Background:
Gigantomastia causes severe back pain, postural imbalance, intertrigo, and psychosocial disablement. Multiple breast reduction techniques exist. Breast reduction with free nipple graft reconstruction is the preferred treatment. We found that the medial pedicle Wise-pattern (MPWP) technique is an equally safe and effective technique.
Methods:
Review of our institution’s electronic medical record between February 2020 and February 2023 identified women with gigantomastia who underwent bilateral reduction with more than 1500 g resected in at least one breast. Multinomial logistical regressions were used to identify associations between comorbidities, operative techniques, postoperative complications, and nipple areolar complex function.
Results:
Thirty-one patients underwent bilateral reduction mammaplasty. Total bilateral resection weight and average body mass index (BMI) were 3828 g and 40 kg per m2. Common comorbidities were hypertension (38%) and tobacco use (26%). MPWP was used predominantly (65%), followed by inferior pedicle (16%) and superior-medial pedicle (10%). Complications included loss of nipple areolar complex sensation (23%) and wound dehiscence (16%). Reduction technique was not associated with increased surgical complications (odds ratio = 0.75, P = 0.273). Age, excision amount, use of postsurgical drains, and BMI were not associated with increased complications (P = 0.29, P = 0.55, P = 0.74, P = 0.41). Rates of areolar sensation loss were higher in larger BMIs, but this was not statistically significant (P = 0.051).
Conclusions:
The MPWP reduction technique is an equally safe and effective treatment of gigantomastia when compared with reduction with free nipple graft reconstruction. There is the added benefit of preserved nipple sensation without increased postoperative complications.
Takeaways
Question: Is the medial pedicle technique a safe surgical technique for treating gigantomastia?
Findings: There were 31 patients diagnosed with gigantomastia at our facility who underwent mammoplasty. Of these patients, 65% underwent reduction with a medial pedicle Wise-pattern technique. The majority of our patient population maintained full sensitivity to the nipple areolar complex after a medial pedicle Wise-pattern technique reduction without experiencing an increase in other common surgical complications.
Meaning: The patient outcomes presented demonstrate the potential of the medial pedicle technique to be a safe and effective method for reductions for a wide range of breast sizes, including those meeting inclusion criteria for gigantomastia.
INTRODUCTION
Gigantomastia is a rare condition that is characterized by excessive breast growth. This condition is associated with obesity, but may also present idiopathically with normal BMI.1 Literature review suggests that sufficient treatment of gigantomastia requires a reduction of at least 1500 g per breast; however, there is discordance amongst the literature, with weights ranging from 800 to 2000 g.2–4 Although it can be technically challenging, reductive surgery for gigantomastia yields significant rewards to the patient, such as relief of front-loaded weight and posture correction. Nevertheless, there are multiple complications associated with breast reduction surgery, including, but not limited to hypopigmentation, nipple-areola complex (NAC) necrosis, and reduced or complete loss of NAC sensation.1–3,5–8 This is more common in women who are overweight, use tobacco products, and have a larger breast reduction resection weight.9,10
There are multiple techniques for breast reduction surgery for mild to moderate breast hypertrophy. There is debate about which method is considered the safest and most effective for gigantomastia. Traditionally, breast reduction with a free-nipple grafting (FNG) has been the mainstay in large reductions, as it avoids potential NAC necrosis, which results from compression of the nipple blood vessels from a bulky pedicle. Indications for breast reduction using FNG may include breast removal weight of 2000 g per breast and if the patient is of advanced age, has poor microcirculation, prior breast incision that would limit skin flap viability, or a history of radiation or systemic illness that impairs wound healing.9,11,12 Despite its advantages, breast reduction using FNG is associated with several drawbacks, including loss of NAC sensation, poor projection, loss of lactation, and uneven NAC pigmentation.13,14 The goal of this study was to identify a reduction technique that could achieve great aesthetic results while maintaining nipple function.
Our institution utilizes a variety of reduction techniques, including inferior and superior-medial pedicle with preserved NAC and breast reduction with FNG. Recently, the medial pedicle Wise-pattern (MPWP) reduction has become a common practice at our academic institution for both macromastia and gigantomastia. Our data demonstrate that a MPWP reduction for patients with gigantomastia requiring a significant nipple elevation is safe and allows for nipple sensation preservation.
