Abstract
Purpose
Kienböck’s disease consists of intrinsic and extrinsic characteristics that coalesce into a pathology with multifactorial etiology. Mechanical, morphological, and vascular factors have been identified as contributory. Radial osteotomy is one of the most commonly used surgical treatment for late-stage Kienböck’s disease. Despite its frequent use and reported value, the specifics of radial osteotomy have not been described in aggregate. Our objective was to review the recent literature for descriptions of the radial osteotomy techniques used for treatment of Kienböck’s disease.
Methods
The inclusion criteria for the systematic review were as follows: (1) patients aged >18 years, (2) a publication date no older than 2012, and (3) a complete description of the distal radius osteotomy technique, including verbiage that specified numeric dimensions of bony resection or verbiage that detailed a goal in terms of a radiographic parameter that would guide the bony resection.
Results
The studies were grouped according to the stated description of radial osteotomy. This process yielded the following three main groups: (1) studies that used radial shortening, (2) studies that used lateral closing wedge osteotomy or combined lateral closing wedge with radial shortening, and (3) novel osteotomy descriptions.
Conclusions
The Kienböck’s disease literature predominantly describes an osteotomy to shorten the radius by 2–3 mm. In some studies, the degree of radial shortening corresponded to the value necessary to achieve near-neutral ulnar variance. The common goal in using lateral closing wedge osteotomy was to achieve a radial inclination of 5° to 15°. Unique wedge resections, some with multiplanar corrections, have been recently described with each purporting specific advantages.
Clinical relevance
Our findings support the premise of mechanical and biologic efficacy for radial osteotomy, with satisfactory results being reported across a wide spectrum of osteotomy techniques.
Key words: Distal radius osteotomy, Distal radius shortening, Kienböck’s disease, Lunatomalacia
Kienböck’s disease consists of intrinsic and extrinsic characteristics that coalesce into a pathology with multifactorial etiology. Mechanical, morphological, and vascular factors have been identified as contributory. When surgical treatment is indicated, preferred options encompass a wide spectrum from osteotomy of the capitate and radius, vascularized bone grafting, and core decompression to salvage procedures, such as wrist arthrodesis and proximal row carpectomy.1,2 Factors associated with choice in surgical technique include stage of disease, degree of symptomology, and patient characteristics.
Radial osteotomy is one of the most used surgical treatments for late-stage Kienböck’s disease, the intent being to decrease applied loads on the lunate. Various techniques of radial osteotomy have been described, with radial shortening (RS) and lateral closing wedge osteotomy (LCWO) being the most common. Clinical outcomes have been generally satisfactory across the spectrum of osteotomy techniques; however, there is conflicting evidence.3, 4, 5, 6 A recent systematic review showed superior clinical outcomes including pain and wrist range of motion in cases of Kienböck’s disease treated with radial osteotomy compared with cases treated nonsurgically.4 Importantly, the authors noted that the radial osteotomy group had more advanced disease than the nonsurgical group. A biomechanical study has validated the decompressive effect of radial osteotomy on the lunate.5 The magnitude of lunate unloading substantially varied between osteotomy techniques, with some techniques providing minimal decrease in radiolunate loading.
Despite its frequent use and reported value, the specifics of radial osteotomy for Kienböck’s disease have not been described in aggregate. The dimensions and osseous location of radial osteotomy are integral characteristics which require consideration. These variables combine to yield a change in mechanics which may reduce biologic stress and loading onto the lunate. These factors may induce the desired adaptations. Additionally, characteristics of the radial osteotomy may contribute to redistribution of loads across the wrist and restore a more native relationship of the soft tissues.
Our objective was to review the recent literature to compare clinical outcomes among the various types of radial osteotomy techniques used for the treatment of Kienböck’s disease. Despite the rarity of this disorder, our understanding has improved for its pathophysiology and the mechanical and biologic enhancement provided by surgical intervention. The current endeavor aims to clarify the outcomes for one of the most common surgical treatment options for Kienböck's disease-the radial osteotomy.
