Abstract
Background and Objectives
In the United States, Black, Hispanic, and Asian Americans experience excessively high incidence rates of hemorrhagic stroke compared with White Americans. Women experience higher rates of subarachnoid hemorrhage than men. Previous reviews detailing racial, ethnic, and sex disparities in stroke have focused on ischemic stroke. We performed a scoping review of disparities in the diagnosis and management of hemorrhagic stroke in the United States to identify areas of disparities, research gaps, and evidence to inform efforts aimed at health equity.
Methods
We included studies published after 2010 that assessed racial and ethnic or sex disparities in the diagnosis or management of patients aged 18 years or older in the United States with a primary diagnosis of spontaneous intracerebral hemorrhage or aneurysmal subarachnoid hemorrhage. We did not include studies assessing disparities in incidence, risks, or mortality and functional outcomes of hemorrhagic stroke.
Results
After reviewing 6,161 abstracts and 441 full texts, 59 studies met our inclusion criteria. Four themes emerged. First, few data address disparities in acute hemorrhagic stroke. Second, racial and ethnic disparities in blood pressure control after intracerebral hemorrhage exist and likely contribute to disparities in recurrence rates. Third, racial and ethnic differences in end-of-life care exist, but further work is required to understand whether these differences represent true disparities in care. Fourth, very few studies specifically address sex disparities in hemorrhagic stroke care.
Discussion
Further efforts are necessary to delineate and correct racial, ethnic, and sex disparities in the diagnosis and management of hemorrhagic stroke.
Attention to racial, ethnic, and sex disparities in the diagnosis and management of acute ischemic stroke is surging.1,2 The focus is shifting from documenting disparities in care to seeking solutions and evaluating interventions.3 Less is known about disparities in the diagnosis and management of hemorrhagic stroke, perhaps because ischemic strokes outnumber hemorrhagic strokes in the United States by nearly 7:1.4 Hemorrhagic stroke, however, has substantially higher short-term and long-term mortality compared with ischemic stroke5 and disproportionately afflicts Black, Hispanic, and Asian Americans compared with White Americans.6 Furthermore, the incidence of intracerebral hemorrhage (ICH), the predominant form of hemorrhagic stroke, is increasing.7 Meanwhile, aneurysmal subarachnoid hemorrhage (SAH) disproportionately afflicts women. It is therefore important to understand and address disparities in both ischemic and hemorrhagic stroke. To address this gap, we performed a scoping review of racial, ethnic, and sex disparities pertaining to the diagnosis and management of hemorrhagic stroke. We aimed to identify targets for future research with the goal of improving health equity for hemorrhagic stroke patients.
Methods
We developed a search strategy focusing on racial and ethnic or sex disparities regarding the diagnosis or management of hemorrhagic stroke. We chose a scoping review design to map the literature on the topic and identify key gaps in current research. Scoping reviews differ from systematic reviews because they do not attempt to answer a specific question or inform practice; rather, they identify important concepts or knowledge gaps, delineate the available evidence, and examine how research is conducted in a field.8 We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guideline.9
Standard Protocol Approvals, Registrations, and Patient Consents
This scoping review was not registered. As a scoping review of published literature, we did not seek institutional review board approval.
Eligibility Criteria
We included English language studies that assessed racial and ethnic or sex disparities as either a primary or secondary outcome in the diagnosis or management of patients aged 18 years or older in the United States with a primary diagnosis of spontaneous ICH or aneurysmal SAH. We limited our search to studies after 2010 to accurately portray the current state of disparities. We did not include studies assessing disparities in incidence, risks, or mortality and functional outcomes of hemorrhagic stroke. We excluded studies that did not present results by stroke subtype and disparities by race/ethnicity or sex. Of note, we treated all sex and gender differences as assessments of biologic sex differences because these 2 terms were conflated in most studies, and there were no specific references to gender identity.
Search Strategy and Study Selection
On September 1, 2020, and February 22, 2022, we searched EMBASE, PubMed, and Cochrane Register of Controlled Trials (full search strategy in eAppendix 1, links.lww.com/WNL/C824). We also included any relevant articles found in references of included studies that were not captured in the search. Two authors (L.K., N.A.M.) independently reviewed all abstracts that met the search criteria. In case of disagreement, a third author (M.M.) served as arbiter. We repeated this for a full-text review. We used American Heart Association/American Stroke Association (AHA/ASA) guidelines for the management of ICH and SAH as a framework for reporting our findings, but not to limit the search or grade the strength of the evidence.10,11 When possible, we conformed to the AHA/ASA guidelines on disparities research.12
Data Availability
A full list of studies excluded from the review made by the authors will be available on request.
Results
Our search yielded 6,161 unique studies for screening, and 59 studies met eligibility criteria (Figure; eTable 1, links.lww.com/WNL/C826). Forty-two studies assessed disparities among patients with ICH; 17 studies assessed disparities among patients with SAH. AHA/ASA guideline content areas without any studies meeting study eligibility criteria are summarized in Tables 1 and 2.
