Abstract
The prognosis of aggressive adult T-cell leukemia/lymphoma (ATL) is poor, and allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative treatment. In order to identify favorable prognostic patients after intensive chemotherapy, and who therefore might not require upfront allo-HSCT, we aimed to improve risk stratification of aggressive ATL patients aged <70 years. The clinical risk factors and genetic mutations were incorporated into risk modeling for overall survival (OS). We generated the m7-ATLPI, a clinicogenetic risk model for OS, that included the ATL prognostic index (PI) (ATL-PI) risk category, and non-silent mutations in seven genes, namely TP53, IRF4, RHOA, PRKCB, CARD11, CCR7, and GATA3. In the training cohort of 99 patients, the m7-ATLPI identified a low-, intermediate-, and high-risk group with 2-year OS of 100%, 43%, and 19%, respectively (hazard ratio [HR] =5.46; P<0.0001). The m7-ATLPI achieved superior risk stratification compared to the current ATL-PI (C-index 0.92 vs. 0.85, respectively). In the validation cohort of 84 patients, the m7-ATLPI defined low-, intermediate-, and high-risk groups with a 2-year OS of 81%, 30%, and 0%, respectively (HR=2.33; P=0.0094), and the model again outperformed the ATL-PI (C-index 0.72 vs. 0.70, respectively). The simplified m7-ATLPI, which is easier to use in clinical practice, achieved superior risk stratification compared to the ATL-PI, as did the original m7-ATLPI; the simplified version was calculated by summing the following: high-risk ATL-PI category (+10), low-risk ATL-PI category (-4), and non-silent mutations in TP53 (+4), IRF4 (+3), RHOA (+1), PRKCB (+1), CARD11 (+0.5), CCR7 (-2), and GATA3 (-3).
Introduction
Adult T-cell leukemia/lymphoma (ATL) is an aggressive peripheral T-cell neoplasm characterized by the clonal proliferation of human T-cell leukemia virus type 1 (HTLV-1)-infected T cells.1 ATL is classified into four subtypes, namely the acute, lymphoma, chronic, and smoldering types.2 Acute, lymphoma, and chronic types with one or more unfavorable prognostic factors (high lactate dehydrogenase, high blood urea nitrogen, and low albumin) are defined as aggressive ATL.3 The current frontline treatments for aggressive ATL vary by geographic location.4 In the US and Europe, antiviral therapy using zidovudine and interferon α (IFN-α) is the standard treatment for leukemic-type ATL. In Europe, chemotherapy is the first-line therapy for lymphoma-type ATL. In Japan, the current standard therapy for aggressive ATL is combination chemotherapy,5,6 and Katsuya et al. and we reported that the median overall survival (OS) was less than 1 year for aggressive ATL.6,7 Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is a curative treatment option for ATL, and 30–40% of patients who underwent allo-HSCT exhibited longer survival.8-10 Since 10–20% of aggressive ATL patients survived longer even after chemotherapy alone, a method of predicting the optimal treatment for each patient is keenly anticipated.11
Several ATL prognostic models have been reported. All are based on clinical and basic laboratory findings. The acute-and lymphoma-type ATL prognostic index (ATL-PI), which is the most widely used prognostic model, includes stage, Eastern Cooperative Oncology Group performance status (ECOG PS), age, albumin, and soluble interleukin-2 receptor (sIL-2R) level,12 while the Japan Clinical Oncology Group prognostic index (JCOG-PI) includes corrected calcium (cCa) level and ECOG PS.11 The modified ATL-PI, which includes acute type, poor PS, high sIL-2R level, high cCa level, and high C-reactive protein (CRP) level, has been proposed for patients aged ≤70 years who have aggressive ATL and who are candidates for allo-HSCT.13
We previously reported the landscape of gene mutations in ATL.14-16 Among 50 significantly mutated genes in ATL, 13 of which were affected in more than 10% of patients, and many influenced T-cell receptor (TCR)–NF-κB signaling.14 In order to select aggressive ATL patients who achieve longer survival with intensive chemotherapy, we clarified the effect of gene mutations on their prognosis and developed a clinicogenetic prognostic model for aggressive ATL by integrating gene mutation status and clinical parameters.
Methods
Study design and participants
We conducted an analysis of gene mutations and clinical risk factors in two independent cohorts of patients aged <70 years with aggressive ATL who had ATL cells or tumor biopsy specimens before starting chemotherapy. Details regarding diagnostic criteria, methods for collecting tumor DNA and clinical data, and methods for targeted capture sequencing are described in the Online Supplementary Appendix and Online Supplementary Table S1. The training cohort was derived from patients in University of Miyazaki Hospital and Imamura General Hospital (Online Supplementary Figure S1). Aggressive-type ATL samples were obtained from 43 patients aged <70 years who were diagnosed from 2014 to 2017 and who received standard chemotherapy. We previously reported the gene mutation status of 117 ATL patients who were diagnosed from 2003 to 2014 at these two institutions.17 Among them, 83 had aggressive-type ATL. In order to establish the training cohort, we first excluded 26 patients aged ≥70 years old, five patients with serious comorbidities (solid cancer or liver cirrhosis), and 11 patients who did not undergo intensive chemotherapy. This cohort ultimately included 41 patients with aggressive-type ATL who were aged <70 years and who received standard chemotherapy. We obtained DNA samples of formalin-fixed, paraffin-embedded lymph nodes from 20 patients in the training cohort who were diagnosed from 2000 to 2015. The validation cohort comprised two groups: 58 patients diagnosed from 1994 to 2017 at four institutions, whose mutational status was previously reported;17 and 52 patients from six institutions who were diagnosed from 2006 to 2017 and who underwent intensive chemotherapy. DNA samples were obtained from the second group (52 patients) for analysis in this study. This study was approved by the Research Ethics Committee of the Faculty of Medicine, University of Miyazaki, and those of other participating institutes in accordance with the Helsinki Declaration.
Statistical analysis
The detailed statistical analysis methods are described in the Online Supplementary Appendix. Briefly, we used elastic-net regression with a Cox proportional hazards model for feature selection.18 This elastic-net model was trained only on the training set, and was then applied to the independent validation set to obtain predictions. When developing the clinicogenetic risk models, patients who received mogamulizumab therapy or underwent allo-HSCT were censored on the day of mogamulizumab administration or allo-HSCT, respectively, to reduce the impact of these therapies on OS. A simplified PI, which is easier to use in clinical practice, was then developed based on the simplified β-coefficients of the original model.
