Abstract
The COVID-19 pandemic, and the response of governments to mitigate the pandemic’s spread, resulted in exceptional circumstances that comprised a major global stressor, with broad implications for mental health. We aimed to delineate anxiety trajectories over three time-points in the first 6 months of the pandemic and identify baseline risk and resilience factors that predicted anxiety trajectories. Within weeks of the pandemic onset, we established a website (covid19resilience.org), and enrolled 1,362 participants (n=1064 from US; n=222 from Israel) who provided longitudinal data between April-September 2020. We used latent growth mixture modeling to identify anxiety trajectories and ran multivariate regression models to compare characteristics between trajectory classes. A four-class model best fit the data, including a resilient trajectory (stable low anxiety) the most common (n=961, 75.08%), and chronic anxiety (n=149, 11.64%), recovery (n=96, 7.50%) and delayed anxiety (n=74, 5.78%) trajectories. Resilient participants were older, not living alone, with higher income, more education, and reported fewer COVID-19 worries and better sleep quality. Higher resilience factors’ scores, specifically greater emotion regulation and lower conflict relationships, also uniquely distinguished the resilient trajectory. Results are consistent with the pre-pandemic resilience literature suggesting that most individuals show stable mental health in the face of stressful events. Findings can inform preventative interventions for improved mental health.
Keywords: Resilience, Risk, COVID-19, Anxiety, LGMM
1. Introduction
COVID-19 was declared a global pandemic by the World Health Organization on March 11th 2020 (Cucinotta & Vanelli, 2020). Early in the pandemic it imposed an exceptional array of stressors that demanded individual and social adaptation (Brooks et al., 2020). The initial stress, which reflected an immediate health threat to the population, was compounded by subsequent compulsory measures to control the spread of the virus, such as lockdowns, isolation, and social distancing, (Fancourt et al., 2021). The unexpected outbreak and course of the pandemic, along with the combination of sudden impositions then lifting of government restrictions impacted every aspects of life, making the pandemic a major stressor with pervasive implications for mental health (Bhattacharjee & Ghosh, 2022). Accordingly, the pandemic created a significant challenge to individuals to enact successful coping mechanisms, adjust to the situation, and preserve mental health homeostasis (Bonanno, 2004; Cheng et al., 2014).
Previous studies suggest that variability in reaction to stress or adversities can be captured by a relatively small set of prototypical response trajectories (Bonanno, 2004). First, resilience, the most common trajectory, is characterized by a stable trajectory of healthy functioning even following an acute stressor. Most individuals exhibit stable well-being after exposure to various forms of acute adversity (Mancini et al., 2011), including after outbreaks of high-risk infectious diseases (Bonanno et al., 2008; Bults et al., 2011; Leung et al., 2005). Second, a recovery trajectory is characterized by elevated mental health symptoms and a gradual return to normal levels of functioning. Resilience and recovery represent empirically discrete trajectories in response to widely varying acute stressors (Bonanno et al., 2011). However, context is important, and a recovery trajectory may also indicate resilience. That is, recovery to resilience follows on from the process of harnessing resources, getting back to well-being, and bouncing back in the face of adversity (Southwick et al., 2014). Indeed, research has documented significant improvements in mental health following stress exposure (Mancini, 2019; Mancini et al., 2011). One explanation for these improvements is that acute stress stimulates affiliative, cooperative, and trusting behaviors, that might improve social environments (Taylor, 2016; von Dawans et al., 2012; Fowler & Christakis, 2010). Third, a chronic distress trajectory is characterized by elevated symptoms that persist. Identification of a chronic distress trajectory makes it possible to distinguish difficulties specific to the stressful event from longer-term difficulties that precede the stressor. Finally, a delayed trajectory is characterized by moderate to elevated symptoms that worsen over time (Bonanno, 2004). Together, these patterns are thought to capture most of the variation in responses to acute stressors (Bonanno et al., 2012) and notably a recent review of 28 trajectory studies confirmed these heterogeneous patterns of response. Furthermore, the predominant response was resilience, with an estimated prevalence of 66.0% (Schäfer et al., 2022) consistent with pre-pandemic estimates of resilience to other stressors.
An especially relevant outcome in trajectory studies of COVID-19 is anxiety. Health concerns commonly evoke anxious responses (Abramowitz et al., 2007) and the COVID-19 pandemic represented a health threat of historic magnitude. Anxiety reactions to stress combine mostly future-oriented unpleasant emotions and cognitions, (Barlow, 2002), which involve physiological (e.g., hyperarousal, tension) and cognitive (e.g., preoccupation with worries, sense of lack of control) components (Butcher et al., 2017). Although anxious reactions can be adaptive in the face of threat, for some the inability to manage anxiety can undermine functioning and quality of life (Mertens et al., 2020). Early longitudinal studies conducted during the onset of the pandemic (March-May 2020) demonstrated an increase in stress responses, with elevated rates of anxiety and other manifestations of mental health symptoms (Robinson et al., 2022). Later reports suggested that anxiety symptoms subsequently declined, were small in magnitude, and may have even recovered to pre-pandemic levels (Fancourt et al., 2021). Moreover, a systematic review and meta-analysis of 64 longitudinal studies found that anxiety symptoms generally declined during the COVID-19 pandemic (Cénat et al., 2022).
Nevertheless, there are relatively few investigations of anxiety symptoms in the early pandemic, and a critical task of COVID-related science is to build a cumulative database on reactions to the pandemic. In one longitudinal cohort study of a representative sample of 1296 Australian adults during the first three months of the pandemic, most participants (77%) did not experience changes in mental health symptoms including anxiety symptoms (Batterham et al., 2021). Similarly, during the first 12 weeks of the United Kingdom’s initial national COVID-19 lockdown, two thirds of the sample self-reported anxious symptomology suggestive of considerable resilience to the unprecedented demands (McPherson et al., 2021). Although similar findings were replicated in various other countries, few studies were done among the adult American population (Schäfer et al., 2022), and to our knowledge, none were undertaken immediately after lockdowns were instituted in late March.
An additional critical task of research on anxiety trajectories is identifying the factors that contribute to more adverse reaction patterns during the acute phase of the pandemic when uncertainty, stress levels, and anxiety symptoms were most acute (H. Chen et al., 2021). Several risk factors have been identified for developing anxiety during the COVID-19 pandemic including demographic factors (e.g., female sex), preexisting anxiety diagnosis, sleep problems, fear of COVID-19 infection, and greater likelihood of getting infected (Fu et al., 2020; Malesza & Kaczmarek, 2021; Özdin & Bayrak Özdin, 2020; Lu et al., 2022). Less data exist on factors that promote resilient outcome. Several studies suggested that induvial-level characteristics such as emotion regulation (Gambin et al., 2021) and community-level factors like family support (McPherson et al. 2021) might contribute to resilient anxiety trajectory, but overall, there has been limited evidence on the role of specific resilience factors.