Figure. PRISMA Flowchart of Study Selection.
After reviewing 6,161 study abstracts for eligibility, we assessed 444 full-text studies, 59 of which met eligibility criteria for review. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Overview of Disparities in the Diagnosis and Management of ICH
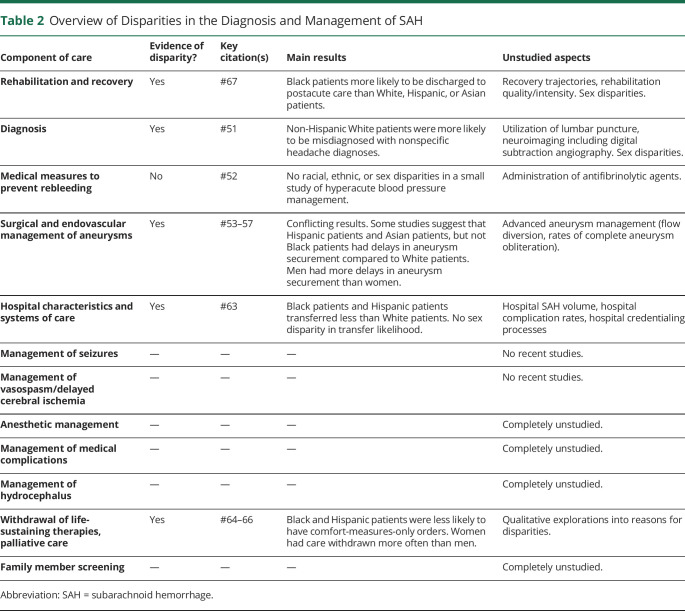
Table 2.
Overview of Disparities in the Diagnosis and Management of SAH
Intracerebral Hemorrhage
Of the 42 studies assessing disparities in patients with ICH, 29 studies assessed racial and ethnic disparities, 5 studies assessed sex disparities, and 8 studies assessed both racial and ethnic and sex disparities. Thirty of 42 studies demonstrated significant disparities or differences in the evaluation or medical management of patients with ICH.
Prehospital and Initial Systems of Care/Diagnostic Assessment
No studies assessed for disparities in prehospital management of patients with ICH. Seven studies assessed emergency department (ED) management care. A retrospective analysis of 543 patients from the National Hospital Ambulatory Medical Care Survey–Emergency Department database that included both ischemic and hemorrhagic stroke types found that Black patients, but not Hispanic patients, had significantly longer ED wait times when they were being evaluated for a possible stroke when compared with White patients.13 A case-control analysis of 123,623 patients from the Get With The Guidelines–Stroke (GWTG-S) registry found that Black patients were less likely than White patients to have a door to CT time of ≤25 minutes after controlling for patient-level and hospital-level characteristics.6 By contrast, a retrospective review of 459 patients with ICH from a single center found that race and ethnicity had no effect on time to bed request or time to admission.14 Conflicting data exist regarding whether Black patients are more likely or not to be screened for drugs of abuse after ICH compared with White patients.15,16 One retrospective study found that male patients with ICH were more likely than female patients with ICH to undergo urine drug screening.16
A retrospective single-center study of 265 patients found that providers activated stroke codes less for female patients presenting with ICH to the ED compared with that for male patients.17 Last, a multivariable analysis of 205 patients from the Genetic and Environmental Risk Factors for Hemorrhagic Stroke study found that Black patients were more likely to be transferred to a tertiary center than non-Black patients presenting to nontertiary EDs.18 Disparities in advanced neuroimaging aimed at identifying underlying pathogenesis such as CT angiography/venography, MRI, or catheter angiography have not been investigated.
Medical and Neurointensive Treatment
Acute Blood Pressure Lowering
One study scrutinized disparities in acute blood pressure management. A multivariate analysis of 2,069 patients from the Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study, a prospective multicenter case-control study of ICH among Black patients, Hispanic patients, and White patients found that Hispanic patients and Black patients had higher prehospital and ED blood pressure compared with White patients and that Black patients continued to have higher blood pressure than both Hispanic patients and White patients 24 hours after admission despite more often receiving continuous antihypertensive infusions.19 We did not find any studies investigating sex disparities in acute blood pressure lowering after ICH.
Anticoagulant-Related Hemorrhage/Antiplatelet-Related Hemorrhage/General Hemostasis
We did not find any studies investigating disparities in the reversal of anticoagulation in patients with anticoagulant-related ICH. In a multiple logistic regression model including more than 2,500 patients with ICH from the ERICH study, Black patients with antiplatelet-related ICH were less likely to receive platelet transfusions after ICH.20 This analysis was performed before the PATCH study, which found no benefit and possible harm from platelet transfusion.21 No studies explored sex disparities in hemostasis.
Inpatient Care Setting/General Medical Management
The AHA/ASA ICH guideline covers multiple aspects of inpatient care including care setting, prevention and management of medical complications, thromboprophylaxis and treatment of thrombosis, nursing care, glucose management, and temperature management. No studies evaluated care setting, nursing care, glucose management, or temperature management.