METHODS
This is a retrospective review of our facility’s electronic medical record system of patients diagnosed with gigantomastia between February 2020 and February 2023 who underwent bilateral reduction surgery. Gigantomastia was defined as requiring greater than 1500 g resected in at least one breast. We identified 31 patients who met this inclusion criteria. Demographic variables abstracted included age, body mass index (BMI), comorbid conditions, tobacco use, and total surgical resection weight. We also compiled data on the frequency at which each surgical technique was used as well as types and rates of complications associated with each technique. Complications included infection (diagnosed within 30 days of operation), wound dehiscence requiring wound care, nipple loss (full and partial), decreased sensation to the NAC, complete sensation loss to the NAC, seromas and/or hematomas which required evacuation, need for reoperation, and scar revision (including keloid). Nipple sensation was assessed preoperatively by subjective reporting of the presence or absence of nipple sensation. Postoperatively, patients were again assessed for nipple sensation and degree of sensation change. Reoperation was classified as any complication that required the patient to undergo general anesthesia in the operating room for a surgical correction. A multinomial logistical regression in STATA SE16 was used to identify associations between types of postoperative complications and the type of reduction technique used. Statistical significance was designated at a P value of less than 0.05.
MEDIAL PEDICLE TECHNIQUE
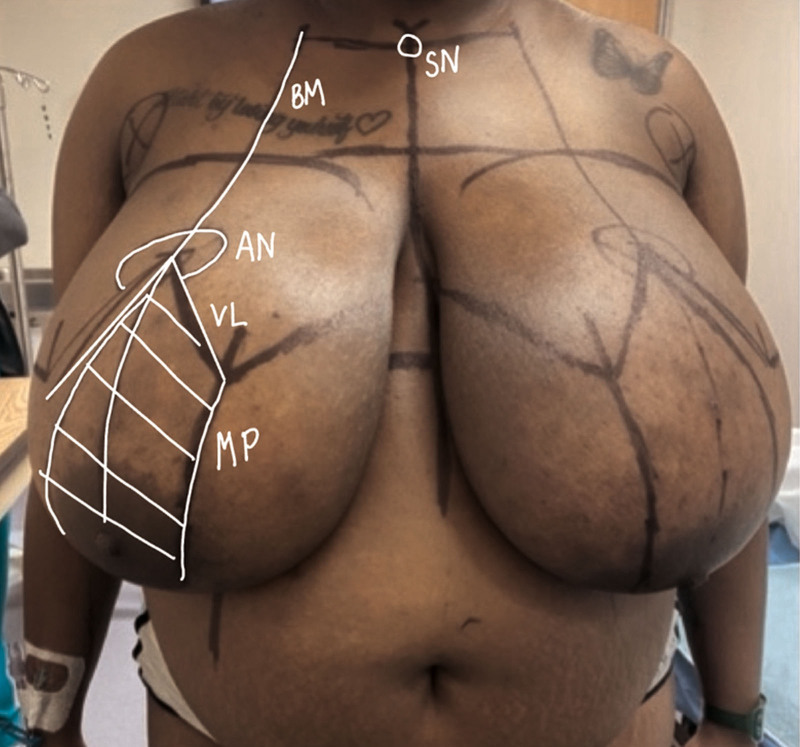
Preoperative marking is imperative to achieve aesthetic results. Patients are marked while standing, as shown in Figure 1. Breast landmarks for reduction include the sternal notch, mid-chest, breast meridian, inframammary fold, the new NAC position, and predicted skin and soft tissue resection.
Fig. 1.
Preoperative markings define SN (sternal notch), BM (breast meridian), AN (anticipated NAC placement), VL (vertical limbs of the Wise patterns), and MP (medial pedicle).