It is widely thought that factors that contribute to resilience are multidimensional (Cicchetti & Curtis, 2007; Luthar et al., 2000), and there is no single pathway to resilience (Bonanno, 2004). To assess a wide variety of potentially contributing factors, prior to the pandemic, we developed and tested a single battery that evaluates resilience factors. The resilience factors were previously clinically validated using commonly-used scales of mental health and function level (Moore et al., 2020; White et al., 2022). Our battery encompasses several resilience domains, including intrapersonal (self-reliance, emotion regulation), interpersonal (positive and negative aspects of close relationships) and broader social environmental contexts (perceptions of the neighborhood environment). In April 2020, we established a website (covid19resilience.org) and administered this battery along with measures of current mental health, including anxiety (Barzilay et al., 2020).
In the current study we examined longitudinal change in anxiety symptoms over three waves of data collection in the early pandemic from April to September 2020. We were particularly interested in whether distinct anxiety trajectories could be identified using growth mixture modeling techniques. We further sought to identify specific risk and resilience factors at baseline that contribute to inter-individual variation in anxiety trajectories. We expected that participants would belong to heterogeneous subpopulations that comprised distinct anxiety trajectories over time, with a resilient trajectory being the most prevalent (Leung et al., 2005; Mancini et al., 2011).
2. Methods
2.1. Participants and Procedures
On April 6th 2020, we launched a website (https://www.covid19resilience.org/) that hosted an online survey and included questionnaires assessing resilience factors, COVID-19 stressors and COVID-19 worries, as well as an anxiety-symptoms assessment (Barzilay et al., 2020). At the end of the survey, participants received feedback on their resilience scores with personalized recommendations for stress management. The feedback functioned to incentivize participants to complete the survey thoughtfully. Following the feedback, participants were asked if they were interested in being re-contacted for future surveys. The website was advertised through (a) researchers’ social networks, including emails to colleagues around the world, (b) social media, (c) The University of Pennsylvania and Children’s Hospital of Philadelphia internal notifications and websites, and (d) organizational mailing lists. All participants consented to participate in the study. The study was approved by the Institutional Review Board of the University of Pennsylvania.
Analyses included 1,362 participants above the age of 18 who completed the anxiety assessment in at least two out of three timepoints: T1, April 6th to May 10th; T2, May 12th to July 6th; and T3, August 25th to September 27th. Overall, 448 participants had T1 and T2 data only, 162 had T1 and T3 only, and 73 had T2 and T3 data only. A total of 679 participants, 49.8%, had complete data for all three timepoints, and 50.2% had data available for at least two timepoints. Participants could only complete the survey once because all longitudinal surveys were distributed via email with a personalized link that could only be used once.
2.2. Measures
Anxiety-symptoms assessment (T1, T2, and T3).
Participants completed the Generalized Anxiety Disorder 7 (GAD-7) questionnaire, a self-report screening device developed to assess the defining symptoms of anxiety (Spitzer et al. 2006). Items are rated on a 4-point Likert-type scale (0 = not at all to 3 = nearly every day) and scores ranged from 0 to 21 (T1, α=.89; T2, α=.92, T3, α=.92).
COVID-19-related worries (T1).
Participants indicated the degree to which they were worried about a variety of COVID-19 related outcomes on 5-point Likert scale (0 = not at all to 4 = a great deal). Worries included: 1) contracting COVID-19, 2) dying from COVID-19, 3) family members contracting COVID-19, 4) unknowingly infecting others with COVID-19, 5) currently having COVID-19, and 6) having significant financial burden because of the COVID-19 pandemic.
COVID-19 related stress exposures burden (T1).
Participants were asked to rate whether they had experienced each of the following COVID-19 stressors: (a) testing positive for COVID-19, (b) knowing someone who died from COVID-19, (c) job loss since the start of the COVID-19 pandemic, and (d) reduced pay since the start of the COVID-19 pandemic. For analysis, items ratings were recoded as either: (a) yes (1 = experienced), or (b) no (0 = did not experience). The 4 stressors then summed to create a cumulative COVID-19-related stress exposures burden measure.
Pre-existing anxiety diagnosis (T1).
Participants were asked whether they had received a diagnosis of generalized anxiety disorder prior to the COVID-19 pandemic (1 = yes, 0 = no).
Sleep measure (T1).
Participants completed the Insomnia Severity Index (ISI), a 7-item self-report scale developed to assess insomnia symptoms over the past two weeks. Items are rated on a 5-point Likert-type scale (0 = none to 4 = very severe) (Morin et al., 2011).
Self-reported resilience factors (T1).
Participants completed a validated 21-item scale that efficiently assesses resilience factors within a single battery (Barzilay et al., 2020; Gur et al., 2021, 2020; Kornfield et al., 2021) with five subscales: (a) self-reliance (3 items; e.g., can usually find a way out of difficult situations), with items coded on a 7-point Likert Scale (1 = strongly disagree to 7 = strongly agree), (b) emotion regulation (5 items; e.g., difficulty concentrating or controlling behaviors when upset, limited access to emotion regulation strategies), with items coded on a 5-point Likert Scale (1 = almost never [0–10%] to 5 = almost always [91–100%]), (c) positivity and support in close relationships (4 items; e.g., lasting relationship and level of care), with items coded on a 5-point Likert Scale (1 = little or none to 5 = the most), (d) negativity and hostility in close relationships (5 items; e.g., level of arguing), with items coded on a 5-point Likert Scale (1 = little or none to 5 = the most), and (e) perceptions of the neighborhood environment (4 items; e.g., perceived level of trust and safety in neighborhood), with items coded on an 5-point Likert Scale (1 = strongly disagree to 5 = strongly agree). To maximize interpretability, we coded all items such that a higher score indicated greater resilience.
