Abstract
BACKGROUND:
US health plans are adopting benefit designs that shift greater financial burden to patients through higher deductibles, additional copay tiers, and coinsurance. Prior systematic reviews found that higher cost was associated with reductions in both appropriate and inappropriate medications. However, these reviews were conducted prior to contemporary benefit design and medication utilization.
OBJECTIVES:
To assess the relationship and factors associated with cost-sharing and (1) medication adherence, (2) clinical outcomes, (3) health care resource utilization (HRU), and (4) costs.
METHODS:
A systematic review of literature published between January 2010 and August 2020 was conducted to identify the relationship between cost-sharing and medication adherence, clinical outcomes, HRU, and health care costs. Data were extracted using a standardized template and were synthesized by key questions of interest.
RESULTS:
From 1,995 records screened, 79 articles were included. Most studies, 71 of 79 (90%), reported the relationship between cost-sharing and treatment adherence, persistence and/or discontinuation; 16 (20%) reported data on cost-sharing and HRU or medication initiation, 11 (14%) on costsharing and health care costs, and 6 (8%) on cost-sharing and clinical outcomes. The majority of publications found that, regardless of disease area, increased cost-sharing was associated with worse adherence, persistence, or discontinuation. The aggregate data suggested the greater the magnitude of cost-sharing, the worse the adherence. Among studies examining clinical outcomes, cost-sharing was associated with worse outcomes in 1 study and the remaining 3 found no significant differences. Regarding HRU, higher-cost-sharing trended toward decreased outpatient and increased inpatient utilization. The available evidence suggested higher cost-sharing has an overall neutral to negative impact on total costs. Studies evaluating elimination of copays found either decreased or no impact in total costs.
CONCLUSIONS:
The published literature shows consistent impacts of higher cost sharing on initiation and continuation of medications, and the greater the cost-sharing, the worse the medication adherence. The evidence is limited regarding the impact of cost-sharing on clinical outcomes, HRU, and costs. Limited evidence suggests increased cost-sharing is associated with more inpatient care and less outpatient care; however, a neutral to no difference was suggested for other outcomes. Although increased costsharing is intended to decrease total costs, studies evaluating reducing or eliminating cost-sharing found that total costs did not rise. Today’s growing cost-containment environment should carefully consider the broader impact cost-sharing has on treatment adherence, clinical outcomes, resource use, and total costs. It may be that cost-sharing is a blunt, rather than precise, tool to curb health care costs, affecting both necessary and unnecessary health care use.
What is already known about this subject
Patient out-of-pocket health expenditures have increased over the past decade because of rising health care costs and evolving benefit designs.
Prior systematic reviews found higher levels of cost-sharing negatively affect prescription drug adherence.
What this study adds
This systematic literature review provides a contemporary review of the available evidence regarding costsharing and 4 outcomes (medication adherence, clinical outcomes, health care resource utilization, and health care costs).
We describe the relationship between higher cost-sharing and outcomes (worse, no difference, or better) and factors that influence this relationship.
When designing plan benefits and costsharing, a holistic view of cost-sharing and clinical and economic outcomes should be considered.
Increasing the share of health care costs for which beneficiaries are responsible is a strategy aimed at reducing the use of unnecessary health care goods and services and, ultimately, decreasing total health care costs. It is reasoned that cost-sharing will compel consumers to be more thoughtful and selective in their health care choices if they are required to shoulder a greater burden for such services. Cost-sharing was first examined 50 years ago in the RAND Health Insurance Experiment (HIE)1 in which it was found that increased cost-sharing decreased health care utilization and prescription drug use.2 Results from the HIE also suggested that decreased health care utilization and medication use did not impact health outcomes. However, an exception to this was found for an important demographic: the poorest and sickest participants. Since that landmark study, health care insurance options and plan designs have continued to evolve and the cost of health care, health premiums, and consumer cost-sharing have risen.
Patients seeking care pay out-of-pocket (OOP) expenditures (through plan deductibles, copays, or coinsurance) and this cost-sharing has increased substantially over time. Between 2005 and 2016, in employee-sponsored US health insurance plans, the annual deductible increased by 59% for beneficiaries with single coverage.3 Cost-sharing for medications has grown from 1 or 2 medication tiers to 3 or 4 tiers with wider cost-sharing differences (eg, on average $11 for tier 1, $35 for tier 2, $62 for tier 3, and $116 for tier 4).4 Beyond typical formulary copays, coinsurance for specialty medications is common with patient contributions averaging 26% in 2020.4 In 2018, the average family in a large-employer plan paid more than $3,000 in OOP costs annually on top of $5,000 in premium costs.5 Notably, the increase in OOP and premium costs were disproportionate to wage increases and inflation5 such that for many households, OOP health care costs consumed 10% or more of their annual income.6
Previous systematic reviews have found that higher levels of cost-sharing negatively affect prescription drug adherence.7-9 Additionally, individual studies have suggested that poor medication adherence correlates with increased disease complications,10,11 hospitalizations,12,13 mortality,13 and health care costs.14 In a 2007 systematic review, the use of medical (nonpharmacy) services increased with greater prescription cost-sharing for certain clinical conditions.7 Thus, although insurers and employers view cost-sharing as a means to control costs,15 high cost-sharing may paradoxically increase health care costs if it leads to poorer disease control and, ultimately, greater health care utilization and costs.
A systematic review of the published cost-sharing literature has not been recently undertaken. This systematic literature review (SLR) was conducted to answer the following questions: (1) Does the literature address the relationship between cost-sharing and treatment use, clinical outcomes, health care utilization, and health care costs? (2) What is the relationship between increased cost-sharing and outcomes (eg, worse outcomes, no difference, or better)? (3) What factors influence this relationship? For example, does the relationship differ by the type of cost-sharing (eg, copays, coinsurance, deductibles), the magnitude of cost-sharing (eg, $5, $50, or $250), or by disease or clinical condition?
Methods
This SLR was conducted according to best practices (ie, Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidance16) with the SLR methodology defined a priori in a study protocol. Embase and MEDLINE (via Embase.com) were searched (Supplementary Table 1 (393KB, pdf) , available in online article) for white papers or peer-reviewed, English-language articles published from January 1, 2010, to August 18, 2020, and reporting results from observational studies or randomized controlled trials (RCTs) conducted in the United States. Included studies met the following criteria: included individuals of any age with health insurance other than Medicaid or Veteran’s Administration coverage and reported results on the association between cost-sharing and at least 1 of the 4 outcomes of interest, (1) treatment use (eg, drug adherence, persistence, or discontinuation); (2) disease control, morbidity or mortality; (3) health care resource utilization (HRU; including inpatient services, emergency department [ED] visits, ambulatory care, or medication initiation); or (4) health care direct costs (total health care, medical, or pharmacy costs). Costsharing was required to be reported in monetary amounts. Studies including patients with health insurance coverage solely through Medicaid or Veterans Affairs were excluded because of low or zero cost-sharing. Studies focused on cost-sharing for diagnostic tests or medical care, rather than prescription medications, were also excluded.
