Abstract
Species of the genus Kalanchoe have a long history of therapeutic use in ethnomedicine linked to their remarkable healing properties. Several species have chemical and anatomical similarities, often leading to confusion when they are used in folk medicine. This review aims to provide an overview and discussion of the reported traditional uses, botanical aspects, chemical constituents, and pharmacological potential of the Kalanchoe species. Published scientific materials were collected from the PubMed and SciFinder databases without restriction regarding the year of publication through April 2023. Ethnopharmacological knowledge suggests that these species have been used to treat infections, inflammation, injuries, and other disorders. Typically, all parts of the plant are used for medicinal purposes either as crude extract or juice. Botanical evaluation can clarify species differentiation and can enable correct identification and validation of the scientific data. Flavonoids are the most common classes of secondary metabolites identified from Kalanchoe species and can be correlated with some biological studies (antioxidant, anti-inflammatory, and antimicrobial potential). This review summarizes several topics related to the Kalanchoe genus, supporting future studies regarding other unexplored research areas. The need to conduct further studies to confirm the popular uses and biological activities of bioactive compounds is also highlighted.
Keywords: traditional use, chemical composition, botanical description, pharmacological activities, natural products, bioactive compounds, Kalanchoe, Crassulaceae
1. Introduction
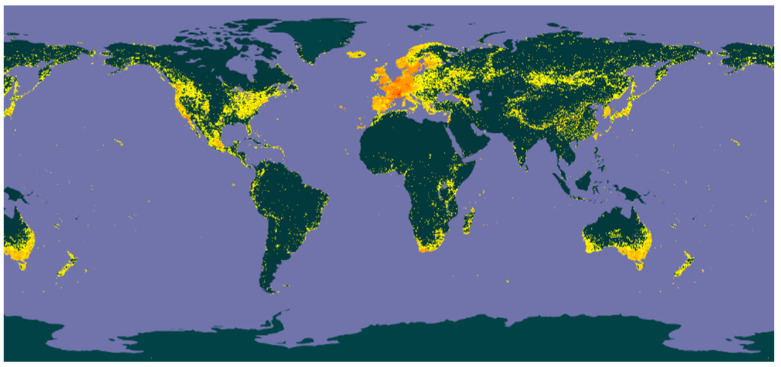
The Crassulaceae J. St.-Hil. family is composed of 36 genera [1]. Species of this family are distributed in Africa and Asia, predominantly in Madagascar and Arabia [2,3] but are also found in the Americas and in Australia (Figure 1) [4].
Figure 1.
Distribution of the species of the family Crassulaceae (yellow spots).
The genus Kalanchoe Adans (Heterotypic Synonyms: Baumgartenia Tratt., Bryophyllum Salisb., Crassuvia Comm. ex Lam., Geaya Costantin and Poiss., Kitchingia Baker, Meristostylus Klotzsch, Physocalycium Vest, and Vereia Andrews) belongs to the Crassulaceae family and comprises 179 accepted species [5]. The synonyms (according to Plants of the World Online, facilitated by the Royal Botanic Gardens) and number of occurrences worldwide (according to Global Biodiversity Information Facility) of the accepted species are shown in Table 1.
Table 1.
Kalanchoe species, synonyms, and number of occurrences.
| Scientific Name | Synonym | Occurrences |
|---|---|---|
| Kalanchoe adelae Raym.-Hamet | Bryophyllum adelae (Raym.-Hamet) A.Berger, Kalanchoe floribunda Tul. | 2 |
| Kalanchoe aliciae Raym.-Hamet | Bryophyllum aliciae (Raym.-Hamet) A.Berger, Kalanchoe miniata var. tsinjoarivensis H.Perrier, Kalanchoe pubescens var. brevicalyx Boiteau and Mannoni, Kalanchoe pubescens var. grandiflora Boiteau and Mannoni | 4 |
| Kalanchoe alternans (Vahl) Pers. | Cotyledon alternans Vahl, Vereia alternans (Vahl) Spreng. | 56 |
| Kalanchoe alticola Compton | - | 5 |
| Kalanchoe ambolensis Humbert | - | 10 |
| Kalanchoe angolensis N.E.Br. | - | 1 |
| Kalanchoe antennifera Desc. | - | 2 |
| Kalanchoe arborescens Humbert | - | 43 |
| Kalanchoe aromatica H.Perrier | - | 27 |
| Kalanchoe aubrevillei Raym.-Hamet ex Cufod. | - | 12 |
| Kalanchoe × auriculata (Raadts) V.V.Byalt | Kalanchoe nyikae subsp. auriculata Raadts | 47 |
| Kalanchoe ballyi Raym.-Hamet ex Cufod. | - | 27 |
| Kalanchoe beauverdii Raym.-Hamet | Bryophyllum beauverdii (Raym.-Hamet) A.Berger, Kalanchoe beauverdii var. typica Boiteau and Mannoni | 152 |
| Kalanchoe beharensis Drake | Kalanchoe vantieghemii Raym.-Hamet | 386 |
| Kalanchoe benbothae Gideon F.Sm. and N.R.Crouch | - | 6 |
| Kalanchoe bentii C.H.Wright ex Hook f. | - | 37 |
| Kalanchoe berevoensis Rebmann | - | - |
| Kalanchoe bergeri Raym.-Hamet and H.Perrier | Bryophyllum bergeri (Raym.-Hamet and H.Perrier) Govaerts, Kalanchoe bergeri var. typica Boiteau and Mannoni, Kalanchoe bergeri var. glabra Boiteau and Mannoni | 27 |
| Kalanchoe bhidei T.Cooke | - | 16 |
| Kalanchoe bipartita Chiov. | - | 14 |
| Kalanchoe blossfeldiana Poelln. | Kalanchoe coccinea (H.Perrier) Boiteau, Kalanchoe coccinea var. blossfeldiana (Poelln.) Boiteau, Kalanchoe globulifera var. coccinea H.Perrier | 493 |
| Kalanchoe bogneri Rauh | Bryophyllum bogneri (Rauh) V.V.Byalt | 10 |
| Kalanchoe boisii Raym.-Hamet and H.Perrier | - | 2 |
| Kalanchoe boranae Raadts | - | 10 |
| Kalanchoe bouvetii Raym.-Hamet and H.Perrier | Bryophyllum bouvetii (Raym.-Hamet and H.Perrier) A.Berger | 16 |
| Kalanchoe bouvetii Raym.-Hamet and H.Perrier | Kalanchoe baumii Engl. and Gilg, Kalanchoe multiflora Schinz, Kalanchoe pruinosa Dinter, Kalanchoe pyramidalis Schönland | 16 |
| Kalanchoe bracteata Scott Elliot | Kalanchoe bracteata var. aurantiaca Rauh and Hebding, Kalanchoe bracteata var. glabra Rauh and Hebding, Kalanchoe bracteata subsp. glabra Rauh and Hebding, Kalanchoe bracteata var. longisepala Boiteau ex L.Allorge, Kalanchoe bracteata var. pubescens Rauh and Hebding, Kalanchoe bracteata var. virescens Desc., Kalanchoe nadyae Raym.-Hamet | 88 |
| Kalanchoe brevicalyx (Raym.-Hamet and H.Perrier) Gideon F.Sm. and Figueiredo | Kalanchoe pinnata var. brevicalyx Raym.-Hamet and H.Perrier | 1 |
| Kalanchoe briquetii Raym.-Hamet | - | 2 |
| Kalanchoe campanulata (Baker) Baill. | Bryophyllum campanulatum (Baker) V.V.Byalt, Udalova and I.M.Vassiljeva, Kitchingia campanulata Baker, Kalanchoe amplexicaulis (Baker) Baill., Kalanchoe campanulata subsp. orthostyla Boiteau and Mannoni, Kalanchoe panduriformis (Baker) Baill., Kalanchoe parviflora (Baker) Baill., Kitchingia amplexicaulis Baker, Kitchingia panduriformis Baker, Kitchingia parviflora Baker | 80 |
| Kalanchoe ceratophylla Haw. | 111 | |
| Kalanchoe chapototii Raym.-Hamet and H.Perrier | 2 | |
| Kalanchoe cherukondensis Subba Rao and Kumari | Vereia ceratophylla (Haw.) D.Dietr. | - |
| Kalanchoe chevalieri Gagnep. | Kalanchoe integra var. chevalieri (Gagnep.) H.H.Pham | 9 |
| Kalanchoe citrina Schweinf. | Kalanchoe citrina var. ballyi Raym.-Hamet ex Wickens, Kalanchoe citrina var. erythreae Schweinf. | 102 |
| Kalanchoe costantinii Raym.-Hamet | Bryophyllum costantinii (Raym.-Hamet) A.Berger | 1 |
| Kalanchoe craibii Raym.-Hamet | - | 1 |
| Kalanchoe crenata (Andrews) Haw. | Cotyledon crenata (Andrews) Vent., Cotyledon verea Jacq., Kalanchoe afzeliana Britten, Kalanchoe crenata var. verea Cufod., Kalanchoe integra var. crenata (Andrews) Cufod., Kalanchoe integra var. varea Cufod., Kalanchoe verea Pers., Vereia crenata Andrews | 1320 |
| Kalanchoe crouchii Gideon F.Sm. and Figueiredo | - | 3 |
| Kalanchoe crundallii I.Verd. | - | 6 |
| Kalanchoe curvula Desc. | Bryophyllum curvulum (Desc.) V.V.Byalt | 16 |
| Kalanchoe cymbifolia Desc. | Bryophyllum cymbifolium (Desc.) V.V.Byalt | - |
| Kalanchoe daigremontiana Raym.-Hamet and H.Perrier | Bryophyllum daigremontianum (Raym.-Hamet and H.Perrier) A.Berger | 768 |
| Kalanchoe darainensis D.-P.Klein and Callm. | - | 22 |
| Kalanchoe decumbens Compton | - | - |
| Kalanchoe deficiens (Forssk.) Asch. and Schweinf. | Cotyledon deficiens Forssk., Kalanchoe glaucescens var. deficiens (Asch. and Schweinf.) Senni | 342 |
| Kalanchoe delagoensis Eckl. and Zeyh. | Bryophyllum delagoense (Eckl. and Zeyh.) Druce, Bryophyllum tubiflorum Harv., Kalanchoe tubiflora (Harv.) Raym.-Hamet, Bryophyllum verticillatum (Scott Elliot) A.Berger, Geaya purpurea Costantin and Poiss., Kalanchoe verticillata Scott Elliot | 5341 |
| Kalanchoe densiflora Rolfe | - | 687 |
| Kalanchoe × descoingsii Shtein, Gideon F.Sm. and J.Ikeda | - | - |
| Kalanchoe dinklagei Rauh | Kalanchoe brevisepala (Humbert) L.Allorge, Kalanchoe millotii var. brevisepala Humbert | 14 |
| Kalanchoe dyeri N.E.Br. | - | 21 |
| Kalanchoe elizae A.Berger | Cotyledon elizae (A.Berger) Raym.-Hamet, Cotyledon insignis N.E.Br., Kalanchoe insignis (N.E.Br.) N.E.Br., Kalanchoe laurensii Raym.-Hamet | 80 |
| Kalanchoe eriophylla Hils. and Bojer ex Tul. | Cotyledon pannosa Baker | 43 |
| Kalanchoe × estrelae Gideon F.Sm. | - | - |
| Kalanchoe fadeniorum Raadts | - | 8 |
| Kalanchoe farinacea Balf.f. | - | 55 |
| Kalanchoe faustii Font Quer | Kalanchoe laciniata subsp. faustii (Font Quer) Maire | 33 |
| Kalanchoe fedtschenkoi Raym.-Hamet and H.Perrier | Bryophyllum fedtschenkoi (Raym.-Hamet and H.Perrier) Lauz.-March., Kalanchoe fedtschenkoi var. isalensis Boiteau and Mannoni | 514 |
| Kalanchoe fernandesii Raym.-Hamet | - | 4 |
| Kalanchoe × flaurantia Desc. | - | - |
| Kalanchoe gastonis-bonnieri Raym.-Hamet and H.Perrier | Bryophyllum gastonis-bonnieri (Raym.-Hamet and H.Perrier) Lauz.-March., Kalanchoe adolphi-engleri Raym.-Hamet, Kalanchoe gastonis-bonnieri var. ankaizinensis Boiteau ex L.Allorge | 173 |
| Kalanchoe germanae Raym.-Hamet ex Raadts | - | 16 |
| Kalanchoe gideonsmithii N.R.Crouch and Figueiredo | - | 1 |
| Kalanchoe glaucescens Britten | Kalanchoe beniensis De Wild., Kalanchoe elliptica Raadts, Kalanchoe flammea Stapf, Kalanchoe holstii Engl., Kalanchoe magnidens N.E.Br., Kalanchoe marinellii Pamp., Kalanchoe ndorensis Schweinf. ex Engl. | 379 |
| Kalanchoe globulifera H.Perrier | - | 15 |
| Kalanchoe gracilipes (Baker) Baill. | Bryophyllum gracilipes (Baker) Eggli, Kitchingia gracilipes Baker | 89 |
| Kalanchoe grandidieri Baill. | - | 64 |
| Kalanchoe grandiflora Wight and Arn. | Vereia grandiflora (Wight and Arn.) D.Dietr. | 77 |
| Kalanchoe guignardii Raym.-Hamet and H.Perrier | Kalanchoe beauverdii var. guignardii (Raym.-Hamet and H.Perrier) Boiteau and Mannoni | 1 |
| Kalanchoe × gunniae Gideon F.Sm. and Figueiredo | - | - |
| Kalanchoe hametiorum Raym.-Hamet | - | 4 |
| Kalanchoe hauseri Werderm. | - | - |
| Kalanchoe hildebrandtii Baill. | Kalanchoe gomphophylla Baker, Kalanchoe hildebrandtii var. glabra Rauh and Hebding | 95 |
| Kalanchoe hirta Harv. | - | 13 |
| Kalanchoe × houghtonii D.B.Ward | Bryophyllum × houghtonii (D.B.Ward) P.I.Forst. | 1650 |
| Kalanchoe humifica Desc. | Bryophyllum humificum (Desc.) V.V.Byalt | 1 |
| Kalanchoe humilis Britten | - | 30 |
| Kalanchoe hypseloleuce Friis and M.G.Gilbert | - | 1 |
| Kalanchoe inaurata Desc. | Bryophyllum inauratum (Desc.) V.V.Byalt | - |
| Kalanchoe integra (Medik.) Kuntze | Cotyledon integra Medik., Bryophyllum serratum Blanco, Cotyledon acutiflora (Haw.) W.T.Aiton, Cotyledon hybrida Dum.Cours., Cotyledon spathulata (DC.) Poir., Echeveria spathulata (DC.) W.Bull ex É.Morren, Kalanchoe acutiflora (Andrews) Haw., Kalanchoe annamica Gagnep., Kalanchoe corymbosa Wall., Kalanchoe dixoniana Raym.-Hamet, Kalanchoe garambiensis Kudô, Kalanchoe hybrida Desf. ex Steud., Kalanchoe integra var. annamica (Gagnep.) H.H.Pham, Kalanchoe nudicaulis Buch.-Ham. ex C.B.Clarke, Kalanchoe schumacheri Koord., Kalanchoe spathulata DC., Kalanchoe spathulata var. annamica (Gagnep.) H.Ohba, Kalanchoe spathulata var. baguioensis H.Ohba, Kalanchoe spathulata var. ciliata, Kalanchoe spathulata var. dixoniana (Raym.-Hamet) H.Ohba, Kalanchoe spathulata var. garambiensis (Kudô) H.Ohba, Kalanchoe spathulata var. schumacheri (Koord.) H.Ohba, Kalanchoe spathulata var. simlensis H.Ohba, Kalanchoe spathulata var. staintonii H.Ohba, Kalanchoe subamplectens Wall., Kalanchoe varians Haw., Kalanchoe yunnanensis Gagnep., Vereia acutiflora Andrews, Vereia spathulata (DC.) D.Dietr. | 289 |
| Kalanchoe integrifolia Baker | Kalanchoe bitteri Raym.-Hamet and H.Perrier, Kalanchoe heckelii Raym.-Hamet and H.Perrier, Kalanchoe integrifolia var. bitteri Raym.-Hamet and H.Perrier, Kalanchoe integrifolia var. flava Boiteau | 85 |
| Kalanchoe jongmansii Raym.-Hamet and H.Perrier | Bryophyllum jongmansii (Raym.-Hamet and H.Perrier) Govaerts, Kalanchoe jongmansii subsp. ivohibensis Humbert | 54 |
| Kalanchoe klopperae Gideon F.Sm. and Figueiredo | - | - |
| Kalanchoe laciniata (L.) DC. | Cotyledon laciniata L., Vereia laciniata (L.) Willd., Kalanchoe angustifolia A.Rich., Kalanchoe biternata Wight ex Wall., Kalanchoe carnea N.E.Br., Kalanchoe gloveri Cufod., Kalanchoe lentiginosa Cufod., Kalanchoe petitiaesii Rich. ex Jacques, Kalanchoe rohlfsii Engl., Kalanchoe rosea A.Chev., Kalanchoe schweinfurthii Penz., Kalanchoe teretifolia Haw. | 430 |
| Kalanchoe laetivirens Desc. | Bryophyllum laetivirens (Desc.) V.V.Byalt | 223 |
| Kalanchoe lanceolata (Forssk.) Pers. | Cotyledon lanceolata Forssk., Vereia lanceolata (Forssk.) Spreng., Cotyledon amplexicaulis B.Heyne ex C.B.Clarke, Cotyledon corymbosa Rottler ex Wight and Arn., Cotyledon heterophylla Roxb., Cotyledon hirsuta B.Heyne ex C.B.Clarke, Cotyledon paniculata Rottler ex Wight and Arn., Kalanchoe amplexicaulis B.Heyne, Kalanchoe brachycalyx A.Rich., Kalanchoe crenata var. collina Engl., Kalanchoe ellacombei N.E.Br., Kalanchoe floribunda Wight and Arn., Kalanchoe floribunda var. glabra C.B.Clarke, Kalanchoe glandulosa Hochst. ex A.Rich., Kalanchoe glandulosa var. benguellensis Engl., Kalanchoe glandulosa var. rhodesica Baker f., Kalanchoe glandulosa var. tomentosa Keissl., Kalanchoe goetzei Engl., Kalanchoe gregaria Dinter, Kalanchoe heterophylla (Roxb.) Wight and Arn., Kalanchoe heterophylla (Roxb.) Prain, Kalanchoe homblei De Wild., Kalanchoe homblei f. reducta De Wild., Kalanchoe junodii Schinz, Kalanchoe laciniata var. brachycalyx (A.Rich.) Chiov., Kalanchoe lanceolata var. glabra (C.B.Clarke) S.R.Sriniv., Kalanchoe lanceolata var. glandulosa (Hochst. ex A.Rich.) Cufod., Kalanchoe modesta Kotschy and Peyr., Kalanchoe pentheri Schltr., Kalanchoe pilosa Baker, Kalanchoe platysepala Welw. ex Britten, Kalanchoe pubescens R.Br. ex Britten, Kalanchoe ritchieana Dalzell, Kalanchoe spathulata Wall., Kalanchoe wightianum Wall., Meristostylus macrocalyx Klotzsch, Vereia floribunda (Wight and Arn.) D.Dietr., Vereia heterophylla (Wight and Arn.) D.Dietr. | 893 |
| Kalanchoe lateritia Engl. | - | 284 |
| Kalanchoe latisepala N.E.Br. | - | 31 |
| Kalanchoe laxiflora Baker | Bryophyllum laxiflorum (Baker) Govaerts, Bryophyllum crenatum Baker, Kalanchoe crenata (Baker) Raym.-Hamet, Kalanchoe laxiflora subsp. stipitata Boiteau and Mannoni, Kalanchoe laxiflora subsp. subpeltata Boiteau and Mannoni, Kalanchoe laxiflora subsp. violacea Boiteau and Mannoni, Kalanchoe tieghemii Raym.-Hamet | 469 |
| Kalanchoe leblanciae Raym.-Hamet | - | 17 |
| Kalanchoe lindmanii Raym.-Hamet | Kalanchoe gossweileri Croizat, Kalanchoe humbertii Guillaumin, Kalanchoe pearsonii N.E.Br. | 16 |
| Kalanchoe linearifolia Drake | Kalanchoe bonnieri Raym.-Hamet | 118 |
| Kalanchoe lobata R.Fern. | - | 6 |
| Kalanchoe × lokarana Desc. | Bryophyllum × lokarana (Desc.) V.V.Byalt | 2 |
| Kalanchoe longiflora Schltr. | - | 35 |
| Kalanchoe longifolia E.T.Geddes | - | 2 |
| Kalanchoe lubangensis R.Fern. | - | 1 |
| Kalanchoe luciae Raym.-Hamet | Kalanchoe albiflora H.M.L.Forbes | 60 |
| Kalanchoe macrochlamys H.Perrier | Bryophyllum macrochlamys (H.Perrier) A.Berger | 12 |
| Kalanchoe mandrarensis Humbert | - | 7 |
| Kalanchoe manginii Raym.-Hamet and H.Perrier | Bryophyllum manginii (Raym.-Hamet and H.Perrier) Nothdurft | 67 |
| Kalanchoe marmorata Baker | Kalanchoe grandiflora A.Rich., Kalanchoe macrantha Baker ex Maire, Kalanchoe macrantha var. marmorata (Baker) Maire, Kalanchoe macrantha var. richardiana Maire | 264 |
| Kalanchoe marnieriana H.Jacobsen ex L.Allorge | Bryophyllum marnierianum (H.Jacobsen ex L.Allorge) Govaerts, Kalanchoe humbertii Mannoni and Boiteau | 46 |
| Kalanchoe maromokotrensis Desc. and Rebmann | - | 5 |
| Kalanchoe migiurtinorum Cufod. | - | 7 |
| Kalanchoe millotii Raym.-Hamet and H.Perrier | - | 82 |
| Kalanchoe miniata Hils. and Bojer ex Tul. | Bryophyllum miniatum (Hils. and Bojer ex Tul.) A.Berger, Kalanchoe miniata var. typica H.Perrier, Kitchingia miniata (Hils. and Bojer ex Tul.) Baker | 252 |
| Kalanchoe mitejea Leblanc and Raym.-Hamet | - | 29 |
| Kalanchoe montana Compton | Kalanchoe luciae subsp. montana (Compton) Toelken | 2 |
| Kalanchoe mortagei Raym.-Hamet and H.Perrier | Bryophyllum mortagei (Raym.-Hamet and H.Perrier) Wickens, Kalanchoe poincarei var. mortagei (Raym.-Hamet and H.Perrier) Boiteau | 42 |
| Kalanchoe ndotoensis L.E.Newton | - | 1 |
| Kalanchoe neglecta Toelken | Kalanchoe rotundifolia f. peltata R.Fern. | 7 |
| Kalanchoe nyikae Engl. | Kalanchoe hemsleyana Cufod. | 53 |
| Kalanchoe obtusa Engl. | - | 39 |
| Kalanchoe olivacea Dalzell | - | 10 |
| Kalanchoe orgyalis Baker | Kalanchoe antanosiana Drake | 162 |
| Kalanchoe paniculata Harv. | Sedum harveyanum Kuntze, Kalanchoe oblongifolia Harv. | 193 |
| Kalanchoe pareikiana Desc. and Lavranos | - | 2 |
| Kalanchoe peltata (Baker) Baill. | Bryophyllum peltatum (Baker) V.V.Byalt, Udalova and I.M.Vassiljeva, Kitchingia peltata Baker | 152 |
| Kalanchoe peltigera Desc. | Bryophyllum peltigerum (Desc.) V.V.Byalt | 5 |
| Kalanchoe perrieri Shtein, Gideon F.Sm. and D.-P.Klein | - | - |
| Kalanchoe peteri Werderm. | - | 35 |
| Kalanchoe petitiana A.Rich. | - | 95 |
| Kalanchoe pinnata (Lam.) Pers. | Bryophyllum pinnatum (Lam.) Oken, Cotyledon pinnata Lam., Crassula pinnata (Lam.) L.f., Kalanchoe pinnata var. genuina Raym.-Hamet, Vereia pinnata (Lam.) Spreng., Baumgartenia sobolifera Tratt., Bryophyllum calcicola (H.Perrier) V.V.Byalt, Bryophyllum calycinum Salisb., Bryophyllum germinans Blanco, Bryophyllum pinnatum simplicifolium Kuntze, Cotyledon calycina (Salisb.) B.Heyne, Cotyledon calyculata Sol. ex Sims, Cotyledon rhizophylla Roxb., Crassuvia floripendia Comm. ex Lam., Kalanchoe calcicola (H.Perrier) Boiteau, Kalanchoe floripendula Steud, Kalanchoe pinnata var. calcicola H.Perrier, Kalanchoe pinnata var. floripendula Pers. | 7288 |