2.3. Analytic Strategy
To address our first study aim, we applied latent growth mixture modeling (LGMM) to the anxiety scores at T1, T2, and T3 and compared model fit for solutions with one to five classes (Muthén, 2003; Nylund et al., 2007). All analyses were conducted in Mplus version 8 (Muthén & Muthén, 2017) using a robust full information maximum likelihood (FIML) estimation procedure for handling missing data which assumes missing data are unrelated to the outcome variable (i.e., missing at random) (Enders, 2001). We considered multiple criteria to evaluate model fit, including the Bayesian Information Criterion (BIC), Lo–Mendell–Rubin adjusted Likelihood Ratio Test, and entropy values (Muthén, 2003; Muthén, 2004; Nylund et al., 2007). We also evaluated the substantive meaning of class solutions relative to theoretical accounts and prior findings (Bonanno, 2012; Bonanno et al., 2011). We initially compared fit for unconditional models without covariates using conventional indices that penalize more complex models when they fail to provide a better fit to the data (Lo, 2001; Muthén, 2003; Nylund et al., 2007). However, consistent with recommendations, we then included covariates as predictors of class membership in conditional models. Covariates were age, sex, education, income, living alone, and living in the US. This step is recommended because non-significant relationships between covariates and class membership may indicate an incorrect local solution (Muthén, 2003).
We next compared baseline demographic factors, COVID-19 related stress exposures burden, and COVID-19 worries between the anxiety trajectory classes. We used univariate ANOVA to compare the derived trajectory groups on a variety of demographic factors (age, gender, race, income, education, living alone, and living in the US), and ran a multivariate analysis of covariance (MANCOVA) model controlling for these factors. We then used multinomial logistic regression models to test whether T1 COVID-19 related stress exposure burden (e.g., testing positive, knowing someone who died) and worries (e.g., worries about contracting, financial burden of the pandemic) predicted class membership controlling for demographic variables. Finally, we used multinomial logistic regression models to test whether T1 resilience factors (e.g., emotion regulation, harmony in close relationships) or risk (e.g., prior anxiety diagnosis of anxiety, sleep problems) factors predicted class membership, controlling for demographic factors. Note that as a sensitivity analysis, we repeated the LGMM analyses using just participants from the US.
3. Results
3.1. Identifying trajectories of anxiety
Descriptive statistics for study variables at T1, T2, and T3 are presented in Table 1. Bivariate correlations between study variables are presented in Supplemental Table S1. The fit statistics and theoretical interpretability for the unconditional and conditional models showed that a four-class conditional model provided the best fit (see Supplemental Table S2). Most participants (n = 961; 75.08%) showed stable low anxiety over time and a non-significant slope (resilient) (B = .23, SE = .47, p = .62). The next largest group (n = 149; 11.64%) displayed stable high anxiety over time (chronic) (B = .83, SE = .49, p = .09). A smaller group (n = 96; 7.50%) began with high levels of anxiety that decreased over time (recovered) (B = −5.03, SE = 1.13, p<.05). Finally, a small group of participants (n = 74; 5.78%) began with lower levels of anxiety that increased over time (delayed) (B = 6.33, SE = 1.24, p<.01; see Figure 1 and Supplemental Table S3 for details of the intercept and slope factors for each class). When the sample was restricted to US participants, a similar four-class solution also emerged (see Supplemental Tables S4 and S5), suggesting that the emergence of the four anxiety trajectories did not depend on the geographic location of participants.
Table 1.
Sample descriptive statistics (n=1362)
| % of Participants (n) | |
|---|---|
|
| |
| Sex | |
| Female | 82.5% (n=1123) |
| Male | 17.5% (n=238) |
| Missing | 0.1% (n=1) |
| Race | |
| White | 87.4% (n=1191) |
| Other | 10.6% (n=144) |
| Missing | 2.0% (n=27) |
| Ethnicity | |
| Hispanic | 3.9% (n=53) |
| Non-Hispanic | 91.3% (n=1244) |
| Missing | 4.8% (n=65) |
| Income | |
| < 100k | 46.9% (n=639) |
| ≥ $100k | 47.4% (n=645) |
| Missing | 5.7% (n=78) |
| Education | |
| Undergraduate Degree or Lower | 39.2% (n=534) |
| Master’s Degree or Higher | 60.6% (n=826) |
| Missing | 0.1% (n=2) |
| Living Arrangement | |
| Living Alone | 20.0% (n=272) |
| Living with Others | 80.0% (n=1089) |
| Missing | 0.1% (n=1) |
| Country of Residence | |
| USA | 78.1% (n=1064) |
| Israel | 16.3% (n=222) |
| Other Countries | 5.6% (n=76) |
| Missing | 0%% (n=0) |
| Past Diagnosis | |
| Anxiety | 24.5% (n=334) |
| Mean (SD) | |
| Age | |
| In years | 41.02 (13.67) |
| GAD-7 Scores | |
| Time 1 | 6.26 (4.84) |
| Time 2 | 6.12 (5.03) |
| Time 3 | 5.96 (5.02) |
Note. Sample consists of participants who completed the GAD-7 for at least two timepoints. GAD7 = Generalized Anxiety Disorder-7.
Figure 1.
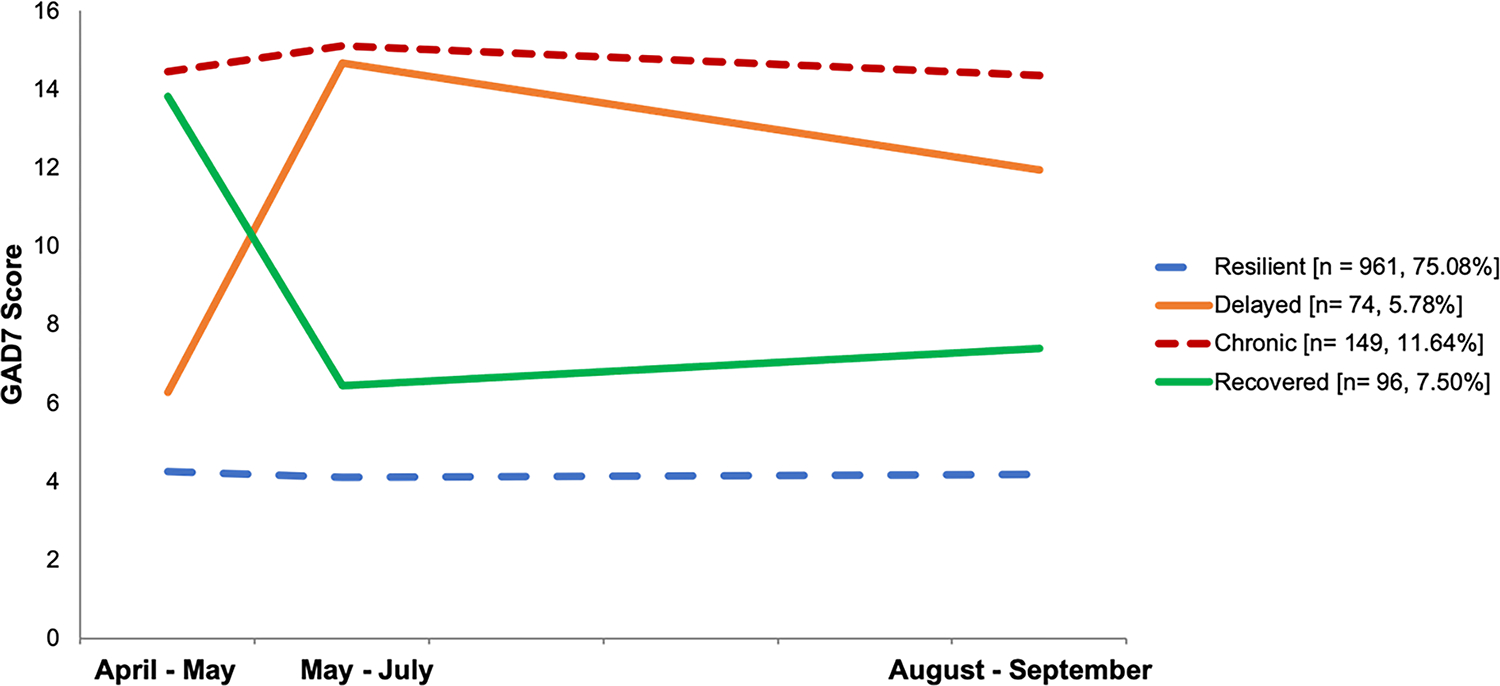
Mean Anxiety Scores Across the Study Period for the Four Anxiety Trajectory Groups
Note. Anxiety was assessed using the GAD-7. Covariates were included on the intercept and slope factors and as predictors of class membership. Covariates included participant age, sex, education (0 = less than a Master’s degree; 1= Master’s degree or higher), income, living alone, and living in the US. All models were run in Mplus version 8. Model results remained unchanged when the sample was restricted to just the US participants.