Abstracts and full-text documents were evaluated for eligibility by 2 independent reviewers, with any discrepancies resolved by a third reviewer. Data from the included articles were entered into a Microsoft Excel template developed for the SLR; all data were validated by a second researcher. Extracted data included published study characteristics (eg, study design, data source, and time period), study sample characteristics (eg, patient population, clinical conditions, and type of health insurance coverage), and outcomes of interest (eg, publication’s outcome definition, relationship to cost-sharing). Information regarding the type and magnitude of cost-sharing (eg, differences in deductibles, differences in copays either due to tiering, the elimination of copays, reductions through copay coupons, or differences in coinsurance amounts) were also extracted. Quality assessment of each study was conducted using a risk-of-bias tool appropriate for the study design.17-20 Data were quantitatively and qualitatively synthesized to address the SLR study questions. Adherence and clinical outcomes were categorized as “worse,” “no difference,” or “better” based on the association with increased cost-sharing (eg, “worse” indicates that increased cost-sharing is associated with statistically significantly poorer adherence or clinical outcomes) (Supplementary Table 2 (393KB, pdf) ). Some studies originally reported the effect of decreased cost-sharing; for categorization, their results have been transformed for simplicity. Some studies reported both significant and nonsignificant results within an outcome category. If at least 1 result was significant, the study was categorized as having a significant association. For adherence, persistence, and discontinuation outcomes, in which this issue was the most common, these multiple results were consistently in the form of assessing multiple levels of cost-sharing in which higher levels of cost-sharing reached significance and lower levels did not. In figures that report specific study results rather than an overall categorization, significant and nonsignificant results are reported separately.
Results
OVERVIEW OF INCLUDED PUBLICATIONS
A total of 1,995 citations were screened (Figure 1), and 7921-99 articles met the predefined inclusion criteria (Supplementary Table 3 (393KB, pdf) ). Most articles (71 of 79, 90%) reported results from retrospective cohort studies, 5 (6%) from RCTs, 2 (3%) from cross-sectional studies, and 1 article reported results from a prospective cohort study. Of the 5 articles reporting results from RCTs, 3 of the publications came from the same trial (the Myocardial Infarction Free Rx Event and Economic Evaluation [MI FREEE] trial). The remaining 2 were from the Affordability and Real-World Antiplatelet Treatment Effectiveness After Myocardial Infarction Study. Most publications were based on administrative claims analyses; the mean sample size across studies was 652,920 (range: 131-27,269,026). Nearly 80% of studies included individuals covered by commercial insurance, whereas 43% included publicly insured individuals (insurance type was not mutually exclusive, as studies often included > 1 type of coverage).
FIGURE 1.
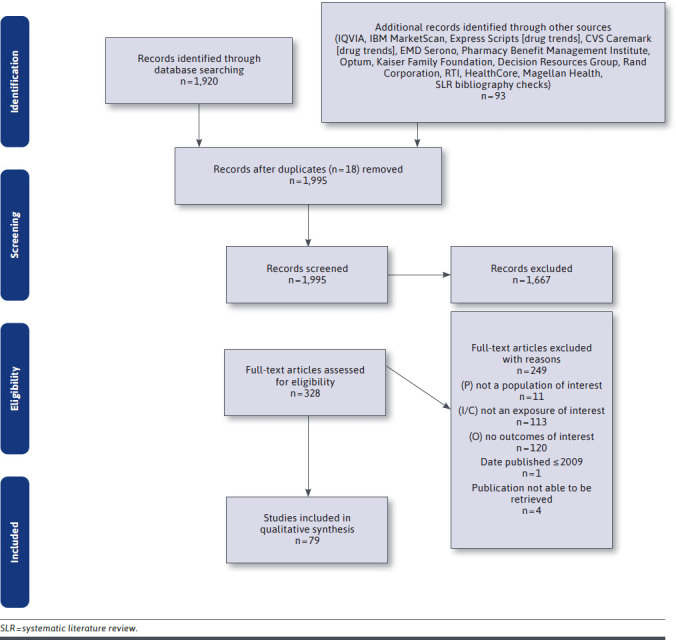
Literature Selection and Review Process
Across publications based on claims databases, a large number of plans and plan designs were included. Specific cost-sharing elements (eg, high-deductible, copay levels) varied even within a publication. However, in terms of the analyses conducted across studies, different copay levels were most often the cost-sharing factor evaluated (eg, the effect of a $0 copay, association between varying levels of copay amounts, etc). Cost differences ranged from a $2.65 difference in copay up to a greater than $3,000 difference in annual OOP costs.
Across the studies, a majority reported data on costsharing and adherence (71 of 79, 90%). Fewer studies addressed the additional review questions; 16 (20%) reported data on cost-sharing and HRU or medication initiation, 11 (14%) on cost-sharing and health care costs, and 6 (8%) on cost-sharing and clinical outcomes.
COST-SHARING AND DRUG TREATMENT ADHERENCE, PERSISTENCE, AND DISCONTINUATION
Of the 71 articles reporting data on the relationship between cost-sharing and treatment adherence, persistence, and/or discontinuation, adherence was the most commonly reported outcome. Adherence outcomes were reported in 63 of 71 (89%) publications; persistence and discontinuation were each reported in 19 of 71 (27%) articles.
Despite heterogeneity in disease, study design, patient characteristics, and outcome definition, the relationship between higher OOP costs and adherence, persistence, and discontinuation results was relatively consistent across included studies. The majority of publications found that increased cost-sharing was associated with worse adherence (84% of studies), persistence (79% of studies), or discontinuation (58% of studies) (Figure 2). This finding was generally consistent across disease areas (Supplementary Table 4 (393KB, pdf) ).
FIGURE 2.
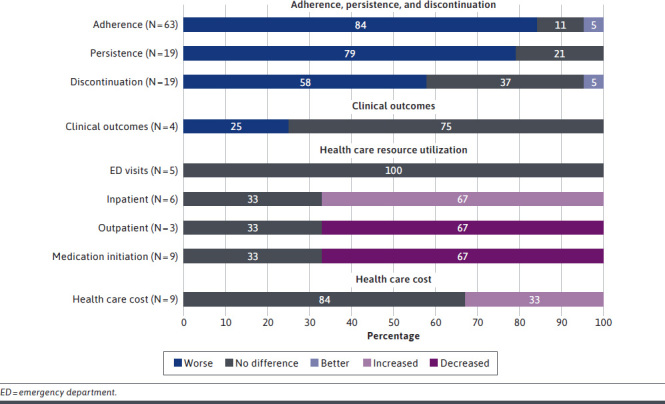
Relationship Between Increased Cost-Sharing and Outcomes of Interest
When taken together, the included studies appear to suggest not only that increased cost-sharing is associated with decreased adherence but also that there is a “dose-response” relationship, in which larger differences in cost-sharing were associated with worse adherence (Figure 3, Supplementary Figure 1 (393KB, pdf) ). Similarly, increased cost-sharing was associated with more patients discontinuing treatment (Supplementary Figure 2 (393KB, pdf) ).
FIGURE 3.