Materials and Methods
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses protocol, a search of peer-reviewed English-language literature was performed in PubMed on May 15, 2022. The search terms included “Kienböck AND osteotomy,” “Kienböck’s AND osteotomy,” and “radius AND joint leveling.” The inclusion criteria were as follows: (1) patients aged >18 years, (2) a publication date no older than 2012, and (3) a complete description of the distal radius osteotomy technique, including verbiage that specified numeric dimensions of bony resection or verbiage that detailed a numeric goal in terms of a radiographic parameter that would guide the bony resection. The exclusion criteria were as follows: (1) studies conducted in patients aged <18 years, (2) studies conducted before 2012, and (3) studies with an insufficient description of the distal radius osteotomy technique.
Data collection
Clinical and surgical data were collected from the included studies. Clinical data included demographic variables, study variables, and outcome metrics. Surgical data included the type of distal radius osteotomy and the details of the osteotomy. These details were the dimensions of bony resection or the numeric goal in terms of a radiographic parameter that dictated the dimensions of bony resection. The radiographic parameters were ulnar variance, radial inclination, and volar tilt. Clinical outcomes that could be stratified by type of radius osteotomy were collected, including the Disabilities of the Arm, Shoulder, and Hand (DASH) score, the Modified Mayo Wrist Score (MMWS), and a visual analog scale (VAS) score for pain.
Subgroup formation
The studies were grouped according to the stated description of radial osteotomy. This process yielded the following 3 groups: (1) studies that used radial shortening (RS) (Table 1), (2) studies that used lateral closing wedge osteotomy (LCWO) or a combination of LCWO and RS (Table 2), and (3) novel osteotomy descriptions (Table 3).
Table 1.
Case Details for Treatment of Kienböck’s Disease With RS Osteotomy
| Study | N | Age∗ (y) | Lichtman Stage† | Follow-Up Term‡ |
|---|---|---|---|---|
| van Leeuwen et al,7 2021 | 14 | 40 | II/IIIA | 13 y |
| Botelheiro et al,10 2019 | 21 | 32 | IIIB | 8 y |
| Ebrahimzadeh et al,14 2015 | 16 | 30 | II/IIIA/IIIB | 7 y |
| Dehghani et al,16 2014 | 12 | 35.2 | II/IIIA | NR |
| Matsui et al,8 2014 | 11 | 24 | IIIA/IIIB/IV | 14.3 y |
| Kayaokay et al,11 2021 | 14 | 34.1 | II/IIIA | 49 mo |
| Mozaffarian et al,12 2012 | 27 | 38.3 | IIIB/IV | 4.6 y |
| Luegmair et al,9 2017 | 36 | 30 | IIIA | 12.1 y |
| Tatebe et al,17 2016 | 8 | 37 | II/IIIA/IIIB | 11.5 y |
| Unal et al,13 2021 | 14 | 33 | IIIA | 4.5 y |
| Afshar et al,15 2015 | 12 | 34 | IIIA | 3.2 y |
| Shiota et al,18 2022 | 9 | 35 | II/IIIA/IIIB | 1 y |
| Total§ | 194 | 33.5 | 7.5 y |
NR, not reported.
Age is reported as a mean in years.
Stage is reported using the Lichtman classification for Kienböck’s disease.
Follow-up term is reported in months or years.
Total—N is reported as sum, and age and follow-up are reported as means.
Table 2.
Case Details for Treatment of Kienböck’s Disease With LCWO and Combined LCWO and RS Osteotomy
| Study | N | Age∗ (y) | Lichtman Stage† | Follow-Up Term‡ |
|---|---|---|---|---|
| LCWO | ||||
| Unal et al,13 2021 | 15 | 34 | IIIA | 4.5 y |
| Shin et al,20 2017 | 25 | 31.7 | IIIA/IIIB | 85.6 mo |
| Tatebe et al,17 2016 | 8 | 37 | NR | 10 y |
| Yamamoto I et al,21 2021 | 12 | 23 | II/IIIB | 4 y |
| Yamamoto II et al,21 2021 | 9 | 56 | II/IIIB | 3.7 y |
| Lee et al,19 2021 | 12 | 25 | IIIA/IIIB | 3 y |
| Total§ | 81 | 34.5 | 5.4 y | |
| LCWO + RS osteotomy | ||||
| Hong et al,22 2019 | 18 | 37 | IIIA/IIIB | 22.3 mo |
| Shin et al,20 2017 | 25 | 31.7 | IIIA/IIIB | 85.6 mo |
| Total§ | 43 | 34.4 | 4.5 y |
NR, not reported.