To address the possibility that missingness in the outcome (i.e., 50.2% of the participants had two data points only) was systematically linked with the trajectory class membership, we compared trajectory memberships of participant with missing data (n=683) to those who had data in all three assessment waves (n=679). We found no evidence that missingness was related to trajectory class (χ2=.20, df=3, p=.98). That is, the percent of participants in each trajectory class was similar between the groups (e.g., 75.1% vs. 75.0% of the sample were in the resilient trajectory for participants with missing vs. full data, respectively).
3.2. Demographic characteristics of participants within trajectories
Univariate ANOVA revealed that resilient participants were more likely to be older, male, non-Hispanic, more educated, and less likely to live in the United States relative to the other trajectory groups (Table 2).
Table 2.
Descriptive Statistics and Comparisons of the Anxiety Trajectory Groups, Odd Ratios and Confidence Intervals [95% CI] for Multinominal Logistic Regression. Cumulative COVID-19 stressors and Worries at T1 Differentiation among Trajectory Classes Membership
| Variable | Resilient n = 961 | Delayed n = 74 | Chronic n = 149 | Recovered n = 96 | Omnibus Test | Pairwise Comparisons |
|---|---|---|---|---|---|---|
|
| ||||||
| Age (years) | 41.87 (13.67) | 41.19 (14.50) | 37.44 (12.22) | 36.89 (10.36) | F = 7.94*** | 1 > 3** & 4** |
| Female | 78.7%, n = 756 | 86.5%, n = 64 | 95.3%, n = 142 | 92.7%, n = 89 | χ2 = 41.07*** | 1 < 3*** & 4**; 2 < 3* |
| White | 90.7%, n = 872 | 83.8%, n = 62 | 89.3%, n = 133 | 91.7%, n = 88 | χ2 = 3.69 | ns |
| Hispanic | 3.1%, n = 30 | 1.4%, n = 1 | 8.1%, n = 12 | 4.2%, n = 4 | χ2 = 8.21* | 1 < 3** |
| Income below 100k | 47.6%, n = 458 | 51.3%, n = 38 | 54.3%, n = 81 | 60.4%, n = 58 | χ2 = 7.42 | 1 < 4* |
| Master’s Degree or Higher | 63.4%, n = 609 | 68.9%, n = 51 | 49%, n = 73 | 64.6%, n = 62 | χ2 = 12.95** | 3 < 1**, 2**, & 4* |
| Living Alone | 18.1%, n = 787 | 25.7%, n = 55 | 19.5%, n = 120 | 39.6%, n = 58 | χ2 = 22.87*** | 4 > 1*** & 3** |
| Living in United States | 76.0%, n = 730 | 86.5%, n = 64 | 90.6%, n = 135 | 81.3%, n = 78 | χ2 = 22.65*** | 1 < 2* & 3***; 4 < 3* |
| Anxiety at Time 1 | 4.25 (2.79) | 6.28 (2.76) | 14.44 (3.91) | 13.81 (2.87) | F = 755.83*** | 1 < 2***, 3***, & 4***; 2 < 3*** & 4*** |
| Anxiety at Time 2 | 4.11 (2.95) | 14.68 (2.98) | 15.11 (3.37) | 6.44 (2.55) | F = 704.31*** | 1 < 2***, 3***, & 4***; 4 < 2*** & 3*** |
| Anxiety at Time 3 | 4.18 (3.37) | 11.94 (4.71) | 14.36 (3.95) | 7.40 (3.83) | F = 282.80*** | 1 < 2***, 3***, & 4***; 4 < 2*** & 3***; 2< 3** |
Note.
p < .05
p < .01
p < .001.
Standard deviations are in parentheses. For ANOVA models, a Bonferroni correction for multiple comparisons was applied. DF = 3.
3.3. Prospective predictors of anxiety trajectories
3.3.1. COVID-19 related stress exposures burden.
Multinomial logistic regression models that controlled for demographic factors (i.e., age, sex, education, income, living alone, and living in the US) revealed no significant differences between the trajectory classes based on COVID-19 related stress exposure burden at baseline. However, compared to the resilient group, participants in both the chronic and recovered trajectories experienced significantly higher COVID-19 worries at T1 – specifically about contracting/family contracting COVID-19 and the financial burden of the pandemic. In addition, recovered participants experienced significantly higher worry about family contracting the virus and the financial burden of the pandemic relative to resilient participants. Finally, the chronic trajectory participants reported significantly higher worry about the financial burden of the pandemic compared to the recovered trajectory participants (Table 3). Similar findings emerged when comparing COVID-19-related stress exposures burden and COVID-19 related worries assessed at T2 and T3 (see Supplemental Tables S6 and S7).
Table 3.