| Kalanchoe × poincarei Raym.-Hamet and H.Perrier | Bryophyllum poincarei (Raym.-Hamet and H.Perrier) Govaerts | 10 |
| Kalanchoe porphyrocalyx (Baker) Baill. | Bryophyllum porphyrocalyx (Baker) A.Berger, Kalanchoe porphyrocalyx var. typica Boiteau and Mannoni, Kitchingia porphyrocalyx Baker | 187 |
| Kalanchoe prasina N.E.Br. | Kalanchoe figuereidoi Croizat | - |
| Kalanchoe prittwitzii Engl. | Kalanchoe dielsii Raym.-Hamet, Kalanchoe lugardii Bullock, Kalanchoe robynsiana Raym.-Hamet, Kalanchoe secunda Werderm. | 136 |
| Kalanchoe prolifera (Bowie ex Hook.) Raym.-Hamet | Bryophyllum proliferum Bowie ex Hook., Bryophyllum cochleatum Lem., Kalanchoe cochleatum (Lem.) B.D.Jacks. | 180 |
| Kalanchoe pseudocampanulata Mannoni and Boiteau | Bryophyllum pseudocampanulatum (Mannoni and Boiteau) Govaerts, Kalanchoe miniata var. decaryana H.Perrier | 5 |
| Kalanchoe pubescens Baker | Bryophyllum pubescens (Baker) Govaerts, Kalanchoe pubescens var. typica Boiteau and Mannoni | 162 |
| Kalanchoe pumila Baker | Kalanchoe brevicaulis Baker, Kalanchoe multiceps Baill., Kalanchoe pumila f. venustior Boiteau | 71 |
| Kalanchoe quadrangularis Desc. | - | 3 |
| Kalanchoe quartiniana A.Rich. | - | 23 |
| Kalanchoe rebmannii Desc. | - | 1 |
| Kalanchoe × rechingeri Raym.-Hamet ex Rauh and Hebding | Bryophyllum × rechingeri (Raym.-Hamet ex Rauh and Hebding) V.V.Byalt | 2 |
| Kalanchoe rhombopilosa Mannoni and Boiteau | Kalanchoe rhombopilosa var. argentea Rauh, Kalanchoe rhombopilosa var. viridifolia Rauh | 30 |
| Kalanchoe × richaudii Desc. | - | 2 |
| Kalanchoe robusta Balf.f. | Kalanchoe abrupta Balf.f. | 7 |
| Kalanchoe rolandi-bonapartei Raym.-Hamet and H.Perrier | Bryophyllum rolandi-bonapartei (Raym.-Hamet and H.Perrier) Govaerts, Bryophyllum tsaratananense (H.Perrier) A.Berger, Kalanchoe tsaratananensis H.Perrier | 16 |
| Kalanchoe rosea C.B.Clarke | - | - |
| Kalanchoe rosei Raym.-Hamet and H.Perrier | Bryophyllum rosei (Raym.-Hamet and H.Perrier) A.Berger, Kalanchoe bouvieri Raym.-Hamet and H.Perrier | 74 |
| Kalanchoe rotundifolia (Haw.) Haw. | Crassula rotundifolia Haw., Sedum subrotundifolium (Haw.) Kuntze, Vereia rotundifolia (Haw.) D.Dietr., Kalanchoe guillauminii Raym.-Hamet, Kalanchoe integerrima Lange, Kalanchoe luebbertiana Engl., Kalanchoe rotundifolia var. guillauminii (Raym.-Hamet) Raym.-Hamet, Kalanchoe rotundifolia f. tripartita R.Fern., Kalanchoe seilleana Raym.-Hamet, Kalanchoe stearnii Raym.-Hamet, Meristostylus brachycalyx Klotzsch | 623 |
| Kalanchoe rubella (Baker) Raym.-Hamet | Bryophyllum rubellum Baker | 23 |
| Kalanchoe salazarii Raym.-Hamet | - | 2 |
| Kalanchoe sanctula Desc. | Bryophyllum sanctulum (Desc.) V.V.Byalt | 2 |
| Kalanchoe scandens H.Perrier | Bryophyllum scandens (H.Perrier) A.Berger, Kalanchoe beauverdii var. parviflora Boiteau and Mannoni | 7 |
| Kalanchoe scapigera Welw. ex Britten | - | 15 |
| Kalanchoe schimperiana A.Rich. | Cotyledon deficiens Hochst. and Steud. ex A.Rich. | 78 |
| Kalanchoe schizophylla (Baker) Baill. | Bryophyllum schizophyllum (Baker) A.Berger, Kitchingia schizophylla Baker | 48 |
| Kalanchoe schliebenii Werderm. | - | 3 |
| Kalanchoe serrata Mannoni and Boiteau | Bryophyllum lauzac-marchaliae V.V.Byalt, Bryophyllum serratum (Mannoni and Boiteau) Lauz.-March. | 36 |
| Kalanchoe sexangularis N.E.Br. | - | 130 |
| Kalanchoe stenosiphon Britten | - | 9 |
| Kalanchoe streptantha Baker | Bryophyllum streptanthum (Baker) A.Berger | 28 |
| Kalanchoe suarezensis H.Perrier | Bryophyllum suarezense (H.Perrier) A.Berger, Kalanchoe poincarei var. suarezensis (H.Perrier) L.Allorge | 20 |
| Kalanchoe subrosulata Thulin | - | 4 |
| Kalanchoe synsepala Baker | Kalanchoe brachycalyx Baker, Kalanchoe gentyi Raym.-Hamet and H.Perrier, Kalanchoe trichantha Baker | 214 |
| Kalanchoe tachingshuii S.S.Ying | - | - |
| Kalanchoe tashiroi Yamam. | - | 4 |
| Kalanchoe teixeirae Raym.-Hamet ex R.Fern. | - | 3 |
| Kalanchoe tenuiflora Desc. | - | 3 |
| Kalanchoe tetramera E.T.Geddes | - | 2 |
| Kalanchoe tetraphylla H.Perrier | - | 30 |
| Kalanchoe thyrsiflora Harv. | Kalanchoe alternans Eckl. and Zeyh. ex Harv. | 251 |
| Kalanchoe tomentosa Baker | Bryophyllum triangulare Blanco | 179 |
| Kalanchoe torrejacqii Shtein and Gideon F.Sm. | - | 3 |
| Kalanchoe tuberosa H.Perrier | - | 11 |
| Kalanchoe uniflora (Stapf) Raym.-Hamet | Bryophyllum uniflorum (Stapf) A.Berger, Kitchingia uniflora Stapf, Bryophyllum ambrense (H.Perrier) A.Berger, Kalanchoe ambrensis H.Perrier, Kalanchoe uniflora var. brachycalyx Boiteau and Mannoni | 97 |
| Kalanchoe usambarensis Engl. and Raym.-Hamet | - | 16 |
| Kalanchoe variifolia (Guillaumin and Humbert) Shtein, D.-P.Klein and Gideon F.Sm. | Kalanchoe rosei var. variifolia (Guillaumin and Humbert) J.M.H.Shaw, Kalanchoe rosei subsp. variifolia Guillaumin and Humbert | 13 |
| Kalanchoe velutina Welw. ex Britten | - | 56 |
| Kalanchoe viguieri Raym.-Hamet and H.Perrier | Kalanchoe viguieri var. latisepala Raym.-Hamet and H.Perrier | 68 |
| Kalanchoe waldheimii Raym.-Hamet and H.Perrier | Bryophyllum waldheimii (Raym.-Hamet and H.Perrier) Lauz.-March. | 50 |
| Kalanchoe waterbergensis van Jaarsv. | - | 3 |
| Kalanchoe welwitschii Britten | - | 17 |
| Kalanchoe wildii Raym.-Hamet ex R.Fern. | Kalanchoe aleuroides Stearn | 2 |
| Kalanchoe winteri Gideon F.Sm., N.R.Crouch and Mich.Walters | - | 3 |
| Kalanchoe yemensis (Deflers) Schweinf. | Kalanchoe brachycalyx var. yemensis Deflers | 17 |
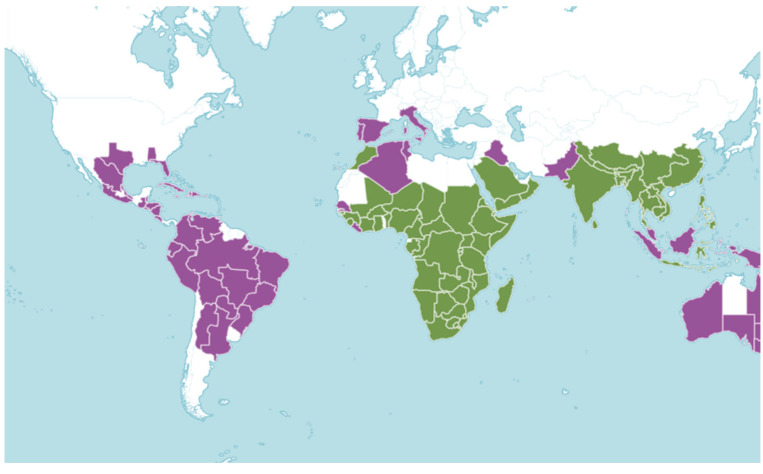
The term Kalanchoe was originally used by Michel Adanson in 1763 and it refers to the phonetic transcription of the Chinese term “Kalan Chauhuy”, which means “what falls and grows”. The name Kalanchoe describes the propagation of leaf embryos. Another explanation for the name relates it to the words “kalanka” and “chaya”, which are used by Brazilian indigenous people and, respectively, mean stain/rust and shine, alluding to the reddish roots and shiny leaves [3,6]. Figure 2 shows the distribution of the native and introduced species of the genus Kalanchoe around the world [7].
Figure 2.
Distribution of the native (green) and introduced (purple) species of the genus Kalanchoe.
Species of this genus are popularly known as “mother-of-thousands” or “mother-of-millions” due to their propagation by leaf embryos [8]. Some members of the genus Kalanchoe have a long history of therapeutic use and are known as “miracle leaf” because of their remarkable healing properties and traditional use in the treatment of several diseases and disorders [6,9,10,11,12]. Some of these biological activities have been correlated with specific classes of secondary metabolites already described in the Kalanchoe species. Examples include cardioactive glycosides and phenolic compounds (phenolic acids, flavonoids, and tannins) [13].
However, a detailed literature search revealed that only a limited number of species described as “miracle leaf” have anatomical and structural similarities and are used in folk medicine to treat a variety of health problems and disorders. Consequently, this review provides a critical overview of the main aspects published in the literature regarding the traditional uses, botanical characteristics, chemical composition, and pharmacological activity of species of the Kalanchoe genus, and aims to contribute to the knowledge of this genus, discussing important biological and chemical aspects described in these studies, and providing material for new evaluation.
2. Results and Discussion
2.1. Traditional Uses
The genus Kalanchoe is widely used in folk medicine to treat different health diseases and disorders. Thus far, only 21 of the 133 species of the genus Kalanchoe have been reported regarding their popular uses, as described in Table 2.
Table 2.
Traditional uses of Kalanchoe species.
| Species | Traditional Uses | Form of Use and Plant Part | References |
|---|---|---|---|
| K. ceratophylla | To treat injuries, pain, fever, and inflammation. | Internal or external administration of crude extracts or plant juice. | [14,15,16,17] |
| K. crenata | Antidiabetic, anti-inflammatory, antimicrobial, vermifuge, and anti-infective agent; to treat wounds, abscesses, abdominal pain, asthma, headache, convulsion, smallpox, peptic ulcer, upper respiratory tract infections, coughs, otitis, palpitations, cancer (or disease states with symptoms related to cancer), diabetes, swollen areas for muscle sprain and myalgia; and to heal umbilical cord wounds in newborns. | Internal administration of crude extracts, plant juice, leaves juice, or chew the leaves; external administration of crude extracts or plant juice and from macerating the leaves into a cream. Use of roots. | [6,14,15,16,18,19,20,21,22,23,24,25,26,27] |
| K. daigremontiana | Anticancer, anti-inflammatory, antimicrobial, antiseptic, carminative and cardioactive agent; to treat skin injuries and wounds; to staunch bleeding; to treat infections, rheumatism, earache, burns, arthritis, gastric and menstrual disorders, cough, fever, cardiovascular dysfunction, diabetes, psychic agitation, restlessness and anxiety, some cancers; a chemo preventive. | Internal or external administration of crude extracts or plant juice and use of roots. | [9,10,11,12,15,21,28,29,30] |
| K. delagoensis | To treat wounds, epilepsy, neoplastic diseases, fever, abscesses, bruises, pneumonia, coughs, stomachache, and as a vermifuge. | Internal or external administration of crude extracts or plant juice and use of roots. | [14,15,21,31,32,33,34] |
| K. densiflora | To treat wounds and skin disorders, rheumatism, hemorrhoids, eye problems, joint and muscle pains, stomach and liver problems, umbilical cord, cardiac disorders, edema, poisonous, abortifacient. | Internal or external administration of crude extracts or plant juice. | [15,24,27,35] |
| K. flammea | To treat fever, wounds, inflammation, and cancer. | [36] | |
| K. fedtschenkoi | Analgesic, cytotoxic, and antimicrobial treatments. | Internal or external administration. Use of leaves and roots. | [21,37] |
| K. gastonis-bonnieri | To treat genital-urinary and vaginal infections and as a vaginal contraceptive. | [38] | |
| K. germanae | After removal of ganglions the leaves are used to treat the affected area. | Internal or external administration of crude extracts or plant juice. | [15] |
| K. glaucescens | To treat coughs and rheumatism. | Internal or external administration of crude extracts or plant juice. | [15,24] |
| K. integra | Antihypertensive. | [39] | |
| K. laciniata | As an anti-inflammatory, astringent, and antiseptic; to treat wounds, inflammation, headache, diabetes, heart discomfort, gastric disorders, lithiasis, diarrhea, fever, cough, snakebites, erysipelas, boils, and human prostate cancer. | Internal administration of crude extracts, plant juice, leaves juice or chew the leaves; external administration of crude extracts or plant juice and from macerating the leaves into a cream. | [6,11,15,40,41,42,43,44,45,46,47,48,49] |
| K. lanceolata | To treat dysentery, rheumatism, hemorrhoids, splenomegaly, hepatomegaly, and pains. | Internal or external administration of crude extracts or plant juice. | [15,24,27,35] |
| K. marmorata | To treat wounds, boils, bruises, periodontal disease, cracked lips, arthritis, gastric ulcers, ear diseases, eye infections, dysentery, fever, common cold, coughs, cholera, urinary diseases, stiff muscles, liver problems, and headaches. | Internal or external administration of crude extracts or plant juice. | [15,24,50,51,52] |
| K. mortagei | As an antimicrobial; to treat digestive disorders, parasites, and neoplastic diseases orally; and as a local remedy for cancer. | Internal or external administration. Use of leaves and roots. | [21,37] |
| K. obtusa | Children’s diseases and as pesticide. | Use the whole plant. | [24] |
| K. petitiana | To treat epilepsy, trachoma, allergies, intestinal parasites, gonorrhea, bone setting after fractures, wound healing, breast tumors, skin cancer, swelling of gland/lymph adenitis, toothache, dysentery, liver problems, stomachache, tonsillitis, gastritis, peptic ulcer disease, and foot problems (fungal nails, corns, and calluses, athlete’s foot, plantar warts). | Internal or external administration of crude extracts or plant juice. | [15,53,54,55,56] |
| K. pinnata | Antipyretic, antibacterial, antiseptic, antimalaria, anti-inflammatory, and antipsychotic agent. To treat the following: wounds, burns; cardiovascular dysfunctions; cancer; rheumatoid arthritis; digestive, menstrual and psychiatric disorders; hypertension; skin, respiratory and genitourinary infections; kidney, liver and urinary disorders; ear, head and toothache; insect, snake and scorpion bites; muscle bruises; cholera; leishmania; leprosy; lithiasis; viruses; restlessness; biostimulator during skin transplantation; to prevent premature labor and help women recover after childbirth; diabetes; cold, whooping cough, bone fracture, Chikungunya virus, and against COVID-19 symptoms. | Internal administration of crude extracts, whole plant, or leaves juice, chew the leaves or leaves infusion; external administration of crude extracts or plant juice and from macerating the leaves into a cream. Use of roots. | [6,8,9,14,15,21,41,42,43,44,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93] |
| K. prittwitzii | Stiff joints and rheumatism. | Use of leaves. | [24] |
| K. serrata | To treat pain, inflammation, fever, and viruses. | Use of leaves and roots. | [21] |
| K. x houghtonii | To treat infections, rheumatism, coughs, fever, and inflammation. | [30] |
From these 21 species, there exists a broad ethnopharmacological knowledge of four species that are more often cited as medicinal plants (K. pinnata, K. laciniata, K. crenata, and K. daigremontiana), suggesting that they can be adopted to treat wounds, cancer, diabetes, infections, and inflammation. However, there are no reports in the scientific literature that describe the amounts of plant or dosages for ethnomedicinal uses.
All parts of the Kalanchoe species are traditionally used for medicinal purposes, but the juice or crude extract preparations (produced by maceration) are cited as the primary forms of administration [6,8,11,15,18,20,21,28,37,43,49,63,65,70,78,79,81].
In the cases of K. × houghtonii, K. flammea, K. gastonis-bonnieri, and K. integra, the literature does not describe which parts of the plant, method of preparation, or the dosage are popularly recommended for medicinal use. As is the case with many medicinal plants, folk-information related to traditional use of medicinal plants contributes to the search for scientific basis in these treatment regimens. These data, and the important lack thereof in most cases, reinforce the importance of additional investigations into the chemistry and bioactivity of this genera.
2.2. Botanical Description
Species of the Crassulaceae family are herbaceous or sub-shrubs, usually succulent, opposite, or alternate, and exstipulate. The flowers are actinomorphic, hermaphrodite, and usually cymose [5]. Species of the Kalanchoe genus are herbaceous or sub-woody; they have small branches and can reach from 1 to 1.5 m in height, especially during their flowering stage. Its leaves are opposite, succulent, oval, and have crenated margins, which are 10 to 20 cm long. Flowers can measure up to 5 cm in length, are pendant, and are arranged in inflorescences. Fruits are membranous, and the seeds are ellipsoid. The stem has thin-walled cells located deep in the epidermis. These cell walls are impregnated with resin, forming a thin layer that can reduce liquid evaporation [94,95,96].
These species adapt well and tolerate extreme conditions, such as lighting and water scarcity. One feature of this plant is a compartment in the leaves and stem tissues that can store and inhibit water loss [2,96,97]. This physical adaptation works in tandem with crassulacean acid metabolism (CAM), a metabolic adaptation to perform photosynthetic CO2 fixation and water loss reduction. During the night, and at low temperatures, the stomata open, and the plant can assimilate atmospheric CO2. However, daylight closes the stomata structure and CO2 fixation occurs [98,99,100]. The stomatas have been described in detail and can be considered anatomical markers of the family [101].
Species of the genus Kalanchoe are popularly known due to their propagation by leaf embryos, and these propagules (also called leaf bulbs or bulbils) from the margins of the leaves are responsible for their tremendous invasiveness. New plants can be produced from parts of the mother plant, especially by clonal growth through the bulbs that arise from the leaf margins. In suitable open places (such as rocky or sandy environments) these populations can quickly form dense stands. This feature is the primary reason they are popularly known as “mother-of-thousands” or “mother-of-millions” [8,12,102].
Only 16 of the 133 species of the genus Kalanchoe have had their botanical aspects formally described in the literature (Table 3). More specifically, 11 of them have a macroscopic description (K. blossfeldiana; K. marmorata; K. beharensis, K. laxiflora, K. orgyalis, K. rhombopilosa, K. synsepala, K. tetraphylla, K. tomentosa, and K. × houghtonii), and only 5 have additional botanical evaluation/microscopical analysis of the plants (K. daigremontiana, K. delagoensis, K. laciniata, K. pinnata, and K. pumila).
In the case of K. blossfeldiana, five genotypes were also distinguished by morphological characterization (assessing the flower’s anatomical aspects and plant height), and molecular profiling (random amplified polymorphism DNA (RAPD), inter-simple sequence repeats (ISSR), and start codon targeted (SCoT)-polymerase chain reaction (PCR) tools) [103].
Table 3.