Results
Patient characteristics
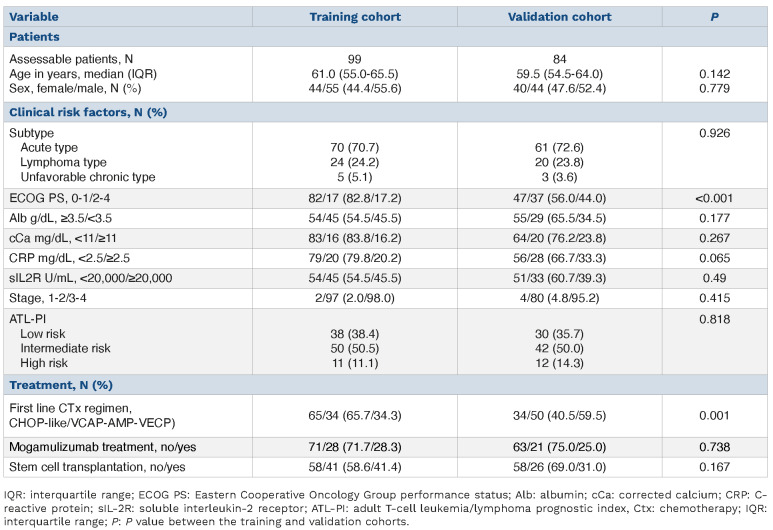
In this study of patients aged <70 years with aggressive ATL who received intensive chemotherapy, 99 patients were included in a training cohort to develop the clinicogenetic risk model, and 84 different patients were included in the validation cohort (Online Supplementary Figure S1). The characteristics of the training and validation cohorts are listed in Table 1. In the training cohort, the median age was 61.0 years (interquartile range [IQR], 55.0–65.5) and 55 patients (56%) were male. Thirty-four patients (34%) received the VCAP– AMP–VECP regimen,5 and the remaining 65 patients (66%) received the CHOP-like regimen. Mogamulizumab was administered to 28 patients (28%), and 41 (41%) underwent allo-HSCT. The 2-year OS in the training cohort was 44.5% (95% confidence interval (CI): 31.1–63.5) (Online Supplementary Figure S2). According to the ATL-PI, 38, 50, and 11 patients were categorized into low, intermediate-, and high-risk groups, respectively, and their 2-year OS was 62%, 40%, and 21%, respectively.
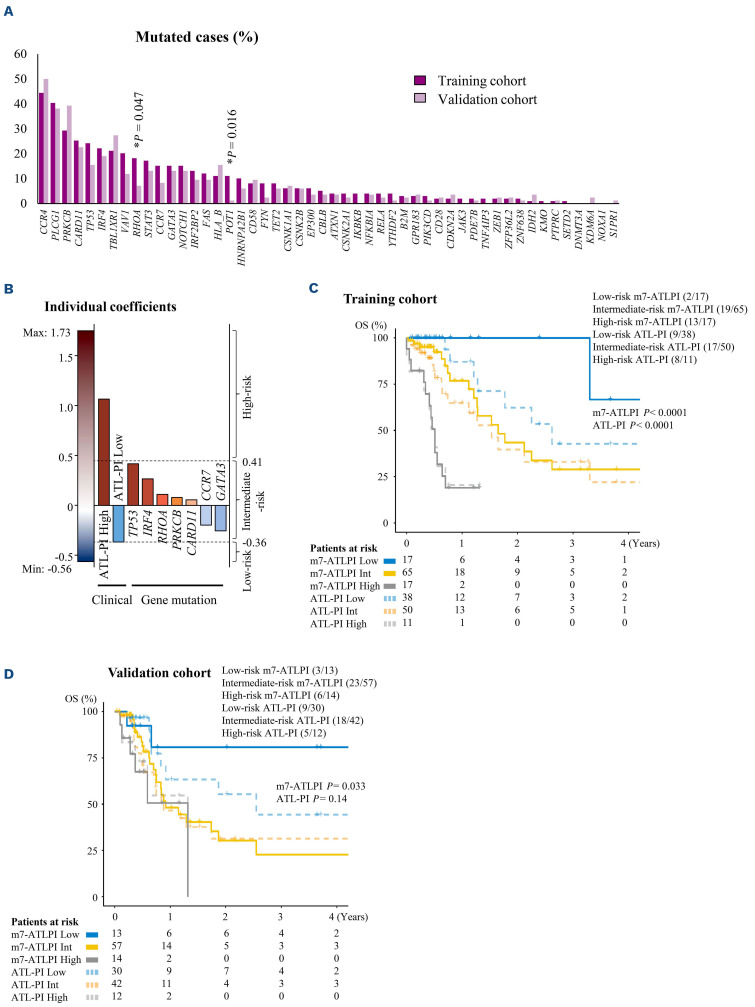
The median number of mutated genes in targeted sequencing in each patient was five (IQR, 4–7) (Online Supplementary Figure S3; Online Supplementary Table S2). Thirteen genes had non-silent mutations in at least 15% of patients (Figure 1A; Online Supplementary Figure S4). Overall, 77 (78%) ATL patients harbored one or more non-silent mutations in genes coding for NF-κB activation molecules downstream of the TCR, namely PLCG1, PRKCB, CARD11, IRF4, VAV1, STAT3, and NFKB1A. Furthermore, 54 patients (55%) had non-silent mutations in one or both of CCR4 and CCR7. Additional mutations were observed in TP53, GATA3, RHOA, and FAS. The frequencies of all mutation types (transitions, transversions, and insertions/deletions) in the 13 genes are shown in the Online Supplementary Figure S5. A subset of mutations was clustered at known hotspots (Online Supplementary Figure S6). Mutations in PRKCB and IRF4 were highly clustered in the catalytic domain and in the DNA binding domain, respectively. In both CCR4 and CCR7, almost all mutations occurred in the cytoplasmic regions.
The effect of gene mutations on clinical parameters and survival
Components of the ATL-PI and other clinical parameters were associated with specific gene mutations in univariate analysis; however, none of these associations were statistically significant after correction for multiple testing (Online Supplementary Table S3). Among them, VAV1 mutations were associated with albumin <3.5 mg/dL, cCa ≥11 mg/dL, and CRP >2.5 mg/dL, and subsequently with high or intermediate risk on the ATL-PI after correction for multiple testing.
Table 1.
Patient and disease characteristics.
Figure 1.
The m7-ATLPI clinicogenetic risk model. (A) Mutation frequencies of recurrent mutant genes in adult T-cell leukemia/lymphoma (ATL) in training and validation cohorts. P values were determined by Fisher’s exact test without correction for multiple testing. Detailed mutation plots for both cohorts are shown in the Online Supplementary Table S2 and the Online Supplementary Figure S6. (B) The m7-adult T-cell leukemia/lymphoma prognostic index (ATLPI) is calculated as the sum of individual clinical and gene mutation predictor values weighted by their individual coefficients. (C) Kaplan-Meier overall survival (OS) curves for the training cohort by ATL-PI and by m7-ATLPI. (D) Kaplan-Meier OS curves for the validation cohort by ATL-PI and by m7-ATLPI. Numbers in parentheses show number of patients with events/number of patients per cohort. ATL-PI low/int/high: low-, intermediate-, or high-risk ATLPI; m7-ATLPI low/int/high: low-, intermediate-, or high-risk m7-ATLPI.