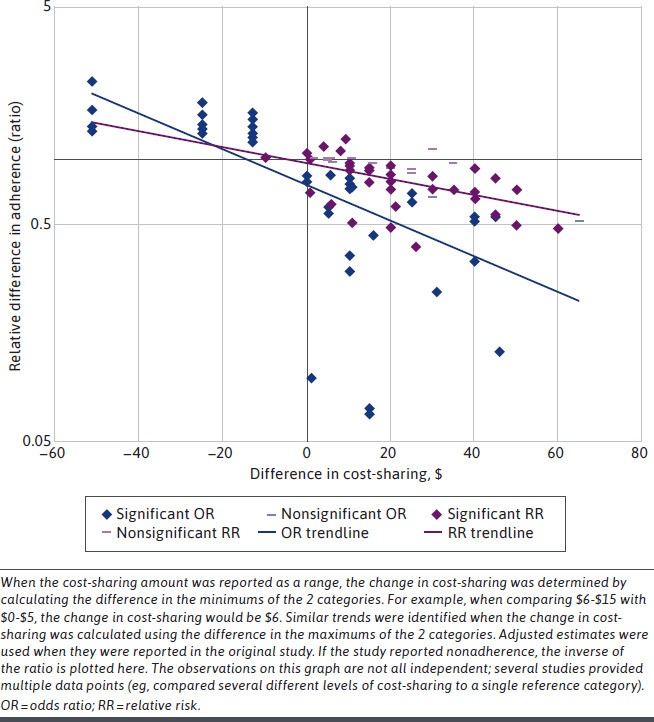
Relative Change in Adherence by Change in Cost-Sharing
The effect of increased cost-sharing may differ by disease. Although most disease areas were not studied frequently enough to identify trends, results among oncology, diabetes, and cardiovascular diseases were each reported in at least 15% of articles reporting on adherence. The relationship between cost-sharing and adherence appears to be somewhat stronger in studies in which patients are being treated for cardiovascular disease, compared with patients receiving oncology or diabetes treatments.
COST-SHARING AND CLINICAL OUTCOMES
Data on the association between cost-sharing and clinical outcomes were reported in 6 articles,32,60,89,90,92,94 representing 4 unique studies (the results of the MI FREEE trial were reported in 3 articles89,90,92). Across the 4 studies, cost-sharing was evaluated as either the effect of copayment removal (n = 3) or copayment differences (n = 1; ie, <$50 vs ≥$50) (Supplementary Table 5 (393KB, pdf) ).
A significant association between higher cost-sharing and worse clinical outcomes was found in only 1 of the 4 studies (the MI FREEE trial) (Figure 2). In that study, copay elimination for patients discharged from the hospital following myocardial infarction had statistically significantly fewer major vascular events, revascularizations, or strokes compared with patients with usual cost-sharing (eg, <$25).89 Additional analyses and subgroup analyses found that the significant reductions in clinical outcomes were specific to non-White patients (Black or African American; Hispanic; American Indian or Alaska Native; Asian, native Hawaiian, or other Pacific Islander; and ≥ 2 races). The study authors noted that “because the numbers in specific race and ethnicity categories were small, patients were classified as being white or nonwhite so that there would be enough statistical power to detect clinically meaningful effects.”89,90,92
The other 3 studies found no significant association between cost-sharing and clinical outcomes. One study compared the use of copay vouchers vs standard copayments (median monthly voucher value of $137) for blood thinners with respect to major adverse cardiovascular events. The second study compared eliminating copays vs standard copay amounts (eg, $10 for generics, $25 for preferred brands, and $50 for nonformulary treatments) for diabetes treatments on blood sugar levels at 1 year. The third study compared lower vs higher monthly copays (<$50 vs ≥$50) for HIV preexposure prophylaxis and found no statistically significant differences in kidney function markers.
COST-SHARING AND HRU
The association between cost-sharing and HRU was reported in 7 studies.32,44,49,52,69,71,78 In 4 of those studies, cost-sharing was evaluated as a difference in copay amount (eg, $10 vs 50 copay, mean copays of $30 vs $54, and copay percentiles ranging from $100 to $190).44,49,69,78 In 2 studies, HRU following a copay reduction (eg, $0 copay or lower copays as part of a value-based insurance benefit) was reported.32,52 Finally, 1 study compared HRU between patients with lower vs higher annual deductibles (eg, <$5,000 or >$5,000)71 (Supplementary Table 6 (393KB, pdf) ). Studies evaluated various utilization: inpatient hospitalizations (6 studies), outpatient care (3 studies), and ED visits (5 studies).
The relationship between higher cost-sharing and HRU was specific to the type of utilization evaluated. Four of the 6 studies evaluating hospitalization use found increased cost-sharing was statistically significantly associated with increased hospitalizations.32,44,49,52,69,78 In 2 of the 3 studies44,69,71 in which outpatient care was assessed, increased cost-sharing was statistically significantly associated with fewer ambulatory visits. In contrast, none of the 5 studies that assessed cost-sharing and ED visits found a statistically significant association (Figure 2).32,44,49,52,69
The association between costsharing and medication initiation was examined in 9 studies (Supplementary Table 7 (393KB, pdf) ).39,54,59,64,65,69,71,85,99 Two studies evaluated contraception uptake after the removal of copays, afforded by the Affordable Care Act, and did not find that removing copays increased contraception initiation.54,64 The remaining 7 studies looked at the association between increased costsharing (assessed as >$29 copays vs ≤$29; a $10 increase in copay; ≥$1 vs no copay; or maximum annual OOP costs of ≤$3,000 vs >$3,000; an HMO plan vs high-deductible health plan benefit design, and a low-deductible vs high-deductible health plan) and medication initiation or vaccinations. Among those 7 studies, 6 found that increased cost-sharing was associated with decreased initiation.39,59,65,71,85,99
COST-SHARING AND HEALTH CARE COSTS
The association between cost-sharing and health care costs was reported in 11 articles (9 studies; 3 articles report data from the MI FREEE trial).23,25,29,32,44,49,52,78,89,90,92 The costs considered included pharmacy (7 studies), medical (5 studies), and total health care (4 studies), as well as the payment perspective (insurer/plan-paid vs patient paid) (Supplementary Table 8 (393KB, pdf) ). Three of the 9 studies found significant associations between increased costsharing and higher health care costs.
Seven studies evaluated the association between cost-sharing and patient- and plan-paid pharmacy costs. Most (5 of 7) studies evaluated changes in cost-sharing for diabetes and cardiovascular treatments. The evidence suggests that reduced patient OOP costs are associated with lower patient pharmacy OOP costs, increased plan-paid pharmacy costs, and a neutral effect on total pharmacy costs in most but not all studies. For example, broader Medicare Part D coverage providing lower overall patient OOP costs increased Medicare-paid pharmacy costs.23 In a second study, increasing copays from $10 to $50 decreased insurer-paid prescription costs.78 However, coupons did not affect patient or plan-paid pharmacy costs in the third study.29 Finally, lowering OOP costs through the elimination of copays (n = 2),32,52 and removal of copays for patients switching to generics (n = 2),25,89,90,92 or through a value-based insurance design had improved employer costs in 1 study, had no difference in total pharmacy costs in 2 studies, and worse (eg, higher) pharmacy costs in a fourth study.
