Abstract
Leptospirosis, a zoonosis with worldwide distribution, is caused by pathogenic spirochetes belonging to the genus Leptospira. Bacterial outer membrane proteins (OMPs), particularly those with surface-exposed regions, play crucial roles in pathogen dissemination and virulence mechanisms. Here we characterized the leptospiral Membrane Protein L36 (MPL36), a rare lipoprotein A (RlpA) homolog with a C-terminal Sporulation related (SPOR) domain, as an important virulence factor in pathogenic Leptospira. Our results confirmed that MPL36 is surface exposed and expressed during infection. Using recombinant MPL36 (rMPL36) we also confirmed previous findings of its high plasminogen (PLG)-binding ability determined by lysine residues of the C-terminal region of the protein, with ability to convert bound-PLG to active plasmin. Using Koch’s molecular postulates, we determined that a mutant of mpl36 has a reduced PLG-binding ability, leading to a decreased capacity to adhere and translocate MDCK cell monolayers. Using recombinant protein and mutant strains, we determined that the MPL36-bound plasmin (PLA) can degrade fibrinogen. Finally, our mpl36 mutant had a significant attenuated phenotype in the hamster model for acute leptospirosis. Our data indicates that MPL36 is the major PLG binding protein in pathogenic Leptospira, and crucial to the pathogen’s ability to attach and interact with host tissues during infection. The MPL36 characterization contributes to the expanding field of bacterial pathogens that explore PLG for their virulence, advancing the goal to close the knowledge gap regarding leptospiral pathogenesis while offering a novel potential candidate to improve diagnostic and prevention of this important zoonotic neglected disease.
Author summary
As part of their diverse virulence machinery, bacterial pathogens bind to human plasminogen (PLG) providing them with a proteolytic platform that promotes invasiveness, dissemination, and virulence. Leptospirosis is the leading zoonotic disease in morbidity and mortality worldwide. The burden of this neglected disease will continue to raise given the effects of climate change and social inequality, important drivers of disease. Furthermore, the gap of knowledge regarding leptospiral pathogenesis has negatively impacted the development of sensitive diagnostic tools and effective prevention methods. Previous studies have shown that pathogenic Leptospira, the causative agent of leptospirosis, can interact with PLG through different protein candidates. In this work, we characterized one of those candidates, Membrane Protein L36 (MPL36), as the main leptospiral plasminogen binding protein. Using genetically modified mutants, in vivo, and in vitro assays we provided evidence that MPL36 can bound PLG, promotes adherence to host cells and subsequent translocation, and degrades fibrinogen by converting bound-PLG to PLA, thus essential to leptospiral virulence. This work contributes to the growing field of bacterial pathogens exploring PLG to increase their virulence, while highlighting important new knowledge on leptospiral pathogenesis. MPL36 is an important candidate to be explored on the continued effort to improve diagnostic and prevention of this important zoonotic disease.
Introduction
Interaction with the human plasminogen (PLG) system significantly contributes to the virulence of many bacterial pathogens by equipping them with a proteolytic platform that enables bacterial invasiveness and tissue destruction [1]. Sequestration of PLG with further activation into plasmin (PLA) is crucial for bacterial survival in the host environment, since surface-bound PLA degrades fibrin clots, ECM molecules, and host’s innate immune proteins facilitating dissemination and escape from immune responses [2,3]. The pathogenic spirochete Leptospira, the causal agent of the life-threatening infectious disease leptospirosis, is known to interact with host´s fibrinolytic system to ensure dissemination during the infection process [4].
Leptospirosis is a zoonotic disease of worldwide occurrence, which has a significant public health impact especially in low-income tropical and sub-tropical countries [5]. Globally, more than one million cases and approximately 60,000 deaths from leptospirosis are estimated each year [6]. The severe form of leptospirosis, accounting for 10% of all cases, may be fatal due to bleeding manifestations and acute kidney injury. Mortality rates of up to 74% have been reported in patients who developed leptospirosis-associated pulmonary hemorrhage-syndrome [7–12]. The disease also affects the agricultural industry, causing abortions, infertility, and death in livestock [5,13]. Since there are no preventive measures to control the infection in humans, leptospirosis remains a threat in developing countries lacking proper sanitation systems [6,13,14].
Currently classified into 69 species, the genus Leptospira was recently grouped in two major clades, namely the “Saprophytes” composed of free-living, nonpathogenic species, and the “Pathogens” which comprise species known to cause disease in humans and animals (P1) or species whose virulence status awaits confirmation, formerly called “Intermediates” (P2) [15,16]. Pathogenic Leptospira enter the host through injured skin or mucous membranes, and rapidly reach the bloodstream [17,18], due to their efficient swimming and crawling motilities through viscous environments [19,20]. The first step in the process of leptospiral infection is cellular adhesion, mediated by surface proteins interacting with various components of the extracellular matrix (ECM) [21]. Several putative adhesins that bind host ECM proteins have been identified in pathogenic Leptospira [22], but consistent evidence regarding cell/ECM-binding activity was only demonstrated for a few of them, such as the Leptospiral immunoglobulin-like proteins A (LigA) and B (LigB) [23] and the outer membrane protein L1 (OmpL1) [24]. These spirochetes are also equipped with additional mechanisms for host colonization, including the secretion of proteases that display proteolytic activity against ECM and plasma proteins [25], and the subversion of host proteases such as PLG through surface receptors [26,27]. Conversion of bound PLG into PLA by specific activators generates a proteolytic platform on the leptospiral surface supposedly increasing its invasiveness potential.
Several leptospiral proteins were previously described to act as PLG receptors. Some of them are well studied outer membrane proteins (OMPs) such as endostatin-like protein A (LenA), Leptospiral immunoglobulin-like proteins A (LigA) and B (LigB), and LipL32 [26,28,29]. Others are moonlighting proteins among which the elongation factor-thermal unstable (Ef-Tu) [30] and the metabolic enzyme enolase [31], also known to act as PLG receptors in other bacteria. The interaction of other less studied leptospiral surface proteins with PLG was also reported [28,32]. Of special interest within this group is the Membrane Protein L36 (MPL36) encoded in Leptospira interrogans strain Fiocruz L1-130 by the gene lic10054. MPL36 is a lipoprotein (321aa) with a Rare lipoprotein A (RlpA) domain (aa 22–257), initially described in Escherichia coli [33,34], a double-psi beta-barrel (DPBB) domain (aa 104–196), and a C-terminal Sporulation related (SPOR) domain (aa 248–318) [35] (Fig 1A). RlpA is localized at the septal ring in E. coli, but a precise role for this protein has not yet been defined in this organism, since no obvious phenotype associated with cell division was observed in rlpA mutants [33]. In Pseudomonas aeruginosa, RlpA was characterized as a peptidoglycan hydrolase digesting "naked" glycans, and the protein was shown to be crucial for proper separation of daughter cells and maintenance of rod morphology [36,37]. In pathogenic Leptospira, MPL36 was shown to bind human PLG with high affinity, presenting the lowest dissociation constant (KD) value among all proteins tested [32]. In the current study, using a random mutant [38] that lacked expression of MPL36, we performed genomic manipulation, in vivo studies, and in vitro assays to demonstrate that the PLG-binding MPL36 protein is necessary for pathogenic Leptospira to disseminate within the host and successfully establish infection.
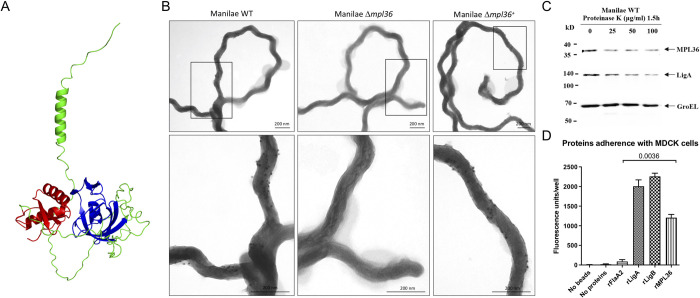
Fig 1. Structure and surface localization of MPL36 in L. interrogans serovar Manilae L495 and rMPL36 interaction with host epithelial cells.
(A) Predicted model of L. interrogans MPL36 with the double-psi beta-barrel domain (DPBB) (blue), a conserved region of RlpA proteins (green), and the SPOR domain (red) in the C-terminal. (B) Immunogold labeling of WT, Δmpl36, and Δmpl36+ Leptospira strains were performed using polyclonal rabbit antiserum against MPL36 and goat anti-rabbit IgG labelled with 10 nm colloidal gold particles. Cells were visualized using 2% UA negative staining. (C) Whole intact spirochetes were incubated with different concentrations of Proteinase K (25–100 μg/mL), and western-blot analysis was conducted using polyclonal rabbit antisera against MPL36, LigA (positive control), and GroEL (negative control). (D) Recombinant proteins coated with fluorescent latex beads were incubated with immobilized MDCK cells and this interaction was assessed by fluorescent emission. LigA and LigB were used as positive control, while FlaA2 was used as negative control. The results are represented as mean ± standard deviation of two independent experiments.
Results
Complementation restores expression of the MPL36 protein and disruption of mpl36 does not affect cell motility and growth rate
L. interrogans serovar Manilae Δmpl36 mutant strain was generated by Himar1 transposon mutagenesis, with the transposon insertion on position 921,626 of the Manilae genome (558 bp from the start codon of the gene) (S1A Fig). The complemented strain was generated by the insertion of the transposon carrying the gene mpl36 and a spectinomycin resistance cassette. After semi-PCR and sequencing screening, we identified four complemented strains, all of which exhibited the transposon in an intergenic region. The complemented strain Manilae Δmpl36+, with the complementing construct inserted at chromosome position 292,919, was chosen for this study (S1A Fig). PCR and Sanger sequencing confirmed the presence of the mpl36 gene in the WT and complemented strains.
Immunoblotting of bacterial whole-cell lysates with a rabbit polyclonal antibody raised against rMPL36 allowed detection of the native protein in both the WT and complemented (Δmpl36+) strains. A specific protein band with the apparent molecular mass of ~40 kDa was not visible in the mutant (Δmpl36) strain (S1B Fig). This result confirmed the disruption of mpl36 gene, and consequently, lack of expression of MPL36 in the mutant, as well as restoration of protein production by the complemented strain. It is important to note that a faint band is still visible on our mutant (S1B Fig) potentially as a result of a non-functional portion of the protein still being expressed (lic10054 gene was disrupted and not completely removed) or unspecific binding to another protein of similar molecular mass. Furthermore, the phenotypes described below show evidence of complete disruption of the functional MPL36 protein in our mutant strain.
No differences in cell morphology were observed among the different strains. Based on these facts, we assessed cell motility and growth ability of our Manilae strains. Using motility plate assays, no differences in motility (S1C Fig) were observed while comparing the wild-type (32 ± 1 mm), with Δmpl36 mutant (31 ± 1 mm, p = 0.2254), and complemented (30.7 ± 0.7 mm, p = 0.6667) strains. Similarly, comparable growth rates in EMJH medium at 30°C were exhibited by all three strains (S1D Fig), indicating that the disruption of the mpl36 gene does not affect motility and the ability of the strain to multiply and grow in vitro.