In the GWTG-S registry, Black patients were more likely than White patients to receive deep vein thrombosis prophylaxis.6 No studies assessed racial, ethnic, or sex disparities in the use of pneumatic boot use or systemic anticoagulation/inferior vena cava filter placement in patients with ICH and symptomatic deep vein thrombosis or pulmonary embolism. Compared with White patients, Asian, Hispanic, and Black patients were more likely to receive dysphagia screening to prevent pneumonia in the GWTG-S registry.6 Sex differences in dysphagia screening have not been examined. In a prospective cohort study of 512 patients from 1 hospital, more non-Hispanic Black patients received percutaneous endoscopic gastrostomy (PEG) tubes than Hispanic or non-Hispanic White patients, but this study did not control for confounders.22 In the same study, higher socioeconomic status was associated with lower odds of pursuing PEG only among Hispanic White patients, suggesting that economic factors may moderate decision-making among different races or ethnicities.
Three retrospective studies using Nationwide Inpatient Study (NIS) data have investigated racial and ethnic PEG placement disparities. A 2016 study of 49,946 ICH admissions found non-White patients were more likely to receive a PEG than White patients, especially in smaller hospitals with lower ICH volumes.23 That finding was confirmed in a separate multivariable analysis from the NIS.24 Another NIS study of 38,080 ICH admissions corroborated the findings but found that hospitals that had ≥ 50% of patients admitted with ICH of either Black race or Hispanic ethnicity did not have higher rates of PEG placement.25 Regarding sex disparities, an analysis from the ERICH study of 2,964 patient records did not find any differences in the placement of PEG tubes.26 In a study of 36,019 admissions from the NIS, minority race/ethnicity (e.g., Hispanic, Black, Asians/Pacific Islander) and male sex were associated with increased odds of nonbeneficial PEG tube placement, with minority male patients more likely than White female patients to receive PEG tube placement.27
Seizures and Antiseizure Medications
An investigation of 744 patients from the ERICH study did not find any racial, ethnic, or sex disparities in the receipt of prophylactic antiseizure medications.28 An analysis of 3,422 patients from a multicenter prospective cohort found that White patients were twice as likely as Black patients to receive seizure prophylaxis after ICH, but the association was eliminated in a single-center subset controlling for hematoma location.29
No studies evaluated for disparities in the application of continuous EEG or utilization of antiseizure medications after seizure. Sex disparities in the utilization of antiseizure medications after ICH have not been investigated.
Neuroinvasive Monitoring, ICP, Edema Treatment, and Surgical Interventions
We found 4 studies addressing disparities in the procedural recommendations of the AHA/ASA ICH guideline: intracranial pressure (ICP) monitoring and treatment, intraventricular hemorrhage (IVH) management, and surgical treatment.
The first study from the NIS of more than 700,000 patients found higher unadjusted rates of external ventricular drain (EVD) utilization and craniectomy among all minority races and ethnicities when compared with White patients. After multivariable adjustment, EVD placement was significantly higher in Black patients than White patients, while craniectomy utilization was higher in Asian or Pacific Islander patients, Hispanic patients, and other patients (but not Black patients) compared with White patients.24 A second retrospective study analyzing 226 Black and White patients from a single institution found that Black patients were more likely to receive an EVD due to higher rates of IVH and hydrocephalus.30An analysis of 2,947 patients from the ERICH study found that there was no significant difference in the use of surgical intervention such as craniotomy or minimally invasive hematoma evacuation between Black, White, and Hispanic patients.31 A second study from ERICH found that EVD utilization, but not other surgical procedures, was increased in male patients with ICH compared with female patients with ICH after adjusting for age, hematoma volume, and hematoma location.26 No studies investigated disparities in ICP monitoring through parenchymal probes or edema therapies.
Outcome Prediction and Goals of Care
More than one-third of the included studies addressed end-of-life management in ICH. Eleven evaluated racial or ethnic differences, 4 evaluated sex differences, and 3 evaluated both. Fifteen of 18 articles demonstrated differences in end-of-life care between racial and ethnic groups or between sexes. Twelve studies found that White patients opted for fewer life-sustaining interventions than Black patients.6,32-42 Prevalence of care limitations was also low among Hispanic patients.6,33,35-37,39-42
Seven studies explicitly included Asian patients. Five studies found that Asian patients have a higher use of life-sustaining interventions than White patients. Three of these studies grouped Asians with other non-White patients to demonstrate that minorities are more likely to use life-sustaining interventions compared with White patients.33,39,40 Three studies found that Asian patients received less palliative care than White patients.6,35,36 A single-center study of 396 patients from Hawaii found that there were no differences in the withdrawal of life-sustaining therapies between non-Hispanic White patients and Native Hawaiian and other Pacific Islander patients after adjusting for age.43
A 2017 study from the NIS of 46,735 admissions found that minority-serving hospitals (e.g., hospitals with >50% minority patients) used less palliative care services regardless of the race of the patient when compared with predominantly White-serving hospitals (e.g., hospitals with <25% minority patients).39 In addition, the same study noted that racial and ethnic minorities received less palliative care than White patients independent of hospital status as minority serving or not.