Age is reported as a mean in years.
Stage is reported using the Lichtman classification for Kienböck’s disease.
Follow-up term is reported in months or years.
Total—N is reported as sum, age and follow-up are reported as means.
Table 3.
Osteotomy Details and Clinical Outcomes for Kienböck’s Disease Cases Treated Novel Radial Osteotomy Techniques
| Study | N | Follow-Up Term∗ | Osteotomy Dimensions | Osteotomy Goal | Clinical Outcome Metrics∗ |
|
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | |||||
| Oblique medial CWO | ||||||
| Camus et al,23 2012 | 10 | 7 y | 2-mm wedge base | >12° lunate fossa slope | Grip strength, 13.5 kg; pain, 8.3 | Grip strength, 31 kg; pain, 1.6 |
| TRO without shortening | ||||||
| Blanco and Blanco,24 2012 | 11 | 3.3 y | Induce biologic response without shortening | Grip strength, 29 kg; RoM 73° | Grip strength, 38 kg; RoM, 96° | |
| Biplanar DLCWO | ||||||
| Barrera-Ochoa et al,25 2018 | 11 | 3.3 y | <15° radial inclination and <5° volar tilt | QuickDASH, 32.1; MMWS, 43.2; pain, 6.5 | QuickDASH, 6.7; MMWS, 73; pain, 1.1 | |
| Distal oblique LCWO | ||||||
| Okubo et al,26 2017 | 6 | 2.7 y | 15° wedge | Grip strength, 35%; RoM, 93° | Grip strength, 87%; RoM, 128° | |
CWO, closing wedge osteotomy; DASH, Disabilities of the Arm, Shoulder, and Hand; DLCWO, dorsolateral closing wedge osteotomy; LCWO, lateral closing wedge osteotomy; MMWS, Modified Mayo Wrist Score; pain; RoM, wrist flexion extension arc of motion; TRO, transverse radial osteotomy.
Follow up term in years, grip strength reported as a percentage of the contralateral side, pain is reported as visual analog scale score on a scale of 0–10.
Results
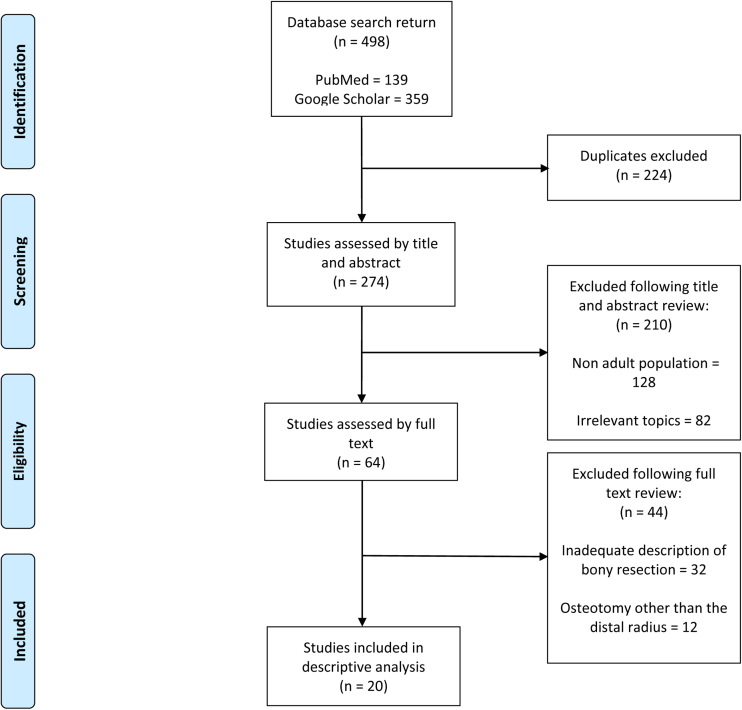
The database search returned 20 studies that met the inclusion criteria. The Figure depicts the search criteria and return.