Botanical aspects of Kalanchoe species.
| Species | Macro Aspects | Micro Aspects | References |
|---|---|---|---|
| K. beharensis | The largest species of the genus, with 3 m in height; unbranched stems; leaves crowded at the branch tips; lobed, covered in a dense felt; ranging from 12–35 cm in length and 7–35 cm in width. | [6] | |
| K. blossfeldiana | Dark green, succulent, and perennial plant, with scallop-edged leaves and large umbels of flower clusters held above the foliage. The fleshy, dark shiny green leaves have lobed edges and can reach 7.7 cm in length and 3.8 cm in width. Floral colors range from traditional red to yellow, orange, salmon and pink. | [104] | |
| K. daigremontiana | Perennial short-lived succulent herb; monocarpic multi-annuals. The most characteristic feature of the species is its method of asexual reproduction by auto-propagation. Flowering tends to be sporadic, in winter, and, when it occurs, the main stalk elongates vertically, developing a terminal inflorescence of small, bell-shaped, pendulous flowers with a pinkish or purple corolla. The stem is unbranched, up to 1.5 m in height. The leaves are thick, fleshy, lanceolate, tapered at the apex and serrated in the margins, dark green colored, and have purple-brown spots on the abaxial side. The apex bears hydathodes and adventitious buds, from which propagules are formed and developed. | The epidermis is single-layered, with parenchymatic cells, convex outer walls surface, wax patches in cuticles, is smooth-undulating, and striated only on subsidiary cells. The leaves are amphistomatic, with anisocytic stomata. The subepidermal mesophyll consists of one or several layers of small, closely adherent cells. The central vascular bundles are surrounded by perivascular sheaths composed of mesophyll cells. Between the epidermis and mesophyll in the petioles there are 1–3 layers of compact angular collenchyma. The vascular bundles are collateral. In the central veins in the petiole and the leaf are three large bundles. The cross-sections show fine lateral vascular bundles surrounding large bundles in the petioles and leaf blades. The different tissues of the leaf contain numerous phenolic idioblasts, accumulating phenolic compounds in their vacuoles, present in epidermal cells, in the subepidermal layer, near the vascular elements, around the large vascular bundles in the leaf petioles, and surrounding the smaller vascular bundles, dispersed in the parenchyma as single cells or form multicellular aggregates. | [6,12,29,97,105,106] |
| K. delagoensis | It has dark purplish, speckled, tubular leaves, which are filled with plantlets. It typically grows to about 1 m in height before blooming. It overwinters as a terminal inflorescence bearing orange or red pendant bell-shaped flowers and then dies. | The leaves are tubular and have 6–8 apical buds. The epidermal cells are uniseriate with sinuous anticlinal walls. The leaves are amphistomatic with anisocytic stomata. The mesophyll has regular chlorenchyma. The vascular system has collateral bundles distributed in the form of an arc. Anthocyanin idioblasts occur throughout the leaf blade, in the epidermis; hypodermis; layer beneath the hypodermis; scattered in the chlorenchyma; surrounding the vascular bundles; vascular tissues; and apical buds. | [6,107] |
| K. ceratophylla | Perennial, succulent, and glabrous species. | [16] | |
| K. laciniata | Perennial or biennial herb that grows from 30 cm to 1.5 m in height. Its leaves are oval, opposite, fleshy, simple, short-petiolate, glossy, and pale green to dark green in color. They have dentate to crenate leaf margins, with a cylindrical herbaceous stem and fleshy petiole. | The secretory structures found in the stems, petioles and leaf blades consist of idioblasts that contain anthocyanins. The epidermis of K. laciniata is a single layer with adhering and oblong cells. The outer cell wall is convex and covered with cuticles. The leaves are amphistomatic and the chlorenchyma tissue is uniform. The cells of the chlorenchyma tissue have irregular, spherical-ellipsoidal shapes. The vacuoles of some mesophyll cells located near the epidermis, vascular bundles, and hydathodes contain phenolic compounds. The leaves show the presence of adaptive traits that enable them to survive in dry environments | [42,44,108] |
| K. laxiflora | Perennial species with multicolored leaves, that are crenate, green in shady settings, and pink or purple in bright sun. The flower buds are almost transparent but when they open, they turn orange. | [6] | |
| K. marmorata | The leaves are large, oval, blue-green colored, with purple markings, arranged in stacked, opposite pairs to a height of 30 cm. The brown spots become brighter during summer dormancy and in strong sunlight; during winter they become pale or disappear altogether. | [3,6] | |
| K. orgyalis | It is a much-branched slow-growing shrub that can reach approximately 1–2 m in height. It has spoon-shaped leaves, which are bronze to gray on the underside, and felted on the top of each leaf, with cinnamon-toned fuzz. Late winter or early spring brings bright yellow flowers in terminal clusters at the branch tips. | [6] | |
| K. pinnata | An erect, succulent, perennial and glabrous plant that grows up to 1.5 m in height. The species reproduces through seeds and from leaf bulbils. The freshly dark green leaves are large (12–18 cm and 6–8 cm in size), simple, opposite, ovate, or elliptic, have serrate-crenate margins with buds, an obtuse apex, asymmetric base, reticulate venation, and long petiole. The flowers are pendulous, dark, and bell-like. The stems are tall, hollow, obtuse, and four-angled. The fruits are enclosed in the calyx and corolla. The seeds are small, smooth, oblong-ellipsoid, rarely striate, and smooth. | The leaves are broadly shallow on the adaxial side and convex on the abaxial side. The epidermal layer is thin, with small prominent cells on the adaxial side and less distinct on the abaxial side. The ground tissue of the midrib is parenchymatous and homogenous. The cells are circular or angular and compact. The vascular strand is single, collateral, small, and hemispherical; it consists of a thick horizontal band of xylem and a wide band of phloem. The lamina is uniformly flat with an even surface. The mesophyll tissue is not differentiated into palisade and spongy parenchyma. The stomata are anisocytic. The leaf petiole shows prismatic crystals of calcium oxalate embedded in parenchymatous cells, and annular and spiral vessels. In the powder, part of the vascular bundle, epidermis, annular and spiral xylem vessels were observed. The secretory structures found in the stems, petioles, and leaf blades consisted of idioblasts containing anthocyanins. | [12,42,44,63,78,79,106,109] |
| K. pumila | It is a 30 cm high shrublet with small, fleshy leaves covered with powdery deposits formed by calcium carbonate sediments. The leaves are obovate (2.8 cm long, 1.7 cm wide, and 2.5 mm thick), opposite, wedge-shaped, and have a sinuate basis and dentate-serrate margins. | The reddish-brown or purple color appears along the leaf margins after exposure to sunlight due to the presence of anthocyanins in the epidermal cells and mesophyll vacuoles. The epidermal cells are polygonal–isodiametric or slightly oblong; they are more numerous on the abaxial surface. The anticlinal walls are curved or straight and are convex on the outer walls. The walls are thickened due to the presence of wax. The cuticula is smooth or slightly undulating, elevated or with striae, with sparse white or gray irregularly shaped and sized wax structures on the surface. The leaves are amphistomatic, with anisocytic stomata. The vascular bundles are collateral and closed. The sheath cells, or phloem, xylem parenchyma cells, subepidermal ground tissue, mesophyll tissue, and chlorenchyma tissue cells may contain tannin substances. | [110] |
| K. rhombopilosa | Small plant (no more than 10 cm tall), which blooms in spring. The leaves are hard and triangular, with a pale and wavy margin and green-yellow flowers with red lines. | [6] | |
| K. synsepala | One of the more unusual species of the genus because it is one of the few that produces stolon (lateral spreading stems). The leaves are arranged in rosettes and are thick, succulent, smooth, shiny, and green, with violet-red marks along the margins. This species is dormant in winter. The flowers are small, hairy, tubular, numerous, and pink. | [6] | |
| K. tetraphylla | The leaves are silvery pale green, which turn red in bright sun and revert to green in active growth. It has a large rosette of rounded or wavy leaves. The inflorescence is terminal and erect, with densely clustered panicles of greenish, waxy, narrow, urn-shaped flowers. | [6] | |
| K. tomentosa | The leaves are silvery, about 30 cm tall, reflecting the sun’s rays, lessening the chances of leaves overheating. | Its dense trichomes arise in triplets and perform a vital function in dry environments, helping to reduce the transpiration of water from the leaf surface | [6] |
| K. × houghtonii | A perennial erect herb, monocarpic, and can reach a height of up to 1.5 m. The leaves are opposite or verticillate, petiolate, with the leaf blade simple. The leaves vary from triangular to narrowly lanceolate, are serrate and mottled. The species forms corymbiform inflorescences of more than 100 pendulous, tetra or pentameric, dark-red flowers. | [102] |
These data demonstrate that even with some similarities between the species, an adequate morpho-anatomical study of the material can allow the correct identification of the studied species and validation of the scientific data (biological or chemical study). In this review, species identification errors that could disavow the scientific data obtained have been identified [29,106].
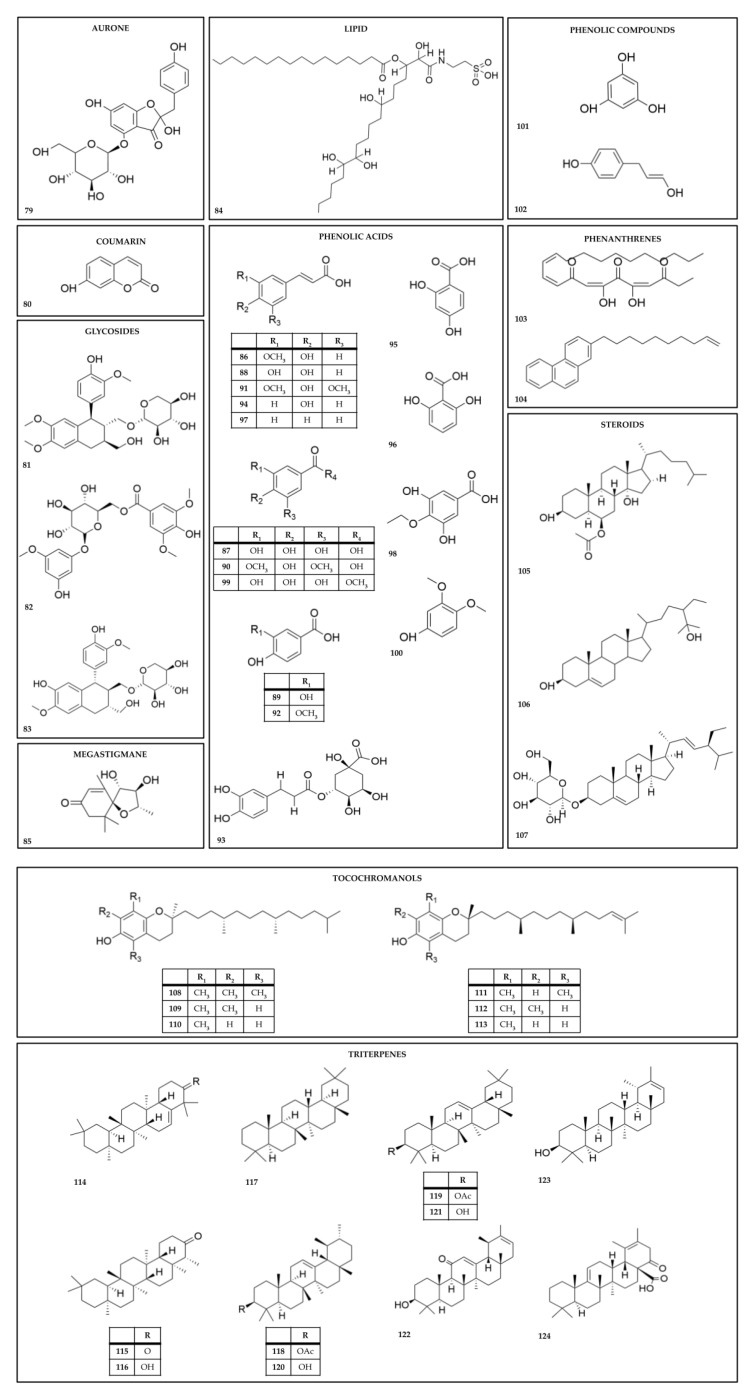
2.3. Chemical Composition
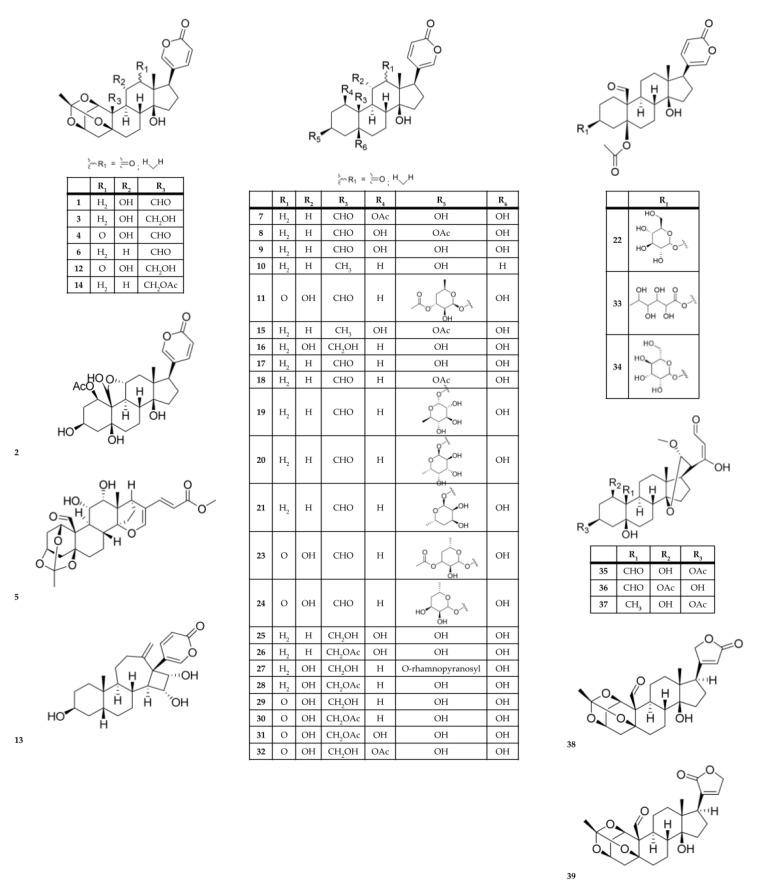
There have been 124 chemical metabolites reportedly isolated from Kalanchoe species (Table 4, Table 5 and Table 6 and Figure 3, Figure 4 and Figure 5). The most common are cardiac glycosides (compounds 1–39, in Table 4 and Figure 3) and flavonoids (compounds 40–78, in Table 5 and Figure 4). The primary species from which these compounds have been reported are K. daigremontiana, K. pinnata, K. delagoensis, and K. ceratophylla. Cardiac glycosides (such as the bufadienolide class) have been identified in the species K. ceratophylla, K. daigremontiana, K. delagoensis, K. hybrida, K. lanceolata, and K. pinnata (compounds 1–39, in Table 4 and Figure 3).
Figure 3.
Chemical structures of cardiac glycosides from Kalanchoe species.
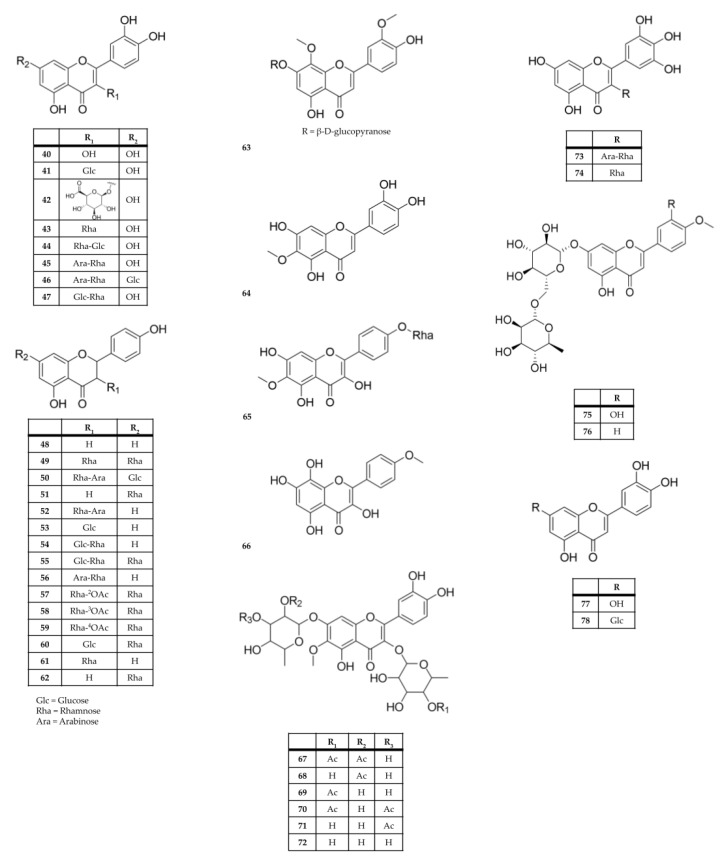
Figure 4.
Chemical structures of flavonoids from Kalanchoe species.
Figure 5.
Chemical structures of other secondary metabolites from Kalanchoe species.
Table 4.
Cardiac glycosides from Kalanchoe species.
| Extract and/or Plant Part | Compound Name | Species | References |
|---|---|---|---|
| Dichloromethane extract; methanol extract of aerial parts; flowers |
bryophyllin A (bryotoxin C) (1) |
K. daigremontiana; K. pinnata; K. delagoensis; K. ceratophylla |
[11,32,86,111,112,113,114,115] |
| Aqueous extract from the roots or whole plant; methanol extract of aerial parts |
bryophyllin B (2) |
K. daigremontiana; K. ceratophylla; K. delagoensis; K. pinnata |
[30,111,113,114,116] |
| Leaves, dichloromethane extract; methanol extract of the leaves; dichloromethane fraction from methanol extract | bryophyllin C (3) daigremontianin (4) methyl daigremonate (5) |
K. daigremontiana; K. pinnata |
[11,112,117] |
| Dichloromethane extract; aqueous extract from the roots | bersaldegenin-1,3,5-orthoacetate (6) |
K. daigremontiana; K. pinnata; K. delagoensis |
[11,30,32,86,116] |
| Aqueous extract from the roots; ethanol and dichloromethane extracts from the roots; leaves | bersaldegenin 1-acetate (7) |
K. daigremontiana; K. pinnata; K. delagoensis |
[11,30,32,86] |
| Leaves; ethanol and dichloromethane extracts from the leaves | bersaldegenin 3-acetate (8) | K. pinnata | [11,86,114] |
| Aqueous extract from the roots | bersaldegenin (9) | K. daigremontiana | [30] |
| Ethanol and dichloromethane extracts from the leaves | bufalin (10) | K. pinnata | [86] |
| Flower heads | bryotoxin A (11) | K. delagoensis | [111] |
| Aqueous extract from the roots; flowers | bryotoxin B (12) |
K. daigremontiana; K. delagoensis; K. pinnata |
[30,111,115,116] |
| Aqueous leaf extract; leaves | bufadienolide A (13) bufadienolide B (14) |
K. daigremontiana | [118] |
| Aqueous extract from the roots | daigredorigenin 3-acetate (15) | K. daigremontiana | [30,116] |
| 11α,19-dihydroxytelocinobufagin (16) | |||
| Methanol extract of aerial parts |
hellebrigenin (17) | K. ceratophylla | [113] |
| Methanol extract of aerial parts |
hellebrigenin-3-acetate (18) |
K. ceratophylla; K. daigremontiana |
[113,116] |
| Methanol extract of aerial parts |
kalanchoside A (19) kalanchoside B (20) kalanchoside C (21) |
K. ceratophylla | [113] |
| Methanol extract of aerial parts |
thesiuside (22) | K. ceratophylla | [113] |
| Ethanol extract; whole plant | kalantuboside A (23) kalantuboside B (24) |
K. delagoensis | [32] |
| Aqueous extract from the roots | 1β,3β,5β,14β,19-pentahydroxybufa-20,22-dienolide (kalandaigremoside A) (25) 19-(acetyloxy)-1β,3β,5β,14β-tetrahydroxybufa-20,22-dienolide (kalandaigremoside B) (26) 3β-(O-α-L-rhamnopyranosyl)-5β,11α,14β,19-tetrahydroxybufa-20,22-dienolide (kalandaigremoside C) (27) 19-(acetyloxy)-3β,5β,11α,14β-tetrahydroxybufa-20,22-dienolide (kalandaigremoside D) (28) 3β,5β,11α,14β,19-pentahydroxy-12-oxo-bufa-20,22-dienolide (kalandaigremoside E) (29) 19-(acetyloxy)-3β,5β,11α,14β-tetrahydroxy-12-oxo-bufa-20,22-dienolide (kalandaigremoside F) (30) 19-(acetyloxy)-1β,3β,5β,11α,14β-pentahydroxy-12-oxo-bufa-20,22-dienolide (kalandaigremoside G) (31) 1β-(acetyloxy)-3β,5β,11α,14β,19-pentahydroxy-12-oxo-bufa-20,22-dienolide (kalandaigremoside H) (32) |
K. daigremontiana | [30] |
| Ethyl acetate extract of the fresh; whole plant | lanceotoxin A (33) lanceotoxin B (34) |
K. lanceolata | [119] |
| Methanol extract; whole plant | kalanhybrin A (35) kalanhybrin B (36) kalanhybrin C (37) |
K. hybrida | [120] |
| Ethanol extract of the whole plant | kalantubolide A (38) kalantubolide B (39) |
K. delagoensis | [32] |
Flavonoids have been identified in aqueous, hydroalcoholic, and alcoholic extracts from the leaves of K. blossfeldiana, K. crenata; K. daigremontiana, K. delagoensis, K. fedtschenkoi, K. laciniata, K. marmorata, K. mortagei, and K. pinnata (compounds 40–78, Table 5 and Figure 4). The most common flavonoids/glycosylated flavonoids described from these species are derivatives of quercetin (40), patuletin (69–71), eupafolin (64), and kaempferol (48–62).
Table 5.