Studies of sex disparities in end-of-life care have reached disparate conclusions. A single-center prospective study of 245 patients from 2013 found that new do-not-resuscitate (DNR) orders were placed more often for female patients with ICH than for male patients with ICH in the first 24 hours of admission despite no significant differences in clinical severity, hemorrhage volume, or medical comorbidities.44 A retrospective single-center study of 372 patients from 2013 confirmed that after adjustment for relevant variables, early DNR orders were more likely for female patients than for male patients.45 A national analysis of 176 hospitals in the United States found that among 8,069 patients with ICH, female patients were more likely to be discharged to hospice after controlling for age.46 These findings were further supported by 2 large NIS studies that found increased DNR and palliative care use in female patients compared with those in male patients.35,41 Smaller, more recent single-center studies have not found sex differences in the use or timing of DNR orders36,40 nor did an ERICH study looking at DNR, palliative care, and hospice use after controlling for ICH score, prior stroke, and dementia.26
Post-ICH Recovery, Rehabilitation, and Complications
Results from the GWTG-S registry indicated that Black patients were more likely than White patients to receive a rehabilitation assessment during their hospital stay. Black patients, but not Hispanic or Asian patients, were less likely to be discharged to an inpatient rehabilitation facility compared with White patients.6
Secondary Prevention
Three studies found that Black patients are at a higher risk of ICH recurrence compared with White patients.47-49 One of those studies, using records from a single center and the ERICH study found that among 2,291 patients, Hispanic patients are also at an increased risk,47 while a longitudinal analysis of prospectively collected claims data from 31,355 patients at nonfederal California hospitals found that Asian patients and not Hispanic patients are at an increased risk.48 A single-center prospective cohort study of 1,305 patients found that non-White patients were at a higher risk of uncontrolled hypertension at 3 months when compared with White patients, partially due to inadequately prescribed antihypertensive medication.49 A prospective cohort study of 162 patients found that Black patients were more likely to have stage I/II hypertension 1 year after ICH than White patients despite showing no difference in hypertension at 30 days.50 Analysis from a combined single-center and ERICH cohort found that Black and Hispanic patients had more hypertension at follow-up, but this finding only partially explained their excess ICH recurrence risk.47 No studies investigated sex disparities in blood pressure management after ICH nor disparities in the management of medications including antithrombotic agents, lifestyle modifications, or patient/caregiver education.
Subarachnoid Hemorrhage
We found 10 studies focused on racial/ethnic disparities, 3 looking at sex disparities, and 4 looking at both in the diagnosis and management of SAH. Seven focused on time to treatment, and 1 focused on time to admission.
Diagnostic Assessment of SAH
An administrative claims study of more than 3,500,000 patient records from 2006 to 2012 found that among patients discharged to home from the ED with a nonspecific diagnosis of headache, male sex and non-Hispanic White race were associated with a significantly higher incidence of returning with a life-threatening neurologic condition.e1 SAH was the second most common missed serious neurologic condition (after ischemic stroke), while ICH was the seventh most common.
Medical Measures to Prevent Rebleeding After SAH
A small study from the Greater Cincinnati/Northern Kentucky Stroke Study found no racial, ethnic, or sex disparities in hyperacute blood pressure management after SAH in a cohort of 94 patients.e2 No studies addressed disparities in antifibrinolytic therapy.
Surgical and Endovascular Methods of Treatment of Ruptured Cerebral Aneurysms
Nine studies probed disparities in aneurysm treatment with 6 studies focused on racial and ethnic disparities and 3 on sex disparities. Five studies considering racial and ethnic disparities in time to SAH treatment yielded conflicting results. Two studies found longer delays to aneurysm treatment for racial and ethnic minorities compared with those for White patients,e3,e4 while 3 other studies did not.e5-e7 The 2 studies that reported disparities in time to SAH treatment both analyzed the NIS. The first examined 78,070 patients from 2002 to 2010 who underwent either clip placement or coil embolization.e3 Using a multivariable model, they found that Hispanic patients had a 46% increased likelihood of delayed clipping or coiling compared with White patients. Disparities were not found for other races or ethnicities. The second study assessed disparities in 7,109 patients who underwent endovascular coiling procedures from 2002 to 2011.e4 They found that Hispanic patients and Asian Pacific patients, but not Black patients or Native American patients, were more likely to have delays in treatment compared with White patients.