Of the 5 studies that reported on the association between cost-sharing and medical costs, the results were mixed. One study found that increased cost-sharing (raising prescription costs from $10 to $50) was associated with increased hospitalization costs.78 A second study found no difference in hospitalization costs between low vs high annual OOP medication costs.49 Similarly, 2 studies that evaluated the elimination of copays found no significant change in plan total medical costs.32,89,90,92 Finally, 1 study that compared copay reductions plus nurse counseling with a control group of usual care without copay reductions, found that higher OOP costs for the control group were associated with higher overall medical costs.52
Overall, 4 studies evaluated the impact of cost-sharing on total health care costs. One study found the inclusion of Medicare Part D coverage (resulting in lower OOP costs) did not affect total health care costs.23 Similarly, 2 additional studies found higher cost-sharing (eg, $10 copay increase in 1 study or the effect of copay removal) found no impact on total health care costs.49,89,90,92 In 1 study, plan type differentially impacted total health care costs, with a fixed copay being associated with greater adjusted mean total health care costs compared with coinsurance.44 The evidence suggests that increased patient cost-sharing, although associated with decreased insurer-paid pharmacy costs, has an overall neutral to negative (ie, increased payer costs) effect on total health care costs.
Discussion
In this SLR, we sought to understand if the published literature provided answers to the questions of whether cost-sharing for prescription drugs was associated with medication adherence, clinical outcomes, health care utilization, and costs. We found a consistent inverse relationship between cost-sharing and worse adherence across many studies. Higher cost-sharing was consistently associated with lower adherence to prescribed medication. The association persisted regardless of the condition/patient population under study or type of cost-sharing (eg, copays, coinsurance, deductibles). The aggregate data also suggested that larger increases in cost-sharing were associated with worse adherence. The aggregate data suggest that increased cost-sharing may be associated with decreased outpatient visits but increased hospitalizations and no association with ED visits. Thus, the evidence found in this review support a hypothesis that there is an association between increased cost-sharing and prescription adherence and outpatient care, which in turn could be associated with increased hospitalizations. Missing from this hypothesized relationship was an association between increased cost-sharing and poorer clinical outcomes. We found very limited published data on cost-sharing and clinical morbidity, and of the studies found, most did not report a statistically significant association. Overall, increased costsharing did not appear to decrease health care costs.
The relationship between cost-sharing and adherence found in this SLR is consistent with that found 50 years ago in the HIE. Additionally, the results in this review regarding prescription abandonment and adherence with the magnitude of the effect differing by the clinical condition were consistent with those of previous reports. For example, Doshi31 found initiation of specialty drugs for cancer was less sensitive than for other conditions such as rheumatoid arthritis or multiple sclerosis. We also found that increased cost-sharing was associated with a lower likelihood of initiating treatments. Likewise, the HIE found that cost-sharing had a greater effect on initiation of health care services than it did on the continuation of services.2 Although we found only limited data linking cost-sharing to disease morbidity, an analysis conducted by the National Bureau of Economic Research (published after the searches were completed for this SLR) found that increased OOP prescription costs both decreased adherence and increased mortality.100 Notably, the Congressional Budget Office estimated that for every 10% increase in prescription medication use, Medicare spending on medical services is reduced by 2%.101
Cost-sharing is not only intended to lower costs of payers and employers by apportioning part of pharmacy and HRU expenditures to the beneficiary, but also to lower health care costs overall by addressing the “moral hazard” in health care behavior. That is, if patients are aware of and responsible for the costs associated with medications and health care services, they may be more selective in their choices (opting out of treatments with little evidence of effectiveness and choosing less expensive prescription drugs when given a choice). However, the evidence in this review suggests that patients fail to start and continue therapies based on cost burden alone. Critics of cost-sharing submit that patients will not rationally dissect the pros and cons of different treatments in the face of emergencies, nor will they second guess a doctor’s prescribed treatment, and that the disconnect between health care prices vs actual costs complicates patients’ ability to compare different available therapies.102 It has been posited that the moral hazard theory is ill-suited for health behaviors and that it is a flawed proposition that insurance affords patients additional capital to use superfluous health care.102
A paradoxical effect of cost-sharing is that it may ultimately increase health care costs because patients waive essential health care, which in the long-term results in poorer health and therefore necessitates medical treatments, utilization, and procedures that may have been avoided.102 The limited data we found suggested that cost-sharing does not result in the intended goal of reducing overall health care costs. In most studies, increased cost-sharing had a neutral impact, neither increasing or decreasing health care costs, whereas being associated with poorer health care outcomes. In select studies, there was evidence of higher medical costs being associated with higher patient cost-sharing. For example, Snider78 found that higher copays were associated with significant reductions in pharmacy costs but greater hospitalization costs and total costs. Kim52 found that medical costs were significantly lower following a value-based insurance design copay reduction, despite higher pharmacy costs. In terms of clinical outcomes, the MI FREEE trial found that removal of medication copays was associated with some decrease in important cardiovascular events; no significant association was found between cost-sharing and clinical outcomes in 3 other studies of different patient populations. In terms of health care utilization, the limited published evidence suggests that higher cost-sharing was associated with greater inpatient and lower outpatient utilization and no association with ED visits.
LIMITATIONS
The limitations associated with this review and the relationship between cost-sharing and outcomes are many. First, our review was limited to published studies. Results from abstracts and unpublished results were not included. Second, we used a broad definition for cost-sharing. The type (eg, deductible, coinsurance, and copay) and magnitude (eg, $5, $50, or >$5,000 deductible) of cost-sharing were not homogenous. Third, the outcome definitions varied (eg, the proportion of days covered, medication possession ratios, or specific thresholds for treatment adherence, etc), making comparisons across publications difficult. Fourth, the association between cost-sharing and outcomes may be differentially affected by the specific health condition a patient has, by insurance population (eg, Medicare Part D vs commercial or high-deductible health plans), or by patient characteristics,103 including income, health status, and race and ethnicity, each of which has been shown to be related to overall health care use and other factors.
In the commercial market, certain benefit designs seek to lower cost-sharing for some or all patients. For example, a recent Internal Revenue Service rule allows certain employer-sponsored high-deductible health plans to offer an expanded list of preventive medications at a lower or no cost prior to satisfying the plan deductible. Other benefit designs, including several in this review, aim to reduce or eliminate copays for high-value services. As others have hypothesized, the benefits of reducing or eliminating for select services may not have an equal but opposite impact on health care service use. Tools such as these move from cost-sharing as a blunt tool to a nuanced approach to encourage high-value care.
POLICY IMPLICATIONS
In the public policy dialogues, many recognize that OOP costs can be burdensome. In the Medicare prescription drug program, the Low-Income Subsidy limits cost-sharing for those who are at less than 150% of the federal poverty level. For those under less than 135%, the most they would pay for a brand product in 2021 is $9.20104; however, for those who do not qualify for this subsidy, catastrophic coverage is only permitted after paying $6,550 in prescription drugs. Recent discussions in Congress surround implementing an annual OOP cap, with the potential for “smoothing,” which could spread the cost of the annual OOP over the course of many months, with a cap in monthly spending.105
The connection between OOP and patients is appreciated by a number of states. Some states have implemented patient protections for certain plans to include no deductible for prescription drugs or capping the amount per month in OOP drug costs. Unlike the conditions most frequently studied in this review (eg, cardiovascular, diabetes), most states address OOP costs associated with specialty medications. A recent publication evaluated 3 states that capitated OOP costs for specialty medications and found lower beneficiary costs without raising total health care spending.106
Conclusions
Cost-sharing was developed to reduce unnecessary use of health care services and reduce total health care spending. The published literature shows a consistent impact of higher cost-sharing on initiation and continuation of medications, and the greater the cost-sharing, the worse the medication adherence. The evidence is more limited regarding the impact of cost-sharing on clinical outcomes, resource use, and total health care costs. Although the limited published evidence suggests that higher costsharing was associated with greater inpatient and lower outpatient utilization, it also suggests a neutral to no difference in other outcomes. Today’s growing environment of health care cost-containment should carefully consider the broader impact costsharing has on treatment adherence, clinical outcomes, resource use, and total health care costs. It may be that cost-sharing is a blunt, rather than precise, tool to curb health care costs, affecting both necessary and unnecessary health care use. Findings from the decades-old HIE hold today.