Figure.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart for study selection, including the exclusion parameters.
Group A, RS
Radial shortening was performed in 12 studies with varying dimensions for bony resection (Table 4). Two studies reported a mean of 2 mm of RS, with ranges of 1–5 mm and 1.5–2.5 mm.7,8 One study reported a mean of 3 mm, with a range of 1–4 mm.9 Four studies reported an RS of 2–3 mm.10, 11, 12, 13 One study reported 2 mm of shortening, two studies reported an RS of up to 2 mm and 3 mm, and one study reported 2–5 mm of shortening.14, 15, 16, 17 One study performed RS to achieve neutral to (−1) ulnar variance.18
Table 4.
Osteotomy Details and Clinical Outcomes for Kienböck’s Disease Cases Treated With RS Osteotomy
| Study | Osteotomy Dimensions | Osteotomy Goal | Clinical Outcome Metrics∗ |
|
|---|---|---|---|---|
| Preoperative | Postoperative | |||
| van Leeuwen et al,7 2021 | Mean, 2 mm (range, 1–5 mm) | NR† | Pain 1, QuickDASH 2.3 (median) | |
| Botelheiro et al,10 2019 | 2–3 mm | Grip strength, 26% | Grip strength, 75% | |
| Ebrahimzadeh et al,14 2015 | 2 mm | DASH, 38; MMWS. 29; grip strength, 62% | DASH, 13; MMWS, 77; grip strength, 81% | |
| Dehghani et al,16 2014 | up to 3 mm | MMWS, 27 | MMWS, 75 | |
| Matsui et al,8 2014 | Mean, 2 mm (range, 1.5–2.5 mm) | Grip strength, 62% | DASH, 5; MMWS, 92; grip strength, 90% | |
| Kayaokay et al,11 2021 | 2–3 mm | VAS, 8.6; DASH, 47; MMWS, 20 | VAS, 2.1; DASH, 15; MMWS, 73 | |
| Mozaffarian et al,12 2012 | 2–3 mm | NR† | MMWS, 71 | |
| Luegmair et al,9 2017 | Mean, 3 mm (range, 1–4 mm) | Grip strength, 51% | DASH, 12; MMWS, 83; grip strength, 82% | |
| Tatebe et al,17 2016 | 2–5 mm | neutral to (−1) UV | NR† | NR† |
| Unal et al,13 2021 | 3 mm | QuickDASH, 63; MMWS, 65 | NR† | |
| Afshar et al,15 2015 | up to 2 mm | neutral UV | DASH, 68.7 | DASH, 24; grip strength, 70% |
| Shiota et al,18 2022 | neutral to (−1) UV | MMWS, 51 | MMWS, 83 | |
DASH, Disabilities of the Arm, Shoulder, and Hand score; MMWS, Modified Mayo Wrist Score; NR, not reported; NRS, numeric rating scale; UV, ulnar variance; VAS, visual analog scale.
Grip strength is reported as a percentage of the contralateral side.
Clinical outcomes were reported in a way that did not allow delineation based on osteotomy technique.
Group B, LCWO
Lateral closing wedge osteotomy was performed in five studies (Table 5). In one study, LCWO was performed using a wedge that tapered from 5 mm radially to 2 mm ulnarly.19 In four studies (20%), LCWO was performed with the goal being 5° to 10° of radial inclination, 10° to 15° of radial inclination, and 15° of radial inclination.13,17,20,21
Table 5.