The median sternal line is marked from the sternal notch to the umbilicus. The breast meridian is measured and marked at 6 to 8 cm from the sternal notch, and a vertical line is made down each breast. The upper breast border is identified by elevating the breast and determining where the breast begins to project. The anticipated NAC position is marked 20 cm from the sternal notch along the breast meridian or 8 cm from the UBB. From this point, two vertical limbs are created to make an inverted V, each limb measuring 10–11 cm. The length of the pillars will be longer for dense and very ptotic breast (defined as breast 40–45 cm long). The inframammary fold (IMF) is outlined and connected to the inverted V. The pedicle base width is about 8 cm and is outlined from the medial vertical limb, going around the nipple, ensuring to leave a rim of skin around the areola, and terminating of the inferior edge of the medial vertical limb.
The breast is held taut with a tourniquet, and the diameter of the NAC is marked between 35 and 42 mm. The pedicle is de-epithelialized, as shown in Figure 2, leaving a cuff of tissue around the NAC. Dissection is carried down to the pectoralis fascia along the previous markings, taking care to maintain a wide pedicle and to refrain from undermining to preserve the neurovascular supply to the flap and NAC. A lateral breast flap of 2–3 cm thickness is elevated starting at the apex of the vertical pillars and extending to the upper and lateral breast borders. Adequate soft tissue is excised above the superior margin of the pedicle to allow for optimal insetting of the pedicle. The excess skin and parenchyma is excised en bloc. The resultant medial pedicle and skin flaps are shown in Figure 3. The pedicle is then rotated such that the NAC is now at the apex of the wound. Debulking the pedicle may be required for proper insetting. Tacking stitches to secure the pedicle in place is optional. The skin is approximated with staples, and the patient is placed in reverse Trendelenburg position to assess shape, size, and symmetry, and determine ideal NAC placement, also shown in Figure 3. The nipple is generally 7 cm from the IMF with a 42 cm diameter. Keyholes are incised for the nipples. The medial portion is de-epithelialized rather than a full thickness incision so as to not compromise the pedicle. A drain may be placed before definitive closure based on surgeon preference. Formal insetting of all incisions is performed with 3-0 Monocryl deep dermal suture and 3-0 Monocryl subcuticular suture. The skin closure of the NAC around the areola is done with 5-0 absorbable Monocryl suture. Figure 4 shows the reduction after closure with sutures and placement of the Dermabond Pernio skin closure system.
Fig. 2.
De-epithelialized medial pedicle.
Fig. 3.
The patient’s right-hand side depicts the remaining breast parenchyma after excision of the excess inferolateral skin and breast tissue. Remaining is the medial pedicle with intact NAC. The patient’s left-hand side depicts the anticipated size and shape after the pedicle has been tailor tacked.
Fig. 4.
Immediate postoperative photograph after medial pedicle breast reduction. Periareolar incisions are dressed with steristrips.
RESULTS
This study identified 31 patients diagnosed with gigantomastia who underwent bilateral mammaplasty. Median age was 39 years, and average total bilateral resection was 3828 g. Average BMI was 40 kg per m2, and the most common comorbidities were hypertension (38%), diabetes mellitus (16%), and hyperlipidemia (9.68%). Current or former cigarette use was reported in 26% of patients. Patient demographics, resection weights, and patient comorbidities are shown in Table 1.
Table 1.