Univariate analysis was performed to identify potentially significant correlations between shorter survival and mutations in each gene (Online Supplementary Figure S7). In our previous report,17 PLCG1 mutations were associated with shorter survival in aggressive ATL patients, but they had no influence in the training cohort. TP53 mutations alone were not associated with inferior OS (HR=1.92; P=0.077), but did show an association after adjustment for the ATL-PI (HR=2.11; P=0.044).
We next performed an exploratory correlation matrix analysis to determine whether populations with statistically co-occurring combinations of genetic mutations existed, and if so, whether these populations formed independent prognostic groups (Online Supplementary Figure S8). We identified one positive weak correlation between CCR7 and NOTCH1 mutations, with a false discovery rate (FDR) q<0.05, and this combination of mutations was observed in seven (7%) of 99 patients. However, this combination did not influence survival (Online Supplementary Figure S9).
Development of a clinicogenetic risk model for aggressive adult T-cell leukemia/lymphoma
Using 13 recurrent gene mutations with a mutation frequency of 15% or higher, along with the score of the clinically based ATL-PI model, we generated a clinicogenetic risk model for OS using elastic-net penalized Cox regression. This clinicogenetic model, which we termed the m7-ATLPI, was calculated as the sum of predictor values weighted by elastic-net coefficients, and included the high-risk ATL-PI category (βelastic net = +1.1), low-risk ATL-PI category (-0.36), and non-silent mutations in seven genes: TP53 (+0.41), IRF4 (+0.26), RHOA (+0.11), PRKCB (+0.079), CARD11 (+0.056), CCR7 (-0.20), and GATA3 (-0.25) (Figure 1B; Online Supplementary Table S4). Coefficients of six other genes were effectively shrunken and set to zero. Cutoffs of -0.36 and 0.41 were adopted to define low-, intermediate-, and high-risk groups by the m7-ATLPI. In the training cohort of 99 patients, the m7-ATLPI identified a low-risk group (17 [17%]) with 2-year OS of 100% (95% CI: 100–100), an intermediate-risk group (65 [66%]) with 2-year OS of 43% (95% CI: 27–70%), and a high-risk group (17 [17%]) with 2-year OS of 19% (95% CI: 7–52%) (HR=5.46; 95% CI: 2.73–10.9; P<0.0001) (Figure 1C).
External validation
The validation cohort consisted of 84 patients from ten institutions (Online Supplementary Figure S1). Compared with the training cohort, more patients in the validation cohort had a poor PS (17% vs. 44%, respectively; P<0.001) and received the VCAP-AMP-VECP regimen as first-line chemotherapy (34% vs. 60%, respectively; P=0.001) (Table 1). The two cohorts were similar regarding the percentages of patients determined to be low-risk by the ATL-PI (38% vs. 36%, respectively; P=0.82). The median number of gene mutations was five (IQR, 3–7), which did not differ from that of the training cohort (Online Supplementary Figure S3). The mutational landscape is summarized in the Online Supplementary Figure S4. The frequencies of gene mutations did not differ between the training and validation cohorts except for RHOA and POT1, which demonstrated lower mutation frequencies in the validation cohort (Figure 1A). With the same cutoffs as those used in the training cohort, the m7-ATLPI applied to the validation cohort defined a low-risk group (13 [15%]) with 2-year OS of 81% (95% CI: 60–100), an intermediate-risk group (57 [68%]) with 2-year OS of 30% (95% CI: 17–55), and a high-risk group (14 [17%]) with 2-year OS of 0% (95% CI: not available [na] - na) (HR=2.33; 95% CI: 1.23– 4.41; P=0.0094) (Figure 1D).
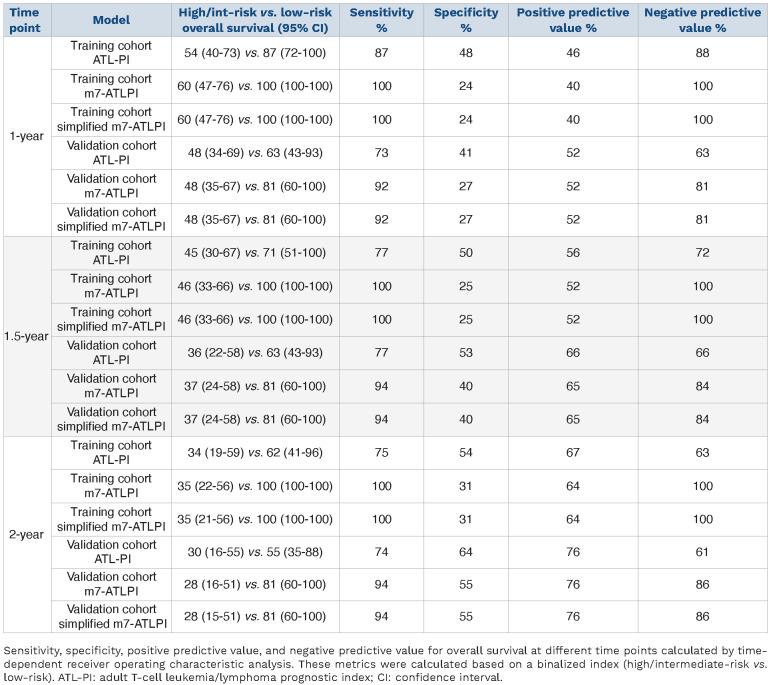
Table 2.
Improved concordance index with the m7-ATLPI and simplified m7-ATLPI.
