Abstract
Soft-tissue sarcomas (STS) comprise a heterogeneous category of malignant tumors originating from mesenchymal tissue. Spindle cell sarcoma, characterized by its infrequent occurrence, poses diagnostic and therapeutic complexities owing to its rarity. We present a case of an 80-year-old male with a diagnosis of spindle cell sarcoma in the retroperitoneal space. The patient underwent midline exploratory laparotomy for tumor excision and was planned for postoperative chemotherapy. Unfortunately, the tumor recurred aggressively, leading to a fatal outcome. This case highlights the uncommon occurrence of retroperitoneal spindle cell sarcoma (RPSCS) and the importance of accurate diagnosis, appropriate surgical management, and adjuvant therapy.
Keywords: soft tissue tumors, oncology, atypical spindle cell/pleomorphic lipomatous tumor, recurrent spindle cell sarcoma, retroperitoneal spindle cell sarcoma
Introduction
Less than 1% of all adult malignancies are sarcomas, a rare type of malignant tumor originating from the mesenchymal tissue [1]. Based on the presumed tissue of origin and architectural pattern, the World Health Organization divides the category of soft-tissue neoplasms into >50 different histological categories. Undifferentiated soft-tissue sarcomas (STS) are a significant group [2]. Sarcomas typically manifest as a painless lump, and they seldom have distant metastases, particularly in the lungs [3].
One of the unusual types of undifferentiated STS is spindle cell sarcoma. Only a few cases have been documented in the medical literature due to their rarity [4]. Spindle cell tumors are uncommon, have a low incidence, and can develop in any portion of the human body, including the retroperitoneal space. Their histological characteristics include a mixture of fat cells and fibroblast-like spindle cells in a matrix of collagen and mucoid material. It may have a carcinomatous or neoplastic morphological appearance [5]. The objective of this case report is to present and discuss a difficult case of recurrent retroperitoneal spindle cell sarcoma (RPSCS), focusing on the diagnostic and treatment challenges related to this uncommon cancer.
Case presentation
An 80-year-old male presented to the surgical outpatient department with the complaint of a mass in the left hypochondrium and intermittent constipation. The patient had first observed the mass two months ago. Mass had gradually increased in size. It was non-tender, extending from the left hypochondrium to the umbilical region. Umbilicus was inverted, and there were visible veins on the mass and the adjacent quadrants as well. Intermittent constipation was associated with the abdominal mass. His history was remarkable. He had been treated for a left-sided direct inguinal hernia five years ago. He had a left-sided orchidectomy due to an extra-testicular atypical lipomatous tumor three years ago.
The patient was vitally stable. A general physical examination revealed that the patient was blind in the left eye, secondary to a road traffic accident. No remarkable findings in the examination of other systems, namely nervous, respiratory, and cardiac, were found. A complete blood workup was done. No significant finding was present. Ultrasound of the abdomen and pelvis pointed toward a retroperitoneal mass. Based on this finding, a computed tomography (CT) scan of the chest, abdomen, and pelvis was performed. Along with it, levels of serum alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (hCG) were also measured. Both were within normal ranges (1.42 IU/mL and <2ng/ml). CT scan showed a large complex abdominal mass occupying most of the abdominal cavity, measuring 28.5 × 20.0 cm, having internal soft tissue density and fat density mass. The lesion was found pushing the left kidney superiorly, along with compression of descending colon. No remarkable finding in the chest or pelvic region was found. There was no lymphadenopathy. Furthermore, a core biopsy of the lesion was performed. Section revealed tissue cores with spindle cell neoplasm, composed of sheets and fascicles of moderately pleomorphic spindle cells with 15 mitoses per 10 high power fields. Immunohistochemical staining showed CD34 and S100 positive. Hence a diagnosis of spindle cell sarcoma was established. Based on the complete workup and established diagnosis of spindle cell sarcoma, midline exploratory laparotomy was performed. A mass measuring 21 × 20 cm was excised after separation from surrounding structures. Mass was 15 kg in weight, measured after the operation. The post-operative recovery of the patient was uneventful. Histopathology of the excised lesion confirmed the results of initial investigations (core biopsy). The patient was explained about the nature of his illness and the importance of regular follow-ups. The patient was directed to the oncology department for postoperative chemotherapy. However, the patient failed to comply with the surgeons’ advice even after repeated explanations and did not get an oncology consult.