Another study from the NIS evaluated for disparities in the treatment of Hispanic patients in southwestern border states (California, Arizona, New Mexico, and Texas). In a cohort of 18,368 patients, they found that Hispanic patients in border states were more likely than non-Hispanic White patients to undergo surgical clipping rather than coiling as a treatment for SAH. This difference was not present in nonborder states.e8
NIS data from 1998 to 2007 found potential racial disparities in the proportion of patients treated through clipping vs coiling. In a cohort of 20,134 patients, White patients had a higher likelihood of coil embolization than Black patients from 1998 to 2002. After the publication of the International Subarachnoid Aneurysm Trial in 2002, which found improved 1-year outcomes for those treated by endovascular coiling,e9 the difference decreased but did not disappear.e10
Regarding sex disparities, 2 studies analyzing data from the NIS found that female patients were treated earlier than male patients.e4,e11 Regarding the decision to clip vs coil, data from NIS suggest that male patients were more likely than female patients to be treated by coil embolization until 2002 when this difference dissipated.e10 A study analyzing 21,047 discharges from NIS 2003–2008 found that female patients were more likely than male patients to have an aneurysm clipped or coiled after SAH.e12 Disparities in advanced aneurysm management techniques and rates of complete aneurysm obliteration have not been evaluated.
Hospital Characteristics and Systems of Care
A study of 4,373 patients from the NIS that controlled for hospital and patient characteristics found Black patients and Hispanic patients were less likely to be transferred than White patients.e13 In the same analysis, there was no significant difference by sex in transfer status. The study did not account for the volume of patients with SAH treated as a hospital characteristic.
Withdrawal of Life-Sustaining Therapies, Palliative Care
We found conflicting evidence in the evaluation of differences in the withdrawal of life-sustaining therapies. A multivariate-adjusted analysis of 8,912 patients from the NIS from 2002 to 2010 found that female patients were more likely than male patients to have care withdrawn after SAH. Patients in whom care was withdrawn were less likely to be Black or Hispanic than White individuals in the same analysis.e14 A prospectively enrolled observational study of 1,255 patients at a single center found that Hispanic patients were less likely than White patients to receive comfort-measures-only orders, after adjusting for age and Hunt-Hess grade.e15 There were no significant sex differences. A different prospective observational single-center study of 1,134 patients did not find any racial, ethnic, or sex differences in the withdrawal of life-sustaining therapies.e16
Rehabilitation and Recovery
Data from 31,631 admissions from the NIS from 2005 to 2010 indicated that Black patients were more likely than White patients to be discharged to postacute care despite a similar risk of death.e17 White, Hispanic, Asian/Pacific Islander, and Native American patients were all discharged to postacute care facilities at similar rates.
Discussion
In our scoping review of racial, ethnic, and sex disparities in the diagnosis and management of hemorrhagic stroke among adult patients in the United States, several themes emerged. First, hemorrhagic stroke disparities remain to be elucidated in key aspects of care. Second, racial and ethnic disparities may exist in long-term blood pressure management after ICH, which may contribute to increased recurrence rates among Black and Hispanic patients. Third, both racial and ethnic differences and sex differences in end-of-life care likely exist in both forms of hemorrhagic stroke. Finally, there is a paucity of research on sex disparities in the diagnosis and management of hemorrhagic stroke, especially in SAH. Given the high incidence of SAH in women, it is important to investigate whether there are any sex disparities.
The relative lack of disparity research in hemorrhagic stroke is likely partially explained by its low incidence. Other factors may contribute. While the management of acute ischemic stroke is delineated by guidelines with strong recommendations based on high-quality evidence,e18 the optimal management of hemorrhagic stroke patients remains less certain.e19 Clear quality metrics were only just released for ICH and are yet to be released for SAH.e20 In the AHA/ASA guidelines for ICH, few are guided by high-level evidence. For SAH, Level A evidence guides only 2/53 recommendations. Critical process measures have not been clearly identified, and thus, disparities in process measures may be understudied. The absence of consensus surrounding the management of patients with hemorrhagic stroke may increase disparities. Weak evidence leads to uncertainty, which promotes clinician discretion and opportunities for bias.e21 Higher levels of evidence clarify best practices and may reduce disparity. Before the publication of the International Subarachnoid Aneurysm Trial study, White patients were more likely than Black patients to have their aneurysms coiled, but this disparity decreased after the publication of high-quality data.e10
One notable area of therapeutic disparity despite strong evidence is blood pressure management to prevent recurrence of ICH. Black patients and Hispanic patients continue to have higher blood pressure at long-term follow-up after ICH compared with White patients.47,49,50 Persistent hypertension after ICH contributes to racial and ethnic disparities in ICH recurrence rates47 and is partially explained by inadequate antihypertensive prescribing.49 Racial and ethnic disparities in hypertension are not unique to patients after ICH. The causes are multifactorial and include health care access, other social determinants of health, and biologic differences.e22 In the case of post-ICH hypertension, presentation with such a catastrophic event should ameliorate issues of awareness and access. Innovative approaches should be pursued such as telehealth models, targeted stroke clinics, or health coaching embedded in community settings as secondary prevention of persistent hypertension and recurrent hemorrhagic stroke.e23-e25
The best studied area in hemorrhagic stroke disparities or differences is the receipt or withholding of life-sustaining therapies and palliative care services. As in cohorts of patients with acute myocardial infarction or more general cohorts of hospitalized patients,e26 Black patients (or their surrogates) consistently opt for more aggressive treatments and less care limitations than White patients. This preference may protect Black patients from self-fulfilling prophecies whereby erroneous poor prognoses drive poor outcomes through premature withdrawal of care.33 A Hispanic paradox, whereby Hispanic individuals “paradoxically” have similar or better health outcomes than non-Hispanic White individuals despite lower socioeconomic status, has been previously described and attributed to self-selection in migration patterns; however, this explanation does not adequately explain the paradox.e27 A preference for more aggressive care in Hispanic patients and their surrogates may contribute.