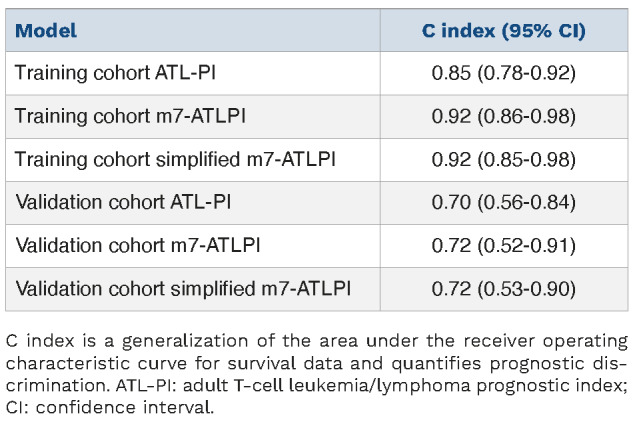
Performance assessment of the m7-adult T-cell leukemia/lymphoma prognostic index
In order to quantify which prognostic model, the ATL-PI or m7-ATLPI, better fit the actual outcomes, we calculated C-indices. The C-index for the m7-ATLPI was 0.92 in the training cohort, which was better than that of 0.85 for the ATL-PI (Table 2). A similar result was obtained in the validation cohort, with C-indices of 0.72 and 0.70 for the m7-ATLPI and ATL-PI, respectively. Receiver operating characteristic (ROC) performance metrics for the m7-ATLPI and ATL-PI based on OS at different time points in both cohorts are outlined in Table 3. The sensitivity and negative predictive value (NPV) for 2-year OS were superior for the m7-ATLPI relative to the ATLPI; that is, 100% and 100% in the training cohort, and 94% and 86% in the validation cohort, respectively. This tendency was consistent with results of 1-year OS. These findings indicate that the m7-ATLPI has a high probability of correctly identifying patients with a good prognosis.
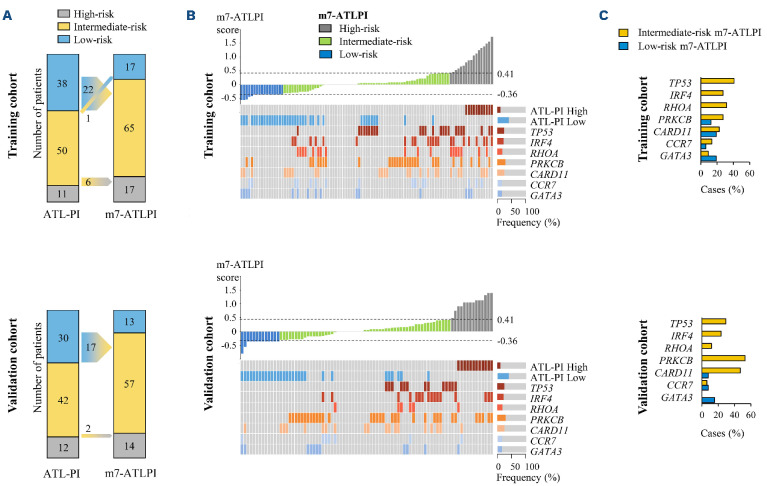
Reclassification of risk categories by the m7-adult T-cell leukemia/lymphoma prognostic index
In both cohorts, the improved performance by the m7-ATLPI resulted mainly from reclassifying a subset of patients defined as low risk by the ATL-PI into the intermediate-risk m7-ATLPI category. This applied to 22 (58%) of 38 patients in the training cohort and 17 (57%) of 30 patients in the validation cohort, and their median survival time was 1.28 years (Figure 2A; Figure 3A). ATL cells from these patients harbored mutations in PRKCB, CARD11, IRF4, RHOA, or TP53 (Figure 2B, C). Patients defined as low risk by the ATL-PI and without TP53, IRF4, RHOA, PRKCB, or CARD11 mutations, or those with PRKCB or CARD11 mutations in addition to mutations in a gene with favorable impact (CCR7 or GATA3), exhibited a favorable prognosis with a median survival time of 7.55 years. Similarly, a subset of patients with intermediate ATL-PI scores was reclassified into the high-risk m7-ATLPI category, and their median survival time was 0.46 years (6 [12%] of 50 patients in the training cohort and 2 [4.8%] of 42 patients in the validation cohort) (Figures 2A and 3A). One ATL-PI intermediate-risk patient was reclassified into the low-risk m7-ATLPI category.
Table 3.
Improved sensitivity and negative predictive value of overall survival at different time points with the m7-ATLPI and simplified m7-ATLPI.
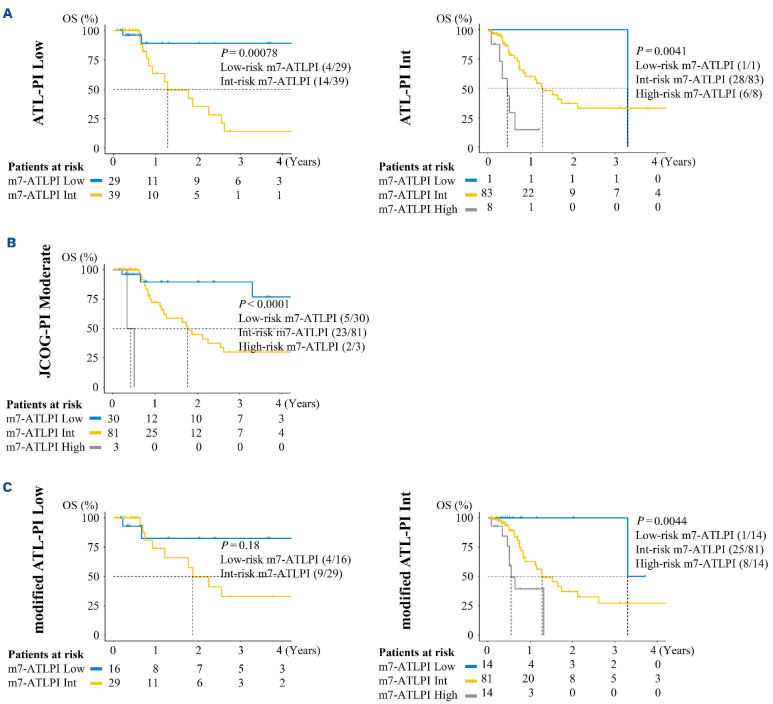
Accordingly, the m7-ATLPI could identify which low-risk ATL-PI patients had favorable versus poor OS (Figure 3A). In the entire cohort, 68 (37%) of 183 patients were classified as low-risk ATL-PI, and they were reclassified by the m7-ATLPI into low- (29 [43%] of 68) and intermediate-risk (39 [57%] of 68) groups with 2-year OS of 89% and 35%, respectively (P=0.0078).
The m7-ATLPI could also segregate low-risk patients defined by other ATL prognostic models based on clinical parameters (Figure 3B, C). Among 114 patients defined as moderate risk by the JCOG-PI, the 2-year OS of 30 (26%) patients who were reclassified as low risk by the m7-ATLPI was 90%, whereas the 2-year OS of 81 (71%) and three (2.6%) patients who were reclassified as intermediate and high risk by m7-ATLPI was 45% and 0%, respectively (P<0.0001). As for 45 patients categorized as low risk by the modified ATL-PI, the 2-year OS of 16 (36%) and 29 (64%) patients who were reclassified into the low- and intermediate-risk groups by the m7-ATLPI was 83% and 49%, respectively, although their survival curves did not differ significantly (P=0.18).