Odd Ratios and Confidence Intervals [95% CI] for Multinomial Logistic Regressions Predicting Anxiety Trajectory from Cumulative COVID Exposures and Worries, Risk Factors and Individual Resilience
| Predictor Variable | Resilient vs. Delayed | Resilient vs. Chronic | Resilient vs. Recovered | Delayed vs. Chronic | Delayed vs. Recovered | Chronic vs. Recovered |
|---|---|---|---|---|---|---|
|
| ||||||
| Covid Exposures | ||||||
| Cumulative Exposures | 1.25 [.67–2.32] | 1.11 [.68–1.81] | 1.31 [.76–2.24] | .89 [.43–1.84] | 1.05 [.49–2.27] | 1.18 [.62–2.26] |
| Covid Worries | ||||||
| Self-contracting | 1.22 [.93–1.61] | 1.42* [1.04–1.81] | 1.37 [1.04–1.79] | 1.17 [.83–1.63] | 1.12 [.78–1.60] | .96 [.69–1.34] |
| Family contracting | 1.25 [.96–1.63] | 1.51* [1.15–1.97] | 1.57** [1.21–2.04] | 1.20 [.85–1.70] | 1.25 [.89–1.77] | 1.04 [.74–1.47] |
| Financial burden | 1.36** [1.12–1.66] | 1.59*** [1.35–1.88] | 1.26* [1.04–1.52] | 1.17 [.93–1.48] | .92 [.72–1.19] | .79* [.63–.98] |
|
| ||||||
| Risk Factors | ||||||
| Past Diagnosis of Anxiety | 1.6 [.89–2.88] | 2.08* [1.30–3.33] | .73 [.41–1.31] | 1.3 [.67–2.50] | .46** [.22–.96] | .35*** [.19–.67] |
| Perceived Health | 1.13 [.83–1.54] | .92 [.72–1.18] | 1.04 [.76–1.43] | .81 [.57–1.16] | .92 [.61–1.39] | 1.13 [.80–1.61] |
| Sleep | 1.13*** [1.08–1.18] | 1.20*** [1.14–1.25] | 1.18*** [1.12–1.24] | 1.06* [1.00–1.11] | 1.04 [.99–1.10] | .99 [.94–1.04] |
|
| ||||||
| Resilience Factor | ||||||
| Emotion Regulation | .91* [.85–99] | .85*** [.79–.90] | .85*** [.80–.90] | .92 [.85–1.01] | .92 [.85–1.01] | 1.00 [.93–1.07] |
| Self-Reliance | 1.06 [.91–1.22] | .99 [.92–1.08] | 1.03 [.94–1.14] | .94 [.81–1.10] | .98 [.83–1.15] | 1.04 [.93–1.160] |
| Positivity and Support in Close Relationships | .98 [.89–1.07] | .94 [.87–1.01] | .97 [.89–1.05] | .96 [.86–1.07] | .99 [.88–1.11] | 1.03 [.94–1.13] |
| Negativity and Hostility in Close Relationships | .95 [.86–1.05] | .92* [.85–.99] | .97 [.89–1.05] | .97 [.86–1.09] | 1.02 [.90–1.16] | 1.06 [.96–1.16] |
| Neighborhood Environment | .96 [.90–1.04] | .96 [.91–1.02] | 1.07 [.996–1.14] | 1.00 [.92–1.09] | 1.11* [1.01–1.21] | 1.11* [1.03–1.20] |
Note. A total of three models were run with the resilient, delayed, or chronic group as the reference group respectively to allow for all possible group comparisons. The model controlled for the following covariates: participant age, sex, race (White= 1, Non-White= 0), Ethnicity (Hispanic=1, not Hispanic= 0), Educational Attainment, Income, and Whether the Participant is living alone and living in the US.
p < .05
p < .01
p < .001
3.3.2. Mental-health risk factors.
Multinomial logistic regression models revealed that resilient participants reported significantly fewer sleep problems at baseline relative to all other trajectories. Likewise, the delayed anxiety participants reported fewer sleep problems than the chronic anxiety participants. Participants in the resilient trajectory were significantly less likely to report having a prior (i.e., pre-COVID-19) anxiety disorder diagnosis compared to those in the chronic trajectory. Similarly, recovered participants were significantly less likely to have a prior anxiety disorder diagnosis compared to the delayed participants (Table 3 and Figure 2)
Figure 2.
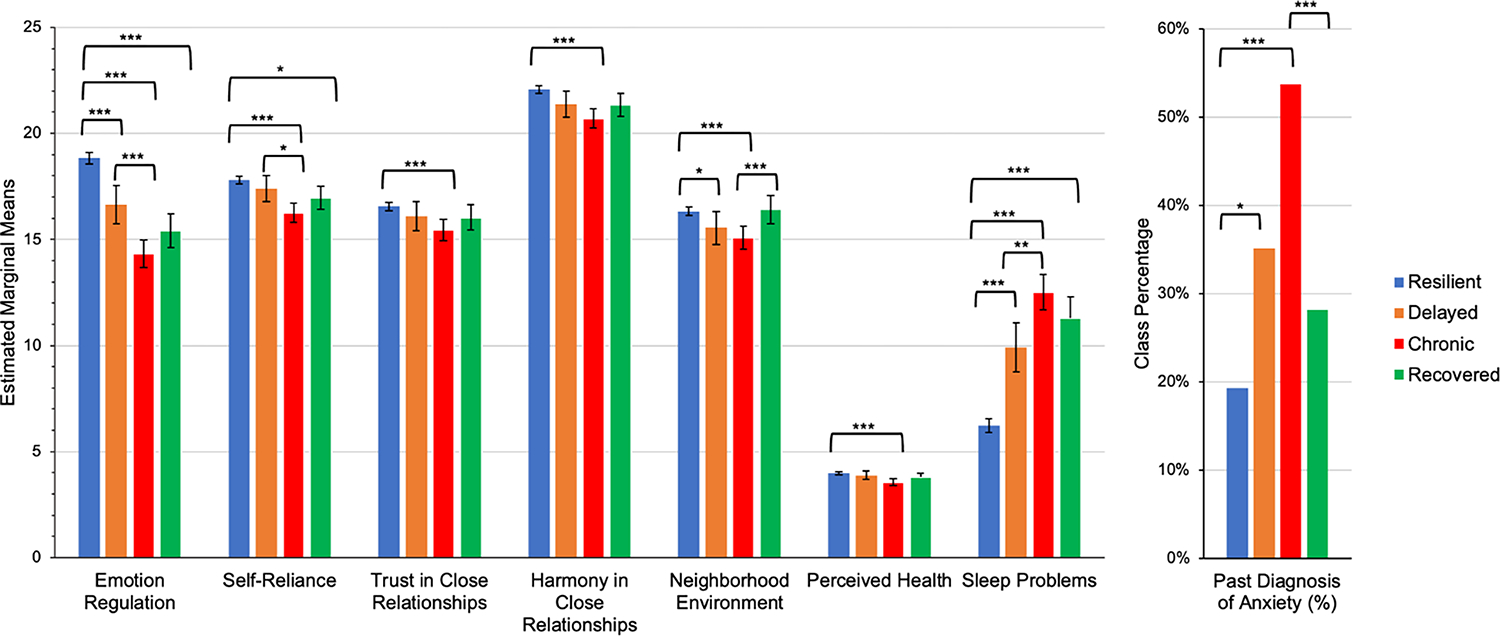
Estimated marginal mean scores and class percentages for the resilient, delayed, chronic, and recovered anxiety trajectory groups on measures of resilience and risk at Time 1
Note. Error bars represent 95% CI. Significant effects were robust after applying a Bonferroni correction for multiple comparisons in SPSS vs. 26. Means were derived from a MANCOVA to aid interpretability. Results were similar when using the Multinomial Logistic Regressions and MANCOVA approach. See the Supplemental Table S8 for full model MANCOVA statistics.