The reasons for racial differences in care limitations or acceptance of palliative care remain uncertain. Authors have suggested a combination of several factors including differences in spirituality, health care system distrust, and beliefs about dying.e28 Much of the variation in DNR utilization, however, is not reflective of patient preference. Significant variation occurs on the hospital and regional level.e29 Thus, some of the differences may reflect true disparity as opposed to culturally appropriate care. More qualitative studies to evaluate differences in end-of-life care in hemorrhagic stroke would be a logical next step in understanding disparities.
Female patients may be more likely than men to receive DNR orders and palliative care after hemorrhagic stroke, although studies do exist to the contrary.26 Data from other catastrophic disease states such as cardiac arrest support the supposition.e30 A survey of 1,648 adults did not find sex difference in the acceptance of life-prolonging treatments at end of life, suggesting that disparities in DNR orders are not driven by patient preference, but instead by medical providers or patient surrogates.e31 Patient comorbidities may also contribute to disparity of care, such as older age and greater frequency of cognitive impairment in female patients presenting with ICH when compared with men.
Our study has several limitations. First, many included studies came from large administrative databases, which lack data regarding important confounders. Single-center studies included such data but may not be generalizable to larger populations. Prospectively collected data from the ERICH study, which comprised 9 of the 40 reviewed ICH studies, bridge this gap but can be biased from self-selection into a study whose purpose is to study racial and ethnic variation and a Hawthorne effect. A corollary to ERICH is not available for SAH. Second, we could not adhere to best practices in disparities research because many studies were published before disparities research guidelines were available.12 We could not always describe how race and ethnicity were categorized because those details were not available. Some studies conflated race and ethnicity. Patients could not be classified into multiple categories. Important racial and ethnic groups, such as American Indians and Alaska Natives, were ignored or subsumed into larger population groups. Substantial heterogeneity exists within racial and ethnic groups that are treated as a single category but span vast differences in geography, language, ancestry, and lived experience such as Hispanic/Latino or Asian. Key contributions from Hawaii illuminate this fallacy because they found disparities in different racial and ethnic groups that would be undiscovered had they been lumped together as “Asian.”e32 Third, descriptors of structural racism were largely absent despite their key role in perpetuating health inequities.e30 Fourth, sex and gender were conflated, and we assumed that studies reporting gender differences were actually reporting sex differences. Conflation of sex and gender favors biologic explanations based on sex traits that may be less relevant to health care disparities than systemic discrimination based on the societal roles occupied by patients that identify as women. We found no studies explicitly evaluating gender identity disparities. By equating sex and gender and presuming a gender binary, the available literature fails to address patients with hemorrhagic stroke that are not cisgender or that are nonbinary, limiting its generalizability.
Disparities in the care of hemorrhagic stroke patients exist, especially in long-term blood pressure management and end-of-life care. More work is necessary to evaluate other aspects of care, elucidate causes, and develop solutions.
Glossary
- AHA
American Heart Association
- ASA
American Stroke Association
- DNR
do not resuscitate
- ED
emergency department
- ERICH
Ethnic/Racial Variations of Intracerebral Hemorrhage
- EVD
external ventricular drain
- GWTG-S
Get With The Guidelines–Stroke
- ICH
intracerebral hemorrhage
- ICP
intracranial pressure
- IVH
intraventricular hemorrhage
- NIS
Nationwide Inpatient Study
- PEG
percutaneous endoscopic gastrostomy
- SAH
subarachnoid hemorrhage
Appendix. Authors
Footnotes
CME Course: NPub.org/cmelist
Study Funding
No targeted funding reported.
Disclosure
L. Kalasapudi, S. Williamson, A.G. Shipper, M. Motta, C. Esenwa, and F.O. Otite report no disclosures relevant to the manuscript. S. Chaturvedi serves as a consultant for Astra Zeneca, an Associate Editor for Stroke, and on the Editorial Board for Neurology® and Journal of Stroke and Cerbrovascular Disease. N.A. Morris serves on the Editorial Board for Neurology. Go to Neurology.org/N for full disclosures.