REFERENCES
- 1.RAND Corporation. RAND’s Health Insurance Experiment (HIE). Accessed March 9, 2021. https://www.rand.org/health-care/projects/hie.html
- 2.Brook RH, Keeler EB, Lohr KN, et al. . The health insurance experiment: a classic RAND study speaks to the current health care reform debate. RAND Corporation; 2006. Accessed March 16, 2021. https://www.rand.org/pubs/research_briefs/RB9174.html [Google Scholar]
- 3.Rice T, Quentin W, Anell A, et al. . Revisiting out-of-pocket requirements: trends in spending, financial access barriers, and policy in ten high-income countries. BMC Health Services Research. 2018;18(1):371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Claxton G, Rae M, Young G, McDermott D. Employer Health Benefits – 2020 Annual Survey. Kaiser Family Foundation; 2020. Accessed March 9, 2021. https://files.kff.org/attachment/Report-Employer-Health-Benefits-2020-Annual-Survey.pdf [Google Scholar]
- 5.Rae M, Copeland R, Cox C. Tracking the rise in premium contributions and cost-sharing for families with large employer coverage: Access & affordability. 2019. Accessed March 9, 2021. https://www.healthsystemtracker.org/brief/tracking-the-rise-in-premium-contribu-tions-and-cost-sharing-for-families-with-large-employer-coverage/
- 6.Hayes SL, Collins SR, Radley DC. How much US households with employer insurance spend on premiums and out-of-pocket costs: a state-by-state look. The Commonwealth Fund. Issue Briefs. May 23, 2019. Accessed March 9, 2021. https://www.commonwealthfund.org/publications/issue-briefs/2019/may/how-much-us-households-employer-insurance-spend-premiums-out-of-pocket [Google Scholar]
- 7.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61-9. doi:10.1001/jama.298.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aziz H, Hatah E, Makmor Bakry M, Islahudin F. How payment scheme affects patients’ adherence to medications? A systematic review. Patient Prefer Adherence. 2016;10:837-50. doi:10.2147/PPA.S103057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eaddy MT, Cook CL, O’Day K, Burch SP, Cantrell CR. How patient cost-sharing trends affect adherence and outcomes: a literature review. P T. 2012;37(1):45-55. [PMC free article] [PubMed] [Google Scholar]
- 10.Yu AP, Yu YF, Nichol MB. Estimating the effect of medication adherence on health outcomes among patients with type 2 diabetes–an application of marginal structural models. Value Health. 2010;13(8):1038-45. doi:10.1111/j.1524-4733.2010.00787.x [DOI] [PubMed] [Google Scholar]
- 11.Simpson SH, Lin M, Eurich DT. Medication adherence affects risk of new diabetes complications: a cohort study. Ann Pharmacother. 2016;50(9):741-6. doi:10.1177/1060028016653609 [DOI] [PubMed] [Google Scholar]
- 12.Han E, Suh DC, Lee SM, Jang S. The impact of medication adherence on health outcomes for chronic metabolic diseases: a retrospective cohort study. Res Social Adm Pharm. 2014;10(6):e87-98. doi:10.1016/j.sapharm.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 13.Walsh CA, Cahir C, Tecklenborg S, Byrne C, Culbertson MA, Bennett KE. The association between medication nonadherence and adverse health outcomes in ageing populations: A systematic review and meta-analysis. Br J Clin Pharmacol. 2019;85(11):2464-78. doi:10.1111/bcp.14075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neiman AB, Ruppar T, Ho M, et al. . CDC grand rounds: improving medication adherence for chronic disease management – innovations and opportunities. MMWR Morb Mortal Wkly Rep. 2018;18(2)514-47. doi:10.1111/ajt.14649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haren MC, McConnell K. Patient cost-sharing on the rise: results from the benefit design index. Am Health Drug Benefits. 2009;2(2):70-7. [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Motheral B, Brooks J, Clark MA, et al. . A checklist for retrospective database studies–report of the ISPOR Task Force on Retrospective Databases. Value Health. 2003;6(2):90-7. doi:10.1046/j.1524-4733.2003.00242.x [DOI] [PubMed] [Google Scholar]
- 18.Lockwood C MZ, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179-87. doi:10.1097/XEB.0000000000000062 [DOI] [PubMed] [Google Scholar]
- 19.Wells GA, Shea B, O’Connell D, et al. . The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. The Ottawa Hospital. Accessed March 9, 2021. http://www.ohrica/programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 20.Higgins JPT, Altman DG, Gøtzsche PC, et al. . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi:10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adams AS, Uratsu C, Dyer W, et al. . Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA Internal Medicine. 2013;173(1):54-61. doi:10.1001/2013.jamainternmed.955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bibeau WS, Fu H, Taylor AD, Kwan AY. Impact of out-of-pocket pharmacy costs on branded medication adherence among patients with type 2 diabetes. J Manag Care Spec Pharm. 2016;22(11):1338-47. doi:10.18553/jmcp.2016.22.11.1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng LI, Rascati KL. Impact of Medicare part D for Medicare-age adults with arthritis: prescription use, prescription expenditures, and medical spending from 2005 to 2008. Arthritis Care Res (Hoboken). 2012;64(9):1423-9. doi:10.1002/acr.21696 [DOI] [PubMed] [Google Scholar]
- 24.Chin AL, Bentley JP, Pollom EL. The impact of state parity laws on copayments for and adherence to oral endocrine therapy for breast cancer. Cancer. 2019;125(3):374-81. doi:10.1002/cncr.31910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clark B, DuChane J, Hou J, Rubinstein E, McMurray J, Duncan I. Evaluation of increased adherence and cost savings of an employer value-based benefits program targeting generic antihyperlipidemic and antidiabetic medications. J Manag Care Spec Pharm. 2014;20(2):141-50. doi:10.18553/jmcp.2014.20.2.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conwell LJ, Esposito D, Garavaglia S, et al. . Out-of-pocket drug costs and drug utilization patterns of postmenopausal Medicare beneficiaries with osteoporosis. Am J Geriatr Pharmacother. 2011;9(4): 241-9. doi:10.1016/j.amjopharm.2011.04.009 [DOI] [PubMed] [Google Scholar]
- 27.Coy KC, Hazen RJ, Kirkham HS, Delpino A, Siegler AJ. Persistence on HIV preexposure prophylaxis medication over a 2-year period among a national sample of 7,148 PrEP users, United States, 2015 to 2017. J Int AIDS Soc. 2019;22(2):e25252. doi:10.1002/jia2.25252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Darkow T, Maclean R, Joyce GF, Goldman D, Lakdawalla DN. Coverage and use of cancer therapies in the treatment of chronic myeloid leukemia. Am J Manag Care. 2012;18(11 Suppl):S272-8. [PubMed] [Google Scholar]