Demographic, Resection Weight Data, and Frequency of Comorbidities from 31 Patients Receiving Bilateral Mammoplasty Reduction for Gigantomastia
| Variables | Mean (IQR) |
|---|---|
| Age (y) | 38.5 (18–68) |
| BMI (kg/m2) | 40.1 (23.6–60.1) |
| Total resection weight (g) | 3828 (2780–7500) |
| Comorbidities | Overall Population, n (%) |
| Hypertension | 12 (38.71) |
| Nicotine use | 7 (22.58) |
| Diabetes mellitus | 5 (16.45) |
| Hyperlipidemia | 3 (9.68) |
| Connective tissue disorder | 2 (6.45) |
| Vitamin deficiency | 1 (3.23) |
| Hyperglycemia | 1 (3.23) |
| Hypercholesteremia | 1 (3.23) |
| Hypothyroidism | 1 (3.23) |
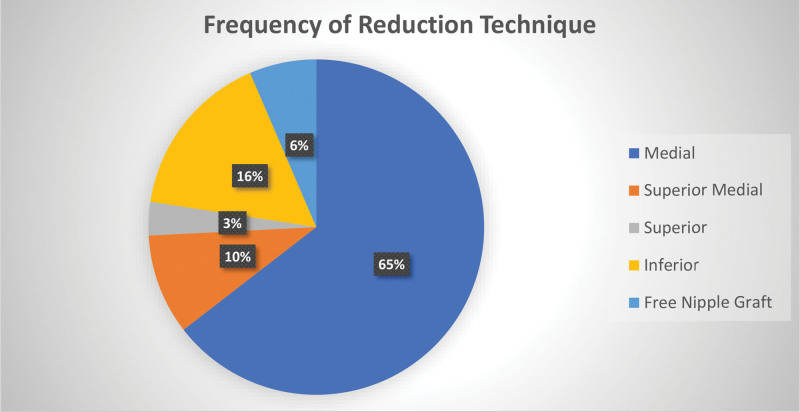
Medial pedicle with Wise-pattern skin reduction was the most common surgical technique used (65%) followed by inferior pedicle (16%), superior-medial pedicle (10%), breast reduction using FNG (6%), and superior pedicle (3%). Surgical drains were used in 94% of cases. Complications encountered are listed in Table 3. The most reported were complete sensation loss to the NAC (N = 5, 16%) and minor wound dehiscence (N = 5, 16%). In total, 23% of all patients had decreased or complete loss of sensation to the NAC. Frequency of reduction technique is shown in Figure 5, and frequency of complications by reduction technique is shown in Table 2. All wound complications were treated out-patient without need for reoperation.
Table 3.
Multinomial Logistical Regression to Test Independent Relationships between Age, Excision Weight, Drains, BMI, Smoking Status, and Surgical Technique to Postsurgical Complications
| Variables | OR Ratio | SE | 95% CI | P |
|---|---|---|---|---|
| Age | 1.04 | 0.034 | [0.970–1.105] | 0.293 |
| Excision weight | 1.00 | 0.002 | [0.995–1.005] | 0.55 |
| Drains | 0.96 | 0.001 | [0.985–1.007] | 0.741 |
| BMI | 0.947 | 0.062 | [0.834–1.076] | 0.405 |
| Smoking status | 2.580 | 2.691 | [0.334–19.928] | 0.334 |
| Surgical technique | 0.654 | 0.296 | [0.269–1.590] | 0.349 |
Fig. 5.
Frequency of surgical techniques.
Table 2.
Frequency of Postsurgical Complications by Reduction Technique
| Complications | Reduction Technique | Total n (%) | ||||
|---|---|---|---|---|---|---|
| Medial, n (%) | Superior Medial, n (%) | Superior, n (%) | Inferior, n (%) | Free Nipple Graft, n (%) | ||
| None | 5 (41.6) | 3 (25) | 0 (0) | 4 (33.3) | 0 (0) | 12 (100) |
| Epidermolysis | 2 (66.6) | 0 (0) | 0 (0) | 0 (0) | 1 (33.3) | 3 (100) |
| Complete sensation loss to areola | 3 (60) | 0 (0) | 1 (20) | 0 (0) | 1 (20) | 5 (100) |
| Wound dehiscence | 4 (80) | 0 (0) | 0 (0) | 1 (20) | 0 (0) | 5 (100) |
| Hypertrophic scarring | 2 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (100) |
| Decreased sensation to areola | 2 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (100) |
| Partial areolar necrosis | 2 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (100) |
| Total | 20 (62.5) | 3 (9.7) | 1 (3.2) | 5 (16.1) | 2 (6.45) | 31 (100) |
Multinomial logistical regression found that reduction technique was not associated with increased odds of having a surgical complication (OR = 0.75, P = 0.273). Additionally, age (OR = 1.04, P = 0.293), excision amount (OR = 1.00, P = 0.55), use of postsurgical drains (OR = 0.96, P = 0.741), and BMI (OR = 0.95, P = 0.405) were not associated with increased complications. Table 3 shows the independent relationship between patient and surgical factors and development of postoperative complications.