The mutations in the seven genes included in the m7-ATLPI also contributed to reclassification of patients categorized as intermediate risk by the modified ATL-PI (Figure 3C). Patients categorized as intermediate risk by the modified ATL-PI could be divided into low-, intermediate-, and high-risk groups by the m7-ATLPI, with 2-year OS of 100%, 37%, and 0%, respectively (P=0.0044).
Copy number alteration
We previously reported that a high number of copy number alterartions (CNA) was a characteristic of aggressive-type ATL.17 Among the seven genes that affect ATL prognosis, IRF4, TP53, CARD11, and GATA3 frequently have CNA. Like somatic mutations, CNA in these driver genes may influence ATL prognosis. In this study, data concerning CNA in IRF4, TP53, CARD11, and GATA3 were available from only 83 of the 183 total samples; specifically, CNA of these genes were detected in 15, 8, 9, and 16 samples, respectively (Online Supplementary Figure S10A). The eight patients with CNA in TP53 exhibited worse prognosis than patients without these CNA, and their risk categories as defined by the m7-ATLPI were high and intermediate in three and five patients, respectively (Online Supplementary Figure S10A, B). Six, one, and one of these patients harbored PRKCB, CARD11, and TP53 mutations, respectively. CNA in IRF4, CARD11, and GATA3 had no effect on OS. In addition, CNA in 9p24 (PD-L1), which had an adverse effect on OS in our previous report,17 had no effect in this cohort.
Figure 2.
Reclassification of risk categories by m7-ATLPI. (A) Transitions in the distribution of risk categories following the change from the adult T-cell leukemia/lymphoma prognostic index (ATL-PI) to the m7-ATLPI, for both the training and validation cohorts. (B) m7-ATLPI scores for patients in the training and validation cohorts, along with clinical predictors (ATL-PI categories) and molecular predictors. Boxes indicate high- or low-risk ATL-PI categories, or mutations in the indicated genes, and the color codes indicate the coefficients of the individual m7-ATLPI predictors. The corresponding Kaplan-Meier overall survival (OS) curves for patients classified as low-risk by the ATL-PI and then reclassified by the m7-ATLPI are shown in Figure 3A. (C) Relative frequencies of molecular predictors by m7-ATLPI category in low-risk ATL-PI patients in the training and validation cohorts.
Overall, 28, 17, 25, and 23 patients had mutations and/or CNA in IRF4, TP53, CARD11, and GATA3, respectively. Among these 83 patients, the risk category defined by the m7-ATLPI changed for nine patients when CNA were considered as risk factors: from low to intermediate risk in one patient, from intermediate to low risk in three patients, and from intermediate to high risk in five patients. Nonetheless, adding CNA data to the m7-ATLPI did not enhance the risk-stratification potential of the model compared with the use of mutation data alone (C-index: 0.88 vs. 0.88, respectively) (Online Supplementary Figure S10C).
Figure 3.
m7-ATLPI segregates patients with favorable prognosis from among low- or intermediate-risk patients defined by ATL prognostic models based on clinical parameters. (A) Kaplan-Meier overall survival (OS) curves stratified by the m7-adult T-cell leukemia/lymphoma prognostic index (m7-ATLPI) for patients in the entire cohort (training and validation cohorts) who were classified as low risk or intermediate risk by the ATL-PI. (B) Kaplan-Meier OS curves stratified by the m7-ATLPI for patients in the entire cohort who were classified as moderate risk by the Japan Clinical Oncology Group prognostic index. (C) Kaplan-Meier OS curves stratified by the m7-ATLPI for patients in the entire cohort who were classified as low risk or intermediate risk by the modified ATL-PI. Numbers in parentheses show the number of patients with events/number of patients per cohort.
Progression-free survival prediction by m7-adult T-cell leukemia/lymphoma prognostic index
The m7-ATLPI was developed to predict OS in patients with aggressive ATL who were treated with standard intensive chemotherapy. In clinical practice in Japan, allo-HSCT is performed shortly after the diagnosis of ATL in eligible patients.10 Sixty-seven patients in this study underwent alloHSCT at a median of 164 days (IQR, 121–220) after diagnosis.
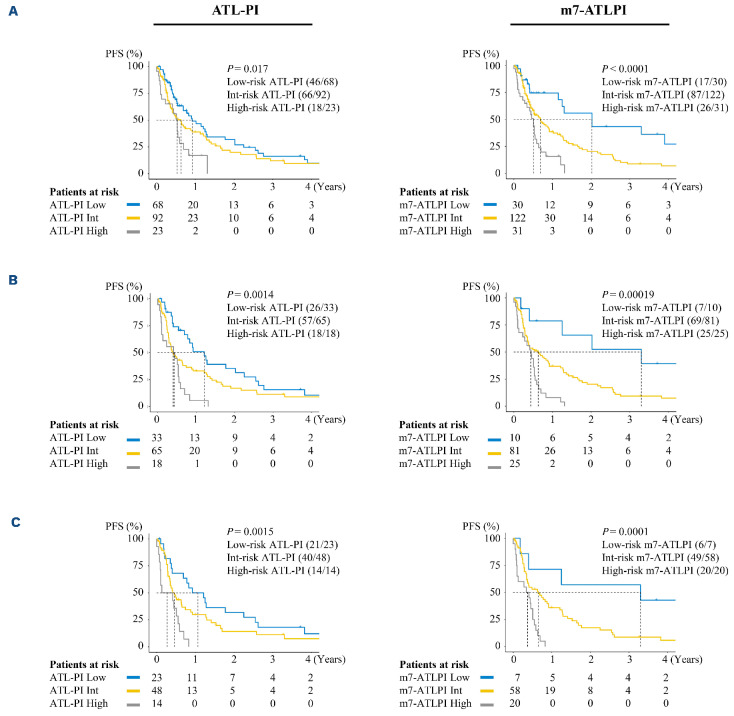
Figure 4.
The m7-ATLPI provides beter risk stratification of progression-free survival than the ATL-PI. (A) Kaplan-Meier progression-free survival (PFS) curves by the adult T-cell leukemia/lymphoma prognostic index (ATL-PI) and m7-ATLPI for the entire cohort (n=183). (B) Kaplan-Meier PFS curves by the ATL-PI and m7-ATLPI for patients without allogenic hematopoietic stem cell transplantation (allo-HSCT) in the entire cohort (n=116). (C) Kaplan-Meier PFS curves by the ATL-PI and m7-ATLPI for patients with neither allo-HSCT nor mogamulizumab therapy in the entire cohort (n=85).