Flavonoids from Kalanchoe species.
| Extract and/or Plant Part | Compound Name | Species | References |
|---|---|---|---|
| Flower; ethanol leaf extractFlowers; Leaves | quercetin (40) |
K. pinnata K. delagoensis K. blossfeldiana; K. mortagei; K. fedtschenkoi; K. daigremontiana; K. longiflora K. ceratophylla |
[32,37,121,122,123,124,125,126,127] |
| Flower extractFlowers | Quercetin 3-O-β-glucoside (quercetin 3-O-glucoside; isoquercetin; isoquercetrin) (41) |
K. pinnata; K. blossfeldiana; K. daigremontiana; K. delagoensis |
[49,122,123,127,128] |
| Flower extractFlowers | quercetin 3-O-β-d-glucuronopyranoside (miquelianin) (42) | K. pinnata | [122] |
| Aqueous and methanolic leaf extractsLeaves | quercetin 3-O-rhamnoside (quercitrin) (43) |
K. pinnata; K. delagoensis; K. longiflora; K. ceratophylla |
[42,82,122,123,125,126,129,130] |
| Flowers, Aqueous leaf extractFlower, Leaves | quercetin-3-O-β-d-xylopyranosyl (1→2)-α-L-rhamnopyranoside (44) |
K. blossfeldiana
K. daigremontiana |
[118,127] |
| Aqueous and methanolic leaf extracts; flower extractFlowers, Leaves | quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (45) | K. pinnata | [8,82,83,122,129,130] |
| Methanol leaf extractLeaves | quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside-7-O-β-d-glucopyranoside (46) | K. pinnata | [129] |
| Ethanol leaf extractLeaves | quercetin 3-O-rutinoside (rutin) (47) | K. pinnata | [121] |
| Methanolic and hydroethanolic extracts from the leavesLeaves | kaempferol (48) |
K. delagoensis; K. pinnata; K. fedtschenkoi; K. longiflora; K. ceratophylla |
[2,37,43,123,125,126,129,131] |
| Water and ethanol extracts Leaves |
kaempferol 3,7-O-dirhamnoside (kaempferitrin) (49) kaempferol 3-O-β-d-xylopyranosyl-(1→2)-α-L-rhamnopyranoside-7-O-β-d-glucopyranoside (daigremontrioside) (50) |
K. daigremontiana | [49] |
| Leaves | kaempferol 7-O-rhamnoside (51) |
K. delagoensis; K. longiflora |
[123,125] |
| Methanol leaf extractLeaves | kaempferol 3-O-β-d-xylopyranosyl-(1→2)-α-l-rhamnopyranoside (kaempferol 3-O-xylosyl-rhamnoside) (52) |
K. pinnata; K. daigremontiana |
[49,118,129] |
| Leaves | kaempferol 3-O-galactoside (trifolin) (53) | K. delagoensis | [123] |
| Leaves | kaempferol 3-rutinoside (nicotiflorin) (54) |
K. pinnata; K. longiflora |
[70,125] |
| Leaves | kaempferol- 3-O-robinoside-7-O- rhamnoside (robinin) (55) |
K. delagoensis; K. longiflora |
[123,125] |
| Aqueous and methanolic leaf extractsLeaves | kaempferol 3-O-α-l-arabinopyranosyl (1→2)-α-l-rhamnopyranoside (kapinnatoside) (56) | K. pinnata | [83,129,130] |
| Ethyl acetate extract of the wholeWhole plant | kaempferol 3-O-α-l-(2-O-acetyl)rhamnopyranoside 7-O-α-l-rhamnopyranoside (57) kaempferol 3-O-α-l-(3-O-acetyl)rhamnopyranoside 7-O-α-l-rhamnopyranoside (58) kaempferol 3-O-α-l-(4-O-acetyl)rhamnopyranoside 7-O-α-l-rhamnopyranoside (59) kaempferol 3-O-α-d-glucopyranoside 7-O-α-l-rhamnopyranoside (60) afzelin (kaempferol 3-O-α-l-rhamnopyranoside) (61) α-rhamnoisorobin (kaempferol 7-O-α-l-rhamnopyranoside) (62) |
K. pinnata | [132] |
| Aqueous leaf extractLeaves | 4′,5-dihydroxy-3′,8-dimethoxyflavone 7-O-β-d-glucopyranoside (63) | K. pinnata | [130] |
| Aerial parts; methanol extract from the stemsStems | eupafolin (6-methoxyluteolin) (64) | K. ceratophylla | [17,126] |
| Aerial parts | eupafolin 4′-O-rhamnoside (65) | K. ceratophylla | [126] |
| Ethanol extract of the wholeWhole plant | 4′-methoxyherbacetin (66) | K. delagoensis | [32] |
| Stems and leaves; Leaves | kalambroside A (67) kalambroside B (68) kalambroside C (69) patuletin 3-O-(4′-O-acetyl-α-l-rhamnopyranosyl)-7-O-(3′-O-acetyl-α-l-rhaminopyranoside) (70) patuletin 3-O-α-l-rhamnopyranosyl-7-O-(3′-O-acetyl-α-L-rhaminopyranoside) (71) |
K. laciniata | [133] |
| Stems and leaves; hydroethanolic extract from leavesStems; Leaves | patuletin 3-O-α-l-rhamnopyranosyl-7-O-α-l-rhamnopyranoside (72) | K. laciniata | [40,44,133] |
| Methanol leaf extract Leaves |
myricetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (73) myricitrin (myricetin 3-O-α-l-rhamnopyranoside) (74) diosmine (diosmetin 7-O-α-l-rhamnopyranosyl-(1→6)-β-d-glucopyranoside) (75) acacetin 7-O-α-l-rhamnopyranosyl-(1→6)-β-d-glucopyranoside (76) |
K. pinnata | [129] |
| Ethanol leaf extractLeaves | luteolin (77) |
K. ceratophylla; K. pinnata |
[121,126] |
| Ethanol leaf extractLeaves | luteolin 7-O-β-d-glucoside (78) | K. pinnata | [121] |
Recently, a comprehensive approach encompassing metabolomics and machine learning techniques was implemented [134] to investigate K. daigremontiana, K. × houghtonii, and K. delagoensis plant tissue cultures. By employing untargeted metabolomics, a remarkable total of 460 phenolic compounds were identified. Among them, the elicitation process significantly influenced the biosynthesis of 164 compounds. Through the utilization of neuro fuzzy logic, the study successfully predicted the impact and interactions involved in plant cell growth as well as the biosynthesis of various subfamilies of polyphenols. The findings highlight the distinct genotype-dependent role of salicylic acid in eliciting Kalanchoe cell cultures, while methyl jasmonate emerged as a secondary contributing factor.
Several other secondary metabolites (steroids, triterpenes, coumarins, and others) have also been isolated from different species of Kalanchoe and are described in the literature (compounds 79–124, in Table 6 and Figure 5).
Table 6.
Other compounds isolated and identified from Kalanchoe species.
| Class | Extract and/or Plant Part | Compound Name | Species | References |
|---|---|---|---|---|
| Aurone | Aqueous root extractRoots | hovetrichoside C (79) | K. daigremontiana | [116] |
| Coumarin | Aerial parts | 7-hydroxycoumarin (80) | K. ceratophylla | [126] |
| Glycoside | Roots | KPB 100 (81) KPB 200 (82) schisandriside (83) |
K. pinnata
K. daigremontiana |
[69,116] |
| Glycoside | Aqueous root extract | schisandriside (83) | K. daigremontiana | [116] |
| Lipid | Ethanol extract of the wholeWhole plant | taurolipid C (84) | K. delagoensis | [32] |
| Megastigmane | Ethanol extract of the wholeWhole plant | (6S,7R,8R,9S)-6- oxaspiro-7,8-dihydroxymegastigman-4-en-3-one (tubiflorone) (85) |
K. delagoensis | [32] |
| Organic/ phenolichenolic acid |
Leaves, ether leaves extract | ferulic acid (86) |
K. delagoensis; Kalanchoe sp. K.daigremontiana K. pinnata; |
[29,123,135,136] |
| Ethanol extract of the wholeWhole plant; leavesLeaves | gallic acid (87) |
K. delagoensis; Kalanchoe sp.; K. daigremontiana |
[29,32,123,135] | |
| Leaves; ether leaves extract | caffeic acid (88) |
K. delagoensis; Kalanchoe sp.; K. longiflora; K. daigremontiana K. pinnata |
[29,123,125,135,136] | |
| Leaves | protocatechuic acid (89) |
K. delagoensis; Kalanchoe sp.; K. daigremontiana |
[29,123,135] | |
| Ethanol extract of the whole plant; leaves; ether leaves extractWhole plant; Leaves | syringic acid (90) |
K. delagoensis; Kalanchoe spp.; K. pinnata |
[32,123,135] | |
| Leaves | sinapic acid 91) | Kalanchoe sp. | [135] | |
| Ethanol extract of the wholeWhole plant; leavesLeaves | vanillic acid (92) |
K. delagoensis; Kalanchoe sp. |
[32,135,136] | |
| Leaves | chlorogenic acid (93) |
Kalanchoe sp.; K. longiflora |
[125,135] | |
| Leaves; ether leaves extract | p-Coumaric acid (94) |
Kalanchoe sp.; K. longiflora; K. daigremontiana K. pinnata |
[29,125,135,136] | |
| Leaves | β- resorcylic acid (95) | Kalanchoe sp. | [135] | |
| γ-resorcylic acid (96) | ||||
| Ethanol extract of the wholeWhole plant | cinnamic acid (97) 4-O-ethylgallic acid (98) methyl gallate (99) |
K. delagoensis | [32] | |
| Phenolic compounds | Whole plant | 4-O-ethylgallic acid (98) methyl gallate (99) 3,4-dimethoxyphenol (100) phloroglucinol (101) 3,4-dihydroxyallylbenzene (102) |
K. delagoensis | [32] |
| Phenanthrene | Leaves | bryophollenone (103) 2(9-decenyl) phenanthrene (104) |
K. pinnata | [137] |
| Steroid | Leaves | bryophyllol (105) 24-ethyl-25-hydroxycholesterol (106) |
K. pinnata | [137] |
| 24-ethyl-25-hydroxycholesterol (106) | ||||
| Ethanol extract of the wholeWhole plant | stigmasterol-O-d-glucoside (107) | K.delagoensis | [32] | |
| Tocochromanol | Hexane leaf extractLeaves | α-tocopherol (108) γ-tocopherol (109) δ-tocopherol (110) β-tocomonoenol (111) γ-tocomonoenol (112) δ-tocomonoenol (113) |
K. daigremontiana | [138] |
| iterpeneTriterpene | Aerial parts; petroleum ether extract from flowers; methanol extract Flowers |
friedelin (114) |
K. fedtschenkoi; K. marnieriana; K. daigremontiana K. integra |
[136,139,140] |
| glutinone (115) | K. miniata | [139] | ||
| glut-5-en-3- β-ol (glutinol) (116) |
K. fedtschenkoi; K. daigremontiana K. integra |
[136,139,140,141] | ||
| Leaves | 18α-oleanane (117) α-amyrin acetate (118) |
K. pinnata | [137] | |
| α-amyrin acetate (118) | ||||
| Leaves | β-amyrin acetate (119) |
K. pinnata; K. miniata |
[137,139] | |
| Leaves; methanol extract | α-amyrin (120) |
K. pinnata
K. daigremontiana |
[137,141] | |
| Leaves; methanol extract | β-amyrin (121) | K. pinnata; | [137,140,141] | |
| Leaves, petroleum ether extract from flowers; Flowers | bryophynol (122) Ψ-taraxasterol (123) bryophollone (124) |
K. daigremontiana
K. pinnata K. integra |
[136,137] |
Until now, of the four species most reported as medicinal plants with ethnopharmacological use (K. pinnata, K. laciniata, K. crenata, and K. daigremontiana), only two had cardiac glycosides identified in published studies (K. pinnata and K. daigremontiana). In contrast, compounds from the flavonoid class were identified in all four species. Additionally, although the juice or crude extract (produced by maceration) is the ethnomedicinal form of use in the literature, phytochemical studies are generally based on polar organic extracts (ethanol, methanol) prepared from leaves, stems, roots, flowers, and whole plant. Few studies using nonpolar or aqueous solvents have been identified. This is an important observation because it is known that popular knowledge needs to be confirmed, and the presence of the biological compounds in an extract are related to the solvent and the procedure used to obtain it.
2.4. Pharmacological Activities
In folk medicine, the use of Kalanchoe species is related to several disease conditions. Due to its widely distributed and popular use, experiments have been performed to corroborate the pharmacological potential activities and to prove the therapeutic potential of different species of Kalanchoe. So far, only 16 of the 133 species of the genus Kalanchoe have been analyzed to assess various pharmacological activities. The primary activities studied have been antioxidant, anti-inflammatory, cytotoxic, and antimicrobial properties. Of these sixteen species, four are not reported in the literature regarding their popular uses, but their pharmacological activities were tested (K. blossfeldiana, K. longiflora, K. scapigera, and K. rhombopilosa).
Kalanchoe blossfeldiana methanolic extract (ME) showed biofilm formation and demonstrated anticytokine properties [128]. Its aqueous extract (AE) in zinc oxide nanoparticles showed promising antibacterial and antifungal potential and a potent cytotoxic effect against a HeLa cell line [142]. In comparison with two other species (K. daigremontiana and K. pinnata), the ethanolic extract (EE) of K. blossfeldiana exhibited the most potent cytotoxic activity (IC50: < 19 µg/mL for HeLa and SKOV-3 cells) and the strongest antibacterial effects (MIC: 8.45, 8.45, 0.25, and <33.75 µg/mL for S. aureus, S. epidermidis, and E. hirae, respectively) but this extract did not contain bufadienolides, which are known to elicit these biological effects (cytotoxic and antibacterial) [11].
Kalanchoe ceratophylla stems ME has been suggested to provide analgesic and anti-inflammatory effects, with its anti-inflammatory mechanisms being well discussed. Eupafolin (64) demonstrated good pharmacological activity, and the antioxidant potential and efficacy of this species may be largely attributed to polyphenolic compounds [16,17]. The antiviral effects of the leaf extract from this species were investigated against RNA enteroviruses, specifically enterovirus 71 (EV71) and coxsackievirus A16 (CVA16). The extract showed little cytotoxicity and exhibited concentration-dependent antiviral activities, including reductions in cytopathic effects, plaque formation, and virus yield. Furthermore, the extract demonstrated greater potency in antiviral activity compared to ferulic acid, quercetin, and kaempferol, significantly inhibiting the in vitro replication of EV71 (IC50: 35.88 μg/mL) and CVA16 (IC50: 42.91 μg/mL). As such, this extract may be considered a safe anti enteroviral agent [143].
Kalanchoe crenata ME was non-toxic when administered orally for animals over a period of 14 days. The ME and its fractions showed fold decreases in IC50 for fractions regarding CYP3A4; phytoconstituents in the ME were a reversible and time-dependent inhibitor of CYP3A4, and the methanol fraction is a potential source of a new oral anti-nephropathic drug [18,20,22]. The cytotoxicity of ME leaves was highlighted in comparison with five other species, with reported IC50 values that ranged from 2.33 μg/mL (SPC212, mesothelioma) to 28.96 μg/mL (HepG2, hepatocarcinoma), and apoptosis induction via ROS production [23]. Its AE were quantitatively assessed for significant elements, and the amounts of Ca, K, and Mg detected could be correlated to its traditional usage in cases of hypertension and arrhythmia. However, the presence of heavy metals (Pb and As inorganic) may be a major health concern [39]. The AE antidepressant potential could be possibly mediated by a complex interplay between serotoninergic, opioidergic, and noradrenergic systems [75]. The EE showed no genotoxic potential and possessed cardioprotective effects against DOX-induced cardiotoxicity in Sprague-Dawley rats [19]. The methylene chloride/methanol extract and its hexane, methylene chloride, ethyl acetate, n-butanol fractions, and aqueous residue were evaluated for their analgesic effects and anticonvulsant activity. The results suggested the presence of peripheral and central analgesic activities, along with an anticonvulsant effect [144].
Bufadienolide-rich fractions (BRF) isolated from the roots of K. daigremontiana presented antioxidant activity against DPPH radicals (EC50: 21.80 µg/mL); moderate activity for peroxynitrite-induced oxidative stress; protective levels of 3-nitrotyrosine and thiol groups (50 µg/mL); effective antioxidant potential for hydroperoxides and TBARS generation (1–5 and 25–50 µg/mL, respectively); uncompetitive inhibitory effect on the enzymatic properties of a serine proteinase-thrombin (1–50 µg/mL) (IC50: 2.79 µg/mL); and of plasmin (0.05–50 µg/mL). No effects were observed to prevent the oxidation of low-molecular plasma thiols, and no cytotoxicity was observed. Docking studies suggested that only some compounds (mostly bersaldegenin 1-acetate (7), bryotoxins (1,11–12), and hovetrichoside C (78)) were bound to plasminogen/plasmin, depending on the presence or absence of the substrate in the active site, suggesting allosteric regulation of plasminogen activation and plasmin activity by components of the examined fraction [14,15,116]. Additionally, root extracts of K. daigremontiana was also evaluated [145] in comparison to other plants (Cyphomandra betacea, Robinia pseudoacacia, Nothofagus pumilio, and Rosmarinus officinalis) in a set of in vitro assays and, regarding the cytotoxic assays, K. daigremontiana was the only species considered to be highly toxic.
The anti-inflammatory activity of AE, EE, and petroleum ether (PEE) extracts obtained from the leaves of K. pinnata and K. daigremontiana were compared and the AE and PEE of K. daigremontiana showed the highest anti-inflammatory effects (−105.69 ± 0.40 and −79.95 ± 0.37, respectively) [106]. Crude extracts from the leaves of K. daigremontiana can contribute to antiviral activity [118] and, most prominently, to high antibacterial activity [10] against E. coli and S. aureus. A macerated ME from the leaves of K. daigremontiana demonstrated high antiparasitic activity against E. histolytica and T. vaginalis (IC50: 70.71 ± 3.08 and 105.27 ± 5.19 μg/mL, respectively) [124]. Antioxidant properties of nanovesicle preparations of K. daigremontiana compared to Artemisia absinthium, Hypericum perforatum, Silybum marianum, Chelidonium majus, and Scutellaria baicalensis demonstrated that the activities are specific to plant species, but K. daigremontiana and S. marianum nanoparticle showed similar characteristics, suggesting future analysis to test the complementary/synergic effects between them [146].
The cytotoxic effects of K. daigremontiana were investigated in relation to human adenocarcinoma (HeLa), ovarian (SKOV-3), breast (MCF-7) and melanoma (A375) cells [49,147], and human multiple myeloma cells [28]. The dichloromethane fraction (DF) showed strong activity against all cell lines (IC50 ≤ 10 µg/mL), and it could be related to the presence of bersaldegenin-1,3,5-orthoacetate (6). The AE reduced the viability of tumor cells by 13% and, in combination with doxorubicin, showed an additive synergism of action, which enhanced this effect. The intracellular glutathione level decreased by 25%, mitochondrial membrane potential decreased by 19%, and ATPase activity increased 50%, which shows that this extract affects the metabolism of tumor cells and contributed to their death and antitumor activity. The AE elevated the oxidative stress levels in SKOV-3 cells as well as exhibited notable antiproliferative and cytotoxic effects, leading to the depolarization of the mitochondrial membrane and causing a significant cell cycle arrest in the S and G2/M phases of this cell line. The non-activation of caspases 3, 7, 8, and 9 suggests a non-apoptotic mode of cell death. Additionally, real-time PCR analysis suggested that the AE may induce cell death through the involvement of TNF receptor (tumor necrosis factor receptor) superfamily members 6 and 10.
The K. delagoensis n-hexane and ethanol extracts suggested wound-healing potential [34]. Its n-butanol-soluble fraction was able to inhibit cell proliferation and reduce cell viability by two mechanisms exclusively involved with cell division (inducing multipolarity and disrupting chromosome alignment during metaphase) [31]. The AE of this species promoted cell cycle arrest and senescence-inducing activities in A549 cells, and tumor growth was effectively inhibited, suggesting that this extract is an antitumor agent [148]. Compounds isolated from the EE of this species were evaluated for anti-inflammatory and cytotoxic activities [32,33]. Some compounds (quercetin (40), syringic acid (84), 3,4-dimethoxyphenol (94), 3,4-dihydroxyallylbenzene (96), and tubiflorone (120)) possessed NO inhibitory activity (IC50 15.1/0.9–98.9/1.3 mM). The biological evaluation indicated that some cardenolides (kalantubolide A (38) and kalantubolide B (39)) and bufadienolide glycosides (bryophyllin A (1), bersaldegenin-1,3,5-orthoacetate (6), bersaldegenin 1-acetate (7), kalantuboside A (23), kalantuboside B (24)) demonstrated strong cytotoxicity against four human tumor cell lines (A549, Cal-27, A2058, and HL-60) (IC50 0.01–10.66 µM). In addition, these compounds blocked the cell cycle in the G2/M-phase and induced apoptosis in HL-60 cells.
The ethyl acetate extract (EAE) of K. flammea is non-genotoxic and exhibits selective cytotoxic activity against several cell lines of prostate cancer, with mechanisms of induced apoptosis by the intrinsic pathway, significant downregulation of apoptosis-related proteins, induced DNA fragmentation, and cell cycle arrest. Additionally, a fraction rich in coumaric acid and palmitic acid, obtained from the EAE, demonstrated selective cytotoxic activity against PC-3 cells [36]. Similarly, fraction rich in fatty acids obtained from the EE of K. pinnata demonstrated inhibited lymphocyte proliferation in vitro and showed in vivo immunosuppressive activity [149].
Kalanchoe fedtschenkoi and K. mortagei were studied to compare their antibacterial potential [37], and K. fedtschenkoi extracts demonstrated growth inhibitory effects against A. baumannii, P. aeruginosa, and S. aureus, and its stem extracts exhibited the best inhibitory activity against A. baumannii (IC50 128 µg/mL). Four treatments (250 µg/mL for 72 h) with different parts of the AE of K. gastonis-bonnieri inhibited the proliferation of benign prostatic hyperplasia (BPH) cells (13.5–56.7%), and the AE of underground parts was the most active, stimulating changes in the BPH cells and modulating crucial processes such as proliferation, viability, and apoptosis [38].
In a study that compared 57 extracts obtained from 18 plants, K. glaucescens possessed the second-highest antioxidant activity and considerable cytotoxicity against leukemia cells [150]. The K. laciniata extracts from leaves picked before and during blooming (BB and DB, respectively) were tested to assess anti-inflammatory effects and both extracts presented no acute toxicity in mice (0.25 to 5 g/kg). Oral doses of the BB (0.25, 0.5, and 1.0 g/kg) significantly inhibited paw edema during the first four hours after injection of 2% carrageenan but oral doses of the DB (0.5, 1.0 and 2.0 g/kg) had no inhibitory activity [81]. The AE of K. laciniata also displayed thyroid peroxidase inhibition [151], immunomodulatory and anti-inflammatory properties [152,153]. The aqueous-methanol (AM) and n-hexane (NH) extracts of this species showed significant mutagenicity and cytotoxicity, and the NH extract treatment was more sensitive than others to E. coli [47,48]. Hydroethanolic extracts (HEE) obtained from K. laciniata leaves indicated dose-dependent cytotoxic activity against a 3T3 cell line (normal) and the 786–0 line (kidney carcinoma) (92.23% cell inhibition). In an in vivo experiment, the extract showed only liver changes and damage related to acute toxicity, and no significant toxicity. The HEE was able to reduce Salmonella growth rate, and the cell number was reduced with the release of the bacterial content. This species is confirmed as a natural source of antioxidant agents [45,154].