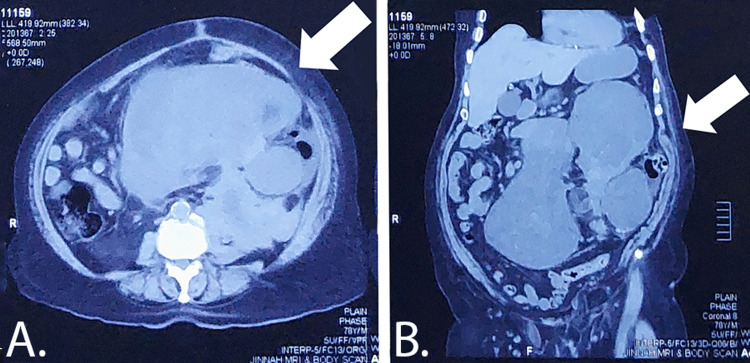
The patient presented again four months later with similar complaints and additional complaints of urinary obstruction and lower back pain. Mass had recurred in the abdomen, and it was in the left hypochondrium. Mass had grown aggressively this time. Mass had started growing for one month (that is three months after the first laparotomy). CT scan showed 210 × 145 × 200 mm hypodense mass in the left hypochondrium and pelvis. It had a bilobed appearance with well-defined margins having internal necrosis and a solid component with no calcific or fatty component, causing compression over the left ureter leading to significant hydronephroureter. Details can be seen in Figure 1. Moreover, bone window images showed wedge-shaped compression collapse at L1 with significant disc osteophytic disease. Based on all the findings and the aggressive nature of the sarcoma, the multidisciplinary team decided to go with exploratory laparotomy and, after that, adjuvant chemotherapy.
Figure 1. Abdomen CT scan. Part A (axial view) shows a hypodense mass in the abdomen and pelvis marked by the arrow. Mass can be seen arising from the left side, and bilobed morphology can also be appreciated. Part B (coronal view) shows a mass arising from the left hypochondrium and extending to the pelvic area, marked by the arrow.
However, the patient’s vitals started crashing intraoperatively. A mass compromising of 10 kg was excised. The patient was shifted to intensive care unit (ICU) post-operatively. Unfortunately, the patient’s vitals did not recover, and the patient expired within 48 hours of the surgery.
Discussion
To the best of our knowledge, limbs are where soft tissue tumors typically manifest. Abdominal soft tissue tumors are, therefore, uncommon, particularly retroperitoneal spindle cell tumors [6]. People of practically any age and sex can develop spindle cell sarcomas [7]. The median age at presentation was 57 years, according to two different investigations by Feng et al. and Smith et al. [2].
Due to their rarity, sarcomas sometimes undergo delayed or incorrect diagnoses, particularly in settings with limited facilities. A patient's history, imaging results, and biopsy are all part of the evaluation of a suspected soft-tissue sarcoma patient. In the case being presented, a CT scan and biopsy helped immensely in directing surgeons toward a definitive diagnosis. The key modality for evaluating soft-tissue masses in the extremities, trunk, head, and neck is magnetic resonance imaging (MRI) [2].
The recurrence of spindle cell sarcoma can vary depending on several variables, such as the location and stage of the tumor, the efficacy of treatment, and unique patient characteristics. Local recurrence following surgery was documented in two distinct investigations by Swamsura et al. and Diageler et al., with median follow-up times of 19 months and 15.7 months, respectively [8,9]. Surgery is the primary approach to treatment for RPSCS, with full tumor excision being the goal whenever possible [10]. The location and size of the tumor must be determined by preoperative imaging, such as CT or MRI. Based on tumor invasion, surgery may involve partial or total removal of nearby organs or structures. Postoperative radiation therapy can improve local control and lower the risk of recurrence by using methods like intensity-modulated radiation therapy (IMRT) or stereotactic body radiation therapy (SBRT) [11]. While there are few systemic treatment options, high-risk cases may benefit from adjuvant chemotherapy using drugs like doxorubicin, ifosfamide, or gemcitabine plus docetaxel. Regular post-treatment surveillance with imaging and clinical tests is required for monitoring and early intervention, and multidisciplinary teamwork between surgical oncologists, radiation oncologists, and medical oncologists is essential [12].
Conclusions
STS must be viewed as a single entity to assist clinical research on these incredibly rare disorders. Due to the diverse natural history and biological behavior exhibited by STS, establishing management guidelines that adequately address the unique clinical presentations of individual patients is exceedingly challenging. With more than 50 distinct histologic subtypes, physicians must tailor guidelines to align with the specific clinical characteristics of each patient's disease. Nonetheless, certain fundamental principles form the basis for a multimodal approach to managing STS, which should be applied within the framework of a highly personalized assessment of both the patient and the tumor.
Publication of this case report on spindle cell sarcoma is essential to add to the limited body of knowledge on this uncommon and heterogeneous disease, providing valuable insights into its clinical presentation, management strategies, and potential therapeutic approaches, ultimately enhancing and improving the care for patients with spindle cell sarcoma.