References
- 1.Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(7):2091-2116. [DOI] [PubMed] [Google Scholar]
- 2.Bushnell C, Howard VJ, Lisabeth L, et al. Sex differences in the evaluation and treatment of acute ischaemic stroke. Lancet Neurol. 2018;17(7):641-650. [DOI] [PubMed] [Google Scholar]
- 3.Ovbiagele B. HEADS-UP: understanding and problem-solving: seeking hands-down solutions to major inequities in stroke. Stroke. 2020;51(11):3375-3381. [DOI] [PubMed] [Google Scholar]
- 4.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics: 2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. [DOI] [PubMed] [Google Scholar]
- 5.Waziry R, Heshmatollah A, Bos D, et al. Time trends in survival following first hemorrhagic or ischemic stroke between 1991 and 2015 in the Rotterdam study. Stroke. 2020;51(3):824-829. [DOI] [PubMed] [Google Scholar]
- 6.Xian Y, Holloway RG, Smith EE, et al. Racial/ethnic differences in process of care and outcomes among patients hospitalized with intracerebral hemorrhage. Stroke. 2014;45(11):3243-3250. [DOI] [PubMed] [Google Scholar]
- 7.Bako AT, Pan A, Potter T, et al. Contemporary trends in the nationwide incidence of primary intracerebral hemorrhage. Stroke. 2022;53(3):e70-e74. [DOI] [PubMed] [Google Scholar]
- 8.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. [DOI] [PubMed] [Google Scholar]
- 10.Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282-e361. [DOI] [PubMed] [Google Scholar]
- 11.Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711-1737. [DOI] [PubMed] [Google Scholar]
- 12.Breathett K, Spatz ES, Kramer DB, et al. The groundwater of racial and ethnic disparities research: a statement from circulation: cardiovascular quality and outcomes. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karve SJ, Balkrishnan R, Mohammad YM, Levine DA. Racial/ethnic disparities in emergency department waiting time for stroke patients in the United States. J Stroke Cerebrovasc Dis. 2011;20(1):30-40. [DOI] [PubMed] [Google Scholar]
- 14.Su CM, Warren A, Kraus C, et al. Lack of racial and ethnic-based differences in acute care delivery in intracerebral hemorrhage. Int J Emerg Med. 2021;14(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tormoehlen LM, Blatsioris AD, Moser EA, et al. Disparities and guideline adherence in drugs of abuse screening in intracerebral hemorrhage. Neurology. 2017;88(3):252-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osman S, Zhu Z, Farag M, et al. Intracerebral hemorrhage: who gets tested for methamphetamine use and why might it matter? BMC Neurol. 2020;20(1):392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doelfel SR, Kalagara R, Han EJ, et al. Gender disparities in stroke code activation in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(12):106119. [DOI] [PubMed] [Google Scholar]
- 18.Adeoye O, Haverbusch M, Woo D, et al. Is ED disposition associated with intracerebral hemorrhage mortality? Am J Emerg Med. 2011;29(4):391-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koch S, Elkind MS, Testai FD, et al. Racial-ethnic disparities in acute blood pressure after intracerebral hemorrhage. Neurology. 2016;87(8):786-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guerrero WR, Gonzales NR, Sekar P, et al. Variability in the use of platelet transfusion in patients with intracerebral hemorrhage: observations from the ethnic/racial variations of intracerebral hemorrhage study. J Stroke Cerebrovasc Dis. 2017;26(9):1974-1980. [DOI] [PubMed] [Google Scholar]
- 21.Baharoglu MI, Cordonnier C, Al-Shahi Salman R, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016;387(10038):2605-2613. [DOI] [PubMed] [Google Scholar]
- 22.Garcia RM, Prabhakaran S, Richards CT, Naidech AM, Maas MB. Race, socioeconomic status, and gastrostomy after spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2020;29(2):104567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Faigle R, Bahouth MN, Urrutia VC, Gottesman RF. Racial and socioeconomic disparities in gastrostomy tube placement after intracerebral hemorrhage in the United States. Stroke. 2016;47(4):964-970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cruz-Flores S, Rodriguez GJ, Chaudhry MRA, et al. Racial/ethnic disparities in hospital utilization in intracerebral hemorrhage. Int J Stroke. 2019;14(7):686-695. [DOI] [PubMed] [Google Scholar]
- 25.Hwang DY, George BP, Kelly AG, Schneider EB, Sheth KN, Holloway RG. Variability in gastrostomy tube placement for intracerebral hemorrhage patients at US hospitals. J Stroke Cerebrovasc Dis. 2018;27(4):978-987. [DOI] [PubMed] [Google Scholar]