MPL36 is a surfaced exposed Leptospira protein that binds to host cells and PLG
MPL36 was predicted to be an outer membrane lipoprotein according to in silico analysis using lipoP and TMHMM software, and by immunofluorescence assay in a previous study [28]. Immunogold labeling using the WT, Δmpl36, and Δmpl36+ strains demonstrated that anti-MPL36 antibodies specifically labeled the surface of the WT and Δmpl36+ strains and did not bind to the surface of the Δmpl36 strain (Fig 1B). Surface exposure was further assessed by proteinase K treatment of intact leptospires (L. interrogans serovar Manilae L495). Both MPL36 and the well-characterized surface protein LigA [5,23] were sensitive to proteinase K-mediated degradation while the cytoplasmic control protein GroEL was not, providing additional evidence for MPL36 cell surface localization (Fig 1C). Immunoblot assay on the phase-partitioned fractions of Leptospira detected the MPL36 and surface LigA protein in the hydrophobic detergent phase, while the cytoplasmic protein GroEL [39] was portioned into the aqueous phase, and the periplasmic protein FlaB [26] was detected in the protoplasmic cylinder fraction (S2A Fig). Using multiple methods, we confirmed here the subcellular localization of MPL36 in Leptospira as an outer membrane protein.
The role of rMPL36 in adhesion to mammalian cells and ECM components was further investigated. Fluorescent latex beads coated with rMPL36 bound to MDCK cells whereas uncoated beads or those coated with rFlaA2 (negative control) did not display cell-binding activity (Fig 1D). As expected, rLigA and rLigB (positive controls) exhibited significant binding to MDCK cells (Fig 1D).
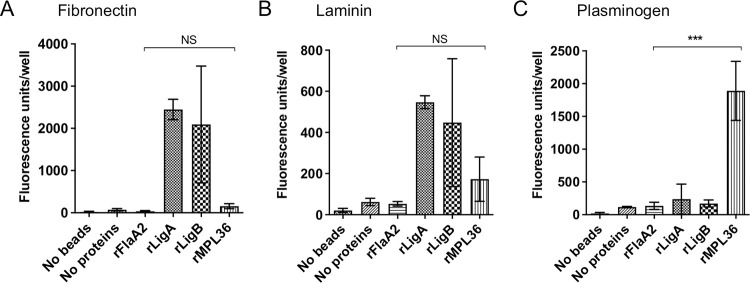
The interaction of rMPL36 with ECM proteins and PLG was also evaluated. No significant binding to fibronectin (p > 0.9, Fig 2A) or laminin (p = 0.9, Fig 2B) was detected with rMPL36, unlike what was observed with rLigA and rLigB proteins (positive controls). However, as previously described [28], rMPL36 displayed a significant binding capacity to human PLG compared to all other recombinant proteins used either as positive or negative controls (p < 0.0001, Fig 2C).
Fig 2. Binding of rMPL36 to ECM components and plasminogen (PLG).
96-well plates were coated with 1 μg of fibronectin (A), laminin (B), and PLG (C). 0.2 nmol of the recombinant proteins MPL36, LigA, LigB or FlaA2 coated with fluorescent latex beads were added per well, and the binding was assessed by fluorescent emission. A control using uncoated fluorescent latex beads was used to measure background signal. Data represent the mean ± standard deviation of results from three independent experiments (NS = non significant; ***p < 0.0001).
Furthermore, rMPL36 is recognized by sera from individuals with laboratory confirmed severe leptospirosis from Salvador, Brazil. Convalescent sera from those individuals have a high level of antibodies against MPL36 in both IgM (S2B Fig) and IgG (S2C Fig) when compared to sera from healthy individuals (p = 0.0023 and p < 0.001). No statically significant difference was observed in the acute sera (S2B and S2C Fig), although 48% of these sera had IgM antibodies levels higher than the identified threshold (S2B Fig, p = 0.08), confirming its expression during host infection, as previously observed [28], and further suggesting a potential role on the initial phases of the disease.
Taken together, those results suggest that rMPL36 can directly associate with MDCK cells, which is consistent with its surfaced-exposed localization and expression in the host during leptospirosis, in addition to its ability to bind to PLG, as previously described [28,40].
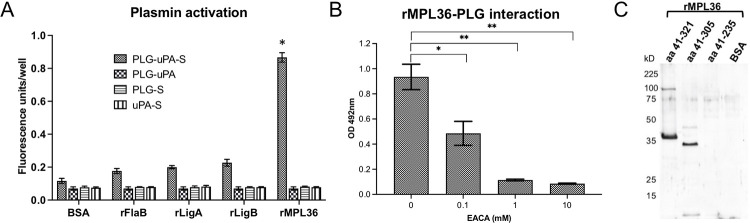
MPL36 binds PLG by its C-terminal lysine residues and MPL36-bound PLG is converted to PLA
To be proteolytically active, PLG needs to be converted to its active form, PLA, by urokinase or tissue PLG activators (uPA or tPA, respectively). Previous analysis of rMPL36-bound PLG have demonstrated the role of lysine residues on this interaction and the ability of PLG to be converted to PLA [28]. By exogenously supplying uPA to rMPL36-bound PLG, we confirmed that the newly generated PLA was able to significantly cleave the chromogenic substrate D-valyl-leucyl-lysine-ρ-nitroanilide dihydrochloride compared to BSA control (p < 0.001) (Fig 3A). Significant PLA activity was not detected with rLigA, rLigB, or rFlaA2 (Fig 3A). rMPL36-PLG interaction was dose-dependently inhibited by EACA, a lysine analog that binds to the PLG Kringle domains, confirming the involvement of lysine residues in the binding of rMPL36 to PLG (Fig 3B). Moreover, by ligand affinity blotting, we showed evidence suggesting that the last 70 amino acids of the protein, related to the conserved SPOR domain [35], is the region of rMPL36 required to bind PLG. The aa41-305 construct bound PLG as did the intact rMPL36 (aa41-321), while the aa41-235 construct lacked binding activity (Fig 3C).
Fig 3. Characterization of plasminogen (PLG) binding to rMPL36.
(A) MPL36-bound PLG activation to plasmin (PLA) by urokinase-type PLG activator (uPA). 96-well plates were coated with 1 μg of rMPL36, rLigA, rLigB, rFlaA2 or BSA, and incubated with PLG (1 μg). After activation with uPA (4 ng) and the chromogenic substrate (S) (0.4 mM), the reaction was measured using a fluorometer. Data represent the mean absorbance value at 405 nm ± the standard deviation of three independent experiments (*p < 0.001). (B) Assessment of lysine residues involvement in MPL36/PLG interactions. PLG (10 μg/mL) was added to MPL36-coated wells (1 μg) in the presence of epsilon-aminocaproic acid (0.1–10 mM). Bound-PLG was detected with a polyclonal anti-PLG (1:2,000), followed by peroxidase-conjugated secondary antibodies (1:10,000). Data show the mean absorbance value at 492 nm ± the standard deviation of three independent experiments (*p < 0.05; **p < 0.01). (C) Mapping of MPL36 region interacting with PLG by ligand affinity blot. Purified full-length (aa41-321) and truncated (aa41-305 and aa41-235) MPL36 recombinant proteins were subjected to SDS-12% PAGE under reducing conditions, transferred to a nitrocellulose membrane, and incubated with 50 μg of purified human PLG. Bound PLG was detected with anti-human PLG (1:500) followed by peroxidase-conjugated anti-rabbit IgG (1:10,000). BSA was included as a negative control.
The SPOR domain of MPL36 has seven lysine residues (S3A Fig). Despite differences in amino acid composition, tertiary structures of the SPOR domain from L. interrogans (P1), L. fainei (P2), and L. biflexa (S1) were similar (S3B Fig) and aligned with a root mean square deviation (RMSD) of 0.497. The major differences are more evident on the localization of lysine residues among different species (S3B Fig). Phylogenetic analysis revealed that the amino acid identity of MPL36 varied between 100% and 86% within pathogenic species (P1) of Leptospira, indicating a high degree of conservation. In contrast, the aa similarity dropped to 64% and 50% identity for pathogenic species of the P2 group and saprophyte species (S1 and S2), respectively, with MPL36 clearly being able to separate all species in different branches (S3C Fig). When we compared the amino acid composition, there were major differences between aa 248 and aa 321 among pathogenic and saprophytic species (S3D Fig), which corresponds to the region identified as to be potentially essential for PLG binding (Fig 3C). Given the limitations of those findings, performed using recombinant proteins and without being able to directly identify the specific site domain related to PLG binding, experiments using site-directed mutagenesis would be necessary to further confirm the role of the SPOR domain as the MPL36 PLG-binding site in pathogenic leptospires.
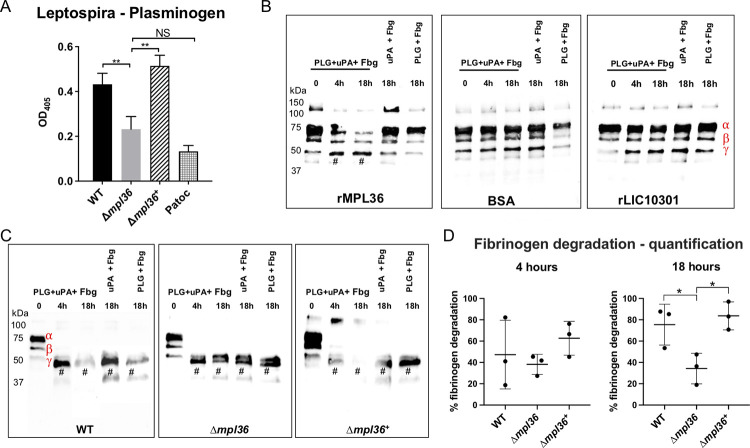
MPL36-bound PLG mediates fibrinogen degradation
Given the results with the rMPL36, we assessed the acquisition of human PLG in pathogenic Leptospira strains. The importance of MPL36 in PLG recruitment to the bacterial surface was endorsed by the reduced ability of the mutant strain to bind PLG (p = 0.0097), and by full restoration of PLG acquisition capacity by the complemented strain (p = 0.0027) (Fig 4A). Of note, although not statistically different from that displayed by the negative control strain Patoc (Fig 4A), the reduced but not completely abolished binding ability of the Δmpl36 knockout strain to PLG indicates the existence of other proteins with similar function, as previously described [28,32].
Fig 4. MPL36 role on the ability of Leptospira cells to bind to PLG and to degrade fibrinogen (Fbg).
(A) PLG binding to Patoc, Manilae WT, mutant Δmpl36, and Δmpl36+ strains was assayed using a whole-cell enzyme-linked immunosorbent assay. A total of 1μg PLG was immobilized and incubated with 108 bacterial cells. Bound leptospires were detected using serum from a hamster infected with an attenuated Manilae strain, and pre-immune serum was used as a control. Data represent the mean ± standard deviation of results of three independent experiments after subtracting the pre-immune serum data. (B) Fibrinogen degradation by immobilized rMPL36-PLA. Microtiter plate wells coated with rMPL36, rLIC10301, or BSA (10 μg/mL), were incubated with purified human PLG (20 μg/mL). After washes, fibrinogen (500 ng) and uPA (1 U) were added and incubated for up to 18 h. A western blot using anti-human fibrinogen (1:5,000) was performed. (C) Fibrinogen degradation by PLA bound to Leptospira strains (Manilae WT, Δmpl36, Δmpl36+). Leptospires (108 cells) were incubated with purified human PLG (10 μg), and after washes uPA (3 U) and fibrinogen (10 μg) were added and incubated for up to 18 h. Leptospiral supernatants were collected and analyzed by western blot using anti-human fibrinogen (1:5,000). Controls excluding uPA or PLG were included. One experiment representative of three is shown. (D) Densitometric quantification of fibrinogen cleavage by Leptospira strains. Band intensities corresponding to α-, β-, and γ- fibrinogen chains in T0h were arbitrarily set as 100%. Quantification of fibrinogen cleavage products at T4h and T18h (relative to T0h) are shown. Data were analyzed with one-way ANOVA and Student t test (*p < 0.05; **p < 0.001). # = proteolytic products. Fibrinogen chains’ position is represented in red (B and C) - α (73kDa), β (60 kDa), and γ (53 kDa).
