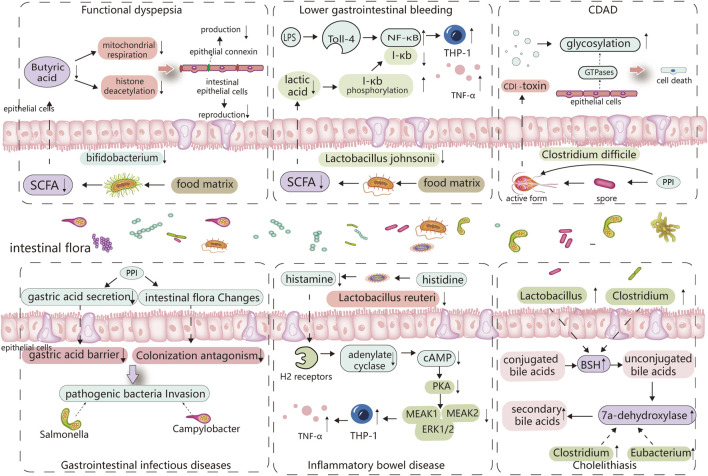
FIGURE 2.
Major altered bacterial strains and possible pathogenesis in different PPI-induced digestive diseases. The altered gut microbiota caused by PPIs and its digestive side effects are inextricably linked, with certain strains of bacteria playing an important role. Reduced Bifidobacterium abundance limits the production of butyric acid, which is linked to the reproduction of intestinal epithelial cells and the synthesis of epithelial connexin. Butyric acid deficiency increases epithelial permeability and induces functional dyspepsia. Lactobacillus johnsonii is linked to the production of lactic acid, which can inhibit the phosphorylated degradation of I-κb and promote its binding to NF-κB, thereby inhibiting TNF-α release from monocytes cells, When the abundance of Lactobacillus johnsonii decreases, THP-1 cells produce more TNF-, which is linked to PPI-induced lower gastrointestinal bleeding. PPI directly promotes Clostridium difficile toxin expression, and elevated pH also stimulates Clostridium difficile spore germination, which is associated with C. difficile-associated diseases. PPI disrupts the gastric acid barrier and normal intestinal flora, allowing exogenous pathogenic bacteria to invade and cause gastrointestinal infectious diseases. Lactobacillus reuteri can convert histidine to histamine and activates H2 receptors, cause adenylate cyclase produce more cAMP, which through PKA restrains downstream MEK/ERK-MAPK signaling, inhibiting the production of TNF-α, thus delaying the incidence of IBD. So, Lactobacillus reuteri reduction promotes the occurrence of IBD. PPI increases the abundance of bacteria that produce 7a-dehydroxylase and bile salt hydrolase in the intestine, comprises Eubacterium, Clostridium, and Lactobacillus, thereby cause an increase in the synthesis of secondary bile acids, especially deoxycholic acid (LDA). These bile acids act as a lithogenic core and promote the development of cholelithiasis.