Osteotomy Details and Clinical Outcomes for Kienböck’s Disease Cases Treated With LCWO and combined RS With LCWO
| Study | Osteotomy Dimensions | Osteotomy Goal | Clinical Outcome Metrics∗ |
|
|---|---|---|---|---|
| Preoperative | Postoperative | |||
| LCWO | ||||
| Unal et al,13 2021 | 5° to 10° radial inclination | QuickDASH, 63; MMWS, 64 | NR† | |
| Shin et al,20 2017 | 5° to 10° radial inclination | NR† | NR† | |
| Tatebe et al,17 2016 | 10° to 15° radial inclination | NR† | NR† | |
| Yamamoto I et al,21 2021 | 15° radial inclination | Pain, 5.4; grip strength, 57% | Pain, 1; grip strength, 96% | |
| Yamamoto II et al,21 2021 | 15° radial inclination | Pain, 6.2; grip strength, 59% | Pain, 2.7; grip strength, 85% | |
| Lee et al,19 2021 | 5 mm radially to 2 mm ulnarly | decrease of 5° to 10° radial inclination | QuickDASH, 44; grip strength, 16 kg | QuickDASH, 6; grip strength, 31 kg |
| LCWO + RS | ||||
| Hong et al,22 2019 | 2 mm | 10° to 15° radial inclination | DASH, 56; MMWS, 37 | DASH, 4; MMWS, 78 |
| Shin et al,20 2017 | less than 3 mm | 5° to 10° radial inclination | NR† | NR† |
DASH, Disabilities of the Arm, Shoulder, and Hand score; MMWS, modified Mayo wrist score; NR, not reported; NRS, numeric rating scale.
Grip strength is reported as a percentage of the contralateral side.
Clinical outcomes were reported in a way that did not allow delineation based on osteotomy technique.
The combination of RS and LCWO were performed in two studies, both of which specified this osteotomy protocol for patients with negative ulnar variance. One study had a goal of 10° to 15° of radial inclination with 2 mm of shortening, and the other study had a goal of 5° to 10°of radial inclination with <3 mm of RS.20,22
Group C, novel osteotomy descriptions
Novel descriptions of radial osteotomy include an oblique medial closing wedge osteotomy, a transverse osteotomy of the radius without shortening, a dorsolateral closing wedge for biplanar correction, and an oblique lateral closing wedge.23, 24, 25, 26 Camus et al23 used a medial “side to center wedge cut” intended to yield a lunate fossa slope of >12°. Blanco et al24 performed a single radial osteotomy with bone loss, equating only to the kerf of the saw blade or thin osteotome. Barrera-Ochoa et al25 used a dorsolateral closing wedge to achieve a radial inclination of <15° and a volar tilt of <5°. Okubo et al26 described an obliquely oriented 15° LCWO with the apex of the wedge at the ulnar corner of the distal radius.
Discussion
Kienböck’s disease is a disorder that we still do not fully understand. There are various theories for its etiology, with agreement on tits multifactorial nature. Kienböck’s disease is the pathologic result of intrinsic and extrinsic factors that lead to lunate necrosis. The morphology and compositional structure of the lunate are contributory intrinsic factors. Extrinsic factors include mechanics of the capitolunate joint, load distribution across the wrist, the mechanobiology of the surrounding structures, and the radioulnar relationship. Mechanical theories are not sufficient to describe the etiopathology of Kienböck’s disease. There is a multifactorial etiology that predisposes the lunate to pathology in the presence of mechanical overload.
Extra-articular radial osteotomy is a common surgical treatment in late-stage Kienböck’s disease. The intent is decompression of the lunate. Treatment techniques include RS osteotomy, closing wedge osteotomy, and variations of these. There is enduring controversy for the primary mechanism of value in radial osteotomy. A mechanical value and a biologic value have been widely discussed. Mechanical alterations have demonstrated a reduction in load onto the lunate.5 The biologic value of radial osteotomy may be the induction of biochemical factors which initiate the healing cascade. Furthermore, stress-induced adaptations in lunate architecture after radial osteotomy may provide value without accompanying shortening.24 Our findings support the premise of mechanical and biological efficacy for radial osteotomy, with satisfactory results being reported across a wide spectrum of osteotomy techniques.