*p < .05, **p < .01, ***p < .00
3.3.3. Resilience factors.
Multinomial logistic regression models that controlled for demographic factors revealed that the resilient trajectory participants showed significantly greater emotion regulation relative to all other trajectories. In addition, resilient participants reported significantly lower hostility in close relationships relative to the chronic trajectory. Recovered participants reported significantly higher levels of positive neighborhood environment relative to delayed and chronic trajectories participants (Table 3 and Figure 2).
4. Discussion
In this cohort study, we identified distinct anxiety trajectories across the first months of the COVID-19 pandemic and identified risk and protective predictors of anxiety trajectory membership. A major strength of our analysis is the use of prospective data that allowed us to map anxiety trajectories over the first months of the pandemic when uncertainty and threat regarding lockdowns and SARs-Cov-2 were most acute. This timing of longitudinal data collection enabled the (1) investigation of anxiety symptom trajectories in a resilience framework (operationalized as low symptoms in the face of the pandemic) and (2) identification of prospective predictors in April 2020 of anxiety trajectories over the first months of the pandemic. The trajectory patterns that emerged are consistent with theoretical expectations, revealing four distinct patterns of response to the initial stress imposed by the pandemic (Bonanno, 2004; Mancini et al., 2011).
The most prevalent response (75%) was a resilient trajectory manifested with low stable anxiety-symptoms. Our findings are consistent with pre-COVID-19 studies that have documented the resilient trajectory as the most common pattern in response to a wide variety of stressors, including bereavement (Mancini et al., 2011), traumatic injury (deRoon-Cassini et al., 2010), combat (Maguen et al., 2020) and school shootings (Mancini et al., 2016). In reference to other COVID-19 related research, our results are consistent with two cohort studies from Australia (N = 1,296) and Canada (N = 373) that assessed participants longitudinally during 2020, demonstrating similar anxiety trajectory patterns, including a resilient pattern characterizing 77% of the Australian sample (Batterham et al., 2021) and 66% of the Canadian sample (Dufour et al., 2021). They are also consistent with a meta-analysis of longitudinal studies on the psychological impact of COVID-19 pandemic lockdowns (Prati & Mancini, 2021). As we discuss below, widely varying risk and resilience factors were associated with these trajectories (Malesza & Kaczmarek, 2021).
Notably, demographic characteristics differed considerably among participants in the different anxiety trajectory classes. In line with studies that have investigated response to the current pandemic (Filgueiras & Stults-Kolehmainen, 2021; Sherman et al., 2020) and as documented in previous research on resilience (Bonanno et al., 2015), a number of contextual variables were significantly associated with resilient or recovering trajectories, including older age, male gender, and greater level of education. Indeed, men generally report lower levels of psychological distress and overall have lower GAD-7 anxiety scores compared with women (Löwe et al., 2008). It is possible that in the context of the first months of the pandemic, the gender difference we observed could be partly attributed to the increased burden around childcare during school closures, which is known to have disproportionally affected working mothers (Power, 2020). Likewise, women were more likely to lose their jobs or to take unpaid leaves of absence to care for children, contributing to a more pronounced stress burden and increasing the mental health burden (Johnston et al., 2020). Findings regarding the more resilient trajectory of older adults may reflect their tendency to develop strengths through a lifetime of experiences, or their ability to negotiate life challenges better than younger adults (Charles, 2010).
We found that participants in the chronic anxiety trajectory reported significantly more worries related to COVID-19 early in the course of the pandemic, notably in relation to financial burdens, as well as concerns for self and others contracting the virus, and suffered from poorer sleep quality, replicating prior findings in a study of German participants (Gilan et al. 2020). Sleep represents a neurobiological balance between arousal and de-arousal and considered as a basic dimension for brain function and mental health (Harvey et al., 2011). Sleep quality was previously found to mediate the association between COVID-related stressors and mental health outcomes in a large community samples of adults from the United States and Israel during the first months of the pandemic, highlighting the central role that sleep plays in promoting resilience in the face of stress during COVID-19 pandemic (Coiro et al., 2021; Lenzo et al., 2022), as well as life stressors more broadly (Liu et al., 2016; Palagini et al., 2018). Finally, we found that more than 50% of participants in the chronic anxiety group reported a past diagnosis of anxiety. This finding is consistent with prior studies suggesting that the negative effects of the COVID-19 pandemic appear more pronounced among vulnerable populations (Pan et al., 2021).
In terms of resilience factors, we found that emotion regulation was significantly higher among participants in the resilient trajectory compared to other anxiety trajectories. Notably, emotion regulation scores significantly differed between participants in the resilient trajectory and those in the delayed anxiety trajectory, suggesting that this capacity may be important to sustain low anxiety-symptoms levels throughout longitudinal exposure to the pandemic related stress (i.e., 5-months of this study period). Broadly defined, emotion regulation includes the ability to identify and accept emotional experiences, control impulsive behaviors when distressed, and flexibly modulate emotional responses as situationally appropriate (Renna et al., 2017). Low levels of emotion regulation have previously been linked to risk for anxiety and depression (Chen & Bonanno 2021), as well as externalizing problems (Cappadocia et al., 2009; Mitchell et al., 2012). Hence, low levels of emotion regulation are not merely a signal for anxiety, but represent instead, a transdiagnostic risk marker of psychopathology more broadly (Aldao et al., 2010; Beauchaine & Thayer, 2015). In contrast, high levels of emotion regulation, biologically indexed by prefrontal inhibition, represents a key mechanism in psychological health and is vital for adaptive functioning (Aldao et al., 2010; Gross, 2007). Our findings support prior studies suggesting that individual differences in emotion regulation prospectively predict early COVID-19 related acute stress (Tyra et al., 2021) and advances the existing literature by providing much needed longitudinal data on the relationship between anxiety and emotion regulation, especially during the pandemic (Schneider et al., 2021). These findings can help to illuminate what drives variability in mental health trajectories following the pandemic’s onset (Mancini, 2020). From a translational perspective, we suggest that interventions aimed at enhancing emotion regulation might be especially warranted as a modality to enhance resilience not only in the context of the pandemic (Lee et al., 2020; Renna et al., 2020), but also as we move beyond COVID-19 with interventions aimed at enhancing resilience in a tailored manner way following adversities (Liu et al., 2016; Palagini et al., 2018).