We then assessed if MPL36-bound PLG, once converted to its active form PLA, could cleave ECM substrates and immune mediators of physiological importance. Recombinant protein, as well as Leptospira strains, were first incubated with PLG. After successive washes, preparations were incubated with fibrinogen, vitronectin, laminin, fibronectin, and C3b in the presence of the PLG activator uPA for 4 h or 18 h. rMPL36-bound PLA cleaved fibrinogen α-chain in a time-dependently manner, producing a degradation fragment of ~50 kDa that co-migrates with fibrinogen γ-chain (Fig 4B). No degradation products were detected when the plates were immobilized with the negative control proteins BSA or rLIC10301, a lipoprotein of unknown function that is unable to bind PLG [30] (Fig 4B). As expected, fibrinogen degradation was much more pronounced when we used intact bacteria, with all three strains degrading both α and β chains of fibrinogen (Fig 4C). However, a more pronounced degradation was only achieved in the presence of the WT and the complemented strains after 18 h incubation period, thus indicating that MPL36, by acquiring PLG, effectively contributes to fibrinogen degradation (Fig 4C). Furthermore, in the presence of the Δmpl36 strain the degradation products detected in the absence of active PLA (uPA + Fbg and PLG + Fbg) were similar to those observed in the presence of PLG (PLG + uPA + Fbg), thus indicating that this degradation results from non-PLA action, most likely leptospiral proteases.
Fibrinogen degradation in the presence of both the WT and complemented strains at 18 h was significantly more efficient (p = 0.0447 and p = 0.0119, respectively) compared to the one observed in the presence of the mutant strain (Fig 4D). As ECM and complement proteins are among PLA targets, we also assessed the ability of MPL36-bound PLA to degrade vitronectin (S4A Fig), laminin (S4B Fig), and complement C3b (S4C Fig). No differences regarding the degradation patterns were observed for the WT, Δmpl36 and Δmpl36+ strains (S4A–S4C Fig), thus indicating that MPL36-bound PLA specifically targets fibrinogen. Complete degradation of vitronectin probably results from the action of bacterial secreted proteases since the cleavage profiles are quite similar for all three strains (S4A Fig). Taken together, those results indicate that MPL36 is a major PLG binding protein with a potential contribution to the proteolytic ability of pathogenic leptospires, which could increase the invasiveness capacity of this bacterium.
Native MPL36 promotes Leptospira adhesion to epithelial host cells and translocation
To further confirm the adhesive and invasiveness properties of MPL36 on epithelial cells, the interaction of Manilae WT, Δmpl36, and Δmpl36+ strains with cultured MDCK cells was investigated. The saprophyte Patoc strain was included as a negative control. An average of 6 WT leptospires adhered to each MDCK cell while approximately 0.2 and 0.5 of mutant and saprophytic leptospires, respectively, were found associated with each MDCK cell (Fig 5A). The binding capacity of the mutant strain was significantly reduced compared to the ones displayed by the WT (p = 0.001) and the complemented strain (p = 0.0107), but the phenotype of adherence was not completely restored on the complemented strain (average of 4 leptospires/MDCK cell) when compared to the WT (p = 0.0452, Fig 5A).
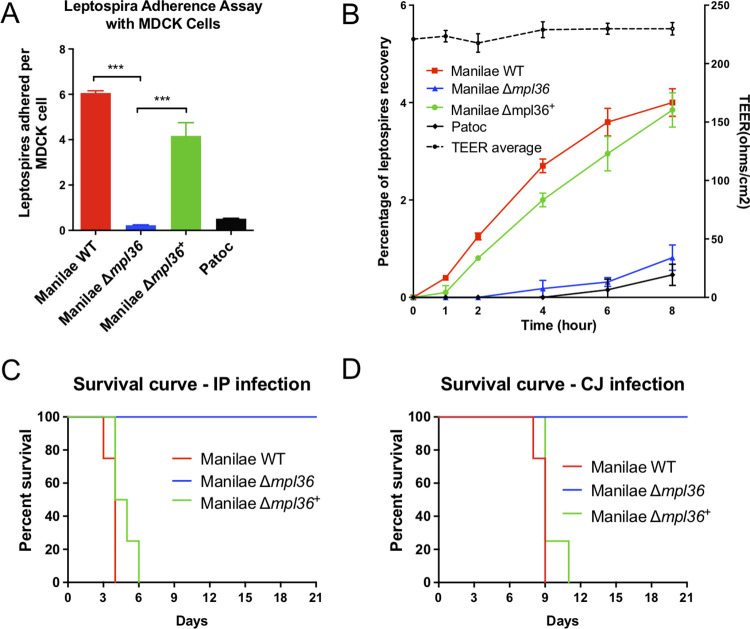
Fig 5. Role of MPL36 on the pathogenesis of Leptospira interrogans.
(A) Ability of leptospires strains to adhere to MDCK epithelial cells. Manilae WT, Δmpl36, and Δmpl36+ strains were incubated with immobilized MDCK cells for one hour at 37°C and adhesion assessed by immunofluorescence. Data represent the mean ± standard deviation of results from three independent experiments. (B) Ability of Leptospira strains to translocate through polarized monolayers of MDCK cells. The Patoc strain was used as negative control. Strains were inoculated (100 MOI) in the upper chamber of a Millicell culture plate containing MDCK cell monolayer. Percent recovery of leptospires was determined by counting bacteria in the lower chamber between 0 and 8 hours after inoculation. Right Y axis shows TEER measurements. Data represents the mean ± standard deviation of results from three independent experiments. (C, D) Survival curve of hamsters infected with Leptospira strains. Animals were infected either by intraperitoneal (IP) or conjunctival (CJ) route with 108 leptopires. Data represent results of one of two independent experiments.
We also investigated the ability of these Leptospira strains to translocate through monolayers of MDCK cells. Within the first two hours after infection, only the WT and complemented strains were recovered from the lower chamber of the Millicell culture plates, indicating their ability to successfully cross the MDCK cell monolayers (Fig 5B). The mutant strain (Δmpl36) was recovered starting at 4 h post-infection. However, over the 8-hour course of the experiment, there is a statistical difference in the number of mutant cells that were recovered compared to the WT (p = 0.0284) and complemented strains (p = 0.0456). There were no statistical differences between the numbers of WT and complemented strains recovered (p = 0.0625), indicating that the complementation restored the ability of the mutant to translocate. As expected, the Patoc strain was unable to successfully translocate, as previously observed [41] (Fig 5B). Consistent TEER measurements indicated that disruption of cell monolayers’ TJ did not occur during the translocation process (Fig 5B). Taken together, those experiments indicate that MPL36 abrogation partially impairs the ability of leptospires to adhere to and translocate through polarized monolayers of MDCK cells, which in turn would affect the ability of the pathogen to efficiently disseminate and cause disease.
MPL36 is essential for virulence of pathogenic Leptospira during acute infection
To determine the role of MPL36 during the infection process, the WT, Δmpl36 and Δmpl36+ strains were tested for virulence in the hamster model of leptospirosis infection. Hamsters challenged by IP route with 108 leptospires of the Δmpl36 strain survived up to 21 days without any symptoms of infection, whereas hamsters challenged with the same number of bacteria of the WT strain died between 3–5 days post-infection (Fig 5C and S2 Table). The mutant phenotype complemented by reintroduction of mpl36 yielded 100% lethality at dose 108 in 4–6 days after IP challenge (Fig 5C and S2 Table).
When using the CJ route of infection, hamsters challenged with 108 leptospires with the Δmpl36 mutant survived without disease manifestation, whereas all animals challenged with the WT strain died between days 8–9 post-infection (Fig 5D and S2 Table). Animals infected with the complemented strain all died between 9- and 11-days post-infection (Fig 5D and S2 Table). Leptospires were not detected in the kidney of animals infected with Δmpl36 by both routes of infection at day 21 post-infection, when animals were euthanized (S2 Table). Those results indicate that MPL36 is an essential protein for the pathogenesis of Leptospira (Fig 6).
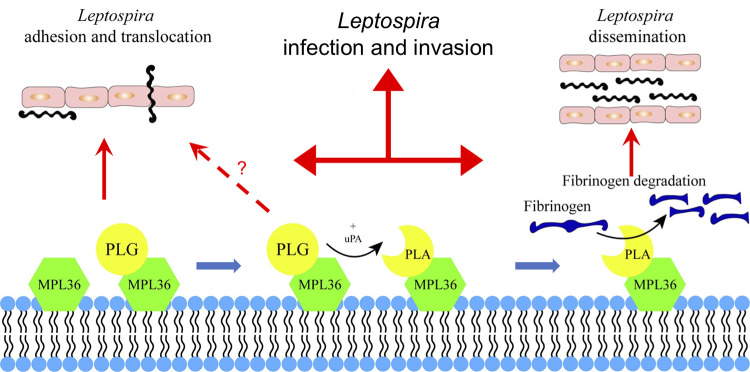
Fig 6. Schematic summary view of MPL36 role on leptospiral pathogenesis.
Hypothetical model showing how acquisition of PLG by MPL36 contributes to Leptospira adhesion and translocation through cell monolayers, and to the proteolytic potential of this spirochete.
Discussion
Our results showed that MPL36 is an outer membrane protein acting as a major PLG binding in pathogenic Leptospira, with the ability to degrade fibrinogen, being essential for leptospiral virulence. The mechanisms behind the pathogenesis of leptospiral infection continues to be a major knowledge gap preventing the advance on diagnostic and prevention. Despite the recent major breakthroughs on the research of this important neglected zoonotic disease [21], more work is needed to better understand how leptospires can rapidly disseminate, evade host-immune responses, and cause life-threatening disease worldwide. A previous study has shown that only virulent strains of Leptospira spp. were capable of acquiring PLG from human plasma, strongly suggesting the involvement of this process in leptospiral virulence [27]. Through capturing PLG on their surface, followed by activation to PLA, these spirochetes augment their proteolytic capacity, and consequently, potentiate dissemination through tissue barriers. It has also been suggested that direct binding of fibrinogen to the leptospiral surface could lead to an increased consumption of those molecules, causing a reduction in fibrin clot formation [42]. Leptospira proteome contains multiple proteins with the ability to bind different ECM and PLG [4,32]. However, those studies were conducted using recombinant proteins and none of those targets have been confirmed to have a direct role in virulence.
The leptospiral MPL36 belongs to a family of proteins containing a Rare lipoprotein A (RlpA) domain [43] and a C-terminal SPOR (sporulation related repeat) domain [35]. Similar to its homologous in E. coli and P. aeruginosa [37,44], MPL36 has been characterized as a putative surface exposed protein in Leptospira [28,40]. The gene mpl36 has been shown to be upregulated in a dialysis membrane chamber (DMC) system implanted in the peritoneal cavities of rats [45], representing a mammalian host-adapted state, and it has been identified as one of the genes regulated by Leptospira virulence regulator (lvrAB) [46], a signaling system that controls virulence in Leptospira. More recently, MPL36 has been identified as one of the targets associated as correlates of cross-protection on an attenuated-vaccine model for leptospirosis [47]. Furthermore, we demonstrated that human patients with leptospirosis produced antibodies that recognize MPL36 [40], and that IgM antibodies against MPL36 are detected during the early stages of the disease, thus indicating that MPL36 is expressed during host infection, has an important role on pathogenesis, and might serve as a target for serodiagnosis and vaccine development.