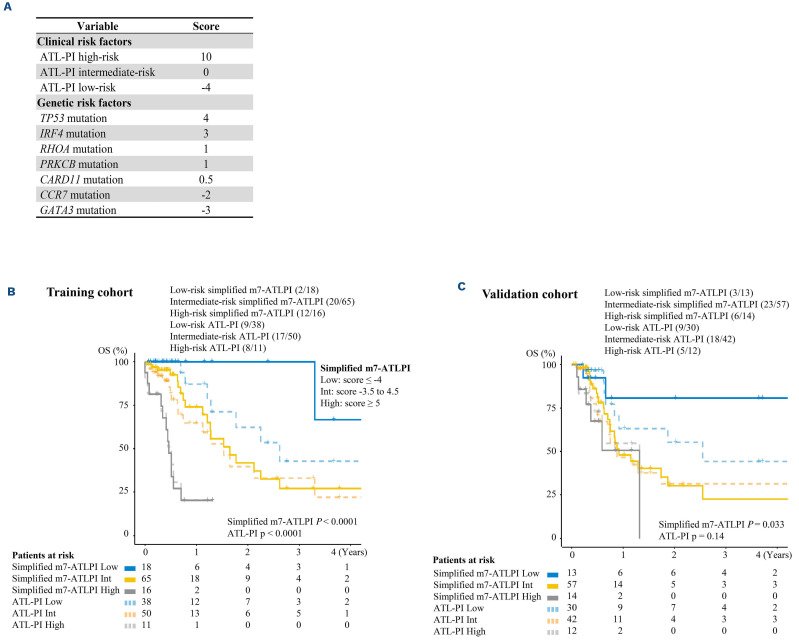
Figure 5.
The simplified m7-ATLPI has comparable prognostic ability as the original m7-ATLPI. (A) Scoring of the simplified m7-adult T-ceLL leukemia/lymphoma prognostic index (m7-ATLPI). In order to create the simplified m7-ATLPI, the coefficients of the ATL-PI categories and mutation status of the 7 genes were converted to numbers reflecting their original values. After summing these values, scores <-4, -3.5 to 4.5, and >5 points were categorized as low-, intermediate-, and high-risk simplified m7-ATLPI, respectively. (B) Kaplan-Meier overall survival (OS) curves for the training cohort using the ATL-PI and simplified m7-ATLPI. (C) Kaplan-Meier OS curves for the validation cohort using the ATL-PI and simplified m7-ATLPI. Numbers in parentheses show the number of patients with events/number of patients per cohort. ATL-PI low/int/high: low-, intermediate-, or high-risk ATL-PI; Simplified m7-ATLPI low/int/high: low-, intermediate-, or high-risk simplified m7-ATLPI.
Low-risk patients defined by the m7-ATLPI were more likely to undergo allo-HSCT: 20 of 30 low-risk patients, 41 of 122 intermediate-risk patients, and six of 31 high-risk patients. The disease status at transplantation in the 20 low-risk, 41 intermediate-risk, and six high-risk patients was complete response (CR)/partial response (PR) in 13, 25, and six, respectively, and stable disease (SD)/progressive disease (PD) in seven, 16, and zero, respectively. Eight of 44 patients who underwent allo-HSCT in CR/PR died of regimen-related toxicities rather than of ATL progression. In order to accurately determine the clinical course of ATL treated with chemotherapy, we performed censoring at allo-HSCT. When patient survival was not censored by allo-HSCT or mogamulizumab therapy, the m7-ATLPI identified a low-risk group with 2-year OS of 57% (95% CI: 41–79), an intermediate-risk group with 2-year OS of 37% (95% CI: 28–47), and a high-risk group with 2-year OS 6.7% (95% CI: 1.8–26) (Online Supplementary Figure S11A). Analyses of patients who did not undergo allo-HSCT and those who were treated only with chemotherapy and not with mogamulizumab or alloHSCT also showed superior risk stratification compared to the current ATL-PI (C-index 0.78 vs. 0.73, and 0.80 vs. 0.75, respectively) (Online Supplementary Figure S11B, C). Progression-free survival (PFS) might be suitable as a means of evaluating the sensitivity to chemotherapy in ATL. In order to analyze this question, patients who underwent allo-HSCT or mogamulizumab therapy in CR/PR were censored at the time of allo-HSCT or the administration of mogamulizumab, respectively (Figure 4A). In the low-risk group defined by the m7-ATLPI, the median PFS of 2.0 years was longer than that of 0.92 years in the corresponding group defined by the ATL-PI, and the m7-ATLPI achieved superior risk stratification compared to the current ATL-PI (C-index: 0.67 vs. 0.63, respectively). These results suggest that the m7-ATLPI predicts sensitivity to chemotherapy. When the analysis was restricted to patients without allo-HSCT (n=116) or to patients with neither allo-HSCT nor mogamulizumab therapy (n=85), the m7-ATLPI exhibited superior risk stratification compared to the ATL-PI (C-index 0.70 vs. 0.68, and 0.73 vs. 0.68, respectively) (Figure 4B, C).
The effect of gene mutations on patients treated with mogamulizumab or allo-hematopoietic stem cell transplantation
In addition to chemotherapy, widely used treatments for aggressive-type ATL include IFN-α, zidovudine, mogamulizumab, and brentuximab vedotin. Since no patients in our cohort received first-line therapy with any of these agents, it follows that m7-ATLPI could be applied only for patients who received conventional intensive chemotherapy. Even though mogamulizumab was not administered as first-line therapy, 49 patients were treated with mogamulizumab as second- or later-line therapy. Since three and eight patients received mogamulizumab therapy in CR/PR status after first-line chemotherapy or alloHSCT, respectively, 38 patients received mogamulizumab therapy in chemotherapy-resistant status at any time during their clinical course. We tested whether determining the prognosis of the 38 patients treated with mogamulizumab in chemotherapy-resistant status was impacted by considering the mutations in the seven genes included in the m7-ATLPI (Online Supplementary Figure S12A). The m7-ATLPI could not determine which patients treated with mogamulizumab in chemotherapy-resistant status had a favorable prognosis. Sakamoto et al. reported that patients with CCR4 mutations who received mogamulizumab-based treatment and not allo-HSCT had a favorable prognosis.19 Of 49 patients who underwent mogamulizumab therapy, 27 had CCR4 mutations and 22 did not. Survival time after mogamulizumab therapy was comparable regardless of CCR4 mutation status: 0.53 and 0.31 years in patients with and without CCR4 mutations, respectively (P=0.85) (Online Supplementary Figure S13A). When the analysis was restricted to patients who did not undergo allo-HSCT, the survival time after mogamulizumab therapy was comparable between patients with and without CCR4 mutations (Online Supplementary Figure S13B). In our study, CCR4 mutations had little effect on the prognosis of patients treated with mogamulizumab. Among the entire cohort, 67 patients underwent allo-HSCT. The survival curves of the three risk groups defined by the m7-ATLPI almost overlapped, indicating that the m7-ATLPI had no ability to predict the prognosis of ATL patients after allo-HSCT (Online Supplementary Figure S12B).