The gastroprotective activity of the leaf juices of K. laciniata was evaluated and compared with K. pinnata, and both species showed gastroprotective effects; however, the K. laciniata extract reduced the lesions in all the tested doses [43]. Other authors [155] determined the effect of aqueous, ethanol, and hexane extracts of K. laciniata leaves in comparison to other plants (Drymoglossum piloselloides leaves and Aegle marmelos flowers) against CaOx urolithiasis in vitro and the results clearly demonstrated that all species have the capacity to inhibit the nucleation, growth, and aggregation of CaOx crystals. Preliminary phytochemical screening also revealed the presence of reducing sugars, proteins, flavonoids, tannins, and polyphenol compounds in K. laciniata.
Kalanchoe longiflora was evaluated and compared to eight species of Kalanchoe in relation to antitrypanosomal, antimalarial, antileishmanial, cytotoxic, and antimicrobial activities [125]. This study revealed that K. longiflora leaf extracts showed activity against T. brucei with an inhibition concentration of sample at 50% (IC50 17.6 µg/mL). To determine the mechanism of action of K. longiflora extract as a potent anti-trypanosomal and cytotoxic agent, the authors investigated the ability to inhibit topoisomerase I enzyme and found the K. longiflora extract showed the best activity (IC50 0.148 µg/mL).
The antioxidant potential of various extracts of K. pinnata were evaluated and significant dose-dependent antioxidant activity was demonstrated in all of them. The antioxidant activities of the AE from the leaves improves the antioxidant potential in various organs (mainly the aorta), prevents adverse changes due to CCl4 intoxication in rats by pre-treatment (25 and 50 mg/kg b.w.), and the inhibits arginase II, as well as increasing antioxidant status in CCl4-intoxicated rats, which suggests a protection of the kidneys against CCl4-induced oxidative damage [59,63,65,83]. The EE from its stem/bark was evaluated by DPPH and exhibited high antioxidant activity (IC50 37.28 µg/mL). In comparison with other extracts (AE and PEE) obtained from the leaves, the EE showed the greatest radical inhibitory effect by DPPH, reaching a maximum inhibitory effect of 49.5 ± 5.6% (2000 µg/mL) [106,156]. The antioxidant property of ME from leaves showed 69.77% of free radical inhibition (100 µg/mL) of DPPH [62].
The concentration of vitamin C in AE of two Kalanchoe species (K. daigremontiana and K. pinnata) was evaluated and compared [12]; the amount of vitamin C was highest for the AE of K. pinnata (81 mg/100 g). Four major flavonoids obtained from HEE of K. pinnata leaves were evaluated by xanthine oxidase (XO) inhibition and antioxidant activity (DPPH and ABTS). It was found that kaempferol and quercetin derivatives moderately inhibited XO, while only quercetin derivatives displayed average radical scavenging activity, suggesting that quercetin 3-O-α-L-arabinopyranosyl-(1→2)-α-L-rhamnopyranoside (45) can be indicated as a specific marker of this species [71].
The K. pinnata AE and quercetin (40) inhibited degranulation and cytokine production of bone marrow-derived mast cells following IgE/FcRI crosslinking in vitro: they decreased the development of airway hyperresponsiveness, airway inflammation, goblet cell metaplasia, and production of IL-5, IL-13, and TNF in vivo. In contrast, treatment with quercitrin (43) did not affect the tested parameters [42]. Additionally, the AE and quercitrin showed protective effects in fatal anaphylactic shock [157].
The antinociceptive, antiedematogenic, and anti-inflammatory potential as well as the possible mechanisms of action of the subcutaneous administration of K. pinnata AE of flowers, its ethyl acetate (EAF), and butanol (BF) fractions, and the main flavonoid (45) were investigated in a mouse model; the AE and its main flavonoid produced antinociceptive, antiedematogenic, and anti-inflammatory activities through COX inhibition and TNF-𝛼 reduction [8]. The flowers AE also are described as a rich source of T-suppressive flavonoids that may be therapeutically useful against inflammatory diseases [122]. The AE and the EE of K. pinnata leaves were found to be effective as hepatoprotective, and the AE was more effective [158]. The AE of the K. pinnata leaves were also examined [159] to investigate the ulcer healing properties and gastroprotective activity. The results indicate that treatment with the AE exhibited a higher inhibition percentage compared to pretreatment with an isolated quercetin derivative. This suggests that while the isolated flavonoid may possess gastroprotective activity, other compounds present in K. pinnata could potentially act synergistically to enhance its effect.
Studies comparing the anti-inflammatory [131] and the anti-ophidic [44] activities of K. laciniata and K. pinnata have been performed. The anti-inflammatory activity of topical formulations containing AE of both species showed good results; however, K. laciniata was most effective, with excellent results on the formulation containing a low concentration of its AE (5%). On the other hand, even though HE extracts from both species significantly reduced the hemorrhagic activity of B. jararaca venom in pre-treatment protocol, only K. pinnata was active in the post-treatment protocol and in the anti-edematogenic activity assay. It was also more active in the phospholipase test. Continuing the study, the authors conducted a study [160] to evaluate the healing properties and mechanism of action of the topical formulation of K. pinnata, which demonstrated the ability to stimulate the healing of skin wounds, leading to a reduction in wound area. Additionally, it exhibited a notable decrease in inflammatory infiltrate, as well as lowered levels of IL-1β and TNF-α. Moreover, the formulation induced angiogenesis by increasing the expression of VEGF, similar to the effects of Fibrinase. These findings highlight the significant potential of this formulation as a novel active ingredient in the development of pharmaceuticals for wound healing. The EE of K. pinnata also shows wound healing activity [161].
A method for targeting and identifying molecules with antimicrobial activity was implemented, which could potentially replace chemical preservatives in cosmetic applications [70]. An in vitro evaluation of the antimicrobial activity of different extracts (petroleum ether, chloroform, methanol, and aqueous) produced from K. pinnata roots was performed against E. coli, S. aureus, P. aeruginosa, and C. albicans [78], and the ME presented as an effective antibacterial, while none of the extracts showed activity against C. albicans. The EE of stem bark was tested against antimicrobial activity [156]; it inhibited the growth of microorganisms such as B. cereus, E. coli, S. aureus, P. aeruginosa, K. pneumoniae, and A. niger, while the extract was inactive against S. typhi and C. albicans.
The AE of K. pinnata displayed a significant reduction in hepatic and splenic parasite burden, indicating that the oral efficacy of this species extends to visceral leishmaniasis caused by L. chagasi [73,162]. The antileishmanial activity of three flavonoid glycoside and free quercetin (40) (isolated from the AE of K. pinnata) were also demonstrated [82,130], with a low toxicity profile. The anthelmintic capacity of the PEE and ME of K. pinnata was explored [163]. Both extracts were investigated in different concentrations for anthelmintic activity against P. posthuma and they exhibited no anthelmintic activity even at the highest concentration (200 mg/mL); the conclusion was that they had no vermicide activity. Two compounds (KPB-100 (122) and KPB-200 (123)) identified from K. pinnata are promising targets for synthetic optimization and in vivo study against human alpha herpesvirus 1 and 2 and vaccinia virus. KPB-100 (122) inhibited all the tested viruses [69]. The bryophyllin A (1) (isolated from K. pinnata), bersaldegenin 1,3,5-orthoacetate (6) and daigremontianin (4) (isolated from K. x houghtonni) showed good inhibitory potential on the Epstein-Barr virus, but bryophyllin A (1) was the most effective (IC50: 0.4 µM) [112]. Additionally, both bryophyllin A and C isolated from a ME of the leaves of K. pinnata showed strong insecticidal activity against third instar larvae of the silkworm.
The EE of K. pinnata shows great hypoglycemic effect and the improvement of the number of pancreatic Langerhans beta cells at medium-dose treatment (11.6 mg/kg); it has a hypoglycemic effect through the improvement of the number of pancreatic Langerhans beta-cells. On the other hand, the DF from AE of K. pinnata demonstrates a dose-dependent insulin secretagogue action; reducing fasting blood glucose values (from 228 mg/dL to 116 mg/dL, on 10 mg/kg); improving the glycated hemoglobin to 8.4% (compared with 12.9% in diabetic controls); and restoring insulin level and lipid profile values close to normal [87,90]. The antioxidant effects of combined preparations of K. pinnata and metformin were investigated [164]. The treatment with K. pinnata alone (400 µg/mL), resulted in a significant increase in catalase activity in both non-diabetic and diabetic human skeletal muscle myoblasts, as well as in a human skeletal muscle myoblast cell line subjected to H2O2-stress-induced stress. Simultaneously, K. pinnata treatment led to a significant reduction in malondialdehyde levels. Notably, the combination of K. pinnata and metformin appeared to modulate antioxidant responses by increasing the enzymatic activity of superoxide dismutase, elevating the levels of reduced glutathione, and reducing glutathione levels in both non-diabetic and diabetic human skeletal muscle myoblasts, as well as in the H2O2-stress-induced human skeletal muscle myoblasts, which demonstrates the potential of these treatment in addressing the pathophysiological complications linked to oxidative stress in individuals with type II diabetes.
Investigations of the in vitro cytotoxicological and genotoxicological effects of K. pinnata were performed using its AE [85], leaf juice [64], and EE [165]. All the results indicated significantly lower results than those found for a positive control, suggesting a weak genotoxic response or a non-genotoxic effect. Hence, these extracts of K. pinnata can be used, but not for long durations or at higher doses, which indicates that this material may cause DNA damage and/or may have mutagenic effects. Consequently, its use should be restricted. Its chloroform extract (CE) obtained from the leaves demonstrated potential as anticancer and anti-HPV therapeutic for treatment of HPV infection and cervical cancer [166]. The cytotoxic activities of the EE of K. pinnata leaves were compared with the EE of three other species of the genus (K. daigremontiana, K. milloti, K. nyikae). The EE of K. pinnata showed the highest cytotoxicity against a lymphoma cell line, in a dose-dependent manner [135]. The anticancer mechanisms were revealed through a molecular approach [167] to support the use of K. pinnata as an adjuvant in cancer treatment. Gallic acid, caffeic acid, coumaric acid, quercetin, quercitrin, isorhamnetin, kaempferol, bersaldegenin, bryophyllin A, bryophyllin C, bryophynol, bryophyllol, bryophollone, stigmasterol, and campesterol were identified as bioactive compounds which participate. Some compounds were identified as bioactive, participating in the regulation of proliferation, apoptosis, cell migration, angiogenesis, metastasis, oxidative stress, and autophagy, with the potential to act as epigenetic drugs by reverting the acquired epigenetic changes associated with tumor resistance to therapy—such as the promoter methylation of suppressor genes, inhibition of DNMT1 and DNMT3b activity, and HDAC regulation—through methylation, thereby regulating the expression of genes involved in the PI3K/Akt/mTOR, Nrf2/Keap1, MEK/ERK, and Wnt/β-catenin pathways. Bryophyllin A, bryophyllin B, and bersaldegenin-3-acetate isolated from AE of K. pinnata are well known regarding their cytotoxic effects against A-549, HCT-8, P-388, and L-1210 tumor cells [114].
Two creams containing the AE of K. pinnata leaves (6%) and its major flavonoid quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (45) (0.15%) were developed and compared [67]. Both creams were topically evaluated and resulted in better re-epithelialization and dense collagen fibers. The flavonoid plays a fundamental role in wound healing but similar results that were found for both creams indicate that the use of the AE could be more profitable than the isolated compound. This extract of the AE also significantly prevented the increase of systolic and diastolic arterial pressures in salt hypertensive rats, and the concomitant administration of high-salt + the AE significantly prevented salt-induced hypertension in rats [65].
The effects of pressed juice (PJ), flavonoid-enriched fractions (FEF), bufadienolide-enriched fractions (BEF), and a flavonoid aglycone mixture (FAM) on detrusor contractility were investigated as a major target in overactive bladder disease [60]. The PJ increased the contraction force of muscle strips, the FEF had almost no effect on contractility, while the BEF and FAM led to a dose-dependent lowering of contraction force. The data indicated that several components of the PJ may contribute to the inhibitory effect on detrusor contractility, which in turn provides support for overactive bladder treatment. Other authors aimed to substantiate the use of the PJ [89] and AE in the treatment of premature labor [168] and in the uterine contractility [169]. In the first case, several fractions and compounds obtained from the PJ led to a dose-dependent decrease of oxytocin signaling (induced by an increase in free calcium concentration), but none was as strong as the PJ. However, the combination of a BEF and a FEF was as effective as the PJ, and the combination had a synergistic effect. The PJ inhibited oxytocin-driven activation, and this effect was comparable to that of the Atosiban oxytocin-receptor antagonist and tocolytic agent. In the second case, the AE showed to be as effective as beta-agonists, but significantly better tolerated. The antioxidant activity of 34 juices of species of the Kalanchoe genus were also compared, and the species K. scapigera and K. rhombopilosa showed the highest antioxidant activity (1981 mg/L and 1911 mg/L, respectively) [170]. A market product from PJ of K. pinnata was tested in prospective-observational studies in pregnancy [171], in patients with cancer and suffering from sleep problems [172], and the results suggested that these tablets can be a suitable treatment in both conditions.
The anticonvulsant activity from the ME of roots and stems of K. pinnata decreased with increased doses of the ME of roots, whereas the effect of the ME of stems was dose-dependent (it increased with higher doses) and this effect was preserved when the mixture of chloroform and ethyl acetate were tested. The dose of 400 mg/kg of the ME significantly improved the memory and learning of mice [62,80]. A study utilizing a larval zebrafish model was conducted to assess the potential of the AE obtained from K. pinnata leaves; the results indicated that the AE exhibited both anxiolytic and psychoactive effects, in a dose-dependent manner [173]. The findings of this study contribute to a deeper understanding of the underlying mechanisms responsible for these behavioral effects, thereby providing valuable insights that support the safe and effective utilization of AE in the treatment of mood disorders.
There are few studies about the isolation and characterization of bioactive molecules from Kalanchoe species correlated to their pharmacological potential. Detailed information regarding the studies reported in the literature can be observed in Table 7.
Table 7.
Biological activities of compounds isolated from Kalanchoe species.
| Species Plant Part |
Compound Tested | Pharmacological Activity | Results | Mechanisms of Action | References |
|---|---|---|---|---|---|
|
K. delagoensis Whole plant |
quercetin (40) (6S,7R,8R,9S)-6-oxaspiro-7,8-dihydroxymegastigman-4-en-3-one (tubiflorone) (85) syringic acid (90) 4-O-ethylgallic acid (98) 3,4-dimethoxyphenol (100) phloroglucinol (101) 3,4-dihydroxyallylbenzene (102) |
Anti-inflammatory Lipopolysaccharide (LPS)-induced nitric oxide (NO) production in RAW264.7 cells |
The compounds demonstrated dose-dependent relationships for LPS-induced NO production. The MTT assay showed high cell viability in the presence of LPS in the culture medium at various concentrations. The results showed that quercetin (40), and 3,4-dihydroxyallylbenzene (102) possessed NO inhibitory activities, whereas (6S,7R,8R,9S)-6-oxaspiro-7,8-dihydroxymegastigman-4-en-3-one (85), syringic acid, and 3,4-dimethoxyphenol (100) exhibited weak activities. | Not reported | [32] |
| kalantubolide A (38) kalantubolide B (39) kalantuboside A (23) kalantuboside B (24) bryotoxin C (1) bersaldegenin-1,3,5-orthoacetate (6) bersaldegenin-1-acetate (7) taurolipid C (84) gallic acid (87) cinnamic acid (97) ferulic acid (86) stigmasterol-O-d-glucoside (107) |
Cytotoxicity In vitro cytotoxicity assay, cell cycle analysis, and apoptosis assay |
Cardenolides (kalantubolide A (38) and kalantubolide B (39)) and bufadienolide glycosides (kalantuboside A (23), kalantuboside B (24), bryotoxin C (1), bersaldegenin-1,3,5-orthoacetate (6), bersaldegenin-1-acetate (7)) showed strong cytotoxicity against four human tumor cell lines (A549, Cal-27, A2058, and HL-60) with IC50 values ranging from 0.01 µM to 10.66 µM. Cardenolides (kalantubolide A (38) and kalantubolide B (39)) also displayed significant cytotoxicity toward HL-60 tumor cell line. In addition, kalantuboside A (23), kalantuboside B (24), bryotoxin C (1), bersaldegenin-1,3,5-orthoacetate (6), and bersaldegenin-1-acetate (7) blocked the cell cycle in the G2/M-phase and induced apoptosis in HL-60 cells. | Not reported | [33] | |
|
K. pinnata Whole plant |
bryophyllin A (1) bryophyllin B (2) bersaldegenin-3-acetate (8) |
Cytotoxicity In vitro cytotoxicity assay |
Bryophyllin A (1), bryophyllin B (2), and bersaldegenin-3-acetate (8) showed potent cytotoxicity effects. | Not reported | [114] |
|
K. pinnata Roots |
KPB-100 (81) KPB-200 (82) |
Antivirus Virus spread inhibition and virus yield reduction assays of vaccinia virus, and viral cytopathic effect inhibition assay of HHV-2-TK-mutant and VYR assay of HHV-1 wild type |
Both compounds are promising targets for synthetic optimization and in vivo study against human alpha herpesvirus 1 and 2 and vaccinia virus. KPB-100 (122) strongly inhibited all the tested viruses. | The authors consider that further studies are required to establish the mechanism of action of these compounds. | [69] |
|
K. pinnata Flowers |
quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (45) | Anti-inflammatory Acetic acid-induced abdominal writhing |
The flavonoid (1, 3, and 10 mg/kg) produced a dose-related inhibition of the number of acetic acid-induced writhing by 20.5% (44.2 ± 3.1 w), 35.8% (35.7 ± 4.5 w), and 50.5% (27.5 ± 3.5 w), respectively (ID50 9.4 mg/kg), when compared with the vehicle group (55.6 ± 3.3 w). The positive control indomethacin (10 mg/kg) reduced the number of writhings by 56.5% (24.2 ± 3.5 w). | The aglycone quercetin present in the chemical structure of the isolated compound proved to be an anti-inflammatory and immunosuppressive agent. This flavonol has a well-known immunomodulatory effect through the regulation of inflammatory mediators, such as inhibiting cytokine and inducible nitric oxide synthase expression via inhibition of the NF-κβ pathway. | [8] |
| Anti-inflammatory Carrageenan-induced pleurisy |
The flavonoid (0.3, 1.0, and 3.0 mg/kg) exhibited a dose-related reduction of leukocyte migration by 8.0% (6.9 ± 0.6 leukocytes × 106/mL), 38.8% (4.6 ± 0.2 leukocytes × 106/mL), and 57.2% (3.2 ± 0.3 leukocytes × 106/mL), respectively (ID50 2.0 mg/kg), whereas the treated with dexamethasone (2 mg/kg), positive control group, inhibited by 71.9% (2.1 ± 0.2 leukocytes × 106/mL) when compared with the vehicle-treated group (7.5 ± 0.6 leukocytes × 106/mL). | The reduction in the total leukocyte migration to the pleural cavity induced by carrageenan is dependent on the synthesis/release of the chemoattractant mediators leukotrienes such as LTB4, cytokines IL-1 and TNF-α, and chemokines. | |||
| Anti-inflammatory Croton oil-induced mice ear edema |
Pretreatment with the flavonoid (0.3, 1.0, or 3.0 mg/kg, s.c.) produced a dose-related antiedematogenic effect by 38.2% (=4.2 ± 0.4 mg), 54.4% (=3.1 ± 0.4 mg), and 70.6% (=2.0 ± 0.4 mg), respectively, whereas the treatment with dexamethasone (2 mg/kg) reduced the ear edema by 85.3% (=1.0 ± 0.4 mg) when compared with the vehicle group (=6.8 ± 0.6 mg), with ID50 0.76 mg/kg. | The edema formation is initially mediated by histamine and serotonin and later by the release of prostaglandins. Prostaglandins play an important role in the setting of the cardinal signs of inflammation, pain, heat, redness, edema, and loss of function. The biosynthesis of PGE2, the main inflammatory prostaglandin, involves three key enzymes, phospholipase A2 (PLA2), cyclooxygenase (COX), and PGE synthase (PGES). | |||
| Anti-inflammatory TNF-α ex vivo measurement |
The flavonoid (3.0 mg/kg, s.c.) decreased the TNF-α concentration in pleural exudates by 66.6% (22.6 ± 3.1 pg/mL) when compared to the vehicle group (67.5 ± 4.9 pg/mL), whereas dexamethasone (2 mg/kg, s.c.) reduced the TNF-α concentration by 74.5% (17.2 ± 3.2 pg/mL). | Pretreatment reduced the TNF-α concentration in pleural exudates, suggesting that they produce an anti-inflammatory effect, at least in part, by TNF-α inhibition. | |||
| Anti-inflammatory In vitro cyclooxygenase (COX) inhibition assay |
The flavonoid inhibited both COX-1 and COX-2 in vitro activities (COX-1 IC50 = 3.8 × 10−5 M (22.1 μg/mL) and COX-2 IC50 ≥ 8.4 × 10−5 M). The selectivity index was <0.44. The positive control indomethacin also inhibited both COX-1 and COX-2 activities (IC50 for COX-1 and COX-2 was 5.9 and 31.2 μg/mL, resp., and SI was 0.19). | Some flavonoids may reduce PGE2 synthesis by inhibiting the activity of these enzymes or by inhibiting the expression of the inflammatory-induced enzymes, COX-2, or microsomal PGES-1. | |||
|
K. pinnata Leaves |
quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (45) | Wound healing In vivo rat excision model |
A cream containing quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-L rhamnopyranoside (45) (0.15%) was developed and topically compared to a cream containing the aqueous extract. Both creams showed a better re-epithelialization and dense collagen fibers compared to control groups. | Wound healing agents can act in the inflammation, cellular proliferation and/or remodeling phases of wound healing. Classic symptoms of inflammation are caused by the release of prostaglandins, leukotrienes and reactive oxygen and nitrogen species. The strong antioxidant activity and in vivo anti-inflammatory activity exhibited by quercetin 3-O-α-L-arabinopyranosyl-(1→2)-α-L rhamnopyranoside (45) might explain its healing performance, being considered the main responsible for the wound healing activity of this species. | [67] |
| quercetin 3-O-α-l-arabinopyranosyl-(1→2)-O-α- L-rhamnopyranoside (45) kaempferol 3-O-α-l-arabinopyranosyl-(1→2)-O-α-L-rhamnopyranoside (56) |
Antioxidant In vitro DPPH and ABTS assays |
Kaempferol and quercetin derivatives moderately inhibited XO, while only quercetin derivatives displayed average radical scavenging activity, suggesting that quercetin 3-O-α-l-arabinopyranosyl-(1→2)-α-l-rhamnopyranoside (45) can be indicated as a specific marker of this species. | Not reported | [71] | |
| Anti-inflammatory Xanthine oxidase (XO) inhibition assay | |||||
| quercitrin (43) | Antianaphylactic Mouse hypersensitization and antigen challenge, OVA-specific IgE measurement, T cell proliferation, cytokine production, mast cell degranulation in the mesentery, and histamine release assay. |
Pretreatment with the flavonoid quercitrin (43) showed protective effects in death caused by anaphylactic shock. In this study, the treatment conferred resistance to fatal anaphylactic shock in 75% of the animals. | The mechanism by which quercitrin acts its still unknown. | [157] | |
| Anti-inflammatory Mast cell activation in vitro and allergic airway disease model in vivo |
Treatment with quercitrin (43) did not affect the tested parameters. | [68] | |||
| Antileishmanial In vitro antiamastigote and antipromastigote acitivity assays |
Antiamastigote activity-guided fractionation of ethyl acetate fraction led to the isolation of quercitrin (43), which inhibited 93.9% of amastigote growth (100 µg/mL (223 µM). The compound exhibited significant antileishmanial activity. | [130] | |||
| bryophyllin A (1) bryophyllin C (3) |
Insecticidal Third instar larvae of silkworm bioassay |
Bryophyllin A (1) and bryophyllin C (3) showed strong insecticidal activity against third instar larvae of the silkworm (Bombyx mori). | The authors suggest that the 1,3,5-orthoacetate moiety played an important role in exhibiting the insecticidal activity. | [112] | |
| bryophyllin A (1) bryophyllin B (2) bryophyllin C (3) |
Antivirus Tumor promoter-induced Epstein-Barr virus (EBV) activation assay |
Bryophyllin A (1), bersaldegenin 1,3,5-orthoacetate (6) and daigremontianin (4) showed good inhibitory potential on the Epstein-Barr virus, but bryophyllin A (1) was the most effective (IC50: 0.4 µM). These results strongly suggest that bufadienolides are potential cancer chemopreventive agents. | Tumor promoters possibly induce EBV activation through the activation of protein kinase C and mitogen-activated protein kinase. | [174] | |
|
K. × houghtonni
Leaves |
daigremontianin (4) bersaldegenin 1,3,5-orthoacetate (6) |
3. Methodology
This literature review used published scientific materials collected from the PubMed® and SciFinder® databases without restriction regarding the year of publication and includes literature published through April of 2023. The search term used was “Kalanchoe”. The chemical names agree with the original references.