MPL36 was first characterized as a PLG-binding molecule in a study aiming to identify Leptospira PLG receptors [28]. In this study, we explored further the interaction of MPL36 with PLG by evaluating the functional consequences of PLG acquisition by leptospires through this surface receptor as well as leptospiral virulence in the absence of mpl36. Our results with both recombinant protein and mutant Leptospira strains not only confirmed the ability of MPL36 to bind to host epithelial cells, but also demonstrated that a mutant unable to express MPL36 (Δmpl36) had an impaired binding capacity to PLG, similar to the phenotype observed for the saprophyte L. biflexa. The process of PLG binding to bacterial receptors on the cell surface has been shown for several pathogens to be mediated by the PLG Kringle domains containing lysine-binding sites [1]. Our results based on ligand affinity blotting and in silico analysis suggested that the PLG-interacting region of MPL36 is located at the SPOR domain on the protein C-terminus, with binding potentially occurring through lysine residues within this domain, respectively. However, further in depth experiments are needed to confirm those findings and potentially identify the particular site domain for this interaction.
SPOR domains are about 70 amino acids long consisting of four antiparallel β-sheet flanked on one side by two α-helices. The domain primary structure is not highly conserved, but it is present in several bacteria as a peptidoglycan (PG) binding domain and its function is mainly related to remodeling the PG sacculus during cell division [35,36]. Most bacterial SPOR domain proteins are present in the periplasm, although both P. aeruginosa and E. coli RlpA are outer membrane proteins [34,37]. P. aeruginosa outer membrane RlpA was described as a lytic transglycosylase [37], with mutants having striking morphological defects. However, none of the E. coli SPOR proteins have been reported to have an enzymatic activity [48] or being related to growth or cell viability [34]. MPL36 binding to PG and participation in cell division were not directly assessed in this study. However, the Δmpl36 strain had no morphological or growth defects, strongly suggesting that MPL36 is not involved in these processes in Leptospira. Although found in all Leptospira species, with 50% amino acid identity in the saprophyte L. biflexa, our in-silico analysis disclosed differences in primary structure composition, mainly clustered on the SPOR domain of the protein, suggesting a potential different function of this protein in non-pathogenic species.
MPL36-mediated PLA formation has a role on fibrinogen degradation in pathogenic leptospires. When incubated with rMPL36, we observed only a partial yet significant degradation of fibrinogen α-chain. This result suggests the existence of additional PLG-interacting proteins on the leptospiral surface able to degrade fibrinogen, as previously reported [4,26,32,49]. This assumption is further supported by the fact that Leptospira binding to PLG, although significantly reduced, was not completely abolished when we used the Δmpl36 mutant strain. It is also important to highlight that fibrinogen degradation by Leptospira results from two distinct mechanisms: PLA-binding activity and proteolytic action of extracellular metalloproteases secreted by virulent strains, which target ECM and plasma proteins from the host [25]. The combined strategies ensure an efficient degradation of host fibrinogen by Leptospira as demonstrated here. However, after 18 h of incubation almost complete hydrolysis of this coagulation cascade molecule was observed only when WT or Δmpl36+ strains were incubated with PLG, uPA and fibrinogen. Curiously, our experiments showed that MPL36-bound PLA had no apparent effect on vitronectin, laminin or complement C3b. Taken together, our results indicate that the MPL36-bound PLA seems to have an essential and targeted role on fibrinogen degradation, and more studies are needed to confirm and better understand this peculiar activity.
MPL36 mediates binding of leptospires to MDCK cells, a crucial step for subsequent translocation through cell monolayers. Studies have shown that in Streptococcus sp. the adherence process for colonization and translocation were dependent of PLG recruitment in the surface, with PLG acting as a linker molecule independently of the plasmin activity [50,51]. rMPL36 did not bind purified fibronectin or laminin, indicating the possibility that MPL36-bound PLG could anchor leptospires to the cell surface, serving as a bridging molecule. There is no evidence of ECM degradation related to MPL36, thus the inability of Δmpl36 strain to translocate could be strongly related to the low capability to adhere to host cells. Nevertheless, lack of expression of MPL36 in pathogenic Leptospira lead to a complete attenuation phenotype in hamsters, challenged by both IP and CJ routes, with the latter mimicking a more natural route of infection that involves adhesion and translocation of host cells. Bacterial PLG receptors are described as multifunctional surface proteins during infection process [1], and it has been shown that lysine residues must be precisely positioned during presentation to substrates and catalysts in order to activate the plasminogen system [52], thus influencing the pathogenic process. For that reason, further experiments are needed to understand the mechanism of action for MPL36 during the infectious process and other potential roles that MPL36 might have on the leptospiral pathogenesis process, leading to the observed attenuated phenotype.
In this study, we characterized the MPL36 protein as a surface exposed virulence factor, with the ability to bind to PLG and degrade fibrinogen, playing a role on adhesion and subsequent translocation of the leptospiral spirochete on host cells (Fig 6). Genetic manipulation tools for targeted mutagenesis in Leptospira are still limited and restricted to a few research laboratories, and the identification and characterization of leptospiral proteins’ interaction with host components have been mostly based on recombinant proteins. Our results are based on in vitro and in vivo analysis using knockout and complemented mutants, fulfilling molecular Koch’s postulates, providing new insights regarding bacterial proteins that explore PLG for their pathogenesis. There is a major interest in the identification of antigenically conserved surface-exposed proteins with the capacity to serve as broader vaccine candidate targets. In addition, the characterization of leptospiral components contributing to pathogenesis would aid in the development of improved diagnostic strategies. Our results demonstrate that MPL36 is a highly conserved protein among pathogenic species, expressed and able to elicit immune response during the infection process, satisfying all the requirements to be further explored on research designed to better understand leptospiral pathogenesis and advance diagnostic and prevention of this important zoonotic disease.
Material and methods
Ethics statement
The protocol of animal experimentation was prepared and approved according to the guidelines of the Institutional Committee for the Use of Experimental Animals, Yale University (protocol # 2023–11424).
Bacterial strains, cells, and culture conditions
The pathogen Leptospira interrogans serovar Manilae strain L495 (Manilae WT), the Manilae mpl36 mutant (Δmpl36), the Manilae mpl36 mutant complemented strain (Δmpl36+) and the saprophyte L. biflexa serovar Patoc strain Patoc 1 (Patoc) were grown in Ellinghausen-McCullough-Johnson-Harris (EMJH) liquid medium [53] with agitation or on 1% agar plates at 30°C. E. coli cells were grown in Luria-Bertani (LB) medium at 37°C with agitation. When appropriate, spectinomycin and/or kanamycin were added to the culture medium at a final concentration of 50 μg/mL. Madin–Darby canine kidney (MDCK) cells were cultured in minimum essential medium (MEM) containing 10% fetal bovine serum (GIBCO Laboratories). Cells were grown at 37°C in a humidified atmosphere with 5% CO2.
For growth curves of WT, mutant and complemented strains, bacteria were initially enumerated under dark-field microscopy by using Petroff-Hausser counting chambers (Fisher Scientific) and diluted to a starting bacterial concentration of 104 mL at 30°C. Growth was monitored daily by counting. Three independent experiments were performed. For the motility assay, 5 μL of 105 leptospires were inoculated on 0.5% agarose EMJH plates and incubated for 10 days at 30°C, as previously described [41]
Proteinase K treatment of intact bacteria
MPL36 cell surface localization was first assessed by proteinase K treatment as previously described [39]. Briefly, Manilae WT cells were grown to a density of 5×108 cells/mL and harvested by low-speed centrifugation at 2,000 × g for 10 min at room temperature. The pellet was gently washed with phosphate buffered saline (PBS) containing 5 mM MgCl2, and collected by centrifugation at 2,000 × g for 10 min. After resuspension in PBS-5 mM MgCl2, proteinase K (Sigma-Aldrich) diluted in proteolysis buffer (10 mM Tris-HCl pH8.0, 5 mM CaCl2) was added to the washed leptospires in a final concentration of 25 to 100 μg/mL. Proteolysis buffer without proteinase K was added to the negative control. The reaction was quenched by the addition of phenylmethylsulfonyl fluoride (PMSF). Leptospires were subsequently collected by centrifugation and washed twice with PBS-5 mM MgCl2, and the cells were resuspended in sample buffer for SDS-PAGE. Immunoblot analysis was performed using rabbit antibodies against proteins MPL36, LigA and GroEL at a dilution of 1:1,000. Bound antibodies were detected using horseradish peroxidase (HRP)-conjugated anti-rabbit IgG (GE Lifesciences) at a dilution of 1:100,000. Positive signals were detected by SuperSignal West Pico Kit (Pierce), according to the manufacturer’s instructions, and blots were analyzed using ChemiDoc Imager (Bio-Rad).
Immunogold labeling
Bacterial cultures (1 x 108 cells/mL) were centrifuged (6,500 x g for 20 min), washed with PBS three times and fixed with 4% formaldehyde for 30 min. After fixation, preparations were washed three times with PBS and blocked with 0.2% bovine serum albumin (BSA) in PBS (PBS-BSA) for 30 min. Preparations were then incubated overnight with rabbit anti-MPL36 antiserum (1:10 dilution in PBS) at 4°C. Subsequently, preparations were washed with PBS-BSA, and incubated with goat anti-rabbit antibody labeled with 10 nm colloidal gold particles (Sigma-Aldrich) diluted 1:10 in PBS, for 4h at room temperature. After further washings, preparations were mixed (1:1) with 2% uranyl acetate (UA) in water and placed onto Formvar-coated nickel grids for 2 min. After completely dried with filter paper, preparations were then analyzed under TEM (LEO 906E –Zeiss, Germany) at 80 kV.
Phase partitioning of Leptospira membrane proteins using Triton X-114
Phase separation of the integral membrane proteins of Leptospira to localize the protein MPL36 was performed using Triton X-114 solution as described elsewhere [54]. Briefly, a 50 mL mid-log-phase culture of L. interrogans serovar Copenhageni Fiocruz L1-130 (5×109 cells) was washed in PBS containing 5 mM MgCl2. The membrane proteins were extracted at 4°C with 1% Triton X-114, 150 mM NaCl, 10 mM Tris (pH 8.0) and 1 mM EDTA. The insoluble debris was removed by centrifugation at 12,000 × g for 15 min and then 20 mM CaCl2 was added to the supernatant. Phase separation was performed by warming the supernatant at 37°C and subjecting it to centrifugation for 10 min at 1,000 × g. The detergent and aqueous phases were separated and precipitated with 10 volumes of chilled acetone. The aqueous and detergent phases were then resolved onto 12% SDS-polyacrylamide gel before transferring to nitrocellulose membrane for immunoblot analysis using polyclonal rabbit sera anti-MPL36, anti-LigA, and anti-GroEL (1:1,000).