A second resilience factor that differentiated between the chronic and resilient groups was minimal hostility experienced in close relationships. This finding may be indicative of the different interpersonal challenges facing individuals during the pandemic, with people spending many weeks under lockdown with close others, for better or worse (Gadermann et al., 2021). That is, close relationships could have served to enhance an individual’s ability to deal with the demands, stress and concerns related to the pandemic (Donato et al., 2021) or may simply have exacerbated existing interpersonal hostility, further contributing to negative mental health trajectories (Prime et al., 2020). Finally, we found that a more positive neighborhood environment, a resilience factor reflecting feelings of personal safety and community cohesion (Mujahid et al., 2007), was significantly higher among participants of the recovered anxiety trajectory compared to participants in the delayed and chronic anxiety trajectories. This finding highlights the importance of social cohesion and community support in mitigating negative effects of the pandemic (Fone et al., 2014). Indeed, community resilience may be supported by the enhanced availability of social support after shared stressors (Mancini et al., 2021) and both individual and community aspects of resilience are thought to enhance our ability to cope with external demands and threats (Kimhi et al., 2020; Ungar & Theron, 2020).
The current study leveraged a large sample with prospective longitudinal data collected over three timepoints at a critical period of the pandemic. Still, our findings should be considered alongside several limitations. First, we used an on-line “snow-ball” recruitment method, which reduced the representativeness of our sample and the generalizability of the findings. Specifically, people who complete online surveys differ from people who do not, and thus the proportions of people in each trajectory should not be taken as population-level estimates (Pierce et al., 2020). Second, just under half of our sample had missing outcome data on one timepoint for the anxiety measure. Although we used recommended FIML procedures to handle missing data, it is possible that this missing data influenced the resulting trajectories. However, in post-hoc tests, we found no evidence that trajectory class membership differed between participants with versus without missing data. Third, our cohort included participants from the US and Israel, countries characterized by considerable differences in virus spread, government restrictions, and health care. Indeed, living in Israel predicted membership in the resilient group. Notably, however, at time T1 data collection, the restrictions on residents were similar in both Israel and the US. Moreover, a recent study in the US, the United Kingdom, and Israel similarly found that Israeli participants exhibited lower levels of general anxiety compared to others (Bareket-Bojmel et al., 2020), which might reflect cultural differences in expressing anxiety symptoms. Importantly, the trajectory patterns were largely robust to these differences, and similar findings emerged when the sample was restricted to only the US participants. Fourth, we refer to resilience outcomes based on low-recovering anxiety symptom levels, determined based on the measures we collected, which did not allow us to evaluate other resilient outcomes, such as post traumatic growth. Lastly, the measure we used for anxiety was a screening measure (GAD-7), and not a detailed clinical evaluation of anxiety, hence we do not have data on specific anxiety domains which are likely social anxiety that may have been heightened due to the pandemic’s imposed social isolation. Nonetheless, GAD-7 is highly validated as a screening tool for general anxiety and has been extensively used to monitor mental health during the pandemic (Cénat et al., 2022).
5. Conclusion
In sum, we found distinct patterns of anxiety trajectories in response to the first months of the COVID-19 pandemic. Several risk and resilience factors assessed prospectively contributed to these trajectories. In terms of risk, we replicate finding on risk factors such as female sex, younger age, preexisting anxiety, excessive worrying, and sleep problems as predictors of anxiety trajectory. In terms of resilience factors, our findings suggest that emotion regulation, low hostility in close relationships and neighborhood environment can help predict longitudinal resilient outcomes in response to a major stressor. Given that resilience factors prospectively contributed to the resilient anxiety symptoms trajectory, our findings highlight resilience mechanisms as future targets for intervention that can help to reduce the mental health burden following major stressors.
Supplementary Material
Acknowledgements
We thank participants of covid19resilience.org for their contribution to data generation.
Financial support
This work was supported by NIH grant K23MH-120437, R01MH-117014, the Binational Science Foundation (BSF, grant 2017369) and the Lifespan Brain Institute of Children’s Hospital of Philadelphia and Penn Medicine, University of Pennsylvania to RB. RW was support by institutional funding from the University of Pennsylvania. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest
Dr. Barzilay serves on the scientific board and reports stock ownership in ‘Taliaz Health’, with no conflict of interest relevant to this work. All other authors declare no potential conflict of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.”