4. Conclusions and Future Perspectives
This review describes the popular uses, anatomical, and biological aspects of the Kalanchoe species, a plant genus widely prescribed in folk medicine and popularly known as the “miracle leaf”. Even though the Kalanchoe genus has 133 accepted species names, only 19 species with popular uses have been described in the literature; 16 species have received botanical and pharmacological evaluation and only 6 species have received some chemical research in relation to isolated compounds. The species are mainly used in folk medicine to treat wounds, cancer, diabetes, infections, and inflammation. However, in the pharmacological evaluation, these species were not always studied in these models. Of the four species with the highest incidence of popular medicinal use, only K. pinnata was tested in relation to cutaneous wounds and the re-epithelialization process, and diabetes. The others (K. crenata, K. laciniata, and K. daigremontiana) have not yet been studied, but are popularly reported with these uses. Kalanchoe crenata, for example, has only been evaluated for cytotoxicity so far, but is often recommended for wound treatment as well as for diabetes, infections, and inflammation. All parts of the plant are utilized but the juice or crude extract are most widely used. The most utilized species are K. pinnata, K. crenata, K. laciniata, and K. daigremontiana. The literature does not describe which parts of the plant or methods of preparation are popularly recommended for medicinal use in relation to K. × houghtonii, K. flammea, K. gastonis-bonnieri, and K. integra. Several species have structural similarities, although few of them have macroscopic or microscopic information described in the literature. Further studies are necessary to differentiate the species. One hundred and twenty-three compounds were isolated from the Kalanchoe genus, mainly phenols, cardiac glycosides, and triterpenes. Most of the compounds were isolated from K. daigremontiana, K. pinnata, K. delagoensis, and K. ceratophylla. Pharmacological studies have validated antioxidant, anti-inflammatory, cytotoxic, and antimicrobial activities, some of which are related to ethnopharmacological uses. Of the sixteen studied species four are not reported in the literature regarding their popular uses; however, they have been tested regarding pharmacological activities (K. blossfeldiana, K. longiflora, K. scapigera, and K. rhombopilosa). More in vivo studies should be conducted to obtain information about the bioavailability of the chemical compounds present in the extracts, and to propose active doses of these extracts that could be used in vivo to promote the expected biological activities. These experiments could also help to determine the toxicity of these doses, and the possible adverse effects that might be related to these bioactive compounds. Analytical experiments to standardize the extracts and identify possible chemical markers that could be used for quality control are also required. Finally, the authors consider that pharmacological studies dealing with yet unexplored areas should be encouraged to increase other possible medicinal uses of the extracts of these species of Kalanchoe.
Acknowledgments
The authors are grateful to the State University of Ponta Grossa and University of North Carolina Wilmington for the partnership.
Author Contributions
Data curation, E.A.d.A. and I.M.; original draft preparation, E.A.d.A.; tables preparation, E.A.d.A., I.M., A.C.T.V. and S.A.B.; chemical structures preparation, E.A.d.A. and S.A.B.; review and editing, A.V.P., F.L.B., W.K.S. and R.T.W.; supervision and project administration, F.L.B., W.K.S. and R.T.W. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Sample Availability
Not applicable.
Funding Statement
The scholarship of E.A.A. was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (88881.689971/2022-01).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.POWO Crassulaceae. Plants of the World Online. Facilitated by the Royal Botanic Gardens, Kew. Published on the Internet. 2023. [(accessed on 6 April 2023)]. Available online: https://powo.science.kew.org/taxon/urn:lsid:ipni.org:names:30000887-2.
- 2.Fernandes J.M., Cunha L.M., Azevedo E.P., Lourenco E.M.G., Fernandes-Pedrosa M.F., Zucolotto S.M. Kalanchoe laciniata and Bryophyllum pinnatum: An updated review about ethnopharmacology, phytochemistry, pharmacology and toxicology. Rev. Bras. Farmacogn. 2019;29:529–558. doi: 10.1016/j.bjp.2019.01.012. [DOI] [Google Scholar]
- 3.Smith G.F., Figueiredo E., Wyk A.E. Chapter 4-The Genus Kalanchoe (Crassulaceae) in Southern Africa. Academic Press; Cambridge, MA, USA: 2019. pp. 23–28. [DOI] [Google Scholar]
- 4.GBIF Crassulaceae. The Global Biodiversity Information Facility. Published on the Internet. 2023. [(accessed on 15 June 2023)]. Available online: https://www.gbif.org/species/2406.
- 5.POWO Kalanchoe. Plants of the World Online. Facilitated by the Royal Botanic Gardens, Kew. Published on the Internet. 2023. [(accessed on 6 April 2023)]. Available online: https://powo.science.kew.org/taxon/urn:lsid:ipni.org:names:30060186-2.
- 6.Akulova-Barlow Z. Kalanchoe. Cactus Succul. J. 2009;81:268–276. doi: 10.2985/015.081.0601. [DOI] [Google Scholar]
- 7.GBIF Kalanchoe. The Global Biodiversity Information Facility. Published on the Internet. 2023. [(accessed on 15 June 2023)]. Available online: https://www.gbif.org/species/2985928.
- 8.Ferreira R.T., Coutinho M.A., Malvar D.C., Costa E.A., Florentino I.F., Costa S.S., Vanderlinde F.A. Mechanisms Underlying the Antinociceptive, Antiedematogenic, and Anti-Inflammatory Activity of the Main Flavonoid from Kalanchoe pinnata. Evid. Based. Complement. Altern. Med. 2014;2014:429256. doi: 10.1155/2014/429256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mawla F., Khatoon S., Rehana F., Jahan S., Shelley M.R., Hossain S., Haq W.M., Rahman S., Debnath K., Rahmatullah M. Ethnomedicinal plants of folk medicinal practitioners in four villages of Natore and Rajshahi districts, Bangladesh. Am.-Eurasian J. Sustain. Agric. 2012;6:406–416. [Google Scholar]
- 10.Molina G.A., Esparzab R., López-Mirandab J.L., Hernández-Martínez A.R., Espana-Sanchez B.L., Elizalde-Pena E.A., Estevez M. Green synthesis of Ag nanoflowers using Kalanchoe daigremontiana extract for enhanced photocatalytic and antibacterial activities. Colloids Surf. B. 2019;180:141–149. doi: 10.1016/j.colsurfb.2019.04.044. [DOI] [PubMed] [Google Scholar]
- 11.Stefanowicz-Hajduk J., Asztemborska M., Krauze-Baranowska M., Godlewska S., Gucwa M., Moniuszko-Szajwaj B., Stochmanl A., Ochocka J.R. Identification of Flavonoids and Bufadienolides and Cytotoxic Effects of Kalanchoe daigremontiana Extracts on Human Cancer Cell Lines. Planta Med. 2020;86:239–246. doi: 10.1055/a-1099-9786. [DOI] [PubMed] [Google Scholar]
- 12.Zawirska-Wojtasiak R., Jankowska B., Piechowska P., Szkudlarz S.M. Vitamin C and aroma composition of fresh leaves from Kalanchoe pinnata and Kalanchoe daigremontiana. Sci. Rep. 2019;9:19786. doi: 10.1038/s41598-019-56359-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okwu D.E., Josiah C. Evaluation of the chemical composition of two Nigerian medicinal plants. Afr. J. Biotechnol. 2006;5:357–361. [Google Scholar]
- 14.Kołodziejczyk-Czepas J., Nowak P., Wachowicz B., Piechocka J., Glowacki R., Moniuszko-Szajwaj B., Stochmal A. Antioxidant efficacy of Kalanchoe daigremontiana bufadienolide-rich fraction in blood plasma in vitro. Pharm. Biol. 2016;54:3182–3188. doi: 10.1080/13880209.2016.1214740. [DOI] [PubMed] [Google Scholar]
- 15.Kołodziejczyk-Czepas J., Stochmal A. Bufadienolides of Kalanchoe species: An overview of chemical structure, biological activity and prospects for pharmacological use. Phytochem. Rev. 2017;16:1155–1171. doi: 10.1007/s11101-017-9525-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lai Z.R., Peng W.H., Ho Y.L., Huang S.C., Huang T.H., Lai S.C., Ku Y.R., Tsai J.C., Wang C.Y., Chang Y.S. Analgesic and anti-inflammatory activities of the methanol extract of Kalanchoe gracilis (L.) DC stem in mice. Am. J. Chin. Med. 2010;38:529–546. doi: 10.1142/S0192415X10008032. [DOI] [PubMed] [Google Scholar]
- 17.Lai Z.R., Ho Y.L., Huang S.C., Huang T.H., Lai S.C., Tsai J.C., Wang C.Y., Huang G.J., Chang Y.S. Antioxidant, Anti-Inflammatory, and Antiproliferative Activities of Kalanchoe gracilis (L.) DC Stem. Am. J. Chin. Med. 2011;39:1275–1290. doi: 10.1142/S0192415X1100955X. [DOI] [PubMed] [Google Scholar]
- 18.Asiedu-Gyekye I.J., Antwi D.A., Awortwe C., N’guessan B.B., Nyarko A.K. Short-term administration of an aqueous extract of Kalanchoe integra var. crenata (Andr.) Cuf leaves produce no major organ damage in Sprague-Dawley rats. J. Ethnopharmacol. 2014;151:891–896. doi: 10.1016/j.jep.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 19.Asiedu-Gyekye I.J., Arhin E., Arthur S.A., N’guessan B.B., Amponsah S.K. Genotoxicity, nitric oxide level modulation and cardio-protective potential of Kalanchoe integra var. crenata (Andr.) cuf leaves in murine models. J. Ethnopharmacol. 2022;283:114640. doi: 10.1016/j.jep.2021.114640. [DOI] [PubMed] [Google Scholar]
- 20.Awortwe C., Manda K.V., Avonto C., Khan I.S., Walker L.A., Boiuc P.J., Rosenkranz B. In vitro evaluation of reversible and time-dependent inhibitory effects of Kalanchoe crenata on CYP2C19 and CYP3A4 activities. Drug Metab. Lett. 2015;9:48–62. doi: 10.2174/1872312809666150119110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia-Perez P., Lozano-Milo E., Landin M., Gallego P.P. From Ethnomedicine to Plant Biotechnology and Machine Learning: The Valorization of the Medicinal Plant Bryophyllum sp. Pharmaceuticals. 2020;13:444. doi: 10.3390/ph13120444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamgang R., Foyet A.F., Essame J.L., Ngogang J.Y. Effect of methanolic fraction of Kalanchoe crenata on metabolic parameters in adriamycin-induced renal impairment in rats. Indian J. Pharmacol. 2012;44:566–570. doi: 10.4103/0253-7613.100374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuete V., Fokou F.W., Karaosmanoğlu O., Beng V.P., Sivas H. Cytotoxicity of the methanol extracts of Elephantopus mollis, Kalanchoe crenata and 4 other Cameroonian medicinal plants towards human carcinoma cells. BMC Complement. Altern. Med. 2017;17:280. doi: 10.1186/s12906-017-1793-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mutie F.M., Mbuni Y.M., Rono P.C., Mkala E.M., Nzei J.M., Phumthum M., Hu G.-W., Wang Q.-F. Important Medicinal and Food Taxa (Orders and Families) in Kenya, Based on Three Quantitative Approaches. Plants. 2023;12:1145. doi: 10.3390/plants12051145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngezahayo J., Havyarimana F., Hari L., Stévigny C., Duez P. Medicinal plants used by Burundian traditional healers for the treatment of microbial diseases. J. Ethnopharmacol. 2015;173:338–351. doi: 10.1016/j.jep.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 26.Odukoya J.O., Odukoya J.O., Mmutlane E.M., Ndinteh D.T. Ethnopharmacological Study of Medicinal Plants Used for the Treatment of Cardiovascular Diseases and Their Associated Risk Factors insub-Saharan Africa. Plants. 2022;11:1387. doi: 10.3390/plants11101387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raadts E. The Genus Kalanchoe (Crassulaceae) in Tropical East Africa. Willdenowia. 1997;8:101–157. [Google Scholar]
- 28.Akentieva N.P., Shushanov S.S., Gizatullin A.R., Prikhodchenko T.R., Prikhodchenko T.R., Shkondina N.I., D’agaro E. The Effect of Plant Extracts Kalanchoe daigremontiana and Aloe arborescens on the Metabolism of Human Multiple Myeloma Cells. Biointerface Res. Appl. Chem. 2021;11:13171–13186. doi: 10.33263/BRIAC115.1317113186. [DOI] [Google Scholar]
- 29.Chernetskyy M., Woźniak A., Skalska-Kamińska A., Żuraw B., Blicharska E., Rejdak R., Donica H., Weryszko-Chmielewska E. Structure Of Leaves And Phenolic Acids in Kalanchoe daigremontiana Raym.-Hamet & H. Perrier. Acta Sci. Pol. Hortorum Cultus. 2018;17:137–155. doi: 10.24326/asphc.2018.4.13. [DOI] [Google Scholar]
- 30.Moniuszko-Szajwaj B., Pecio L., Kowalczyk M., Stochmal A. New Bufadienolides Isolated from the Roots of Kalanchoe daigremontiana (Crassulaceae) Molecules. 2016;21:243. doi: 10.3390/molecules21030243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsieh Y.J., Yang M.Y., Leu I.Y., Chen C., Wan C.F., Chang M.Y., Chang C.J. Kalanchoe tubiflora extract inhibits cell proliferation by affecting the mitotic apparatus. BMC Complement. Altern. Med. 2012;12:149. doi: 10.1186/1472-6882-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang H.C., Huang G.J., Liaw C.C., Yang C.S., Yang C.P., Kuo C.L., Tseng Y.H., Wang S.Y., Chang W.T., Kuo Y.H. A new megastigmane from Kalanchoe tubiflora (Harvey) Hamet. Phytochem. Lett. 2013;6:379–382. doi: 10.1016/j.phytol.2013.04.002. [DOI] [Google Scholar]
- 33.Huang H.C., Lin M.K., Yang H.L., Hseu Y.C., Liaw C.C., Tseng Y.H., Tsuzuki M., Kuo Y.H. Cardenolides and bufadienolide glycosides from Kalanchoe tubiflora and evaluation of cytotoxicity. Planta Med. 2013;79:1362–1369. doi: 10.1055/s-0033-1350646. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt C., Fronza M., Goettert M., Geller F., Luik S., Flores E.M.M., Bittencourt C.F., Zanetti G.D., Heinzmann B.M., Laufer S., et al. Biological studies on Brazilian plants used in wound healing. J. Ethnopharmacol. 2009;122:523–532. doi: 10.1016/j.jep.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 35.Getachew M., Belayneh A., Kebede B., Alimaw Y., Biyazin Y., Abebaw A., Abebe D. Medicinal plants used for management of hemorrhoids in Ethiopia: A systematic review. Heliyon. 2022;8:e10211. doi: 10.1016/j.heliyon.2022.e10211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arias-González I., García-Carrancá A.M., Cornejo-Garrido J., Ordaz-Pichardo C. Cytotoxic effect of Kalanchoe flammea and induction of intrinsic mitochondrial apoptotic signaling in prostate cancer cells. J. Ethnopharmacol. 2018;222:133–147. doi: 10.1016/j.jep.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 37.Richwagen N., James T.L., Brandon L.F.D., Quave C.L. Antibacterial activity of Kalanchoe mortagei and K. fedtschenkoi against ESKAPE pathogens. Front. Pharmacol. 2019;10:67. doi: 10.3389/fphar.2019.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palumbo A., Casanova L.M., Corrêa M.F.P., Da Costa N.M., Nasciutti L.E., Costa S.S. Potential therapeutic effects of underground parts of Kalanchoe gastonis-bonnieri on benign prostatic hyperplasia. Evid. Based Complement. Altern. Med. 2019;2019:6340757. doi: 10.1155/2019/6340757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frimpong-Manso S., Asiedu-Gyekye I.J., Naadu J.P., Magnus-Aryitey G.T., Nyarko A.K., Boamah D., Awan M. Micro and macro element composition of Kalanchoe integra leaves: An adjuvant treatment for hypertension in Ghana. Int. J. Hypertens. 2015;2015 doi: 10.1155/2015/579497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Costa A.C.O., Fernandes J.M., Negreiros Neto T.S., Mendonça J.N., Tomaz J.C., Lopes N.P., Soares L.A.L., Zucolotto S.M. Quantification of Chemical Marker of Kalanchoe brasiliensis (Crassulaceae) Leaves by HPLC-DAD. J. Liq. Chromatogr. Relat. Technol. 2015;38:795–800. doi: 10.1080/10826076.2014.971370. [DOI] [Google Scholar]
- 41.Cruz B.P., Chedier L.M., Fabri R.L., Pimenta D.S. Chemical and agronomic development of Kalanchoe brasiliensis Camb. and Kalanchoe pinnata (Lamk.) Pers under light and temperature levels. An. Acad. Bras. Ciências. 2011;83:1435–1441. doi: 10.1590/S0001-37652011000400030. [DOI] [PubMed] [Google Scholar]
- 42.Cruz B.P., Chedier L.M., Peixoto P.H.P., Fabri R.L., Pimenta D.S. Effects of light intensity on the distribution of anthocyanins in Kalanchoe brasiliensis Camb. and Kalanchoe pinnata (Lamk.) Pers. An. Acad. Bras. Ciências. 2012;84:211–217. doi: 10.1590/S0001-37652012005000014. [DOI] [PubMed] [Google Scholar]
- 43.de Araujo E.R.D., Guerra G.C.B., Araújo D.F.S., de Araújo A.A., Fernandes J.M., De Araujo Junior R.F., De Carvalho T.G., Ferreira L.S., Zucolotto S.M. Gastroprotective and antioxidant activity of Kalanchoe brasiliensis and Kalanchoe pinnata leaf juices against indomethacin and ethanol- 45 induced gastric lesions in rats. Int. J. Mol. Sci. 2018;19:1265. doi: 10.3390/ijms19051265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fernandes J.M., Félix-Silva J., da Cunha L.M., Gomes J.A., Siqueira E.M.S., Gimenes L.P., Lopes N.P., Soares L.A.L., Fernandes-Pedrosa M.F., Zucolotto S.M. Inhibitory Effects of Hydroethanolic Leaf Extracts of Kalanchoe brasiliensis and Kalanchoe pinnata (Crassulaceae) against Local Effects Induced by Bothrops jararaca Snake Venom. PLoS ONE. 2016;11:e0168658. doi: 10.1371/journal.pone.0168658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fonseca A.G., Ribeiro Dantas L.L.S.F., Fernandes J.M., Zucolotto S.M., Neves Lima A.A., Soares L.A.L., Rocha H.A.O., Lemos T.M.A.M. In Vivo and In Vitro Toxicity Evaluation of Hydroethanolic Extract of Kalanchoe brasiliensis (Crassulaceae) Leaves. J. Toxicol. 2018;2018:6849765. doi: 10.1155/2018/6849765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haile A.A., Tsegay B.A., Seid A., Adnew W., Moges A. A Review on Medicinal Plants Used in the Management of Respiratory Problems in Ethiopia over a Twenty-Year Period (2000–2021) Evid. Based Complement. Alternat Med. 2022;2022:2935015. doi: 10.1155/2022/2935015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Manan M., Hussain L., Ijaz H., Qadir M.I. Phytochemical screening of different extracts of Kalanchoe laciniata. Pak. J. Pharm. Sci. 2015;29:1321–1324. doi: 10.22200/pjpr.2015258-61. [DOI] [PubMed] [Google Scholar]
- 48.Sharif A., Akhtar M.F., Akhtar B., Saleem A., Manan M., Shabbir M., Ashraf M., Peerzada S., Ahmed S., Raza M. Genotoxic and Cytotoxic Potential Of Whole Plant Extracts Of Kalanchoe Laciniata By Ames And Mtt Assay. EXCLI J. 2017;16:593–601. doi: 10.17179/excli2016-748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stefanowicz-Hajduk J., Hering A., Gucwa M., Hałasa R., Soluch A., Kowalczyk M., Stochmal A., Ochocka R. Biological activities of leaf extracts from selected Kalanchoe species and their relationship with bufadienolides content. Pharm. Biol. 2020;58:732–740. doi: 10.1080/13880209.2020.1795208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bogale M., Sasikumar J.M., Egigu M.C. An ethnomedicinal study in tulo district, west hararghe zone, oromia region, Ethiopia. Heliyon. 2023;9:e15361. doi: 10.1016/j.heliyon.2023.e15361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singab A.B., El-Ahmady S.H., Labib R.M., Fekry S.S. Phenolics from Kalanchoe marmorata Baker, Family Crassulaceae. Bull. Fac. Pharm. Cairo. Univ. 2011;49:1–5. doi: 10.1016/j.bfopcu.2011.07.001. [DOI] [Google Scholar]