- 29.Daubresse M, Andersen M, Riggs KR, Alexander GC. Effect of prescription drug coupons on statin utilization and expenditures: a retrospective cohort study. Pharmacotherapy. 2017;37(1):12-24. doi:10.1002/phar.1802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davis AM, Taitel MS, Jiang J, et al. . A national assessment of medication adherence to statins by the racial composition of neighborhoods. J Racial Ethn Health Disparities. 2017;4(3):462-71. doi:10.1007/s40615-016-0247-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doshi JA, Li P, Huo H, Pettit AR, Armstrong KA. Association of patient out-of-pocket costs with prescription abandonment and delay in fills of novel oral anticancer agents. J Clin Oncol. 2018;36(5):476-82. doi:10.1200/JCO.2017.74.5091 [DOI] [PubMed] [Google Scholar]
- 32.Elliott DJ, Robinson EJ, Anthony KB, Stillman PL. Patient-centered outcomes of a value-based insurance design program for patients with diabetes. Popul Health Manag. 2013;16(2):99-106. doi:10.1089/pop.2012.0031 [DOI] [PubMed] [Google Scholar]
- 33.Engel-Nitz NM, Satram-Hoang S, Cao F, Reyes CM. Lung cancer: Copayments and behavior following erlotinib formulary tier change. Am J Pharm Benefits. 2012;4(6):SP6-17. [Google Scholar]
- 34.Farias AJ, Du XL. Association between out-of-pocket costs, race/ethnicity, and adjuvant endocrine therapy adherence among Medicare patients with breast cancer. J Clin Oncol. 2017;35(1):86-95. doi:10.1200/JCO.2016.68.2807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farias AJ, Hansen RN, Zeliadt SB, Ornelas IJ, Li CI, Thompson B. The association between out-of-pocket costs and adherence to adjuvant endocrine therapy among newly diagnosed breast cancer patients. Am J Clin Oncol. 2018;41(7): 708-15. doi:10.1097/COC.0000000000000351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fendrick AM, Buxbaum JD, Tang Y, et al. . Association between switching to a high-deductible health plan and discontinuation of type 2 diabetes treatment. JAMA Network Open. 2019;2(11):e1914372. doi:10.1001/jamanetworkopen.2019.14372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fowler NR, Chen YF, Thurton CA, Men A, Rodriguez EG, Donohue JM. The impact of Medicare prescription drug coverage on the use of antidementia drugs. BMC Geriatr. 2013;13:37. doi:10.1186/1471-2318-13-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Franklin JM, Mahesri M, Krumme AA, et al. . Time to filling of new prescriptions for chronic disease medications among a cohort of elderly patients in the USA. J Gen Intern Med. 2018;33(11):1877-84. doi:10.1007/s11606-018-4592-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gibson TB, Jing Y, Bagalman JE, et al. . Impact of cost-sharing on treatment augmentation in patients with depression. Am J Manag Care. 2012;18(1):e15-22. [PubMed] [Google Scholar]
- 40.Gibson TB, Jing Y, Kim E, et al. . Cost-sharing effects on adherence and persistence for second-generation antipsychotics in commercially insured patients. Manag Care. 2010;19(8):40-7. [PubMed] [Google Scholar]
- 41.Gibson TB, Song X, Alemayehu B, et al. . Cost sharing, adherence, and health outcomes in patients with diabetes. Am J Manag Care. 2010;16(8):589-600. [PubMed] [Google Scholar]
- 42.Goedken AM, Urmie JM, Farris KB, Doucette WR. Impact of cost sharing on prescription drugs used by Medicare beneficiaries. Res Social Adm Pharm. 2010;6(2):100-9. doi:10.1016/j.sapharm.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 43.Gor D, Lee TA, Schumock GT, et al. . Adherence and persistence with DPP-4 inhibitors versus pioglitazone in type 2 diabetes patients with chronic kidney disease: A retrospective claims database analysis. J Manag Care Spec Pharm. 2020;26(1):67-75P. doi:10.18553/jmcp.2020.26.1.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henk HJ, Lopez JMS, Bookhart BK. Novel type 2 diabetes medication access and effect of patient cost sharing. J Manag Care Spec Pharm. 2018;24(9):847-55. doi:10.18553/jmcp.2018.24.9.847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hershman DL, Tsui J, Wright JD, Coromilas EJ, Tsai WY, Neugut AI. Household net worth, racial disparities, and hormonal therapy adherence among women with early-stage breast cancer. J Clin Oncol. 2015;33(9):1053-9. doi:10.1200/JCO.2014.58.3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hopson S, Saverno K, Liu LZ, et al. . Impact of out-of-pocket costs on prescription fills among new initiators of biologic therapies for rheumatoid arthritis. J Manag Care Spec Pharm. 2016;22(2):122-30. doi:10.18553/jmcp.2016.14261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnson JT, Neill KK, Davis DA. Five-year examination of utilization and drug cost outcomes associated with benefit design changes including reference pricing for proton pump inhibitors in a state employee health plan. J Manag Care Pharm. 2011;17(3):200-12. doi:10.18553/jmcp.2011.17.3.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johnston SS, Juday T, Seekins D, Espindle D, Chu BC. Association between prescription cost sharing and adherence to initial combination antiretroviral therapy in commercially insured antiretroviral-naïve patients with HIV. J Manag Care Pharm. 2012;18(2):129-45. doi:10.18553/jmcp.2012.18.2.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Karaca-Mandic P, Jena AB, Joyce GF, Goldman DP. Out-of-pocket medication costs and use of medications and health care services among children with asthma. JAMA. 2012;307(12):1284-91. doi:10.1001/jama.2012.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karter AJ, Parker MM, Solomon MD, et al. . Effect of out-of-pocket cost on medication initiation, adherence, and persistence among patients with type 2 diabetes: the diabetes study of northern California (DISTANCE). Health Serv Res. 2018;53(2):1227-47. doi:10.1111/1475-6773.12700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim J, Rajan SS, Du XL, Franzini L, Giordano SH, Morgan RO. Association between financial burden and adjuvant hormonal therapy adherence and persistent use for privately insured women aged 18–64 years in BCBS of Texas. Breast Cancer Res Treat. 2018;169(3):573-86. doi:10.1007/s10549-018-4704-3 [DOI] [PubMed] [Google Scholar]
- 52.Kim YA, Loucks A, Yokoyama G, Lightwood J, Rascati K, Serxner SA. Evaluation of value-based insurance design with a large retail employer. Am J Manag Care. 2011;17(10):682-90. [PubMed] [Google Scholar]
- 53.Kim YA, Rascati KL, Prasla K, Godley P, Goel N, Dunlop D. Retrospective evaluation of the impact of copayment increases for specialty medications on adherence and persistence in an integrated health maintenance organization system. Clin Ther. 2011;33(5):598-607. doi:10.1016/j. clinthera.2011.04.021 [DOI] [PubMed] [Google Scholar]
- 54.Law A, Wen L, Lin J, Tangirala M, Schwartz JS, Zampaglione E. Are women benefiting from the Affordable Care Act? A real-world evaluation of the impact of the Affordable Care Act on out-of-pocket costs for contraceptives. Contraception. 2016;93(5):392-7. doi:10.1016/j.contraception.2016.01.008 [DOI] [PubMed] [Google Scholar]