Simplified m7-adult T-cell leukemia/lymphoma prognostic index
We simplified the original m7-ATLPI to make the instrument easier to use in clinical practice. We based this simplified version on the sums of the weights of the following variables obtained from the ATL-PI risk category and the mutational statuses of seven genes: high-risk ATL-PI category (+10), low-risk ATL-PI category (-4), and non-silent mutations in TP53 (+4), IRF4 (+3), RHOA (+1), PRKCB (+1), CARD11 (+0.5), CCR7 (-2), and GATA3 (-3). Scores <-4, from -3.5 to 4.5, and >5 were used to define the low-, intermediate-, and high-risk categories, respectively (Figure 5). In the training cohort, one patient classified as intermediate risk and one classified as high risk according to the m7-ATLPI were reclassified as low risk and intermediate risk according to the simplified m7-ATLPI, respectively. The simplified m7-ATLPI was then applied to the validation cohort. The classification in the validation cohort showed high concordance with that in the original m7-ATLPI (weighted K, 1.00), and no patients were reclassified by the simplified m7-ATLPI. The C-index for the simplified m7-ATLPI was 0.92 and 0.72 in the training and validation cohort, respectively, which was same as that of 0.92 and 0.72 for the original m7-ATLPI (Table 2). The sensitivity and NPV for 2-year OS with the simplified m7-ATLPI were the same as those with the original m7-ATLPI; that is, 100% and 100% in the training cohort, and 94% and 86% in the validation cohort, respectively (Table 3). This tendency was consistent with results of 1-year OS.
Discussion
By considering gene mutation status and clinical parameters in patients with aggressive ATL who received intensive chemotherapy, we established the m7-ATLPI prognostic model, which could select patients with longer survival from among low-risk ATL patients aged <70 years who received intensive chemotherapy. Indices that stratify favorable subsets and help avoid excessive treatment have been developed for malignant lymphoma.20 However, such indices have not been developed in ATL. The m7-ATLPI was based on the previously established ATL-PI, which considers clinical risk factors, and on the mutational status of seven genes, specifically TP53, IRF4, RHOA, PRKCB, CARD11, CCR7, and GATA3. This mutational information was used to identify patients with a favorable prognosis after intensive chemotherapy alone from among low-risk patients defined not only by the ATL-PI, but also by other ATL prognostic models such as the JCOG-PI.
We previously reported that genetic abnormalities affected clinical outcomes in ATL patients.17 In that report, the status of PRKCB mutation and 9p24 (PD-L1) amplification, age ≥70 years, and the JCOG-PI high-risk category defined by poor PS or elevated cCa level were associated with poor survival by multivariate analysis. These adverse prognostic factors could divide aggressive ATL patients into different risk category groups; however, the 2-year OS of patients with none of these adverse factors was still below 30%. In follicular lymphoma, the Follicular Lymphoma International Prognostic Index (FLIPI), which is based on clinical and basic laboratory data, has been widely used in risk models.21 The m7-FLIPI is a clinicogenetic risk model that includes the mutation status of seven genes in addition to FLIPI and PS, and it was found to be able to identify patients at highest risk of treatment failure.22 In our previous report,17 the chemotherapy regimens varied, the clinical information was insufficient, and patients aged ≥70 years comprised 30% of the cohort. In order to identify patients with a favorable prognosis after standard intensive chemotherapy alone, and who therefore might not require upfront allo-HSCT, we focused on patients aged <70 years who were candidates for allo-HSCT, and collected detailed clinical data to generate a clinicogenetic prognostic model based on the ATL-PI.
The m7-ATLPI includes the ATL-PI risk category as well as the presence or absence of non-silent mutations in TP53, IRF4, RHOA, PRKCB, CARD11, CCR7, and GATA3. Of these mutations, the first five were associated with a poor prognosis, while the last two were correlated with a favorable prognosis. Our previous report identified only PRKCB mutations as being associated with a poor prognosis.17 Sakihama et al. also reported that PRKCB mutations were associated with a poor prognosis in patients with aggressive ATL.23 Using the m7-ATLPI, more than half of patients classified as low risk by the ATL-PI were reclassified as intermediate risk. This means that patients determined to be low risk based on clinical and basic laboratory data were divided into two risk groups by also considering gene mutation information. Excluding patients who also had CCR7 or GATA3 mutations, those with mutations in one or more of TP53, IRF4, RHOA, PRKCB, and CARD11 had an inferior prognosis. They demonstrated a relatively poor clinical course with a mean survival time of 1.28 years, which was similar to that in the intermediate-risk group defined by the ATL-PI. Patients classified as low risk by the ATL-PI and who did not have mutations in TP53, IRF4, RHOA, PRKCB, or CARD11, or those with PRKCB or CARD11 mutations in addition to mutations in a gene with favorable impact (CCR7 or GATA3), exhibited a favorable prognosis with a mean survival time of 7.55 years. These patients may not require upfront allo-HSCT, since only 30–40% of such patients who underwent allo-HSCT achieved longer survival.8-10
We previously reported that a high CNA count was a characteristic of aggressive-type ATL.17 In that report, only 9p24 (PD-L1) amplification had an adverse effect on OS in aggressive-type ATL. In the subset of our cohort in which CNA was examined, patients with CNA in TP53 exhibited poor OS. However, adding CNA data to the m7-ATLPI did not enhance the risk stratification potential of the model compared with inclusion of mutation data alone. This might be because all patients with CNA in TP53 also harbored one or more mutations in PRKCB, CARD11, or TP53, and these mutations had a negative impact on OS.
Even though the m7-ATLPI was developed to predict OS in patients with aggressive ATL who are treated with standard intensive chemotherapy, it is also useful to predict PFS. The median PFS in the low-risk group defined by the m7-ATLPI was 2.0 years, which was longer than the 0.92 years in the corresponding group defined by the ATL-PI, suggesting that the m7-ATLPI predicts sensitivity to chemotherapy. As noted above, IFN-α, zidovudine, mogamulizumab, and brentuximab vedotin are commonly used to treat aggressive-type ATL. We were unable to analyze the effects of these drugs on OS and PFS in this study, because all patients were treated with only conventional chemotherapy as first-line therapy. This is a major limitation of this study, and future research should develop prognostic models that integrate IFN-α, zidovudine, mogamulizumab, or brentuximab vedotin treatment.