The current results demonstrate the commonality of RS for the treatment of Kienböck’s disease. Fourteen (70%) of the 20 studies described RS either in isolation or in conjunction with LCWO. Some studies specified a uniform bony resection, whereas others based the resection on achievement of near-neutral ulnar variance. The purported value of RS is to unload the lunate without altering the slope of the articular surface. A radial osteotomy without shortening has been recently described.24 The proposed value of this technique is to induce a biological response without the potential for altered distal radioulnar joint and ulnocarpal mechanics that may arise after RS.27
Eight (40%) of the 20 studies described a LCWO, and 3 (15%) of the 20 studies described a unique wedge osteotomy. For most studies, the wedge dimensions were intended to result in a radial inclination of 5° to 15°. The purported value of LCWO is to provide a more equitable distribution of loading onto the radius between the scaphoid and lunate fossae. The change in slope of the articular surface of the radius is intended to off-load the lunate while maintaining radius length. Okubo et al26 performed an obliquely oriented LCWO with the apex of the wedge ending at the ulnar corner of the distal radius, The proposed value of this technique is to maintain the native longitudinal radioulnar relationship owing to the wedge osteotomy being distal to the distal radioulnar joint.
Camus et al23 described an obliquely oriented medial closing wedge osteotomy-the “Camembert osteotomy”- intended to change the slope of the lunate fossa while maintaining the native position of the scaphoid fossa. The osteotomy extends along a proximal to distal trajectory toward the articular surface, ending subchondrally. Barrera-Ochoa et al25 described a biplanar wedge osteotomy that uses a dorsolateral wedge osteotomy to reduce radial inclination and volar tilt. The reduction in volar tilt is intended to increase the radiolunate space and reduce pressure on the posterior horn of the lunate.28
The majority of the included literature describes patients with late-stage Kienböck’s disease experiencing pain and resultant dysfunction. Therefore, appropriate clinical outcome metrics are those that evaluate patient-reported pain and function. Studies reported favorable scores for DASH and MMWS which indicate pain reduction and satisfactory function. In aggregate, the novel literature displays satisfactory outcomes and restoration of function after radial osteotomy used for treatment for late-stage Kienböck’s disease.
We acknowledge several limitations. Heterogeneity of reporting prevented an aggregated analysis to compare clinical outcomes across osteotomy techniques. Our inclusion criteria required description of the osteotomy dimensions or radiographic parameters that determined the osteotomy dimensions. Although this narrowed the available sample of literature, it allowed us to report the specific details of the radial osteotomy technique. Furthermore, this demonstrated that the specific details of the radius osteotomy are often not provided in the literature. The literature search was restricted to recent studies to provide the most current display of techniques. A wider temporal period may provide additional data within the stated inclusion criteria.
The literature demonstrates the wide spectrum of distal radius osteotomy techniques for the treatment of Kienböck’s disease. The literature predominantly describes an osteotomy to shorten the radius by 2–3 mm. In some studies, the degree of RS corresponded to the necessary value to achieve near-neutral ulnar variance. The common goal in using LCWO was to achieve a radial inclination of 5° to 15°. Unique wedge resections, some with multiplanar correction of the distal radius, have been recently described. As our understanding of Kienböck’s disease continues to improve, there is reasonable expectation for the introduction of new radial osteotomy techniques and further study should delineate the techniques that may provide superior results.
Acknowledgements
The authors thank Cud Alaine Heifner for her contribution to the process.
Footnotes
Declaration of interests: D.M.M. is a member of the speaker’s bureaus for Skeletal Dynamics and Axogen. No benefits in any form have been received or will be received by the other authors related directly to this article.