Complete sensation loss to the NAC was reported at higher rates in patients with increased BMIs; however, it was not statistically significant (N = 31, P = 0.051). Current and former smokers had increased odds for epidermolysis when compared with nonsmokers; however, this was not statistically significant (P = 0.0602). Table 4 reports statistical outcomes for the three most common complications observed in this study: epidermolysis, wound dehiscence, and complete sensation loss to the NAC. Pre- and postoperative photographs of the three patients included in the study are shown in Figures 6–8. Figures include preoperative and postoperative photographs.
Table 4.
Multinomial Logistical Regression to Test Independent Relationships between Surgical Technique, Drains, and BMI to Epidermolysis, Sensation Loss to NAC, and Wound Dehiscence
| Variables | Independent Variable | Beta-Coefficient | SE | 95% CI | P |
|---|---|---|---|---|---|
| Epidermolysis | Surgical technique | −0.576 | 0.778 | [−2.101 to 0.949] | 0.459 |
| Drains | 3.743 | 3.662 | [−3.434 to 10.919] | 0.307 | |
| BMI | −0.132 | 0.102 | [−0.331 to 0.067] | 0.192 | |
| Complete sensation loss to NAC | Surgical technique | 0.333 | 0.479 | [−0.606 to 1.272] | 0.487 |
| Drains | 9.954 | 5.604 | [−1.030 to 20.938] | 0.076 | |
| BMI | −0.291 | 0.149 | [−0.583 to 0.001] | 0.051 | |
| Wound dehiscence | Surgical technique | −0.293 | 0.607 | [−1.484 to 0.898] | 0.898 |
| Drains | 9.427 | 5.356 | [−1.072 to 19.925] | 0.078 | |
| BMI | −0.254 | 0.142 | [−0.533 to 0.245] | 0.074 |
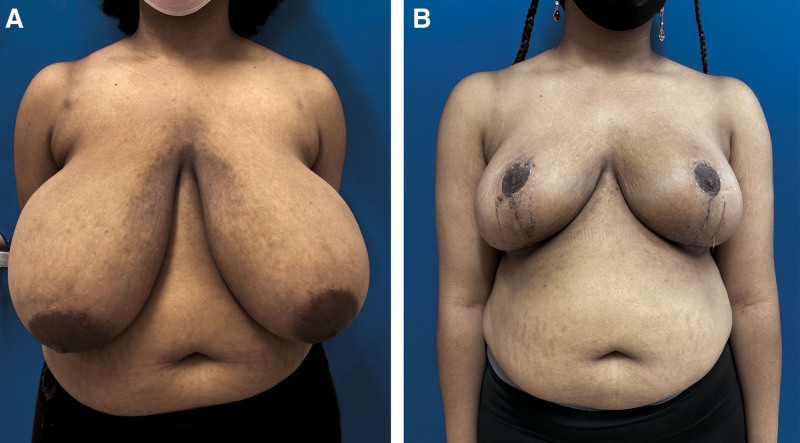
Fig. 6.
A 57-year-old patient who underwent breast reduction with medial pedicle Wise-pattern reduction. A, Preoperative photograph of 57-year-old patient who presented to clinic with gigantomastia. B, Postoperative day 86 after reduction weight of 3365 grams on left, 2810 grams on right.
Fig. 8.
An 18-year-old patient who underwent breast reduction with medial pedicle Wise-pattern reduction. A, Preoperative photograph of an 18-year-old patient who presented to clinic with gigantomastia. B, Postoperative day 25 after reduction weight of 1450 grams on left, 1550 grams on right.
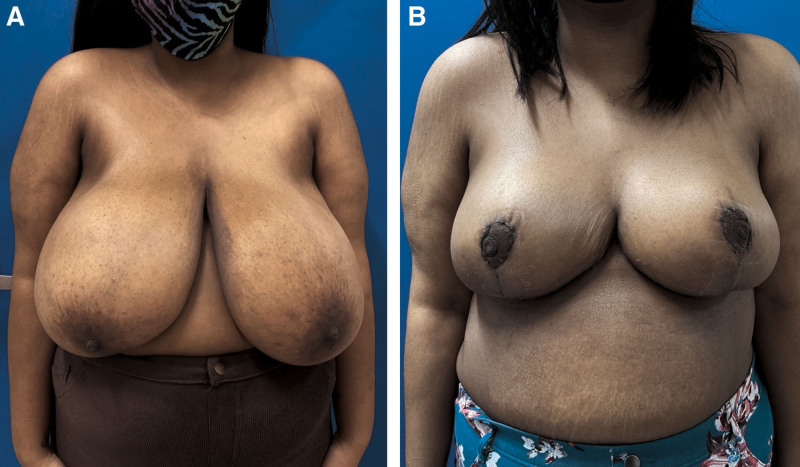
Fig. 7.