In summary, the m7-ATLPI, which was established by integrating the mutational status of seven genes with the previously established ATL-PI, and its simplified version, namely the simplified m7-ATLPI, could divide ATL patients into three risk categories. Sixteen percent of ATL patients aged <70 years were categorized as low risk by the m7-ATLPI, and exhibited a relatively favorable prognosis with a 2-year OS of more than 80% with standard intensive chemotherapy alone. The current standard of care for ATL, which is to perform upfront allo-HSCT, might be reconsidered in this group. On the other hand, patients classified by the m7-ATLPI as intermediate or high risk had shorter survival, and may benefit from alternative treatments such as allo-HSCT.
Supplementary Material
Acknowledgments
The authors would like to thank Y. Kakizoe, T. Kawabata, M. Fukuyama, M. Makino, Y. Aratake, Y. Arashi, and Y. Kurogi for their support with data curation, and M. Matsushita, T. Shinmori, and S. Saitou for their technical assistance.
Funding Statement
Funding: This research was supported by grants JP19ck0106254, 20ck0106538h0001, and 21ck0106538h0002 to KS from the Japan Agency for Medical Research and Development.
References
- 1.Uchiyama T, Yodoi J, Sagawa K, et al. Adult T-cell leukemia: clinical and hematologic features of 16 cases. Blood. 1977;50(3):481-492. [PubMed] [Google Scholar]
- 2.Shimoyama M. Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984-87). Br J Haematol. 1991;79(3):428-437. [DOI] [PubMed] [Google Scholar]
- 3.Shimoyama M. Chemotherapy of ATL. K Takatsuki (Ed), Adult T-Cell Leukemia, Oxford University Press. Oxford. 1994:221-227. [Google Scholar]
- 4.Cook LB, Fuji S, Hermine O, et al. Revised Adult T-cell Leukemia-Lymphoma International Consensus Meeting Report. J Clin Oncol. 2019;37(8):677-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsukasaki K, Utsunomiya A, Fukuda H, et al. VCAP-AMP-VECP compared with biweekly CHOP for adult T-cell leukemia-lymphoma: Japan Clinical Oncology Group Study JCOG9801. J Clin Oncol. 2007;25(34):5458-5464. [DOI] [PubMed] [Google Scholar]
- 6.Sekine M, Kameda T, Shide K, et al. Higher average chemotherapy dose intensity improves prognosis in patients with aggressive adult T-cell leukemia/lymphoma. Eur J Haematol. 2021;106(3):398-407. [DOI] [PubMed] [Google Scholar]
- 7.Katsuya H, Ishitsuka K, Utsunomiya A, et al. Treatment and survival among 1594 patients with ATL. Blood. 2015;126(24):2570-2577. [DOI] [PubMed] [Google Scholar]
- 8.Utsunomiya A, Miyazaki Y, Takatsuka Y, et al. Improved outcome of adult T cell leukemia/lymphoma with allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27(1):15-20. [DOI] [PubMed] [Google Scholar]
- 9.Hishizawa M, Kanda J, Utsunomiya A, et al. Transplantation of allogeneic hematopoietic stem cells for adult T-cell leukemia: a nationwide retrospective study. Blood. 2010;116(8):1369-1376. [DOI] [PubMed] [Google Scholar]
- 10.Fuji S, Fujiwara H, Nakano N, et al. Early application of related SCT might improve clinical outcome in adult T-cell leukemia/lymphoma. Bone Marrow Transplant. 2016;51(2):205-211. [DOI] [PubMed] [Google Scholar]
- 11.Fukushima T, Nomura S, Shimoyama M, et al. Japan Clinical Oncology Group (JCOG) prognostic index and characterization of long-term survivors of aggressive adult T-cell leukaemia-lymphoma (JCOG0902A). Br J Haematol. 2014;166(5):739-748. [DOI] [PubMed] [Google Scholar]
- 12.Katsuya H, Yamanaka T, Ishitsuka K, et al. Prognostic index for acute- and lymphoma-type adult T-cell leukemia/lymphoma. J Clin Oncol. 2012;30(14):1635-1640. [DOI] [PubMed] [Google Scholar]
- 13.Fuji S, Yamaguchi T, Inoue Y, et al. Development of a modified prognostic index of patients with aggressive adult T-cell leukemia-lymphoma aged 70 years or younger: a possible risk-adapted management strategies including allogeneic transplantation. Haematologica. 2017;102(7):1258-1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kataoka K, Nagata Y, Kitanaka A, et al. Integrated molecular analysis of adult T cell leukemia/lymphoma. Nat Genet. 2015;47(11):1304-1315. [DOI] [PubMed] [Google Scholar]
- 15.Kogure Y, Kameda T, Koya J, et al. Whole-genome landscape of adult T-cell leukemia/lymphoma. Blood. 2022;139(7):967-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kataoka K, Shiraishi Y, Takeda Y, et al. Aberrant PD-L1 expression through 3'-UTR disruption in multiple cancers. Nature. 2016;534(7607):402-406. [DOI] [PubMed] [Google Scholar]
- 17.Kataoka K, Iwanaga M, Yasunaga JI, et al. Prognostic relevance of integrated genetic profiling in adult T-cell leukemia/lymphoma. Blood. 2018;131(2):215-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reddy A, Zhang J, Davis NS, et al. Genetic and functional drivers of diffuse large B cell lymphoma. Cell. 2017;171(2):481-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakamoto Y, Ishida T, Masaki A, et al. CCR4 mutations associated with superior outcome of adult T-cell leukemia/lymphoma under mogamulizumab treatment. Blood. 2018;132(7):758-761. [DOI] [PubMed] [Google Scholar]
- 20.Persky DO, Li H, Stephens DM, et al. Positron emission tomography-directed therapy for patients with limited-stage diffuse large B-cell lymphoma: results of intergroup National Clinical Trials Network Study S1001. J Clin Oncol. 2020;38(26):3003-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Relander T, Johnson NA, Farinha P, et al. Prognostic factors in follicular lymphoma. J Clin Oncol. 2010;28(17):2902-2913. [DOI] [PubMed] [Google Scholar]
- 22.Pastore A, Jurinovic V, Kridel R, et al. Integration of gene mutations in risk prognostication for patients receiving first-line immunochemotherapy for follicular lymphoma: a retrospective analysis of a prospective clinical trial and validation in a population-based registry. Lancet Oncol. 2015;16(9):1111-1122. [DOI] [PubMed] [Google Scholar]
- 23.Sakihama S, Morichika K, Saito R, et al. Genetic profile of adult T-cell leukemia/lymphoma in Okinawa: association with prognosis, ethnicity, and HTLV-1 strains. Cancer Sci. 2021;112(3):1300-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.