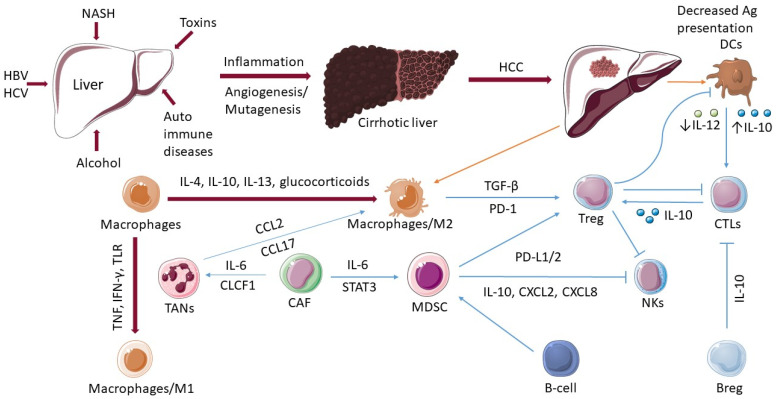
Figure 1.
The role of immune cells in hepatocellular cancer. In the development of HCC, various factors play a decisive role such as hepatitis B virus (HBV), hepatitis C virus (HCV), non-alcoholic fatty liver disease (NAFLD), non-alcoholic steatohepatitis (NASH), toxins, and autoimmune diseases. The actions of numerous immune cells become dysregulated as the disease develops from cirrhosis of the liver to hepatocellular carcinoma (HCC). The ability of dendritic cells (DCs) to present antigens is decreased. The activation of CD8+ T-cells (CTLs) is dependent on the activation of a DCs. Macrophages differentiate into an “alternatively-activated phenotype”, M2, which promotes the recruitment and growth of regulatory T-cells (Tregs). Tregs have a negative impact on CTLs, DCs, and natural killer (NK) cells. M1 macrophages are activated by microbial components or proinflammatory cytokines (TNF, IFN-γ, TLR). Tumor-associated neutrophils (TANs) produce the chemokines, and CCL2 and CCL17 were observed to recruit tumor-associated macrophages (TAMs). Cancer-associated fibroblasts (CAFs) induce activation of TANs via IL-6 and CLCF1 and promote the differentiation of monocytes into MDSCs via IL-6-mediated STAT3 activation. B cells can be associated with pro-tumorigenic processes by activating MDSCs. Regulatory B-cells (Bregs) promote T-cell dysregulation through an IL10-dependent mechanism.