A 25-year-old patient who underwent breast reduction with medial pedicle Wise-pattern reduction. A, Preoperative photograph of 25-year-old patient who presented to clinic with gigantomastia. B, Postoperative day 18 after reduction weight of 2150 grams on left, 2222 grams on right.
DISCUSSION
The mainstay for treatment of gigantomastia is breast reduction using FNG due to concern about adequate nipple perfusion with such a long pedicle. This can result in changes in nipple color, texture, lack of nipple sensation, and an 18% risk of graft failure.7,15 Consequently, breast reduction using FNG is generally reserved for noncomplex reconstruction. Decision to perform reduction with FNG reconstruction was made intraoperatively if the blood supply to the NAC appeared tenuous after final resection. Superior pedicle was performed if patient had previous instrumentation of the medial breast, which would compromise predictable blood flow. Inferior pedicle was used in our patients if the inframammary fold to nipple distance was less than 20 cm in someone with a sternal notch to nipple distance of 40 cm or more.
The superomedial pedicle (SMP) technique provides clinical benefits to the patient without increasing surgical risks or postoperative complications.1,2,5,7,9,16–20 This technique was previously considered precarious because the width of the pedicle was felt to be inadequate to deliver perfusion of the NAC. Recent studies have shown that not only is the blood supply adequate, but there is preservation of sensation and creation of an aesthetic breast shape.1,2,6,15,21
Inherent to its design, the SMP technique preserves the second, third, and fourth internal mammary artery, the dominant blood supply to the NAC.22–25 This technique also preserves the third and fourth anterior cutaneous sensory branches of the intercostal nerves: one of the primary sensory pathways to the NAC. The third and fourth lateral cutaneous branches are often compromised, which have also been shown to be contributory to nipple sensation and may explain possible nipple dysfunction after reductive surgery.26,27 Preservation of upper-middle-inner quadrant of the breast using the SMP provides a more rounded full breast shape, thus avoiding the bottoming-out effect commonly associated with the inferior pedicle. We aimed to perform a superomedial pedicle reduction in all patients to preserve the second intercostal perforator, which lies in the 12 o’clock position; however, if the pedicle was too bulky after rotation, the superior pole was excised, thereby sacrificing the second intercostal artery. The resultant medial pedicle preserves the third and fourth intercostal perforators, yielding adequate blood flow to the NAC and a cosmetic outcome comparable to the that of SMP.
The superior-medial pedicle reduction is not without its own set of surgical risks particularly in the setting of gigantomastia. The risk of complication increases for patients with projected reduction weights of more than 800 g, BMI of more than 28, and grade III ptosis.28 The most common complication is full NAC necrosis. A longer SNN distance yields a longer pedicle, and a higher risk for vascular complications during transposition given variability in the course and vigor of the resultant blood supply after extensive dissection. This demonstrates a clear indication for further research of alternative techniques, particularly for large breast reductions.
Use of the inferior pedicle for gigantomastia reductions has become a popular and more widely used alternative technique, particularly throughout the United States. The use of this pedicle has afforded surgeons great success at preserving sensation to the NAC, and therefore, an obvious advantage over breast reduction using FNG. A well-documented drawback of the inferior pedicle is the “bottoming out” phenomenon, which describes postoperative pseudoptosis with drooping of breast tissue below the inframammary fold secondary to the natural forces of gravity in the inferior pole and impaired skin integrity, resulting in a less aesthetic outcome.16,29
Our MPWP technique constitutes a variation and modification of the well-described medial and superomedial techniques that have been previously described by Hall-Findlay.24,30 When compared with breast reduction using FNG, use of the medial pedicle allows for preservation of blood flow to the NAC, preservation of nipple sensation, and possible breastfeeding potential. The majority of our patient population maintained full sensitivity to NAC after surgery. Light touch sensation was performed in the office, and patients reported subjective presence of sensation. Interestingly, some patients who reported hyposensitivity preoperatively reported hypersensitivity postoperatively. We did not observe complete loss of NAC and only two cases of partial loss. In both cases, nonoperative management led to successful healing.