- 52.Tahir M., Asnake H., Beyene T., Van Damme P., Mohammed A. Ethnobotanical study of medicinal plants in Asagirt District, Northeastern Ethiopia. Trop. Med. Health. 2023;51:1. doi: 10.1186/s41182-023-00493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abebe W. An overview of Ethiopian traditional medicinal plants used for cancer treatment. Eur. J. Med. Plants. 2016;14:1–16. doi: 10.9734/EJMP/2016/25670. [DOI] [Google Scholar]
- 54.Agize M., Asfaw Z., Nemomissa S., Gebre T. Ethnobotany of traditional medicinal plants and associated indigenous knowledge in Dawuro Zone of Southwestern Ethiopia. J. Ethnobiol. Ethnomedicine. 2022;18:48. doi: 10.1186/s13002-022-00546-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mekonnen A.B., Mohammed A.S., Tefera A.K. Ethnobotanical Study of Traditional Medicinal Plants Used to Treat Human and Animal Diseases in Sedie Muja District, South Gondar, Ethiopia. Evid.-Based Complement. Altern. Med. 2022;2022:7328613. doi: 10.1155/2022/7328613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tadesse T.Y., Zeleke M.M., Dagnew S.B. Review of Ethnobotanical and Ethnopharmacological Evidence of Some Ethiopian Medicinal Plants Traditionally Used for Peptic Ulcer Disease Treatment. Clin. Exp. Gastroenterol. 2022;15:171–187. doi: 10.2147/CEG.S384395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahmed M.N., Hughes K. Role of ethno-phytomedicine knowledge in healthcare of COVID-19: Advances in traditional phytomedicine perspective. Beni-Suef Univ. J. Basic. Appl. Sci. 2022;11:96. doi: 10.1186/s43088-022-00277-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ahmed M., Wazir Z.U., Khan R.A., Khan M.I., Waqas S., Iqbal A. Pharmacological evaluation of crude methanolic extract of Kalanchoe pinnata leaves. Environ. Toxicol. Chem. 2013;95:1539–1545. doi: 10.1080/02772248.2013.846569. [DOI] [Google Scholar]
- 59.Anadozie S.O., Akinyemi J.A., Agunbiade S., Ajiboyeet B.O., Adewale O.B. Bryophyllum pinnatum inhibits arginase II activity and prevents oxidative damage occasioned by carbon tetrachloride (CCl4) in rats. Biomed. Pharmacother. 2018;101:8–13. doi: 10.1016/j.biopha.2018.01.156. [DOI] [PubMed] [Google Scholar]
- 60.Bachmann S., Betschart C., Gerber J., Fürer K., Mennet M., Hamburger M., Potterat O., Von Mandach U., Simões-Wüst A.P. Potential of Bryophyllum pinnatum as a detrusor relaxant: An in vitro exploratory study. Planta Med. 2017;83:1274–1280. doi: 10.1055/s-0043-109097. [DOI] [PubMed] [Google Scholar]
- 61.Barbhuiya P.A., Laskar A.M., Mazumdar H., Dutta P., Pathak M.P., Dey B.K., Sen S. Ethnomedicinal Practices and Traditional Medicinal Plants of Barak Valley, Assam: A systematic review. J. Pharmacopunct. 2022;25:149–185. doi: 10.3831/KPI.2022.25.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bhandari R., Gyawali S., Aryal N., Gaire D., Paudyal K., Panta A., Panth P., Joshi D.R., Rokaya R.K., Aryal P., et al. Evaluation of phytochemical, antioxidant, and memory-enhancing activity of Garuga pinnata Roxb. Bark and Bryophyllum pinnatum (Lam) Oken. leaves. Sci. World J. 2021;2021:6649574. doi: 10.1155/2021/6649574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bhatti M., Kamboj A., Saluja A.K., Jain U.K. In vitro evaluation and comparison of antioxidant activities of various extracts of leaves and stems of Kalanchoe pinnatum. Int. J. Green Pharm. 2012;6:340–347. doi: 10.4103/0973-8258.108255. [DOI] [Google Scholar]
- 64.Bhavsar S., Chandel D. Cytotoxic and genotoxic effects of Kalanchoe pinnata (Lam.) Pers. fresh leaf juice in the cultured human blood lymphocytes. Drug Chem. Toxicol. 2019;45:360–366. doi: 10.1080/01480545.2019.1696814. [DOI] [PubMed] [Google Scholar]
- 65.Bopda O.S.M., Longo F., Bella T.N., Edzah P.M.O., Taiwe G.S., Bilada D.C., Tom E.N.L., Kamtchouing P., Dimo T. Antihypertensive activities of the aqueous extract of Kalanchoe pinnata (Crassulaceae) in high salt-loaded rats. J. Ethnopharmacol. 2014;153:400–407. doi: 10.1016/j.jep.2014.02.041. [DOI] [PubMed] [Google Scholar]
- 66.Clemen-Pascual L.M., Macahig R.A.S., Rojas N.R.L. Comparative toxicity, phytochemistry, and use of 53 Philippine medicinal plants. Toxicol. Rep. 2021;9:22–35. doi: 10.1016/j.toxrep.2021.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Coutinho M.A.S., Casanova L.M., Nascimento L.B.D.S., Leal D., Palmero C., Toma H.K., Santos E.P., Nasciutti L.E., Costa S.S. Wound healing cream formulated with Kalanchoe pinnata major flavonoid is as effective as the aqueous leaf extract cream in a rat model of excisional wound. Nat. Prod. Res. 2020;35:6034–6039. doi: 10.1080/14786419.2020.1817012. [DOI] [PubMed] [Google Scholar]
- 68.Cruz E.A., Reuter H., Martin N., Dehzad N., Muzitano M.F., Costa S.S., Rossi-Bergmann B., Buhl R., Stassen M., Taube C. Kalanchoe pinnata inhibits mast cell activation and prevents allergic airway disease. Phytomedicine. 2012;19:115–121. doi: 10.1016/j.phymed.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 69.Cryer M., Lane K., Greer M., Cates R., Burt S., Andrus M., Zou J., Rogers P., Hansen M.D.H., Burgado J., et al. Isolation and identification of compounds from Kalanchoe pinnata having human alphaherpesvirus and vaccinia virus antiviral activity. Pharm. Biol. 2017;55:1586–1591. doi: 10.1080/13880209.2017.1310907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.El Abdellaoui S., Destandau E., Toribio A., Elfakir C., Lafosse M., Renimel I., André P., Cancellieri P., Landemarre L. Bioactive molecules in Kalanchoe pinnata leaves: Extraction, purification, and identification. Anal. Bioanal. Chem. 2010;398:1329–1338. doi: 10.1007/s00216-010-4047-3. [DOI] [PubMed] [Google Scholar]
- 71.Fernandes J.M., Ortiz S., Tavares R.P.M., Mandova T., Araújo E.R., Andrade A.W.L., Michel S., Grougnet R., Zucolotto S.M. Bryophyllum pinnatum markers: CPC isolation, simultaneous quantification by a validated UPLC-DAD method and biological evaluations. J. Pharm. Biomed. Anal. 2021;193:113682. doi: 10.1016/j.jpba.2020.113682. [DOI] [PubMed] [Google Scholar]
- 72.Furer K., Simões-Wüst A.P., von Mandach U., Hamburger M., Potterat O. Bryophyllum pinnatum and Related Species Used in Anthroposophic Medicine: Constituents, Pharmacological Activities, and Clinical Efficacy. Planta Med. 2016;82:930–941. doi: 10.1055/s-0042-106727. [DOI] [PubMed] [Google Scholar]
- 73.Gomes D.C.O., Muzitano M.F., Costa S.S., Rossi-Bergmann B. Effectiveness of the immunomodulatory extract of Kalanchoe pinnata against murine visceral leishmaniasis. Parasitology. 2010;137:613–618. doi: 10.1017/S0031182009991405. [DOI] [PubMed] [Google Scholar]
- 74.Kadam S., Madhusoodhanan V., Bandgar A., Kaushik K.S. From Treatise to Test: Evaluating Traditional Remedies for Anti-Biofilm Potential. Front. Pharmacol. 2020;11:566334. doi: 10.3389/fphar.2020.566334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kukuia K.E.K., Asiedu-Gyekye I.J., Woode E., Biney R.P., Addae E. Phytotherapy of experimental depression: Kalanchoe integra var. crenata (Andr.) Cuf leaf extract. J. Pharm. Bioallied. Sci. 2015;7:26–31. doi: 10.4103/0975-7406.148785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leal-Costa M.V., Nascimento L.B.S., Moreira N.S., Reinert F., Costa S.S., Salgueiro Lage C.L., Tavares E.S. Influence of Blue Light on the Leaf Morphoanatomy of In Vitro Kalanchoe pinnata (Lamarck) Persoon (Crassulaceae) Microsc. Microanal. 2010;16:576–582. doi: 10.1017/S1431927610000279. [DOI] [PubMed] [Google Scholar]
- 77.Lebedeva A.A., Zakharchenko N.S., Trubnikova E.V., Medvedeva O.A., Kuznetsova T.V., Masgutova G.A., Zylkova M.V., Buryanov Y.I., Belous A.S. Bactericide, Immunomodulating, and Wound Healing Properties of Transgenic Kalanchoe pinnata Synergize with Antimicrobial Peptide Cecropin P1 In Vivo. J. Immunol. Res. 2017;2017:4645701. doi: 10.1155/2017/4645701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Majaz A.Q., Khurshid M., Nazim S. The Miracle Plant (Kalanchoe pinnata): A Phytochemical and Pharmacological Review. Int. J. Res. Ayurveda Pharm. 2011;2:1478–1482. [Google Scholar]
- 79.Majaz A.Q., Nazim S., Afsar S., Siraj S., Siddik P.M. Evaluation of Antimicrobial activity of Roots of K. pinnata. Int. J. Pharmacol. Bio. Sci. 2011;5:93–96. [Google Scholar]
- 80.Mora-Pérez A., Hernández-Medel M.D.R. Anticonvulsant activity of methanolic extract from Kalanchoe pinnata (Lam.) stems and roots in mice: A comparison to diazepam. Neurología. 2016;31:161–168. doi: 10.1016/j.nrl.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 81.Mourão R.H.V., Santos F.O., Franzotti E.M., Moreno M.P.N., Antoniolli A.R. Antiinflammatory Activity and Acute Toxicity (LD50) of the Juice of Kalanchoe brasiliensis (Comb.) Leaves Picked Before and During Blooming. Phytother. Res. 1999;13:352–354. doi: 10.1002/(SICI)1099-1573(199906)13:4<352::AID-PTR452>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 82.Muzitano M.F., Bergonzi M.C., De Melo G.O., Lage C.L.S., Bilia A.R., Vincieri F.F., Rossi-Bergmann B., Costa S.S. Influence of cultivation conditions, season of collection and extraction method on the content of antileishmanial flavonoids from Kalanchoe pinnata. J. Ethnopharmacol. 2011;133:132–137. doi: 10.1016/j.jep.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 83.Nascimento L.B.S., Leal-Costa M.V., Coutinho M.A.S., Moreira N.S., Lage C.L.S., Barbi N.S., Costa S.S., Tavares E.S. Increased antioxidant activity and changes in phenolic profile of Kalanchoe pinnata (Lamarck) Persoon (Crassulaceae) specimens grown under supplemental blue light. Photochem. Photobiol. 2013;89:391–399. doi: 10.1111/php.12006. [DOI] [PubMed] [Google Scholar]
- 84.Nascimento L.B.S., Leal-Costa M.V., Menezes E.A., Lopes V.R., Muzitano M.F., Costa S.S., Tavares E.S. Ultraviolet-B radiation effects on phenolic profile and flavonoid content of Kalanchoe pinnata. J. Photochem. Photobiol. B Biol. 2015;148:73–81. doi: 10.1016/j.jphotobiol.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 85.Nascimento L.B.S., Aguiar P.F., Leal-Costa M.V., Coutinho M.A.S., Borsoldi M.P.G., Rossi-Bergmann B., Tavares E.S., Costa S.S. Optimization of Aqueous Extraction from Kalanchoe pinnata Leaves to Obtain the Highest Content of an Anti-inflammatory Flavonoid Using a Response Surface Model. Phytochem. Anal. 2018;29:308–315. doi: 10.1002/pca.2744. [DOI] [PubMed] [Google Scholar]
- 86.Oufir M., Seiler C., Gerodetti M., Gerber J., Fürer K., Mennet-von Eiff M., Elsas S.M., Brenneisen R., von Mandach U., Hamburger M., et al. Quantification of bufadienolides in Bryophyllum pinnatum leaves and manufactured products by UHPLC-ESIMS/MS. Planta Med. 2015;81:1190–1197. doi: 10.1055/s-0035-1546126. [DOI] [PubMed] [Google Scholar]
- 87.Patil S.B., Dongare V.R., Kulkarni C.R., Joglekar M.M., Arvindekar A.U. Antidiabetic activity of Kalanchoe pinnata in streptozotocin-induced diabetic rats by glucose independent insulin secretagogue action. Pharm. Biol. 2013;51:1411–1418. doi: 10.3109/13880209.2013.794364. [DOI] [PubMed] [Google Scholar]
- 88.Paul A., Chakraborty N., Sarkar A., Acharya K., Ranjan A., Chauhan A., Srivastava S., Singh A.K., Rai A.K., Mubeen I., et al. Ethnopharmacological Potential of Phytochemicals and Phytogenic Products against Human RNA Viral Diseases as Preventive Therapeutics. BioMed Res. Int. 2013;2023:1977602. doi: 10.1155/2023/1977602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Santos S., Zurfluh L., Mennet M., Potterat O., von Mandach U., Hamburger M., Simoes-Wust A.P. Bryophyllum pinnatum Compounds Inhibit Oxytocin-Induced Signaling Pathways in Human Myometrial Cells. Front. Pharmacol. 2021;12:632986. doi: 10.3389/fphar.2021.632986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yuliani T., Dewijanti I.D., Banjarnahor S.D.S. Antidiabetic activity of ethanolic extracts of Kalanchoe pinnata leaves in alloxan induced hyperglycemic rats. Indones. J. Pharm. 2016;27:139–144. doi: 10.14499/indonesianjpharm27iss3pp139. [DOI] [Google Scholar]
- 91.Zakharchenko N.S., Lebedeva A.A., Furs O.V., Rukavtsova E.B., Schevchuk T.V., Rodionov I.L., Bur’yanov Y.I. Producing Marker-Free Kalanchoe Plants Expressing Antimicrobial Peptide Cecropin P1 Gene. Russ. J. Plant Physiol. 2016;63:273–282. doi: 10.1134/S1021443716020163. [DOI] [Google Scholar]
- 92.Zakharchenko N.S., Rukavtsova E.B., Shevchuk T.V., Furs O.V., Pigoleva S.V., Lebedeva A.A., Chulina I.A., Baidakova L.K., Bur’yanov Y.I. The Obtainment and Characteristics of Kalanchoe pinnata L. Plants Expressing the Artificial Gene of the Cecropin P1 Antimicrobial Peptide. Appl. Biochem. Microbiol. 2016;52:421–428. doi: 10.1134/S0003683816040189. [DOI] [PubMed] [Google Scholar]
- 93.Zakharchenko N.S., Belous A.S., Biryukova Y.K., Medvedeva O.A., Belyakova A.V., Masgutova G.A., Trubnikova E.V., Buryanov Y.I., Lebedeva A.A. Immunomodulating and Revascularizing Activity of Kalanchoe pinnata Synergize with Fungicide Activity of Biogenic Peptide Cecropin P1. J. Immunol. Res. 2017;2017:3940743. doi: 10.1155/2017/3940743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kamboj A., Saluja A.K. Bryophyllum pinnatum (Lam.) Kurz: Phytochemical and pharmacological profile: A review. Pharmacogn. Rev. 2009;3:364–375. [Google Scholar]
- 95.Lorenzi H., Matos F.J.A. Plantas Medicinais No Brasil: Nativas Exóticas Cultivadas. 2nd ed. Instituto Plantarum de Estudos da Flora; Nova Odessa, Brazil: 2008. p. 223. [Google Scholar]
- 96.Milad R., El-Ahmady S., Singab A.N. Genus Kalanchoe (Crassulaceae): A Review of Its Ethnomedicinal, Botanical, Chemical and Pharmacological Properties. J. Med. Plants. 2014;4:86–104. doi: 10.9734/EJMP/2014/5901. [DOI] [Google Scholar]
- 97.Herrera I., Hernandez M.J., Lampo M., Nassar J.M. Plantlet recruitment is the key demographic transition in invasion by Kalanchoe daigremontiana. Popul. Ecol. 2011;54:225–237. doi: 10.1007/s10144-011-0282-5. [DOI] [Google Scholar]
- 98.Moreira N.S., Nascimento L.B.S., Leal-Costa M.V., Tavares E.S. Comparative anatomy of leaves of Kalanchoe pinnata and K. crenata in sun and shade conditions, as a support for their identification. Rev. Bras. Farmacogn. 2012;22:929–936. doi: 10.1590/S0102-695X2012005000056. [DOI] [Google Scholar]
- 99.Wild B., Wanek W., Postl W., Richter A. Contribution of carbon fixed by Rubisco and PEPC to phloem export in the Crassulacean acid metabolism plant Kalanchoe daigremontiana. J. Exp. Bot. 2010;61:1375–1383. doi: 10.1093/jxb/erq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yang X., Hu R., Yin H., Jenkins J., Shu S., Tang H., Liu D., Weighill D.A., Yim W.C., Ha J., et al. The Kalanchoë genome provides insights into convergent evolution and building blocks of crassulacean acid metabolism. Nat. Commun. 2017;8:1899. doi: 10.1038/s41467-017-01491-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gotoh E., Oiwamoto K., Inoue S.I., Shimazaki K.I., Doi M. Stomatal response to blue light in crassulacean acid metabolism plants Kalanchoe pinnata and Kalanchoe daigremontiana. J. Exp. Bot. 2019;70:1367–1374. doi: 10.1093/jxb/ery450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Herrando-Moraira S., Vitales D., Nualart N., Gómez-Bellver C., Ibáñez N., Massó S., Cachón-Ferrero P., González-Gutiérrez P.A., Guillot D., Herrera I., et al. Global distribution patterns and niche modelling of the invasive Kalanchoe × houghtonii (Crassulaceae) Sci. Rep. 2020;10:3143. doi: 10.1038/s41598-020-60079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Al-Khayri J.M., Mahdy E.M.B., Taha H.A.S., Eldomiaty A.S., Abd-Elfattah M.A., Latef A.A.H.A., Rezk A.A., Shehata W.F., Almaghasla M.I., Shalaby T.A., et al. Genetic and Morphological Diversity Assessment of Five Kalanchoe Genotypes by SCoT, ISSR and RAPD-PCR Markers. Plants. 2022;11:1722. doi: 10.3390/plants11131722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.García-Sogo B., Pineda B., Castelblanque L., Antón T., Medina M., Roque E., Torresi C., Beltrán J.P., Moreno V., Cañas L.A. Efficient transformation of Kalanchoe blossfeldiana and production of male-sterile plants by engineered anther ablation. Plant Cell Rep. 2009;29:61–77. doi: 10.1007/s00299-009-0798-8. [DOI] [PubMed] [Google Scholar]
- 105.Liu C., Zhu C., Zeng H.M. Key KdSOC1 gene expression profiles during plantlet morphogenesis under hormone, photoperiod, and drought treatments. Genet. Mol. Res. 2016;15:1–14. doi: 10.4238/gmr.15017579. [DOI] [PubMed] [Google Scholar]
- 106.Quintero E.J., De León E.G., Morán-Pinzón J., Mero A., Leon E., Cano L.P.P. Evaluation of the Leaf Extracts of Kalanchoe Pinnata and Kalanchoe Daigremontiana Chemistry, Antioxidant and Anti-inflammatory Activity. Eur. J. Med. Plants. 2021;32:45–54. doi: 10.9734/ejmp/2021/v32i530392. [DOI] [Google Scholar]
- 107.Casanova J.M., Nascimento L.B.S., Casanova L.M., Leal-Costa M.V., Costa S.S., Tavares E.S. Differential Distribution of Flavonoids and Phenolic Acids in Leaves of Kalanchoe delagoensis Ecklon & Zeyher (Crassulaceae) Microsc. Microanal. 2020;26:1061–1068. doi: 10.1017/S1431927620024344. [DOI] [PubMed] [Google Scholar]
- 108.Brzezicka E., Karwowska K., Kozieradzka-Kiszkurno M., Chernetskyy M. Leaf micromorphology of Kalanchoë laciniata (Crassulaceae) Mod. Phytomorphology. 2015;8:49–52. [Google Scholar]
- 109.Bhavsar S., Bhavita D., Maitreyi Z., Divya C. A comparative pharmacognostical and phytochemical analysis of Kalanchoe pinnata (Lam.) Pers. leaf extracts. J. Pharmacogn. Phytochem. 2018;7:1519–1527. [Google Scholar]
- 110.Chernetskyy M., Weryszko-Chmielewska E. Structure of Kalanchoë pumila Bak. leaves (Crassulaceae DC.) Acta Agrobot. 2008;61 doi: 10.5586/aa.2008.029. [DOI] [Google Scholar]
- 111.McKenzie R.A., Franke F.P., Dunster P.J. The toxicity to cattle and bufadienolide content of six Bryophyllum species. Aust. Vet. J. 1987;64:298–301. doi: 10.1111/j.1751-0813.1987.tb07330.x. [DOI] [PubMed] [Google Scholar]
- 112.Supratman U., Fujita T., Akiyama K., Hayashi H. New insecticidal bufadienolide, bryophyllin C, from Kalanchoe pinnata. Biosci. Biotechnol. Biochem. 2000;64:1310–1312. doi: 10.1271/bbb.64.1310. [DOI] [PubMed] [Google Scholar]