Acknowledgments
The authorship contributions for the research project are as follows: Raghu Halappa Nagaraj and Han Grezenko made substantial contributions to the conception and design of the study, actively participated in drafting the article, provided their final approval for the version to be published, and agreed to be accountable for all aspects of the work in ensuring accuracy and integrity. Yogesh Raut and Samia Rauf R. Butt played significant roles in the acquisition of data, reviewing it critically, providing their final approval for the version to be published, and agreeing to be accountable for all aspects of the work in ensuring accuracy and integrity. Chukwuyem Ekhator and Mohammad Ahsan Anwaar contributed significantly to the analysis and interpretation of data, actively participated in drafting the article, gave their final approval for the version to be published, and agreed to be accountable for all aspects of the work in ensuring accuracy and integrity. S. M. Iram Shahzed and Sophia B. Bellegarde made substantial contributions to the conception and design, reviewed it critically, gave their final approval for the version to be published, and agreed to be accountable for all aspects of the work in ensuring accuracy and integrity. Archana Das, Abdur Rehman, and Abdullah Shehryar made substantial contributions to the acquisition of data, actively participated in drafting the article, provided their final approval for the version to be published, and agreed to be accountable for all aspects of the work in ensuring accuracy and integrity. With their respective roles and contributions, all individuals meet the necessary criteria to be listed as authors in the publication.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Cancer Statistics, 2021. Siegel RL, Miller KD, Fuchs HE, Jemal A. CA Cancer J Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Spindle cell sarcoma: a case report of diagnostic and therapeutic quandary in a low resource setting. Panthi S, Poudel S, Khanal N, et al. J Surg Case Rep. 2022;2022:0. doi: 10.1093/jscr/rjab612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imaging strategy for detecting lung metastases at presentation in patients with soft tissue sarcomas. Christie-Large M, James SL, Tiessen L, Davies AM, Grimer RJ. Eur J Cancer. 2008;44:1841–1845. doi: 10.1016/j.ejca.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Sarcoma classification: an update based on the 2013 World Health Organization Classification of Tumors of Soft Tissue and Bone. Doyle LA. Cancer. 2014;120:1763–1774. doi: 10.1002/cncr.28657. [DOI] [PubMed] [Google Scholar]
- 5.Retroperitoneal spindle cell tumor: a case report. Hua H, He Z, Lei L, et al. Front Surg. 2021;8:764901. doi: 10.3389/fsurg.2021.764901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Immunohistochemistry in diagnosis of soft tissue tumours. Fisher C. Histopathology. 2011;58:1001–1012. doi: 10.1111/j.1365-2559.2010.03707.x. [DOI] [PubMed] [Google Scholar]
- 7.Soft tissue sarcomas of adults: state of the translational science. Borden EC, Baker LH, Bell RS, et al. https://pubmed.ncbi.nlm.nih.gov/12796356/ Clin Cancer Res. 2003;9:1941–1956. [PubMed] [Google Scholar]
- 8.How long should we follow patients with soft tissue sarcomas? Sawamura C, Matsumoto S, Shimoji T, Okawa A, Ae K. Clin Orthop Relat Res. 2014;472:842–848. doi: 10.1007/s11999-013-3076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Long-term outcome after local recurrence of soft tissue sarcoma: a retrospective analysis of factors predictive of survival in 135 patients with locally recurrent soft tissue sarcoma. Daigeler A, Zmarsly I, Hirsch T, Goertz O, Steinau HU, Lehnhardt M, Harati K. Br J Cancer. 2014;110:1456–1464. doi: 10.1038/bjc.2014.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Variability in Patterns of Recurrence After Resection of Primary Retroperitoneal Sarcoma (RPS): A Report on 1007 Patients From the Multi-institutional Collaborative RPS Working Group. Gronchi A, Strauss DC, Miceli R, et al. Ann Surg. 2016;263:1002–1009. doi: 10.1097/SLA.0000000000001447. [DOI] [PubMed] [Google Scholar]
- 11.Treatment guidelines for preoperative radiation therapy for retroperitoneal sarcoma: preliminary consensus of an international expert panel. Baldini EH, Wang D, Haas RL, et al. Int J Radiat Oncol Biol Phys. 2015;92:602–612. doi: 10.1016/j.ijrobp.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Soft tissue sarcoma, version 2.2018, NCCN Clinical Practice Guidelines in Oncology. von Mehren M, Randall RL, Benjamin RS, et al. J Natl Compr Canc Netw. 2018;16:536–563. doi: 10.6004/jnccn.2018.0025. [DOI] [PubMed] [Google Scholar]