Cloning, expression, and purification of MPL36 fragments
The full recombinant MPL36 protein (rMPL36/aa 41–321) was commercially produced by GenScript Biotech with His-tag in an E. coli expression system. Recombinant MPL36 protein devoid of the last 16 residues (rMPL36/aa 41–305) and devoid of the last 86 residues (MPL36/aa 41–235) were produced following protocol previously described [39]. DNA fragments were amplified by PCR from L. interrogans serovar Copenhageni genomic DNA (strain Fiocruz L1-130) with set of primers aa41-305 and aa41-235, using restrictions enzyme sites for BamHI and NcoI, respectively (S1 Table). The amplified products were cloned into the pGEM-T Easy vector (Promega) and subcloned into the pAE expression vector [55]. This vector allows the expression of recombinant proteins with a minimal His6 tag at the N-terminus. The constructs were transformed into E. coli BL21 DE3. Expression and purification of the recombinant proteins were performed essentially as previously described [39]. Control protein rLIC10301 used in our experiments was expressed following the same protocol. The full rMPL36 and rLIC10301 proteins were purified from the supernatant of E. coli lysates, while the rMPL36 aa41-305 and rMPL36 aa41-235 were purified from the insoluble pellet, by nickel affinity chromatography. Tertiary structure of rMPL36, rMPL36 aa41-305, rMPL36 aa41-235 was assessed by intrinsic tryptophan fluorescence spectroscopy [56]. Data were collected using 1 cm path length rectangular quartz cuvettes on a fluorescence spectrophotometer (Cary Eclipse, Varian). Recombinant proteins (4 μM) were incubated in the presence or absence guanidine hydrochloride (GndHCl, 6 M) for 30 min, and intrinsic fluorescence emission of folded and unfolded proteins was measured in 10 mM PBS, with excitation at 280 nm and emission recorded in the range of 300–400 nm. Full-length rMPL36 and the other 2 constructs display one aromatic and fluorescent tryptophan (Trp) residue. Intrinsic fluorescence spectrum of MPL36 showed a maxima emission wavelength (λmax) at 335 nm, indicating that Trp is located at an apolar environment. The addition of 6 M GdnHCl resulted in a shift to 356 nm, a result compatible with the exposure of the aromatic side chains to the solvent and the total unfolding of the protein (S5 Fig). The same behavior was observed for the 2 other constructs, indicating that the three proteins were structured, but lost tertiary structure upon addition of GdnHCl (S5 Fig).
Binding assay using fluorescent latex beads
To assess the binding ability of rMPL36 to ECM proteins and PLG, l μg of fibronectin (10 nM, Sigma-Aldrich), laminin (20 nM, Sigma-Aldrich), PLG (100 nM, Sigma-Aldrich) and BSA (negative control) was coated on 96-well plates overnight at 4°C. Plates were blocked for 1 h at 37°C with 5% non-fat dried milk in 2% BSA. Recombinant proteins MPL36, FlaA2 (negative control), non-identical regions of LigA (rLigA; amino acid positions 625 to 1225) and LigB (rLigB; amino acid positions 625 to 1257) (positive controls) were diluted in PBS to a final concentration of 0.2 nmol. A 4 μL sample of the stock suspension of latex beads (containing about 3×1010 mL-1 of 0.3 μm diameter beads, Sigma-Aldrich) was added to each protein and incubated for 2 h at 37°C. A sample of 100 μL of this suspension was then added in triplicate to the wells of the previously coated plates and incubated for 2 h at 37°C. Plates were washed four times with PBS-0.05% (vol/vol) Tween 20 (PBST) and the fluorescent emission (excitation at 486–580 nm and emission at 568–590 nm) was measured using Synergy HT (BioTek, Agilent). Uncoated beads and beads coated with BSA were used as controls. For statistical analyses, the experiment was repeated three times and the attachment of recombinant proteins to the host components was compared to its binding to BSA.
To assess the binding ability of rMPL36 to host epithelial cells, Madin-Darby Canine Kidney (MDCK) cells were seeded in a 24-well tissue culture plate at a density of 2 x 105 cells per well and incubated at 37°C with 5% CO2 for 48 h until the formation of a near-confluent MDCK cell monolayer. Samples of 100 μL of the latex bead suspension coated with rMPL36, rFlaA2, rLigA and rLigB, as described above, were added in triplicate to the pre-incubated MDCK cells. After 5 h incubation at 37°C, cells were washed three times with PBS. The fluorescence emission was measured directly in the 24-well plate using Synergy HT (BioTek, Agilent). The experiment was repeated twice.
Conversion of PLG into active PLA
To evaluate if PLG bound to rMPL36 is converted into active PLA 96-well plates were coated with 0.2 μM of recombinant proteins or BSA (negative control) at 4°C overnight. The plates were washed once with PBST and blocked 2 h at 37°C with 10% non-fat dried milk in PBS. The blocking solution was discarded, and the plate washed four times with PBST. Then, 1 μg (100 nM) of human PLG (Sigma-Aldrich) was added to each well and incubated for 2 h at 37°C. Wells were washed four times with PBST, and then 4 ng (0.7 nM) of human urokinase-type PLG activator (uPA, Sigma-Aldrich) was added per well. After that, 100 μl of the PLA specific substrate D-valyl-leucyl-lysine-p-nitroanilide dihydrochloride (Sigma-Aldrich) was added at a final concentration of 0.4 mM in PBS. Plates were incubated overnight, and substrate degradation was measured at 405 nm using Synergy HT (BioTek, Agilent). The experiment was repeated three times for reproducibility.
Role of lysins in rMPL36-PLG interaction
To assess the role of lysins in rMPL36-PLG interactions 96-well plates were coated with rMPL36 (10 μg/mL, 200 nM). After blocking with 3% BSA, PLG (10 μg/mL, 100 nM) and ε -aminocaproic acid (0–10 mM) were added to the coated wells. Bound PLG was detected with a rabbit polyclonal antibody (Sigma-Aldrich) at a 1:2,000 dilution followed by peroxidase-conjugated anti-rabbit IgG (Sigma-Aldrich) at a 1:10,000 dilution. Student´s two-tailed t test was used for statistical analyses.
Interaction of rMPL36 with PLG by ligand affinity blotting
Purified recombinant proteins were subjected to 12% SDS–PAGE and transferred to a nitrocellulose membrane. After blocking with 5% BSA the membrane was incubated for 1 h with 50 μg (200 nM) of purified PLG (Sigma-Aldrich) diluted in PBS. After five washes with PBST, the membrane was incubated with polyclonal rabbit antibodies recognizing human PLG (Sigma-Aldrich, 1:500), followed by peroxidase-conjugated secondary antibodies (1:10,000). Positive signals were detected by SuperSignal West Pico Kit (Pierce). BSA was used as a negative control.
Detection of antibodies to rMPL36 using human sera of individuals with laboratory-confirmed leptospirosis
We performed an ELISA assay using rMPL36 against acute and convalescent sera from 29 individuals with confirmed severe leptospirosis enrolled in our surveillance study in Salvador, Brazil [14]. Control human sera were obtained from healthy US human donors. Microtiter plates (Corning) were coated with 80 ng of rMPL36 and incubated overnight at 4°C. The plates were washed three times with PBST and incubated with 5% milk blocking solution for 2 h at 37°C. After four washes with PBST, wells were incubated in duplicate with human immune sera, diluted 100-fold in 2% BSA, for 1 h at 37°C. Secondary anti-IgM human HRP conjugated antibody (Sigma-Aldrich) or anti-IgG human HRP (Jackson ImmunoResearch) was used at a dilution of 25,000 (2% BSA) and incubated for 1 h at 37°C. Tetramethylbenzidine (TMB, SureBlue Reserve) was used for detection and the reaction was stopped by adding 100 μL of 2 N H2SO4. Absorbance (450 nm) was recorded using Synergy HT (BioTek, Agilent). A threshold was calculated based on 2.5 SD of the average OD from the healthy individuals for each isotype.
Insertion mutagenesis and complementation
Random mutagenesis in L. interrogans serovar Manilae strain L495 using mariner-based transposon Himar1 has been previously described [38]. The insertion site was identified by semi-random PCR followed by DNA sequencing. The insertion within mpl36 was confirmed by PCR using primers flanking the insertion site. For complementation, mpl36 and its native promoter were PCR amplified from Manilae WT using primers mpl36F and mpl36R, designed with KpnI restriction sites (S1 Table). The amplicon was then digested by KpnI and ligated into plasmid pAL614, which carries a modified Himar1 transposon for conjugation [57] containing a spectinomycin resistance cassette. The resulting plasmid (pAL614-mpl36) was used to chemically transform E. coli S17 cells, which were subsequently used to transform serovar Manilae Δmpl36 strain via conjugation. Transposon insertion occurred at nucleotide 292,919 in the gap of two open reading frames. MPL36 expression by the mutant (Manilae Δmpl36) and complemented (Manilae Δmpl36+) strains was verified by Western-blot analysis using anti-MPL36, as described above.
Binding of Leptospira strains to PLG
Adhesion of Leptospira strains (Manilae WT, Δmpl36, Δmpl36+, and Patoc) to human PLG (Sigma-Aldrich) was assessed by ELISA as previously described [23]. A 96-well plate was coated with PLG or BSA (negative control) (10 μg/mL) overnight at 4°C. Plates were washed four times and then blocked with 5% non-fat dried milk in 2% BSA for 1 h at 37°C. After washing with PBST, 1×108 leptospires were added to each well and incubated for 90 min at 37°C. After two washes with PBST to eliminate non-adherent cells, adherent leptospires were fixed with cold-methanol for 10 min at -20°C, and detected with a hamster polyclonal serum of animals infected with 107 L. interrogans serovar Manilae fcpA- [41] (1:1,000) followed by a peroxidase-conjugated anti-hamster IgG (1:50,000). Pre-immune serum was used as a negative control, and final values were calculated from three technical results after subtracting the pre-immune serum data. Absorbance was measured at 405 nm using Synergy HT (BioTek, Agilent).
ECM and plasma protein degradation by PLA bound to Leptospira strains
Mid-log phase leptospires (Manilae WT, Δmpl36, Δmpl36+) were harvested by centrifugation at 9,000 x g for 5 min and 1 x 108 bacteria were incubated with purified human PLG (10 μg, 1 μM) diluted in PBS for 1 h at 37°C. Leptospires were washed three times with PBS and then incubated with 3 U of uPA (Sigma-Aldrich) and 10 μg (300 nM) of human PLG-depleted fibrinogen (Calbiochem), or 2.5 μg (300 nM) of human vitronectin (Sigma-Aldrich), or 5 μg (50 nM) of laminin (derived from mouse Engelbreth-Holm-Swarm sarcoma, Sigma-Aldrich), or 2.5 μg (50 nM) of human plasma fibronectin (Sigma-Aldrich), or 1.5 μg (80 nM) of human complement C3b (Complement Technology) at 37°C for 0, 4 and 18 h. For the control reactions, either PLG or uPA was omitted. After incubation, leptospiral supernatants were collected by centrifugation and subjected to 12% SDS-PAGE. The cleavage fragments were analyzed by western blot with either mouse anti-human fibrinogen polyclonal antibody (Sigma-Aldrich) at a 1:5,000 dilution, rabbit anti-human vitronectin polyclonal antibodies (Complement Technology) at a 1:5,000 dilution, rabbit anti-human laminin polyclonal antibodies (Sigma-Aldrich) at a 1:5,000 dilution, rabbit anti-human fibronectin polyclonal antibodies (Sigma-Aldrich) at a 1:5,000 dilution, or goat anti-human C3 polyclonal antibodies (Complement Technology) at a 1:5,000 dilution, followed by peroxidase-conjugated anti-mouse (1:5,000), rabbit or goat (1:10,000) IgG (Sigma-Aldrich). Positive signals were detected by SuperSignal West Pico Kit (Pierce). Images of the three experiments performed were recorded and band intensities were quantified using the Alliance LD2 system (Uvitec, Cambridge, UK). Band intensities at 0 h, corresponding to α-, β-, and γ- fibrinogen chains, were arbitrarily set as 100%.