- 113.Wu P.L., Hsu Y.L., Wu T.S., Bastow K.F., Lee K.H. Kalanchosides A–C, new cytotoxic bufadienolides from the aerial parts of Kalanchoe gracilis. Org. Lett. 2006;8:5207–5210. doi: 10.1021/ol061873m. [DOI] [PubMed] [Google Scholar]
- 114.Yamagishi T., Haruna M., Yan X.Z., Chang J.J., Lee K.H. Antitumor agents, 110. Bryophyllin B, a novel potent cytotoxic bufadienolide from Bryophyllum pinnatum. J. Nat. Prod. 1989;52:1071–1079. doi: 10.1021/np50065a025. [DOI] [PubMed] [Google Scholar]
- 115.Capon R.J., MacLeod J.K., Oelrichs P.B. Bryotoxins B and C, toxic bufadienolide orthoacetates from the flowers of Bryophyllum tubiflorum (Crassulaceae) Aust. J. Chem. 1986;39:1711–1715. doi: 10.1071/CH9861711. [DOI] [Google Scholar]
- 116.Kołodziejczyk-Czepas J., Pasiński B., Ponczek M.B., Moniuszko-Szajwaj B., Kowalczyk M., Pecio L., Nowak P., Stochmal A. Bufadienolides from Kalanchoe daigremontiana modulate the enzymatic activity of plasmin—In vitro and in silico analyses. Int. J. Biol. Macromol. 2018;120:1591–1600. doi: 10.1016/j.ijbiomac.2018.09.143. [DOI] [PubMed] [Google Scholar]
- 117.Wagner H., Fischer M., Lotter H. Isolation and Structure Determination of Daigremontianin, a Novel Bufadienolide from Kalanchoe daigremontiana. Planta Med. 1985;51:169–170. doi: 10.1055/s-2007-969441. [DOI] [PubMed] [Google Scholar]
- 118.Ürményi F.G., Saraiva G.D., Casanova L.M., Matos A.D., Camargo L.M.M., Romanos M.T.V., Costa S.S. Anti-HSV-1 and HSV-2 flavonoids and a new kaempferol triglycoside from the medicinal plant Kalanchoe daigremontiana. Chem. Biodivers. 2016;13:1707–1714. doi: 10.1002/cbdv.201600127. [DOI] [PubMed] [Google Scholar]
- 119.Anderson L.A.P., Steyn P.S., Heerden F.R. The characterization of two novel bufadienolides, lanceotoxins A and B from Kalanchoe lanceolata [Forssk.] Pers. J. Chem. Soc. Perkin Trans. 1. 1984;15:1573–1575. doi: 10.1039/p19840001573. [DOI] [Google Scholar]
- 120.Kuo P.C., Kuo T.H., Su C.R., Liou M.J., Wu T.S. Cytotoxic principles and α-pyrone ring-opening derivatives of bufadienolides from Kalanchoe hybrida. Tetrahedron. 2018;64:3392–3396. doi: 10.1016/j.tet.2008.01.090. [DOI] [Google Scholar]
- 121.Chibli L.A., Rodrigues K.C.M., Gasparetto C.M., Pinto N.C.C., Fabri R.L., Scio E., Alves M.S., Del-Vechio-Vieira G., Sousa O.V. Anti-inflammatory effects of Bryophyllum pinnatum (Lam.) Oken ethanol extract in acute and chronic cutaneous inflammation. J. Ethnopharmacol. 2014;11:330–338. doi: 10.1016/j.jep.2014.03.035. [DOI] [PubMed] [Google Scholar]
- 122.Coutinho M.A., Muzitano M.F., Cruz E.A., Bergonzi M.C., Kaiser C.R., Tinoco L.W., Bilia A.R., Vincieric F.F., Rossi-Bergmann B., Costa S.S. Flowers from Kalanchoe pinnata are a rich source of T cell-suppressive flavonoids. Nat. Prod. Commun. 2012;7:175–178. doi: 10.1177/1934578X1200700211. [DOI] [PubMed] [Google Scholar]
- 123.Elansary H.O., Abdelgaleil S.A.M., Mahmoud E.A., Yessoufou K., Elhindi K., El-Hendawy S. Effective antioxidant, antimicrobial and anticancer activities of essential oils of horticultural aromatic crops in northern Egypt. BMC Complement. Altern. Med. 2018;18:214. doi: 10.1186/s12906-018-2262-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Elizondo-Luevano J.H., Pérez-Narváez O.A., Sánchez-García E., Castro-Ríos R., Hernández-García M.E., Chávez-Montes A. In Vitro Effect of Kalanchoe daigremontiana and Its Main Component, Quercetin against Entamoeba histolytica and Trichomonas vaginalis. Iran. J. Parasitol. 2021;16:394–401. doi: 10.18502/ijpa.v16i3.7092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hegazy M.M., Metwaly A.M., Mostafa A.E., Radwan M.M., Mehany A.B.M., Ahmed E., Enany S., Magdeldin S., Afifi W.M., ElSohly M.A. Biological and chemical evaluation of some African plants belonging to Kalanchoe species: Antitrypanosomal, cytotoxic, antitopoisomerase I activities and chemical profiling using ultra-performance liquid chromatography/quadrupole-time-of-flight mass spectrometer. Pharmacog. Mag. 2021;17:6–15. [Google Scholar]
- 126.Liu K.C.S., Yang S.L., Roberts M.F., Phillipson J.D. Eupafolin Rhamnosides from Kalanchoe gracilis. J. Nat. Prod. 1986;52:970–974. doi: 10.1021/np50065a009. [DOI] [Google Scholar]
- 127.Nielsen A.H., Olsen C.E., Møller B.L. Flavonoids in flowers of 16 Kalanchoë blossfeldiana varieties. Phytochemistry. 2005;66:2829–2835. doi: 10.1016/j.phytochem.2005.09.041. [DOI] [PubMed] [Google Scholar]
- 128.Sarkar R., Mondal C., Bera R., Chakraborty S., Barik R., Roy P., Kumar A., Yadav K.K., Choudhury J., Chaudhary S.K., et al. Antimicrobial properties of Kalanchoe blossfeldiana: A focus on drug resistance with reference to quorum sensing-mediated bacterial biofilm formation. J. Pharm. Pharmacol. 2015;67:951–962. doi: 10.1111/jphp.12397. [DOI] [PubMed] [Google Scholar]
- 129.Fürer K., Raith M., Brenneisen R., Mennet M., Simões-Wüst A.P., von Mandach U., Hamburger M., Potterat O. Two new flavonol glycosides and a metabolite profile of Bryophyllum pinnatum, a phytotherapeutic used in obstetrics and gynaecology. Planta Med. 2013;79:1565–1571. doi: 10.1055/s-0033-1350808. [DOI] [PubMed] [Google Scholar]
- 130.Muzitano M.F., Cruz E.A., de Almeida A.P., Da Silva S.A., Kaiser C.R., Guette C., Rossi-Bergmann B., Costa S.S. Quercitrin: An antileishmanial flavonoid glycoside from Kalanchoe pinnata. Planta Med. 2006;72:81–83. doi: 10.1055/s-2005-873183. [DOI] [PubMed] [Google Scholar]
- 131.de Araujo E.R.D., Félix-Silva J., Xavier-Santos J.B., Fernandes J.M., Guerra G.C.B., de Araújo A.A., Araújo D.F.S., Ferreira L.S., da Silva Júnior A.A., Fernandes-Pedrosa M.F., et al. Local anti-inflammatory activity: Topical formulation containing Kalanchoe brasiliensis and Kalanchoe pinnata leaf aqueous extract. Biomed. Pharmacother. 2019;113:108721. doi: 10.1016/j.biopha.2019.108721. [DOI] [PubMed] [Google Scholar]
- 132.Tatsimo S., Tamokou J., Havyarimana L., Csupor D., Forgo P., Hohmann J., Kuiate J.-R., Tane P. Antimicrobial and antioxidant activity of kaempferol rhamnoside derivatives from Bryophyllum pinnatum. BMC Res. Notes. 2012;5:158. doi: 10.1186/1756-0500-5-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Costa S.S., Jossang A., Bodo B., Souza M.L., Moraes V.L. Patuletin acetylrhamnosides from Kalanchoe brasiliensis as inhibitors of human lymphocyte proliferative activity. J. Nat. Prod. 1994;57:1503–1510. doi: 10.1021/np50113a005. [DOI] [PubMed] [Google Scholar]
- 134.García-Pérez P., Lozano-Milo E., Zhang L., Miras-Moreno B., Landin M., Lucini L., Gallego P.P. Neurofuzzy logic predicts a fine-tuning metabolic reprogramming on elicited Bryophyllum PCSCs guided by salicylic acid. Front. Plant Sci. 2022;13:991557. doi: 10.3389/fpls.2022.991557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bogucka-Kocka A., Zidorn C., Kasprzycka M., Szymczak G., Szewczyk K. Phenolic acid content, antioxidant and cytotoxic activities of four Kalanchoe species. Saudi J. Biol. Sci. 2018;25:622–630. doi: 10.1016/j.sjbs.2016.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gaind K.N., Gupta R.L. Phenolic components from the leaves of Kalanchoe pinnata. Planta Med. 1973;23:149–153. doi: 10.1055/s-0028-1099426. [DOI] [PubMed] [Google Scholar]
- 137.Siddiqui S., Faizi S., Siddiqui B.S., Sultana N. Triterpenoids and phenanthrenes from leaves of Bryophyllum pinnatum. Phytochemistry. 1989;28:2433–2438. doi: 10.1016/S0031-9422(00)97999-8. [DOI] [Google Scholar]
- 138.Kruk J., Pisarski A., Szymanska R. Novel vitamin E forms in leaves of Kalanchoe daigremontiana and Phaseolus coccineus. J. Plant Physiol. 2011;168:2021–2027. doi: 10.1016/j.jplph.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 139.Siems K., Jas G., Arriaga-Ginerb F.J., Wollenweber E., Dorr M. On the chemical nature of epicuticular waxes in some succulent Kalanchoe and Senecio species. Z. Naturforschung C. 1995;50:451–454. doi: 10.1515/znc-1995-5-617. [DOI] [Google Scholar]
- 140.Van Maarseveen C., Jetter R. Composition of the Epicuticular and Intracuticular Wax Layers On Kalanchoe daigremontiana (Hamet Et Perr. De La Bathie) Leaves. Phytochemistry. 2009;70:899–906. doi: 10.1016/j.phytochem.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 141.Sharker S.M., Hossain K.M., Haque M.R., Hamidul Kabir A.N.M., Hasan C.M., Rashid M.A. Phytochemical and pharmacological studies of Bryophyllum daigremontianum (Raym.) Am. J. PharmTech Res. 2013;3:484–492. [Google Scholar]
- 142.Aldalbahi A., Alterary S., Almoghim R.A.A., Awad M.A., Aldosari N.S., Alghannam S.F., Alabdan A.N., Alharbi S., Alateeq B.A.M., Al Mohsen A.A., et al. Greener Synthesis of Zinc Oxide Nanoparticles: Characterization and Multifaceted Applications. Molecules. 2020;25:4198. doi: 10.3390/molecules25184198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wang C.Y., Huang S.C., Zhang Y., Lai Z.R., Kung S.H., Chang Y.S., Lin C.W. Antiviral Ability of Kalanchoe gracilis Leaf Extract against Enterovirus 71 and Coxsackievirus A16. Evid. Based Complement. Alternat. Med. 2012;2012:503165. doi: 10.1155/2012/503165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Nguelefack T.B., Nana P., Atsamo A.D., Dimo T., Watcho P., Dongmo A.B., Tapondjou L.A., Njamen D., Wansi S.L., Kamanyi A. Analgesic and anticonvulsant effects of extracts from the leaves of Kalanchoe crenata (Andrews) Haworth (Crassulaceae) J. Ethnopharmacol. 2006;106:70–75. doi: 10.1016/j.jep.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 145.Sánchez-Martínez J.D., Valdés A., Gallego R., Suárez-Montenegro Z.J., Alarcón M., Ibañez E., Alvarez-Rivera G., Cifuentes A. Blood-Brain Barrier Permeability Study of Potential Neuroprotective Compounds Recovered from Plants and Agri-Food by-Products. Front. Nutr. 2022;9:924596. doi: 10.3389/fnut.2022.924596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Viršile A., Samuoliene G., Laužike K., Šipailaite E., Balion Z., Jekabsone A. Species-Specific Plant-Derived Nanoparticle Characteristics. Plants. 2022;11:3139. doi: 10.3390/plants11223139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Stefanowicz-Hajduk J., Hering A., Gucwa M., Sztormowska-Achranowicz K., Kowalczyk M., Soluch A., Ochocka J.R. An In Vitro Anticancer, Antioxidant, and Phytochemical Study on Water Extract of Kalanchoe daigremontiana Raym.-Hamet and H. Perrier. Molecules. 2022;27:2280. doi: 10.3390/molecules27072280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hsieh Y.J., Huang H.S., Leu Y.L., Peng K.C., Chang C.J., Chang M.Y. Anticancer activity of Kalanchoe tubiflora extract against human lung cancer cells in vitro and in vivo. Environ. Toxicol. 2015;31:1663–1673. doi: 10.1002/tox.22170. [DOI] [PubMed] [Google Scholar]
- 149.Almeida A.P., Da Silva S.A., Souza M.L., Lima L.M., Rossi-Bergmann B., de Moraes V.L., Costa S.S. Isolation and chemical analysis of a fatty acid fraction of Kalanchoe pinnata with a potent lymphocyte suppressive activity. Planta Med. 2000;66:134–137. doi: 10.1055/s-2000-11131. [DOI] [PubMed] [Google Scholar]
- 150.Adam M., Elhassan G.O.M., Yagi S., Senol F.S., Orhan I.E., Ahmed A.A., Efferth T. In Vitro Antioxidant and Cytotoxic Activities of 18 Plants from the Erkowit Region, Eastern Sudan. Nat. Prod. Bioprospecting. 2018;8:97–105. doi: 10.1007/s13659-018-0155-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ferreira A.C., Rosenthal D., Carvalho D.P. Thyroid peroxidase inhibition by Kalanchoe brasiliensis aqueous extract. Food Chem. Toxicol. 2000;38:417–421. doi: 10.1016/S0278-6915(00)00017-X. [DOI] [PubMed] [Google Scholar]
- 152.Costa S.S., de Souza Mde L., Ibrahim T., de Melo G.O., de Almeida A.P., Guette C., Férézou J.P., Koatz V.L. Kalanchosine dimalate, an anti-inflammatory salt from Kalanchoe brasiliensis. J. Nat. Prod. 2006;69:815–818. doi: 10.1021/np050475+. [DOI] [PubMed] [Google Scholar]
- 153.Ibrahim T., Cunha J.M., Madi K., da Fonseca L.M., Costa S.S., Gonçalves Koatz V.L. Immunomodulatory and anti-inflammatory effects of Kalanchoe brasiliensis. Int. Immunopharmacol. 2002;2:875–883. doi: 10.1016/S1567-5769(02)00020-6. [DOI] [PubMed] [Google Scholar]
- 154.Mayorga O.A.S., da Costa Y.F.G., da Silva J.B., Scio E., Ferreira A.L.P., de Sousa O.V., Alves M.S. Kalanchoe brasiliensis Cambess., a Promising Natural Source of Antioxidant and Antibiotic Agents against Multidrug-Resistant Pathogens for the Treatment of Salmonella Gastroenteritis. Oxid. Med. Cell. Longev. 2019;2019:9245951. doi: 10.1155/2019/9245951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hewagama S.P., Hewawasam R.P. Antiurolithiatic Potential of Three Sri Lankan Medicinal Plants by the Inhibition of Nucleation, Growth, and Aggregation of Calcium Oxalate Crystals In Vitro. Sci. World J. 2022;2022:8657249. doi: 10.1155/2022/8657249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kenderson C.A., Kagoro M.L., Adelakun E.A. Phytochemical and Pharmacological Evaluation of Nigerian Kalanchoe pinnata (Lam.) Stem-Bark. J. Chem. Soc. Nigeria. 2021;46:0751–0756. doi: 10.46602/jcsn.v46i4.654. [DOI] [Google Scholar]
- 157.Cruz E.A., Da-Silva S.A., Muzitano M.F., Silva P.M., Costa S.S., Rossi-Bergmann B. Immunomodulatory pretreatment with Kalanchoe pinnata extract and its quercitrin flavonoid effectively protects mice against fatal anaphylactic shock. Int. Immunopharmacol. 2008;8:1616–1621. doi: 10.1016/j.intimp.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 158.Yadav N.P., Dixit V.K. Hepatoprotective activity of leaves of Kalanchoe pinnata Pers. J. Ethnopharmacol. 2003;86:197–202. doi: 10.1016/S0378-8741(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 159.de Araújo E.R.D., Guerra G.C.B., Andrade A.W.L., Fernandes J.M., Da Silva V.C., De Aragão Tavares E., De Araújo A.A., de Araújo Júnior R.F., Zucolotto S.M. Gastric Ulcer Healing Property of Bryophyllum pinnatum Leaf Extract in Chronic Model In Vivo and Gastroprotective Activity of Its Major Flavonoid. Front. Pharmacol. 2021;12:744192. doi: 10.3389/fphar.2021.744192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.de Araújo E.R.D., Xavier-Santos J.B., da Silva V.C., de Lima J.B.F., Schlamb J., Fernandes-Pedrosa M.d.F., da Silva Júnior A.A., de Araújo Júnior R.F., Rathinasabapathy T., Moncada M., et al. Gel formulated with Bryophyllum pinnatum leaf extract promotes skin wound healing in vivo by increasing VEGF expression: A novel potential active ingredient for pharmaceuticals. Front. Pharmacol. 2023;13:1104705. doi: 10.3389/fphar.2022.1104705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Nayak B.S., Marshall J.R., Isitor G. Wound healing potential of ethanolic extract of Kalanchoe pinnata Lam. Leaf—A preliminary study. Indian J. Exp. Biol. 2010;48:572–576. [PubMed] [Google Scholar]
- 162.Torres-Santos E.C., Da Silva S.A., Costa S.S., Santos A.P., Almeida A.P., Rossi-Bergmann B. Toxicological analysis, and effectiveness of oral Kalanchoe pinnata on a human case of cutaneous leishmaniasis. Phytother. Res. 2003;17:801–803. doi: 10.1002/ptr.1242. [DOI] [PubMed] [Google Scholar]
- 163.Phatak R.S. Lack of anthelmintic activity of Kalanchoe pinnata fresh leaves. J. Pharm. Negat. Results. 2016;7:21–24. doi: 10.4103/0976-9234.177056. [DOI] [Google Scholar]
- 164.Ramon P., Bergmann D., Abdulla H., Sparks J., Omoruyi F. Bioactive Ingredients in K. pinnata Extract and Synergistic Effects of Combined, K. pinnata and Metformin Preparations on Antioxidant Activities in Diabetic and Non-Diabetic Skeletal Muscle Cells. Int. J. Mol. Sci. 2023;24:6211. doi: 10.3390/ijms24076211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Saravanan V., Murugan S.S., Kumaravel T.S. Genotoxicity studies with an ethanolic extract of Kalanchoe pinnata leaves. Mutat. Res./Genet. Toxicol. Environ. Mutagen. 2020;856–857:503229. doi: 10.1016/j.mrgentox.2020.503229. [DOI] [PubMed] [Google Scholar]
- 166.Mahata S., Maru S., Shukla S., Pandey A., Mugesh G., Das B.C., Bharti A. Anticancer property of Bryophyllum pinnata (Lam.) Oken. leaf on human cervical cancer cells. BMC Complement. Altern. Med. 2012;12:15. doi: 10.1186/1472-6882-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hernández-Caballero M.E., Sierra-Ramírez J.A., Valencia R.V., Seseña-Méndez E. Potential of Kalanchoe pinnata as a Cancer Treatment Adjuvant and an Epigenetic Regulator. Molecules. 2022;27:6425. doi: 10.3390/molecules27196425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Plangger N., Rist L., Zimmermann R., von Mandach U. Intravenous tocolysis with Bryophyllum pinnatum is better tolerated than beta-agonist application. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006;124:168–172. doi: 10.1016/j.ejogrb.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 169.Gwehenberger B., Rist L., Huch R., von Mandach U. Effect of Bryophyllum pinnatum versus fenoterol on uterine contractility. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004;113:164–171. doi: 10.1016/S0301-2115(03)00370-1. [DOI] [PubMed] [Google Scholar]
- 170.Sazhina N.N., Lapshin P.V., Zagoskina N.V., Korotkova E.I., Misin V.M. A Comparative Analysis of the Antioxidant Activity of Kalanchoe Juices. Russ. J. Bioorg. Chem. 2014;40:771–776. doi: 10.1134/S1068162014070152. [DOI] [Google Scholar]
- 171.Lambrigger-Steiner C., Simões-Wüst A.P., Kuck A., Fürer K., Hamburger M., von Mandach U. Sleep quality in pregnancy during treatment with Bryophyllum pinnatum: An observational study. Phytomedicine. 2014;21:753–757. doi: 10.1016/j.phymed.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 172.Simões-Wüst A.P., Hassani T.A., Müller-Hübenthal B., Pittl S., Kuck A., Meden H., Eberhard J., Decker M., Fürer K., von Mandach U., et al. Sleep Quality Improves During Treatment with Bryophyllum pinnatum: An Observational Study on Cancer Patients. Integr. Cancer Ther. 2015;14:452–459. doi: 10.1177/1534735415580680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Pereira K.M.F., de Carvalho A.C., Veiga T.A.M., Melgoza A., Hernandez R.B., Grecco S.S., Nakamura U., Guo S. The psychoactive effects of Bryophyllum pinnatum (Lam.) Oken leaves in young zebrafish. PLoS ONE. 2022;17:e0264987. doi: 10.1371/journal.pone.0264987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Supratman U., Fujita T., Akiyama K., Hayashi H., Murakami A., Sakai H., Koshimizu K., Ohigashi H. Anti-tumor Promoting Activity of Bufadienolides from Kalanchoe pinnata and K. daigremontiana × butiflora. Biosci. Biotechnol. Biochem. 2001;65:947–949. doi: 10.1271/bbb.65.947. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.