References
- 1.Danoff J.R., Cuellar D.O., O J., Strauch R.J. The management of Kienböck disease: a survey of the ASSH membership. J Wrist Surg. 2015;4(1):43–48. doi: 10.1055/s-0035-1544225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stahl S., Santos Stahl A., Rahmanian-Schwarz A., et al. An international opinion research survey of the etiology, diagnosis, therapy and outcome of Kienböck’s disease (KD) Chir Main. 2012;31(3):128–137. doi: 10.1016/j.main.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Makabe H., Iwasaki N., Kamishima T., Oizumi N., Tadano S., Minami A. Computed tomography osteoabsorptiometry alterations in stress distribution patterns through the wrist after radial shortening osteotomy for Kienböck disease. J Hand Surg Am. 2011;36(7):1158–1164. doi: 10.1016/j.jhsa.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Shin Y.H., Kim J.K., Han M., Lee T.K., Yoon J.O. Comparison of long-term outcomes of radial osteotomy and nonoperative treatment for Kienbock disease: a systematic review. J Bone Joint Surg Am. 2018;100(14):1231–1240. doi: 10.2106/JBJS.17.00764. [DOI] [PubMed] [Google Scholar]
- 5.Camus E.J., Aimar A., Van Overstraeten L., Schuind F., Innocenti B. Lunate loads following different osteotomies used to treat Kienbock’s disease: a 3D finite element analysis. Clin Biomech (Bristol, Avon) 2020;78 doi: 10.1016/j.clinbiomech.2020.105090. [DOI] [PubMed] [Google Scholar]
- 6.Wang P.Q., Matache B.A., Grewal R., Suh N. Treatment of stages IIIA and IIIB in Kienbock’s disease: a systematic review. J Wrist Surg. 2020;9(6):535–548. doi: 10.1055/s-0040-1716353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Leeuwen W.F., Pong T.M., Gottlieb R.W., Deml C., Chen N., van der Heijden B.E.P.A. Radial shortening osteotomy for symptomatic Kienböck’s disease: complications and long-term patient-reported outcome. J Wrist Surg. 2021;10(1):17–22. doi: 10.1055/s-0040-1714750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsui Y., Funakoshi T., Motomiya M., Urita A., Minami M., Iwasaki N. Radial shortening osteotomy for Kienböck disease: minimum 10-year follow-up. J Hand Surg Am. 2014;39(4):679–685. doi: 10.1016/j.jhsa.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Luegmair M., Goehtz F., Kalb K., Cip J., van Schoonhoven J. Radial shortening osteotomy for treatment of Lichtman stage IIIA Kienböck disease. J Hand Surg Eur Vol. 2017;42(3):253–259. doi: 10.1177/1753193416676723. [DOI] [PubMed] [Google Scholar]
- 10.Botelheiro J.C., Silverio S., Neto A.L. Treatment of advanced Kienbock’s disease (Lichtman stage IIIB with carpal collapse) by a shortening osteotomy of the radius: 21 cases. J Wrist Surg. 2019;8(4):264–267. doi: 10.1055/s-0039-1688947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kayaokay K., Ozcan C., Bulut T., Gursoy M., Mete B.D. Radial shortening osteotomy vs partial capitate shortening osteotomy in Kienböck’s disease: medium-term radiological and clinical results. Hand Surg Rehabil. 2021;40(4):427–432. doi: 10.1016/j.hansur.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Mozaffarian K., Namazi H., Namdari A. Radial shortening osteotomy in advanced stages of Kienbock disease. Tech Hand Up Extrem Surg. 2012;16(4):242–246. doi: 10.1097/BTH.0b013e31826d2f77. [DOI] [PubMed] [Google Scholar]
- 13.Unal K.O., Bingol O., Korucu A., Kilic E., Ozdemir G., Akinci M. Medium-term clinical and radiological results of surgically treated stage 3A Kienböck’s disease. Hand Surg Rehabil. 2021;40(6):737–743. doi: 10.1016/j.hansur.2021.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Ebrahimzadeh M.H., Moradi A., Vahedi E., Kachooei A.R. Mid-term clinical outcome of radial shortening for Kienbock disease. J Res Med Sci. 2015;20(2):146–149. [PMC free article] [PubMed] [Google Scholar]
