PLoS Biol. 2018, 16, e2005143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Wright I; Van Eyk JE A Roadmap to Successful Clinical Proteomics. Clin. Chem. 2017, 6, 245–247. [DOI] [PMC free article] [PubMed] [Google Scholar]