- 55.Lee C, Grigorian M, Nolan R, Binder G, Rice G.. A retrospective study of direct cost to patients associated with the use of oral oncology medications for the treatment of multiple myeloma. J Med Econ. 2016;19(4):397-402. doi:10.3111/13696998.2 015.1130710 [DOI] [PubMed] [Google Scholar]
- 56.Lewey J, Gagne JJ, Franklin J, Lauffenburger JC, Brill G, Choudhry NK. Impact of high deductible health plans on cardiovascular medication adherence and health disparities. Circ Cardiovasc Qual Outcomes. 2018;11(11):e004632. doi:10.1161/CIRCOUTCOMES.118.004632 [DOI] [PubMed] [Google Scholar]
- 57.Lewey J, Shrank WH, Avorn J, Liu J, Choudhry NK. Medication adherence and healthcare disparities: impact of statin co-payment reduction. Am J Manag Care. 2015;21(10):696-704. [PubMed] [Google Scholar]
- 58.MacEwan JP, Sheehan JJ, Yin W, et al. . The relationship between adherence and total spending among Medicare beneficiaries with type 2 diabetes. Am J Manag Care. 2017;23(4):248-52. [PubMed] [Google Scholar]
- 59.Marcus JL, Hurley LB, Chamberland S, et al. . Disparities in initiation of direct-acting antiviral agents for hepatitis c virus infection in an insured population. Public Health Rep. 2018;133(4):452-60. doi:10.1177/0033354918772059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marcus JL, Hurley LB, Hare CB, et al. . Preexposure prophylaxis for HIV prevention in a large integrated health care system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr. 2016;73(5):540-6. doi:10.1097/QAI.0000000000001129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marshall C, Schmittdiel J, Chandra M, Calhoun A, Raine-Bennett T. The relationship between prescription copayments and contraceptive adherence in a new-user cohort. Med Care. 2018;56(7):577-82. doi:10.1097/MLR.0000000000000921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McClellan C, Fingar KR, Ali MM, Olesiuk WJ, Mutter R, Gibson TB. Price elasticity of demand for buprenorphine/naloxone prescriptions. J Subst Abuse Treat. 2019;106:4-11. doi:10.1016/j. jsat.2019.08.001 [DOI] [PubMed] [Google Scholar]
- 63.Neugut AI, Subar M, Wilde ET, et al. . Association between prescription copayment amount and compliance with adjuvant hormonal therapy in women with early-stage breast cancer. J Clin Oncol. 2011;29(18):2534-42. doi:10.1200/JCO.2010.33.3179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pace LE, Dusetzina SB, Keating NL. Early impact of the affordable care act on uptake of long-acting reversible contraceptive methods. Med Care. 2016;54(9):811-7. doi:10.1097/MLR.0000000000000551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Palmer L, Abouzaid S, Shi N, et al. . Impact of patient cost sharing on multiple sclerosis treatment. Am J Pharm Benefits. 2012;4(6):SP29-36. [Google Scholar]
- 66.Patterson ME, Blalock SJ, Smith AJ, Murray MD. Associations between prescription copayment levels and ß-blocker medication adherence in commercially insured heart failure patients 50 years and older. Clin Ther. 2011;33(5):608-16. doi:10.1016/j.clinthera.2011.04.022 [DOI] [PubMed] [Google Scholar]
- 67.Pawaskar MD, Xu L, Tang Y, Puckrein GA, Rajpathak SN, Stuart B. Effect of medication copayment on adherence and discontinuation in Medicare beneficiaries with type 2 diabetes: a retrospective administrative claims database analysis. Diabetes Ther. 2018;9(5):1979-93. doi:10.1007/s13300-018-0489-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pesa JA, Van Den Bos J, Gray T, et al. . An evaluation of the impact of patient cost sharing for antihypertensive medications on adherence, medication and health care utilization, and expenditures. Patient Prefer Adherence. 2012;6:63-72. doi:10.2147/PPA.S28396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Phuar HL, Begley CE, Chan W, Krause TM. Tyrosine kinase inhibitors initiation, cost sharing, and health care utilization in patients with newly diagnosed chronic myeloid leukemia: a retrospective claims-based study. J Manag Care Spec Pharm. 2019;25(10):1140-50. doi:10.18553/jmcp.2019.25.10.1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reynolds K, An J, Wu J, et al. . Treatment discontinuation of oral hypoglycemic agents and healthcare utilization among patients with diabetes. J Diabetes Complications. 2016;30(8):1443-51. doi:10.1016/j.jdiacomp.2016.07.021 [DOI] [PubMed] [Google Scholar]
- 71.Roblin DW, Ritzwoller DP, Rees DI, Carroll NM, Chang A, Daley MF. The influence of deductible health plans on receipt of the human papillomavirus vaccine series. J Adolesc Health. 2014;54(3):275-81. doi:10.1016/j.jadohealth.2013.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Romley J, Goldman D, Eber M, Dastani H, Kim E, Raparla S. Cost-sharing and initiation of disease-modifying therapy for multiple sclerosis. Am J Manag Care. 2012;18(8):460-4. [PubMed] [Google Scholar]
- 73.Saito EP, Davis JW, Harrigan RC, Juarez D, Mau MK. Copayment level and drug switching: findings for type 2 diabetes. Am J Pharm Benefits. 2010;2(7):412-20. [Google Scholar]
- 74.Sambamoorthi U, Garg R, Deb A, Fan T, Boss A. Persistence with rapidacting insulin and its association with A1C level and severe hypoglycemia among elderly patients with type 2 diabetes. Curr Med Res Opin. 2017;33(7):1309-16. doi:10.10 80/03007995.2017.1318121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schmittdiel JA, Nichols GA, Dyer W, Steiner JF, Karter AJ, Raebel MA. Health care system-level factors associated with performance on medicare STAR adherence metrics in a large, integrated delivery system. Med Care. 2015;53(4):332-7. doi:10.1097/MLR.0000000000000328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shah NB, Mitchell RE, Proctor ST, et al. . High rates of medication adherence in patients with pulmonary arterial hypertension: An integrated specialty pharmacy approach. PLoS ONE. 2019;14(6):e0217798. doi:10.1371/journal.pone.0217798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shrank WH, Choudhry NK, Fischer MA, et al. . The epidemiology of prescriptions abandoned at the pharmacy. Ann Intern Med. 2010;153(10):633-40. doi:10.7326/0003-4819-153-10-201011160-00005 [DOI] [PubMed] [Google Scholar]
- 78.Snider JT, Seabury S, Lopez J, McKenzie S, Wu Y, Goldman DP. Impact of type 2 diabetes medication cost sharing on patient outcomes and health plan costs. Am J Manag Care. 2016;22(6):433-40. [PubMed] [Google Scholar]
- 79.Starner CI, Alexander GC, Bowen K, Qiu Y, Wickersham PJ, Gleason PP. Specialty drug coupons lower out-ofpocket costs and may improve adherence at the risk of increasing premiums. Health Aff (Millwood). 2014;33(10):1761-9. doi:10.1377/hlthaff.2014.0497 [DOI] [PubMed] [Google Scholar]