Degradation of fibrinogen by rMPL36 was also assessed. rMPL36, and negative controls rLIC10301 [30] and BSA (10 μg/mL, 200 nM) were immobilized on microtiter plate wells and blocked with 3% BSA diluted in PBS. PLG (20 μg/mL, 200 nM) was added, and plates were incubated for 1 h at 37° C. Wells were then washed six times with PBST and added with human fibrinogen (500 ng/well, 30 nM, PLG depleted; Calbiochem) and uPA (1 U/well). Reaction mixtures were incubated at 37° C for the indicated time points and were then separated by 12% SDS-PAGE. The degradation products of fibrinogen were detected by Western blot using rabbit anti-human fibrinogen polyclonal antibodies (Sigma-Aldrich) at a 1:5,000 dilution as described above.
Adherence to and translocation of leptospires through MDCK cells
Adherence of leptospires to MDCK cells was assessed as previously described [23]. MDCK cells (1 x 105) were added to round coverslips in 24-well plates and incubated until the formation of a near-confluent MDCK cell monolayer. Leptospira cells were incubated with MDCK at a multiplicity of infection (MOI) of 100 for 1 h at 37°C in 5% CO2. Following incubation, the suspensions were removed, and the monolayers were washed six times with warm PBS. The cells were fixed with pre-cold (-20°C) methanol for 10 min at 4°C, followed by three washes. Blocking buffer (10% fetal bovine sera in PBS) was then added to each well and incubation proceeded for 1 h at 37°C. To detect the adherent cells, a rabbit polyclonal antiserum against the protein LipL32 of Leptospira was used as primary antibody at a concentration of 1:200, followed by goat anti-rabbit antibodies conjugated with Alexa488 (Jackson ImmunoResearch) both at a concentration of 1:200 diluted in blocking buffer. Incubations were performed at 37°C for 1 h followed by three washes with PBS. After the final wash, the coverslips were removed from the 24-well plates, stained with DAPI, and mounted on a glass slide. Fluorescent-labeled leptospires associated to 100 MDCK cells on each of three poly-D-Lysine treated glass coverslips were enumerated. These three coverslips served as technical replicates for each strain tested during each trial.
Bacterial translocation across epithelial cells was assessed, as previously described [41]. MDCK cells (2 x 105 cells) were cultured on polycarbonate Millicell culture plate inserts (12-mm diameter, 3-μm pore size; Merck Millipore) at 37°C under 5% CO2 atmosphere. Transepithelial electrical resistance (TEER) of the filter-grown monolayers was measured using a Millicell-ERS device (Merck Millipore) as an index for integrity of the tight junctions (TJ). Polarized monolayers exhibiting TEER values of 150–300 Ωcm2 were used as an in vitro model of the epithelial barrier. The monolayers were infected with leptospires at a MOI of 100. The ability of Leptospira strains to translocate across the epithelial barrier was assessed by quantifying bacteria in the culture medium recovered from the lower chambers at 1, 2, 4, 6, and 8 h after infection.
Evaluation of virulence in hamster model of infection
The virulence of Manilae WT and the mutant strains (Δmpl36 and Δmpl36+) was assessed in 3-week male Golden Syrian hamsters, as described previously [41]. Groups of 4 hamsters were infected via intraperitoneal (IP) and ocular conjunctiva (CJ) routes with 108 leptospires. When appropriated, a LD50 experiment was performed using 108, 106 and 104 leptospires by IP route or 108 and 106 by CJ route. Experiments were repeated at least once for reproducibility. Animals were monitored twice daily for signs of disease and death, up to 21-days post-infection. Surviving animals at the end of the experiment or moribund animals showing difficulty in moving, breathing, and/or signs of bleeding or seizure were immediately sacrificed by inhalation of CO2. Blood, liver, and kidneys were collected from all animals after euthanasia. Kidneys were harvested and DNA was extracted for quantitative real-time PCR (qPCR) targeting lipL32, as previously described [41].
Bioinformatic and phylogenetic analysis
Tertiary structure prediction of the SPOR domains from RlpA of L. interrogans, L. fainei and L. biflexa tertiary structure prediction was determined by AlphaFold [58], and PyMOL software (version 2.5.4) was used for analysis. Sequences of MPL36 SPOR domain of L. interrogans and from 69 different species of Leptospira spp., representing pathogenic (P1 and P2) or saprophytes (S1, S2) bacteria, were obtained and aligned by ClustalX software (version 2.1). Phylogenetic tree was built with ClustalW software (version 2.1).
Statistical analysis
Prism 9 (GraphPad Software) was employed for all the statistical analysis of in vivo data. Fisher’s exact test and analysis of variance (ANOVA) with Bonferroni’s multiple comparisons post-tests were applied to assess statistical differences between pairs of groups and multiple groups, respectively. Experiments for degradation of ECM substrates and C3b were carried out with three or four replicates. Data were presented as mean ± SD or SEM as shown in the figures. All data were assessed by SPSS 11.5 Software. A P value of <0.05 was considered significant.
Supporting information
(A) Schematic representation of Himar1 transposon insertion positions in L. interrogans Manilae L495. The insertion sites of the transposon in the chromosome of the mpl36 gene in strain Manilae WT, and the insertion site of the transposon containing the spectinomycin resistance cassette and mpl36 gene for complementation are indicated. (B) Immunoblot analysis of Manilae WT, mutant Δmpl36 and complemented strain Δmpl36+ using a rabbit polyclonal antibody against rMPL36. The visible band has a molecular weight of ~40 kDa, which is in accordance with the predicted molecular weight of MPL36. The mutant strain lacks the expression of the protein. Molecular mass markers are shown on the left. (C) Motility assay results for Manilae WT, Δmpl36, and Δmpl36+ strains at 30°C. Bacteria (105 cells) were inoculated on 0.5% agarose EMJH plates (each square, 1 cm2) for 10 days. (D) Growth curve analysis of Manilae WT, Δmpl36, and Δmpl36+ strains at 30°C. Bacteria were grown in EMJH medium without agitation, and the counting was performed using dark field microscopy. Results represent the average ± the standard deviation of three independent experiments.
(TIFF)
(A) Whole intact Manilae WT (WCP) was treated with Triton X-114 for phase partitioning of Leptospira membrane proteins. Immuno-blot analysis was conducted with detergent (D) and aqueous (A) phase using polyclonal rabbit antisera against LigA (outer membrane), GroEL (cytoplasmic), and MPL36 proteins. Antibodies to rMPL36 in human sera from individuals with confirmed severe leptospirosis were measured by an ELISA assay. Reactivity of the rMPL36 with acute and convalescent serum samples was tested for IgM (B) and IgG (C) levels separately. The dashed line represents the threshold calculated based on 2.5 SD of the average OD signal of sera from healthy US individuals used as control. Data show the mean absorbance value at 450 nm ± the standard deviation of all individuals tested.
(TIFF)
(A) Tertiary predicted model of the SPOR domain of MPL36 in L. interrogans, visualized by PyMOL, showing the exposed lysine residues in blue. (B) Alignment of tertiary predicted structures of SPOR domain from L. interrogans (P1-red), L. fainei (P2-pink), and L. biflexa (S1-green), visualized by PyMOL, showing the exposed lysine residues. (C) Dendrogram resulting from multiple alignments performed by ClustalW of SPOR domain of MPL36 with other similar sequences of all 69 Leptospira species separated by groups: P1 (red), P2 (pink), S1 (green), and S2 (blue), identified by BLASTp. (D) Alignment of the SPOR domain of MPL36 with other similar sequences of all 69 Leptospira species: P1 (red), P2 (pink), S1 (green), and S2 (blue). Alignment was done using the ClustalX software and similar amino acids have the same colors.
(TIFF)
Strains Manilae WT, Δmpl36, Δmpl36+ (108 cells) were incubated with purified human PLG (10 μg). After washing, laminin (5 μg), vitronectin (2.5 μg) or C3b (1.5 μg) plus uPA (3 U) were added and incubated for up to 18 h. Leptospiral supernatants were collected and analyzed by western blot using anti-human vitronectin, laminin, or C3b (1:5,000) followed by peroxidase-conjugated secondary antibodies (1: 10,000).
(TIFF)
Tryptophan fluorescence emission spectra of rMPL36, rMPL36 aa41-305, rMPL36 aa41-235, and the corresponding unfolded proteins. Fluorescence measurements were carried out on a fluorescence spectrophotometer in a 1 cm path length rectangular quartz cuvette. The intrinsic fluorescence emission of native and unfolded proteins was measured in 10 mM PBS, with excitation at 280 nm and emission recorded in the range of 300–400 nm.
(TIFF)
(XLSX)
(XLSX)
Acknowledgments
We would like to thank Matilde Costa Lima de Souza and Daniella dos Santos Courrol (Laboratory of Bacteriology, Instituto Butantan, São Paulo, Brazil), and Dr. Karukriti K. Ghosh (Yale School of Public Health, CT, US) for technical assistance. We also wanted to thank Dr. Mathieu Picardeau (Institut Pasteur, Paris, France) for providing the Himar1 mutant of MPL36 (LIC10054) used in our studies.
Data Availability
All relevant data are within the manuscript and its supporting information files.