Due to the length of the pedicle, even after the debulking process, this technique produces breast size no smaller than a C or D cup. If patients desired a smaller size, reduction with FNG was offered upfront. Although acceptance of larger breast size was required to preserve the nipple, the reductions were significant enough to provide marked symptomatic relief, and the resultant breast size was aesthetic and proportionate to patients’ body habitus, given the mean BMI was 40. This technique should be considered for patients with large reductions and long pedicles that may prove difficult with SMP reductions while still providing a full symmetric breast shape and intact nerve and blood supply. With such potential advantages, the medial pedicle should be considered as a standard approach for breast reduction surgery for macromastia, including gigantomastia.
LIMITATIONS
Limitations of this study include a limited sample size due to the rare prevalence of the condition. We plan to conduct further studies at our institution that include larger sample sizes to collect additional data on the safety and efficacy of the MPWP technique for reduction surgery in both patients with macromastia and the more challenging cases of gigantomastia.
CONCLUSIONS
The MPWP reduction technique is a viable option for the treatment of gigantomastia. Our facility’s retrospective analysis demonstrated the safety of the technique along with being able to preserve NAC sensation in these large reductions. These results are promising, but further research is warranted to determine patient satisfaction of this procedure with a larger sample of women with gigantomastia.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Mojallal A, Moutran M, Shipkov C, et al. Breast reduction in gigantomastia using the posterosuperior pedicle: an alternative technique, based on preservation of the anterior intercostal artery perforators. Plast Reconstr Surg. 2010;125:32–43. [DOI] [PubMed] [Google Scholar]
- 2.Singolda R, Bracha G, Zoabi T, et al. Superiomedial pedicle breast reduction for gigantic breast hypertrophy: experience in 341 breasts and suggested safety modifications. Aesthetic Plast Surg. 2021;45:375–385. [DOI] [PubMed] [Google Scholar]
- 3.Sak MC, Akin S, Ersen B, et al. Management of gigantomastia: outcomes of superomedial pedicle with vertical scar or wise pattern skin excision. World J Plast Surg. 2017;6:206–211. [PMC free article] [PubMed] [Google Scholar]
- 4.Dancey A, Khan M, Dawson J, et al. Gigantomastia—a classification and review of the literature. J Plast Reconstr Aesthet Surg. 2008;61:493–502. [DOI] [PubMed] [Google Scholar]
- 5.Karsidag S, Akcal A, Karsidag T, et al. Reduction mammaplasty using the free-nipple-graft vertical technique for severe breast hypertrophy: improved outcomes with the superior dermaglandular flap. Aesthetic Plast Surg. 2011;35:254–261. [DOI] [PubMed] [Google Scholar]
- 6.Costa MP, Ching AW, Ferreira MC. Thin superior medial pedicle reduction mammaplasty for severe mammary hypertrophy. Aesthetic Plast Surg. 2008;32:645–652. [DOI] [PubMed] [Google Scholar]
- 7.Landau AG, Hudson DA. Choosing the superomedial pedicle for reduction mammaplasty in gigantomastia. Plast Reconstr Surg. 2008;121:735–739. [DOI] [PubMed] [Google Scholar]
- 8.DeGeorge BR, Colen DL, Mericli AF, et al. Reduction mammoplasty operative techniques for improved outcomes in the treatment of gigantomastia. Eplasty. 2013;13:e54. [PMC free article] [PubMed] [Google Scholar]
- 9.Doren EL, Van Eldik Kuykendall L, Lopez JJ, et al. Free nipple grafting: an alternative for patients ineligible for nipple-sparing mastectomy? Ann Plast Surg. 2014;72:S112–S115. [DOI] [PubMed] [Google Scholar]
- 10.Davison SP, Mesbahi AN, Ducic I, et al. The versatility of the superomedial pedicle with various skin reduction patterns. Plast Reconstr Surg. 2007;120:1466–1476. [DOI] [PubMed] [Google Scholar]