- 26.Guha R, Boehme A, Demel SL, et al. Aggressiveness of care following intracerebral hemorrhage in women and men. Neurology. 2017;89(4):349-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faigle R, Carrese JA, Cooper LA, Urrutia VC, Gottesman RF. Minority race and male sex as risk factors for non-beneficial gastrostomy tube placements after stroke. PLoS One. 2018;13(1):e0191293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheth KN, Martini SR, Moomaw CJ, et al. Prophylactic antiepileptic drug use and outcome in the ethnic/racial variations of intracerebral hemorrhage study. Stroke. 2015;46(12):3532-3535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naidech AM, Toledo P, Prabhakaran S, Holl JL. Disparities in the use of seizure medications after intracerebral hemorrhage. Stroke. 2017;48(3):802-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faigle R, Marsh EB, Llinas RH, Urrutia VC, Gottesman RF. Race-specific predictors of mortality in intracerebral hemorrhage: differential impacts of intraventricular hemorrhage and age among Blacks and Whites. J Am Heart Assoc. 2016;5(8):e003540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen CJ, Ding D, Ironside N, et al. Predictors of surgical intervention in patients with spontaneous intracerebral hemorrhage. World Neurosurg. 2019;123:e700-e708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ormseth CH, Falcone GJ, Jasak SD, et al. Minority patients are less likely to undergo withdrawal of care after spontaneous intracerebral hemorrhage. Neurocrit Care. 2018;29(3):419-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hemphill JC, 3rd, Newman J, Zhao S, Johnston SC. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. Stroke. 2004;35(5):1130-1134. [DOI] [PubMed] [Google Scholar]
- 34.Fraser SM, Torres GL, Cai C, Choi HA, Sharrief A, Chang TR. Race is a predictor of withdrawal of life support in patients with intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2018;27(11):3108-3114. [DOI] [PubMed] [Google Scholar]
- 35.Murthy SB, Moradiya Y, Hanley DF, Ziai WC. Palliative care utilization in nontraumatic intracerebral hemorrhage in the United States. Crit Care Med. 2016;44(3):575-582. [DOI] [PubMed] [Google Scholar]
- 36.Lillemoe K, Lord A, Torres J, Ishida K, Czeisler B, Lewis A. Factors associated with DNR status after nontraumatic intracranial hemorrhage. Neurohospitalist. 2020;10(3):168-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zahuranec DB, Brown DL, Lisabeth LD, et al. Ethnic differences in do-not-resuscitate orders after intracerebral hemorrhage. Crit Care Med. 2009;37(10):2807-2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zurasky JA, Aiyagari V, Zazulia AR, Shackelford A, Diringer MN. Early mortality following spontaneous intracerebral hemorrhage. Neurology. 2005;64(4):725-727. [DOI] [PubMed] [Google Scholar]
- 39.Faigle R, Ziai WC, Urrutia VC, Cooper LA, Gottesman RF. Racial differences in palliative care use after stroke in majority-white, minority-serving, and racially integrated U.S. hospitals. Crit Care Med. 2017;45(12):2046-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McFarlin J, Hailey CE, Qi W, et al. Associations between patient characteristics and a new, early do-not-attempt resuscitation order after intracerebral hemorrhage. J Palliat Med. 2018;21(8):1161-1165. [DOI] [PubMed] [Google Scholar]
- 41.Patel AA, Mahajan A, Benjo A, et al. A national perspective of do-not-resuscitate order utilization predictors in intracerebral hemorrhage. Neurohospitalist. 2016;6(1):7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suolang D, Chen BJ, Faigle R. Temporal trends in racial and ethnic disparities in palliative care use after intracerebral hemorrhage in the United States. Stroke. 2022;53(3):e85-e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shaw KM, Gallek MJ, Sheppard KG, et al. Ethnic differences in withdrawal of life support after intracerebral hemorrhage. Hawaii J Med Public Health. 2015;74(6):203-209. [PMC free article] [PubMed] [Google Scholar]
- 44.Ganti L, Jain A, Yerragondu N, et al. Female gender remains an independent risk factor for poor outcome after acute nontraumatic intracerebral hemorrhage. Neurol Res Int. 2013;2013:219097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakagawa K, Vento MA, Seto TB, et al. Sex differences in the use of early do-not-resuscitate orders after intracerebral hemorrhage. Stroke. 2013;44(11):3229-3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Craen A, Mangal R, Stead TG, Ganti L. Gender differences in outcomes after non-traumatic intracerebral hemorrhage. Cureus. 2019;11(10):e5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rodriguez-Torres A, Murphy M, Kourkoulis C, et al. Hypertension and intracerebral hemorrhage recurrence among white, black, and Hispanic individuals. Neurology. 2018;91(1):e37-e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leasure A, King Z, Torres-Lopez V, et al. Racial/ethnic disparities in the risk of intracerebral hemorrhage recurrence. Neurology. 2019;92(15):e314-e322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Biffi A, Teo KC, Castello JP, et al. Impact of uncontrolled hypertension at 3 months after intracerebral hemorrhage. J Am Heart Assoc. 2021;10(11):e020392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zahuranec DB, Wing JJ, Edwards DF, et al. Poor long-term blood pressure control after intracerebral hemorrhage in a predominantly african american hypertensive population. Stroke. 2012;43(2):2580-2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- eReferences are listed at; links.lww.com/WNL/C825.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A full list of studies excluded from the review made by the authors will be available on request.