Funding Statement
This work was supported by NIH grants U01AI088752 and R01AI121207 (AIK), and R21AI163663 (EAWJ), FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo) grant 2018/12896-2 (ASB), Programa Ciências sem fronteiras, CNPq, Brazil grant 205952/2014-3 (CH), and FAPESP grant 2020/02678-8 (FJP). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lahteenmaki K, Kuusela P, Korhonen TK. Bacterial plasminogen activators and receptors. FEMS Microbiol Rev. 2001;25(5):531–52. doi: 10.1111/j.1574-6976.2001.tb00590.x . [DOI] [PubMed] [Google Scholar]
- 2.Sanderson-Smith ML, De Oliveira DM, Ranson M, McArthur JD. Bacterial plasminogen receptors: mediators of a multifaceted relationship. Journal of biomedicine & biotechnology. 2012;2012:272148. Epub 20121014. doi: 10.1155/2012/272148 ; PubMed Central PMCID: PMC3478875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barthel D, Schindler S, Zipfel PF. Plasminogen is a complement inhibitor. The Journal of biological chemistry. 2012;287(22):18831–42. Epub 20120327. doi: 10.1074/jbc.M111.323287 ; PubMed Central PMCID: PMC3365705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daroz BB, Fernandes LGV, Cavenague MF, Kochi LT, Passalia FJ, Takahashi MB, et al. A Review on Host-Leptospira Interactions: What We Know and Future Expectations. Frontiers in cellular and infection microbiology. 2021;11:777709. Epub 20211125. doi: 10.3389/fcimb.2021.777709 ; PubMed Central PMCID: PMC8657130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ko AI, Goarant C, Picardeau M. Leptospira: the dawn of the molecular genetics era for an emerging zoonotic pathogen. Nature reviews Microbiology. 2009;7(10):736–47. doi: 10.1038/nrmicro2208 ; PubMed Central PMCID: PMC3384523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, et al. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS neglected tropical diseases. 2015;9(9):e0003898. doi: 10.1371/journal.pntd.0003898 ; PubMed Central PMCID: PMC4574773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marotto PC, Nascimento CM, Eluf-Neto J, Marotto MS, Andrade L, Sztajnbok J, et al. Acute lung injury in leptospirosis: clinical and laboratory features, outcome, and factors associated with mortality. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 1999;29(6):1561–3. doi: 10.1086/313501 . [DOI] [PubMed] [Google Scholar]
- 8.Marotto PC, Ko AI, Murta-Nascimento C, Seguro AC, Prado RR, Barbosa MC, et al. Early identification of leptospirosis-associated pulmonary hemorrhage syndrome by use of a validated prediction model. The Journal of infection. 2010;60(3):218–23. Epub 2009/12/23. doi: 10.1016/j.jinf.2009.12.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segura ER, Ganoza CA, Campos K, Ricaldi JN, Torres S, Silva H, et al. Clinical spectrum of pulmonary involvement in leptospirosis in a region of endemicity, with quantification of leptospiral burden. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2005;40(3):343–51. Epub 2005/01/26. doi: 10.1086/427110 ; PubMed Central PMCID: PMC2366057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gouveia EL, Metcalfe J, de Carvalho AL, Aires TS, Villasboas-Bisneto JC, Queirroz A, et al. Leptospirosis-associated severe pulmonary hemorrhagic syndrome, Salvador, Brazil. Emerging infectious diseases. 2008;14(3):505–8. doi: 10.3201/eid1403.071064 ; PubMed Central PMCID: PMC2570821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panaphut T, Domrongkitchaiporn S, Thinkamrop B. Prognostic factors of death in leptospirosis: a prospective cohort study in Khon Kaen, Thailand. International journal of infectious diseases: IJID: official publication of the International Society for Infectious Diseases. 2002;6(1):52–9. doi: 10.1016/s1201-9712(02)90137-2 . [DOI] [PubMed] [Google Scholar]
- 12.Herath N, Uluwattage W, Weliwitiya T, Karunanayake L, Lekamwasam S, Ratnatunga N, et al. Sequel and therapeutic modalities of leptospirosis associated severe pulmonary haemorrhagic syndrome (SPHS); a Sri Lankan experience. BMC infectious diseases. 2019;19(1):451. Epub 20190522. doi: 10.1186/s12879-019-4094-0 ; PubMed Central PMCID: PMC6530063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis: a zoonotic disease of global importance. The Lancet infectious diseases. 2003;3(12):757–71. Epub 2003/12/04. doi: 10.1016/s1473-3099(03)00830-2 . [DOI] [PubMed] [Google Scholar]
- 14.Ko AI, Galvao Reis M, Ribeiro Dourado CM, Johnson WD Jr., Riley LW. Urban epidemic of severe leptospirosis in Brazil. Salvador Leptospirosis Study Group. Lancet. 1999;354(9181):820–5. doi: 10.1016/s0140-6736(99)80012-9 . [DOI] [PubMed] [Google Scholar]
- 15.Vincent AT, Schiettekatte O, Goarant C, Neela VK, Bernet E, Thibeaux R, et al. Revisiting the taxonomy and evolution of pathogenicity of the genus Leptospira through the prism of genomics. PLoS neglected tropical diseases. 2019;13(5):e0007270. Epub 2019/05/24. doi: 10.1371/journal.pntd.0007270 ; PubMed Central PMCID: PMC6532842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korba AA, Lounici H, Kainiu M, Vincent AT, Mariet JF, Veyrier FJ, et al. Leptospira ainlahdjerensis sp. nov., Leptospira ainazelensis sp. nov., Leptospira abararensis sp. nov. and Leptospira chreensis sp. nov., four new species isolated from water sources in Algeria. International journal of systematic and evolutionary microbiology. 2021;71(12). Epub 2021/12/17. doi: 10.1099/ijsem.0.005148 . [DOI] [PubMed] [Google Scholar]
- 17.Wunder EA Jr., Figueira CP, Santos GR, Lourdault K, Matthias MA, Vinetz JM, et al. Real-Time PCR Reveals Rapid Dissemination of Leptospira interrogans after Intraperitoneal and Conjunctival Inoculation of Hamsters. Infection and immunity. 2016;84(7):2105–15. doi: 10.1128/IAI.00094-16 ; PubMed Central PMCID: PMC4936353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gostic KM, Wunder EA Jr., Bisht V, Hamond C, Julian TR, Ko AI, et al. Mechanistic dose-response modelling of animal challenge data shows that intact skin is a crucial barrier to leptospiral infection. Philos Trans R Soc Lond B Biol Sci. 2019;374(1782):20190367. Epub 2019/08/14. doi: 10.1098/rstb.2019.0367 ; PubMed Central PMCID: PMC6711307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tahara H, Takabe K, Sasaki Y, Kasuga K, Kawamoto A, Koizumi N, et al. The mechanism of two-phase motility in the spirochete Leptospira: Swimming and crawling. Sci Adv. 2018;4(5):eaar7975. Epub 20180530. doi: 10.1126/sciadv.aar7975 ; PubMed Central PMCID: PMC5976277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charon NW, Cockburn A, Li C, Liu J, Miller KA, Miller MR, et al. The unique paradigm of spirochete motility and chemotaxis. Annu Rev Microbiol. 2012;66:349–70. Epub 2012/09/22. doi: 10.1146/annurev-micro-092611-150145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coburn J, Picardeau M, Woods CW, Veldman T, Haake DA. Pathogenesis insights from an ancient and ubiquitous spirochete. PLoS pathogens. 2021;17(10):e1009836. Epub 20211021. doi: 10.1371/journal.ppat.1009836 ; PubMed Central PMCID: PMC8530280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vieira ML, Fernandes LG, Domingos RF, Oliveira R, Siqueira GH, Souza NM, et al. Leptospiral extracellular matrix adhesins as mediators of pathogen-host interactions. FEMS microbiology letters. 2014;352(2):129–39. doi: 10.1111/1574-6968.12349 . [DOI] [PubMed] [Google Scholar]
- 23.Figueira CP, Croda J, Choy HA, Haake DA, Reis MG, Ko AI, et al. Heterologous expression of pathogen-specific genes ligA and ligB in the saprophyte Leptospira biflexa confers enhanced adhesion to cultured cells and fibronectin. BMC microbiology. 2011;11:129. doi: 10.1186/1471-2180-11-129 ; PubMed Central PMCID: PMC3133549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robbins GT, Hahn BL, Evangelista KV, Padmore L, Aranda PS, Coburn J. Evaluation of cell binding activities of Leptospira ECM adhesins. PLoS neglected tropical diseases. 2015;9(4):e0003712. Epub 20150414. doi: 10.1371/journal.pntd.0003712 ; PubMed Central PMCID: PMC4397020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.da Silva LB, Menezes MC, Kitano ES, Oliveira AK, Abreu AG, Souza GO, et al. Leptospira interrogans Secreted Proteases Degrade Extracellular Matrix and Plasma Proteins From the Host. Frontiers in cellular and infection microbiology. 2018;8:92. Epub 2018/04/11. doi: 10.3389/fcimb.2018.00092 ; PubMed Central PMCID: PMC5881292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verma A, Brissette CA, Bowman AA, Shah ST, Zipfel PF, Stevenson B. Leptospiral endostatin-like protein A is a bacterial cell surface receptor for human plasminogen. Infection and immunity. 2010;78(5):2053–9. Epub 2010/02/18. doi: 10.1128/IAI.01282-09 ; PubMed Central PMCID: PMC2863546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vieira ML, Vasconcellos SA, Goncales AP, de Morais ZM, Nascimento AL. Plasminogen acquisition and activation at the surface of leptospira species lead to fibronectin degradation. Infection and immunity. 2009;77(9):4092–101. doi: 10.1128/IAI.00353-09 ; PubMed Central PMCID: PMC2738053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vieira ML, Atzingen MV, Oliveira TR, Oliveira R, Andrade DM, Vasconcellos SA, et al. In vitro identification of novel plasminogen-binding receptors of the pathogen Leptospira interrogans. PloS one. 2010;5(6):e11259. doi: 10.1371/journal.pone.0011259 ; PubMed Central PMCID: PMC2889836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castiblanco-Valencia MM, Fraga TR, Pagotto AH, Serrano SM, Abreu PA, Barbosa AS, et al. Plasmin cleaves fibrinogen and the human complement proteins C3b and C5 in the presence of Leptospira interrogans proteins: A new role of LigA and LigB in invasion and complement immune evasion. Immunobiology. 2016;221(5):679–89. Epub 2016/01/30. doi: 10.1016/j.imbio.2016.01.001 . [DOI] [PubMed] [Google Scholar]
- 30.Wolff DG, Castiblanco-Valencia MM, Abe CM, Monaris D, Morais ZM, Souza GO, et al. Interaction of Leptospira elongation factor Tu with plasminogen and complement factor H: a metabolic leptospiral protein with moonlighting activities. PloS one. 2013;8(11):e81818. Epub 20131127. doi: 10.1371/journal.pone.0081818 ; PubMed Central PMCID: PMC3842364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salazar N, Souza MC, Biasioli AG, Silva LB, Barbosa AS. The multifaceted roles of Leptospira enolase. Research in microbiology. 2017;168(2):157–64. Epub 20161029. doi: 10.1016/j.resmic.2016.10.005 . [DOI] [PubMed] [Google Scholar]