- 80.Stein JD, Shekhawat N, Talwar N, Balkrishnan R. Impact of the introduction of generic latanoprost on glaucoma medication adherence. Ophthalmology. 2015;122(4):738-47. doi:10.1016/j.ophtha.2014.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Taira DA, Seto BK, Davis JW, Seto TB, Landsittel D, Sumida WK. Examining factors associated with nonadherence and identifying providers caring for nonadherent subgroups. J Pharm Health Serv Res. 2017;8(4):247-53. doi:10.1111/jphs.12193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tao Z, Li Y, Stemkowski S, et al. . Impact of out-of-pocket cost on herpes zoster vaccine uptake: an observational study in a Medicare managed care population. Vaccines (Basel). 2018;6(4):78. doi:10.3390/vaccines6040078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Vaidya V, Tak S, Hong SH. Impact of patient cost sharing on medication adherence among asthmatic patients on dual-controller therapy. J Pharm Health Serv Res. 2013;4(4):227-33. doi:10.1111. jphs.12035 [Google Scholar]
- 84.Wang SM, Aranda GA, Gao S, Patel BV. Benefit restrictions and gout treatment. J Manag Care Pharm. 2013;19(9):773-82. doi:10.18553/jmcp.2013.19.9.773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wharam JF, Zhang F, Wallace J, et al. . Vulnerable and less vulnerable women in high-deductible health plans experienced delayed breast cancer care. Health Affairs. 2019;38(3):408-15. doi:10.1377/htlhaff.2018.05026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang W, Kahler KH, Fellers T, et al. . Copayment level, treatment persistence, and healthcare utilization in hypertension patients treated with single-pill combination therapy. J Med Econ. 2011;14(3):267-78. doi:10.3111/13696998.2011.570401 [DOI] [PubMed] [Google Scholar]
- 87.Zeng F, Chen CI, Mastey V, Zou KH, Harnett J, Patel BV. Effects of copayment on initiation of smoking cessation pharmacotherapy: an analysis of varenicline reversed claims. Clin Ther. 2011;33(2):225-34. doi:10.1016/j.clinthera.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 88.Zeng F, Knoth RL, Patel BV, Kim E, Tran QV, Jing Y. Impact of health plan restrictions on antipsychotic medication adherence and persistence. Am J Pharm Benefits. 2012;4(1):e22-31. [Google Scholar]
- 89.Choudhry NK, Avorn J, Glynn RJ, et al. . Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088-97. doi:10.1056/NEJMsa1107913 [DOI] [PubMed] [Google Scholar]
- 90.Choudhry NK, Bykov K, Shrank WH, et al. . Eliminating medication copayments reduces disparities in cardiovascular care. Health Affairs. 2014;34(5):863-70. doi:10.1377/htlhaff.2013.0654 [DOI] [PubMed] [Google Scholar]
- 91.Fanaroff AC, Peterson ED, Kaltenbach LA, et al. . Copayment reduction voucher utilization and associations with medication persistence and clinical outcomes: findings from the ARTEMIS trial. Circ Cardiovasc Qual Outcomes. 2020;13(5):e006182. doi:10.1161/CIRCOUTCOMES.119.006182 [DOI] [PubMed] [Google Scholar]
- 92.Kulik A, Desai NR, Shrank WH, et al. . Full prescription coverage versus usual prescription coverage after coronary artery bypass graft surgery: analysis from the post-myocardial infarction free Rx event and economic evaluation (FREEE) randomized trial. Circulation. 2013;128(11 Suppl 1):S219-25. doi:10.1161/CIRCULATIONAHA.112.000337 [DOI] [PubMed] [Google Scholar]
- 93.Ross-Degnan D, Wallace J, Zhang F, Soumerai SB, Garabedian L, Wharam JF. Reduced cost-sharing for preventive drugs preferentially benefits low-income patients with diabetes in high deductible health plans with health savings accounts. Med Care. 2020;58(Suppl 6 1):S4-13. doi:10.1097/MLR.0000000000001295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang TY, Kaltenbach LA, Cannon CP, et al. . Effect of medication co-payment vouchers on P2Y12 inhibitor use and major adverse cardiovascular events among patients with myocardial infarction: the ARTEMIS Randomized Clinical Trial. JAMA. 2019;321(1):44-55. doi:10.1001/jama.2018.19791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.White Paper. Patient affordability and prescription drugs. The implications of increasing pharmacy cost exposure on patient behavior and the mitigating role of co-pay card programs in the commercial market. IQVIA. August 3, 2018. Accessed March 16, 2021. https://www.iqvia.com/locations/united-states/library/white-papers/patient-affordability-and-prescription-drugs
- 96.Brixner D, Mittal M, Rubin DT, et al. . Participation in an innovative patient support program reduces prescription abandonment for adalimumab-treated patients in a commercial population. Patient Pref Adherence. 2019;13:1545-56. doi:10.2147/PPA.S215037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Burton T, Fan Y, Kwong WJ. Dosing frequency and adherence in patients with nonvalvularatrial fibrillation. Am J Pharm Benefits. 2014;6(2):e31-40. [Google Scholar]
- 98.Buxbaum JD, Chernew ME, Bonafede M, et al. . Cost sharing and branded antidepressant initiation among patients treated with generics. Am J Manag Care. 2018;24(4):180-6. [PubMed] [Google Scholar]
- 99.VanderBeek BL, Scavelli K, Yu Y. Determinants in initial treatment choice for diabetic macular edema. Ophthalmology Retina. 2020;4(1):41-8. doi:10.1016/j.oret.2019.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chandra A, Flack E, Obermeyer Z. The health costs of cost-sharing. National Bureau of Economic Research Working Paper Series. February 2021; No. 28439. Accessed March 16, 2021. https://www.nber.org/system/files/working_papers/w28439/w28439.pdf
- 101.Congressional Budget Office. Offsetting effects of prescription drug use on Medicare’s spending for medical services. 2012. Accessed March 16, 2021. https://www.cbo.gov/sites/default/files/cbofiles/attachments/43741-MedicalOffsets-11-29-12.pdf
- 102.Gould E. Increased health care cost sharing works as intended: it burdens patients who need care the most. Economic Policy Institute. Briefing Paper #358. May 8, 2013. Accessed March 9, 2021. https://www.epi.org/publication/bp358-increased-health-care-cost-sharing-works/ [Google Scholar]
- 103.Swartz K. Cost-sharing: effects on spending and outcomes. Robert Wood Johnson Foundation. 2010. Accessed March 9, 2021. https://www.rwjf.org/en/library/research/2011/12/cost-sharing--effects-on-spending-and-outcomes.html [Google Scholar]
- 104.Shapiro JR. 2021 resource and costsharing limits for Low-Income Subsidy (LIS). 2020. Centers for Medicare and Medicaid Services. Accessed March 16, 2021. https://www.cms.gov/files/document/2021-lis-resource-limits-memo.pdf [Google Scholar]
- 105.Cubanski J, Freed M, Dolan R, Neuman T. What’s the latest on prescription drug proposals from the trump administration, congress, and the Biden campaign? Kaiser Family Foundation. Accessed March 16, 2021. http://files.kff.org/attachment/Slideshow-Latest-Prescription-Drug-Proposals-Trump-Biden-Congress.pdf [Google Scholar]
- 106.Yeung K, Barthold D, Dusetzina SB, Basu A. Patient and plan spending after state specialty-drug out-of pocket spending caps. N Engl J Med. 2020;383(6):558-66. doi:10.1056/NEJMsa1910366 [DOI] [PubMed] [Google Scholar]