- 15.Afshar A., Mehdizadeh M., Khalkhali H. Short-term clinical outcomes of radial shortening osteotomy and capitates shortening osteotomy in Kienböck disease. Arch Bone Jt Surg. 2015;3(3):173–178. [PMC free article] [PubMed] [Google Scholar]
- 16.Dehghani M., Moshgelani M.A., Nouraei M.H., Dehghani S., Gholshahi M. Clinical outcomes of radial shortening osteotomy and vascularized bone graft in Kienböck’s disease. Int Sch Res Notices. 2014;2014 doi: 10.1155/2014/956369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tatebe M., Koh S., Hirata H. Long-term outcomes of radial osteotomy for the treatment of Kienböck disease. J Wrist Surg. 2016;5(2):92–97. doi: 10.1055/s-0036-1581099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shiota J., Momma D., Matsui Y., Inoue N., Kondo E., Iwasaki N. Changes in wrist joint contact area following radial shortening osteotomy for Kienbock’s disease. Sci Rep. 2022;12(1):4001. doi: 10.1038/s41598-022-08027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee J.H., Kim J., Hwang J.S., Baek G.H. Improvement in lunate perfusion after radial closing-wedge osteotomy in patients with Kienböck’s disease. Hand Surg Rehabil. 2021;40(5):588–594. doi: 10.1016/j.hansur.2021.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Shin Y.H., Kim J., Gong H.S., Rhee S.H., Cho M.J., Baek G.H. Clinical outcome of lateral wedge osteotomy of the radius in advanced stages of Kienböck’s disease. Clin Orthop Surg. 2017;9(3):355–362. doi: 10.4055/cios.2017.9.3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto M., Tatebe M., Nakagawa Y., Kurimoto S., Iwatsuki K., Hirata H. Radial osteotomy for Kienböck disease: clinical and radiological comparison between younger and older patients. J Hand Surg Asian Pac Vol. 2021;26(3):410–416. doi: 10.1142/S2424835521500405. [DOI] [PubMed] [Google Scholar]
- 22.Hong I.T., Lee S., Jang G.C., Kim G., Han S.H. Kienböck’s disease with non-negative ulnar variance: treatment with combined radial wedge and shortening osteotomy. Orthopade. 2019;48(1):96–101. doi: 10.1007/s00132-018-3641-5. [DOI] [PubMed] [Google Scholar]
- 23.Camus E.J., Van Overstraeten L. Surgical technique of a radial wedge “camembert” osteotomy in Kienböck disease. Tech Hand Up Extrem Surg. 2012;16(2):75–79. doi: 10.1097/BTH.0b013e3182492e9e. [DOI] [PubMed] [Google Scholar]
- 24.Blanco R.H., Blanco F.R. Osteotomy of the radius without shortening for Kienbock disease: a 10-year follow-up. J Hand Surg Am. 2012;37(11):2221–2225. doi: 10.1016/j.jhsa.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 25.Barrera-Ochoa S., Campillo-Recio D., Muñoz-Perdomo T., Esteban-Feliu I., Mendez-Sanchez G., Mir-Bullo X. Dorsolateral biplane closing radial osteotomy and lunate fixation for stage IIIC Kienböck disease: a new surgical approach. Tech Hand Up Extrem Surg. 2018;22(3):74–80. doi: 10.1097/BTH.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 26.Okubo H., Futenma C., Sunagawa H., Kinjo M., Kanaya F. Very distal radius wedge osteotomy for Kienbock’s disease: case series. J Hand Surg Asian Pac Vol. 2017;22(4):490–496. doi: 10.1142/S0218810417500551. [DOI] [PubMed] [Google Scholar]
- 27.Camus E.J., Van Overstraeten L., Schuind F. Lunate biomechanics: application to Kienbock’s disease and its treatment. Hand Surg Rehabil. 2021;40(2):117–125. doi: 10.1016/j.hansur.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 28.Lamas C., Mir X., Llusà M., Navarro A. Dorsolateral biplane closing radial osteotomy in zero variant cases of Kienböck’s disease. J Hand Surg Am. 2000;25(4):700–709. doi: 10.1053/jhsu.2000.6929. [DOI] [PubMed] [Google Scholar]