- 11.Colen SR. Breast reduction with use of the free nipple graft technique. Aesthet Surg J. 2001;21:261–271. [DOI] [PubMed] [Google Scholar]
- 12.Restifo RJ, Lalikos JF. Amputation/free nipple graft reduction mammaplasty. Oper Tech Plast Reconstr Surg. 1996;3:184–188. [Google Scholar]
- 13.Oneal RM, Goldstein JA, Rohrich R, et al. Reduction mammoplasty with free-nipple transplantation: indications and technical refinements. Ann Plast Surg. 1991;26:117–121. [DOI] [PubMed] [Google Scholar]
- 14.Koger KE, Sunde D, Press BH, et al. Reduction mammaplasty for gigantomastia using inferiorly based pedicle and free nipple transplantation. Ann Plast Surg. 1994;33:561–564. [DOI] [PubMed] [Google Scholar]
- 15.Larsen A, Ørholt M, Hemmingsen MN, et al. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72:1219–1243. [DOI] [PubMed] [Google Scholar]
- 16.Wolter A, Fertsch S, Munder B, et al. Double-Unit superomedio-central (DUS) pedicle inverted-T reduction mammaplasty in gigantomastia: a 7-year single-center retrospective study. Aesthetic Plast Surg. 2021;45:2061–2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed OA, Kolhe PS. Comparison of nipple and areolar sensation after breast reduction by free nipple graft and inferior pedicle techniques. Br J Plast Surg. 2000;53:126–129. [DOI] [PubMed] [Google Scholar]
- 18.Rietjens M, De Lorenzi F, Andrea M, et al. Free nipple graft technique to correct nipple and areola malposition after breast procedures. Plast Reconstr Surg Glob Open. 2013;1:e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan RS, Gill NA. Inverted-T reduction mammoplasty with superomedial pedicle for gigantomastia - a case series. J Surg Res. 2021;4:478–483. [Google Scholar]
- 20.Amini P, Stasch T, Theodorou P, et al. Vertical reduction mammaplasty combined with a superomedial pedicle in gigantomastia. Ann Plast Surg. 2010;64:279–285. [DOI] [PubMed] [Google Scholar]
- 21.Ashour T, Khachaba Y, El Naggar A. Supero-medial reduction mammaplasty: a safe and reliable technique in gigantomastia and severe breast ptosis. Electron Physician. 2018;10:7230–7234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.MALINIAC JW. Arterial blood supply of the breast: revised anatomic data relating to reconstructive surgery. Arch Surg. 1943;47:329–343. [Google Scholar]
- 23.Palmer JH, Taylor GI. The vascular territories of the anterior chest wall. Br J Plast Surg. 1986;39:287–299. [DOI] [PubMed] [Google Scholar]
- 24.Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748–759; discussion 760–763. [PubMed] [Google Scholar]
- 25.Michelle le Roux C, Kiil BJ, Pan WR, et al. Preserving the neurovascular supply in the Hall-Findlay superomedial pedicle breast reduction: an anatomical study. J Plast Reconstr Aesthet Surg. 2010;63:655–662. [DOI] [PubMed] [Google Scholar]
- 26.Schlenz I, Kuzbari R, Gruber H, et al. The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg. 2000;105:905–909. [DOI] [PubMed] [Google Scholar]
- 27.Schlenz I, Rigel S, Schemper M, et al. Alteration of nipple and areola sensitivity by reduction mammaplasty: a prospective comparison of five techniques. Plast Reconstr Surg. 2005;115:743–751; discussion 752–754. [DOI] [PubMed] [Google Scholar]
- 28.Sapino G, Haselbach D, Watfa W, et al. Evaluation of long-term breast shape in inferior versus superomedial pedicle reduction mammoplasty: a comparative study. Gland Surg. 2021;10:1018–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baslaim MM, Al-Amoudi SA, Hafiz M, et al. The safety, cosmetic outcome, and patient satisfaction after inferior pedicle reduction mammaplasty for significant macromastia. Plast Reconstr Surg Glob Open. 2018;6:e1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136:531e–544e. [DOI] [PubMed] [Google Scholar]