- 32.Vieira ML, Atzingen MV, Oliveira R, Mendes RS, Domingos RF, Vasconcellos SA, et al. Plasminogen binding proteins and plasmin generation on the surface of Leptospira spp.: the contribution to the bacteria-host interactions. Journal of biomedicine & biotechnology. 2012;2012:758513. doi: 10.1155/2012/758513 ; PubMed Central PMCID: PMC3481863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arends SJ, Williams K, Scott RJ, Rolong S, Popham DL, Weiss DS. Discovery and characterization of three new Escherichia coli septal ring proteins that contain a SPOR domain: DamX, DedD, and RlpA. Journal of bacteriology. 2010;192(1):242–55. doi: 10.1128/JB.01244-09 ; PubMed Central PMCID: PMC2798263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gerding MA, Liu B, Bendezu FO, Hale CA, Bernhardt TG, de Boer PA. Self-enhanced accumulation of FtsN at Division Sites and Roles for Other Proteins with a SPOR domain (DamX, DedD, and RlpA) in Escherichia coli cell constriction. Journal of bacteriology. 2009;191(24):7383–401. Epub 20090814. doi: 10.1128/JB.00811-09 ; PubMed Central PMCID: PMC2786604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yahashiri A, Jorgenson MA, Weiss DS. The SPOR Domain, a Widely Conserved Peptidoglycan Binding Domain That Targets Proteins to the Site of Cell Division. Journal of bacteriology. 2017;199(14). Epub 20170627. doi: 10.1128/JB.00118-17 ; PubMed Central PMCID: PMC5494741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alcorlo M, Dik DA, De Benedetti S, Mahasenan KV, Lee M, Dominguez-Gil T, et al. Structural basis of denuded glycan recognition by SPOR domains in bacterial cell division. Nat Commun. 2019;10(1):5567. Epub 20191205. doi: 10.1038/s41467-019-13354-4 ; PubMed Central PMCID: PMC6895207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jorgenson MA, Chen Y, Yahashiri A, Popham DL, Weiss DS. The bacterial septal ring protein RlpA is a lytic transglycosylase that contributes to rod shape and daughter cell separation in Pseudomonas aeruginosa. Molecular microbiology. 2014;93(1):113–28. Epub 20140523. doi: 10.1111/mmi.12643 ; PubMed Central PMCID: PMC4086221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murray GL, Morel V, Cerqueira GM, Croda J, Srikram A, Henry R, et al. Genome-wide transposon mutagenesis in pathogenic Leptospira species. Infection and immunity. 2009;77(2):810–6. doi: 10.1128/IAI.01293-08 ; PubMed Central PMCID: PMC2632054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barbosa AS, Monaris D, Silva LB, Morais ZM, Vasconcellos SA, Cianciarullo AM, et al. Functional characterization of LcpA, a surface-exposed protein of Leptospira spp. that binds the human complement regulator C4BP. Infection and immunity. 2010;78(7):3207–16. doi: 10.1128/IAI.00279-10 ; PubMed Central PMCID: PMC2897400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gamberini M, Gomez RM, Atzingen MV, Martins EA, Vasconcellos SA, Romero EC, et al. Whole-genome analysis of Leptospira interrogans to identify potential vaccine candidates against leptospirosis. FEMS microbiology letters. 2005;244(2):305–13. doi: 10.1016/j.femsle.2005.02.004 . [DOI] [PubMed] [Google Scholar]
- 41.Wunder EA Jr., Figueira CP, Benaroudj N, Hu B, Tong BA, Trajtenberg F, et al. A novel flagellar sheath protein, FcpA, determines filament coiling, translational motility and virulence for the Leptospira spirochete. Molecular microbiology. 2016;101(3):457–70. doi: 10.1111/mmi.13403 ; PubMed Central PMCID: PMC4979076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oliveira R, Domingos RF, Siqueira GH, Fernandes LG, Souza NM, Vieira ML, et al. Adhesins of Leptospira interrogans mediate the interaction to fibrinogen and inhibit fibrin clot formation in vitro. PLoS neglected tropical diseases. 2013;7(8):e2396. Epub 20130829. doi: 10.1371/journal.pntd.0002396 ; PubMed Central PMCID: PMC3757074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hartwig DD, Seixas FK, Cerqueira GM, McBride AJ, Dellagostin OA. Characterization of the immunogenic and antigenic potential of putative lipoproteins from Leptospira interrogans. Current microbiology. 2011;62(4):1337–41. doi: 10.1007/s00284-010-9865-1 . [DOI] [PubMed] [Google Scholar]
- 44.Ono E, Takase H, Naiki M, Yanagawa R. Purification, characterization and serological properties of a glycolipid antigen reactive with a serovar-specific monoclonal antibody against Leptospira interrogans serovar canicola. Journal of general microbiology. 1987;133(5):1329–36. Epub 1987/05/01. doi: 10.1099/00221287-133-5-1329 . [DOI] [PubMed] [Google Scholar]
- 45.Caimano MJ, Sivasankaran SK, Allard A, Hurley D, Hokamp K, Grassmann AA, et al. A model system for studying the transcriptomic and physiological changes associated with mammalian host-adaptation by Leptospira interrogans serovar Copenhageni. PLoS pathogens. 2014;10(3):e1004004. doi: 10.1371/journal.ppat.1004004 ; PubMed Central PMCID: PMC3953431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adhikarla H, Wunder EA Jr., Mechaly AE, Mehta S, Wang Z, Santos L, et al. Lvr, a Signaling System That Controls Global Gene Regulation and Virulence in Pathogenic Leptospira. Frontiers in cellular and infection microbiology. 2018;8:45. Epub 2018/03/31. doi: 10.3389/fcimb.2018.00045 ; PubMed Central PMCID: PMC5863495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wunder EA, Adhikarla H, Hamond C, Owers Bonner KA, Liang L, Rodrigues CB, et al. A live attenuated-vaccine model confers cross-protective immunity against different species of the Leptospira genus. Elife. 2021;10. Epub 2021/01/27. doi: 10.7554/eLife.64166 ; PubMed Central PMCID: PMC7837694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pazos M, Peters K, Boes A, Safaei Y, Kenward C, Caveney NA, et al. SPOR Proteins Are Required for Functionality of Class A Penicillin-Binding Proteins in Escherichia coli. mBio. 2020;11(6). Epub 20201103. doi: 10.1128/mBio.02796-20 ; PubMed Central PMCID: PMC7642682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Passalia FJ, Heinemann MB, de Andrade SA, Nascimento A, Vieira ML. Leptospira interrogans Bat proteins impair host hemostasis by fibrinogen cleavage and platelet aggregation inhibition. Medical microbiology and immunology. 2020;209(2):201–13. Epub 20200220. doi: 10.1007/s00430-020-00664-4 . [DOI] [PubMed] [Google Scholar]
- 50.Sumitomo T, Nakata M, Higashino M, Yamaguchi M, Kawabata S. Group A Streptococcus exploits human plasminogen for bacterial translocation across epithelial barrier via tricellular tight junctions. Sci Rep. 2016;7:20069. Epub 20160129. doi: 10.1038/srep20069 ; PubMed Central PMCID: PMC4731814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fulde M, Rohde M, Polok A, Preissner KT, Chhatwal GS, Bergmann S. Cooperative plasminogen recruitment to the surface of Streptococcus canis via M protein and enolase enhances bacterial survival. mBio. 2013;4(2):e00629–12. Epub 20130312. doi: 10.1128/mBio.00629-12 ; PubMed Central PMCID: PMC3604778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Law RH, Caradoc-Davies T, Cowieson N, Horvath AJ, Quek AJ, Encarnacao JA, et al. The X-ray crystal structure of full-length human plasminogen. Cell Rep. 2012;1(3):185–90. Epub 20120308. doi: 10.1016/j.celrep.2012.02.012 . [DOI] [PubMed] [Google Scholar]
- 53.Johnson RC, Harris VG. Differentiation of pathogenic and saprophytic letospires. I. Growth at low temperatures. Journal of bacteriology. 1967;94(1):27–31. doi: 10.1128/jb.94.1.27-31.1967 ; PubMed Central PMCID: PMC251866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Haake DA, Matsunaga J. Characterization of the leptospiral outer membrane and description of three novel leptospiral membrane proteins. Infection and immunity. 2002;70(9):4936–45. Epub 2002/08/17. doi: 10.1128/IAI.70.9.4936-4945.2002 ; PubMed Central PMCID: PMC128291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ramos CR, Abreu PA, Nascimento AL, Ho PL. A high-copy T7 Escherichia coli expression vector for the production of recombinant proteins with a minimal N-terminal His-tagged fusion peptide. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas / Sociedade Brasileira de Biofisica [et al. ]. 2004;37(8):1103–9. Epub 20040720. doi: 10.1590/s0100-879x2004000800001 . [DOI] [PubMed] [Google Scholar]
- 56.Ghisaidoobe AB, Chung SJ. Intrinsic tryptophan fluorescence in the detection and analysis of proteins: a focus on Forster resonance energy transfer techniques. Int J Mol Sci. 2014;15(12):22518–38. Epub 20141205. doi: 10.3390/ijms151222518 ; PubMed Central PMCID: PMC4284722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Picardeau M. Toolbox of Molecular Techniques for Studying Leptospira Spp. Current topics in microbiology and immunology. 2018;415:141–62. doi: 10.1007/82_2017_45 . [DOI] [PubMed] [Google Scholar]
- 58.Jumper J, Evans R, Pritzel A, Green T, Figurnov M, Ronneberger O, et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596(7873):583–9. Epub 20210715. doi: 10.1038/s41586-021-03819-2 ; PubMed Central PMCID: PMC8371605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Schematic representation of Himar1 transposon insertion positions in L. interrogans Manilae L495. The insertion sites of the transposon in the chromosome of the mpl36 gene in strain Manilae WT, and the insertion site of the transposon containing the spectinomycin resistance cassette and mpl36 gene for complementation are indicated. (B) Immunoblot analysis of Manilae WT, mutant Δmpl36 and complemented strain Δmpl36+ using a rabbit polyclonal antibody against rMPL36. The visible band has a molecular weight of ~40 kDa, which is in accordance with the predicted molecular weight of MPL36. The mutant strain lacks the expression of the protein. Molecular mass markers are shown on the left. (C) Motility assay results for Manilae WT, Δmpl36, and Δmpl36+ strains at 30°C. Bacteria (105 cells) were inoculated on 0.5% agarose EMJH plates (each square, 1 cm2) for 10 days. (D) Growth curve analysis of Manilae WT, Δmpl36, and Δmpl36+ strains at 30°C. Bacteria were grown in EMJH medium without agitation, and the counting was performed using dark field microscopy. Results represent the average ± the standard deviation of three independent experiments.
(TIFF)
(A) Whole intact Manilae WT (WCP) was treated with Triton X-114 for phase partitioning of Leptospira membrane proteins. Immuno-blot analysis was conducted with detergent (D) and aqueous (A) phase using polyclonal rabbit antisera against LigA (outer membrane), GroEL (cytoplasmic), and MPL36 proteins. Antibodies to rMPL36 in human sera from individuals with confirmed severe leptospirosis were measured by an ELISA assay. Reactivity of the rMPL36 with acute and convalescent serum samples was tested for IgM (B) and IgG (C) levels separately. The dashed line represents the threshold calculated based on 2.5 SD of the average OD signal of sera from healthy US individuals used as control. Data show the mean absorbance value at 450 nm ± the standard deviation of all individuals tested.
(TIFF)
(A) Tertiary predicted model of the SPOR domain of MPL36 in L. interrogans, visualized by PyMOL, showing the exposed lysine residues in blue. (B) Alignment of tertiary predicted structures of SPOR domain from L. interrogans (P1-red), L. fainei (P2-pink), and L. biflexa (S1-green), visualized by PyMOL, showing the exposed lysine residues. (C) Dendrogram resulting from multiple alignments performed by ClustalW of SPOR domain of MPL36 with other similar sequences of all 69 Leptospira species separated by groups: P1 (red), P2 (pink), S1 (green), and S2 (blue), identified by BLASTp. (D) Alignment of the SPOR domain of MPL36 with other similar sequences of all 69 Leptospira species: P1 (red), P2 (pink), S1 (green), and S2 (blue). Alignment was done using the ClustalX software and similar amino acids have the same colors.
(TIFF)
Strains Manilae WT, Δmpl36, Δmpl36+ (108 cells) were incubated with purified human PLG (10 μg). After washing, laminin (5 μg), vitronectin (2.5 μg) or C3b (1.5 μg) plus uPA (3 U) were added and incubated for up to 18 h. Leptospiral supernatants were collected and analyzed by western blot using anti-human vitronectin, laminin, or C3b (1:5,000) followed by peroxidase-conjugated secondary antibodies (1: 10,000).
(TIFF)
Tryptophan fluorescence emission spectra of rMPL36, rMPL36 aa41-305, rMPL36 aa41-235, and the corresponding unfolded proteins. Fluorescence measurements were carried out on a fluorescence spectrophotometer in a 1 cm path length rectangular quartz cuvette. The intrinsic fluorescence emission of native and unfolded proteins was measured in 10 mM PBS, with excitation at 280 nm and emission recorded in the range of 300–400 nm.
(TIFF)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its supporting information files.