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Abramowitz JS, Olatunji BO, & Deacon BJ (2007). Health anxiety, hypochondriasis, and the anxiety disorders. Behavior Therapy, 38(1), 86–94. 10.1016/J.BETH.2006.05.001 [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Bareket-Bojmel L, Shahar G, & Margalit M (2020). COVID-19-related economic anxiety is as high as health anxiety: Findings from the USA, the UK, and Israel. International Journal of Cognitive Therapy, 1–9. 10.1007/s41811-020-00078-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH (2002). Biological aspects of anxiety and panic. Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic, 180–219. [Google Scholar]
- Barzilay R, Moore TM, Greenberg DM, DiDomenico GE, Brown LA, White LK., Gur RC. & Gur RE. (2020). Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Translational Psychiatry, 10(1). 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham PJ, Calear AL, McCallum SM, Morse AR, Banfield M, Farrer LM, Gulliver A, Cherbuin N, Rodney Harris RM, Shou Y, & Dawel A (2021). Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. The Medical Journal of Australia, 214(10), 462–468. 10.5694/MJA2.51043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, & Thayer JF (2015). Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology, 98(2), 338–350. 10.1016/j.ijpsycho.2015.08.004 [DOI] [PubMed] [Google Scholar]
- Bhattacharjee A, & Ghosh T (2022). COVID-19 Pandemic and stress: coping with the new normal. Journal of Prevention and Health Promotion, 3(1), 30. 10.1177/26320770211050058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59, 20–28. 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- Bonanno GA (2012). Uses and abuses of the resilience construct: Loss, trauma, and health-related adversities. Social Science and Medicine, 74, 753–756. 10.1016/j.socscimed.2011.11.022 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Ho SMY, Chan JCK, Kwong RSY, Cheung CKY, Wong CPY, & Wong VCW (2008). Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology, 27(5), 659–667. 10.1037/0278-6133.27.5.659 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Romero SA, & Klein SI (2015). The temporal elements of psychological resilience: An integrative framework for the study of individuals, families, and communities. Psychological Inquiry, 26(2), 139–169. 10.1080/1047840X.2015.992677 [DOI] [Google Scholar]
- Bonanno GA, Westphal M, & Mancini AD (2011). Resilience to loss and potential trauma. Annual Review of Clinical Psychology, 7, 511–535. 10.1146/annurev-clinpsy-032210-104526 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Westphal M, & Mancini AD (2012). Loss, trauma, and resilience in adulthood. Annual Review of Gerontology and Geriatrics, 32(1), 189–210. https://www.academia.edu/19173032/Chapter_10_BR_Loss_Trauma_and_Resilience_in_Adulthood [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bults M, Beaujean DJMA, De Zwart O, Kok G, Van Empelen P, Van Steenbergen JE, Richardus JH, & Voeten HACM (2011). Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health, 11. 10.1186/1471-2458-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappadocia MC, Desrocher M, Pepler D, & Schroeder JH (2009). Contextualizing the neurobiology of conduct disorder in an emotion dysregulation framework. Clinical Psychology Review, 29, 506–518. 10.1016/j.cpr.2009.06.001 [DOI] [PubMed] [Google Scholar]
- Cénat JM, Farahi SMMM, Dalexis RD, Darius WP, Bekarkhanechi FM, Poisson H, Broussard C, Ukwu G, Auguste E, Nguyen DD, Sehabi G, Furyk SE, Gedeon AP, Onesi O, El Aouame AM, Khodabocus SN, Shah MS, & Labelle PR (2022). The global evolution of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis of longitudinal studies. Journal of Affective Disorders, 315, 70–95. 10.1016/J.JAD.2022.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST (2010). Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin, 136(6), 1068–1091. 10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Gao J, Dai J, Mao Y, Wang Y, Chen S, Xiao Q, Jia Y, Zheng P, & Fu H (2021). Generalized anxiety disorder and resilience during the COVID-19 pandemic: Evidence from China during the early rapid outbreak. BMC Public Health, 21(1). 10.1186/S12889-021-11877-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, & Bonanno GA (2021). Components of emotion regulation flexibility: Linking latent profiles to depressive and anxious symptoms. Clinical Psychological Science, 9 (2), 236–251. 10.1177/2167702620956972 [DOI] [Google Scholar]
- Cheng C, Lau H. P. B.ob ., & Chan MPS. all. (2014). Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychological Bulletin, 140(6), 1582–1607. 10.1037/a0037913 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Curtis WJ (2007). Multilevel perspectives on pathways to resilient functioning. Development and Psychopathology, 19, 627–629. 10.1017/S095457940700031 [DOI] [PubMed] [Google Scholar]
- Coiro MJ, Asraf K, Tzischinsky O, Hadar-Shoval D, Tannous-Haddad L, & Wolfson AR (2021). Sleep quality and COVID-19-related stress in relation to mental health symptoms among Israeli and U.S. adults. Sleep Health, 7(2). 10.1016/j.sleh.2021.02.006 [DOI] [PubMed] [Google Scholar]
- Cucinotta D, & Vanelli M (2020). WHO declares COVID-19 a pandemic. Acta Bio-Medica : Atenei Parmensis, 91(1), 157–160. 10.23750/ABM.V91I1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- deRoon-Cassini TA, Mancini AD, Rusch MD, & Bonanno GA (2010). Psychopathology and resilience following traumatic injury: A latent growth mixture model analysis. Rehabilitation Psychology, 55(1), 1–11. 10.1037/a0018601 [DOI] [PubMed] [Google Scholar]
- Donato S, Parise M, Pagani AF, Lanz M, Regalia C, Rosnati R, & Iafrate R (2021). Together against COVID-19 concerns: The role of the dyadic coping process for partners’ psychological well-being during the pandemic. Frontiers in Psychology, 11. 10.3389/fpsyg.2020.578395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufour MM, Bergeron N, Rabasa A, Guay S, & Geoffrion S (2021). Assessment of psychological distress in health-care workers during and after the first wave of COVID-19: A Canadian longitudinal study. Canadian Journal of Psychiatry, 66(9), 807–814. 10.1177/07067437211025217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK (2001). The performance of the full information maximum likelihood estimator in multiple regression models with missing data. Educational and Psychological Measurement, 61, 713–740 10.1177/0013164401615001 [DOI] [Google Scholar]
- Fancourt D, Steptoe A, & Bu F (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet. Psychiatry, 8(2), 141–149. 10.1016/S2215-0366(20)30482-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filgueiras A, & Stults-Kolehmainen M (2021). Risk factors for potential mental illness among Brazilians in quarantine due to COVID-19. Psychol Rep. 33294120976628. doi: 10.1177/0033294120976628. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fone D, White J, Farewell D, Kelly M, John G, Lloyd K, Williams G, & Dunstan F (2014). Effect of neighbourhood deprivation and social cohesion on mental health inequality: A multilevel population-based longitudinal study. Psychological Medicine, 44(11), 2449–2460. 10.1017/S0033291713003255 [DOI] [PubMed] [Google Scholar]
- Fu W, Wang C, Zou L, Guo Y, Lu Z, Yan S, & Mao J (2020). Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational Psychiatry 2020 10:1, 10(1), 1–9. 10.1038/s41398-020-00913-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadermann AC, Thomson KC, Richardson CG, Gagné M, Mcauliffe C, Hirani S, & Jenkins E (2021). Examining the impacts of the COVID-19 pandemic on family mental health in Canada: Findings from a national cross-sectional study. BMJ Open, 11(1). 10.1136/bmjopen-2020-042871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambin M, Oleksy T, Sȩkowski M, Wnuk A, Woźniak-Prus M, Kmita, Holas., Pisula E., Łojek E., Hansen K, Gorgol J., Kubicka K., Huflejt-ŁUkasik M., Cudo A., Łyś A., Szczepaniak A., & Bonanno GA. (2021). Pandemic trajectories of depressive and anxiety symptoms and their predictors: Five-wave study during the COVID-19 pandemic in Poland. Psychological Medicine. 10.1017/S0033291721005420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilan D, Blessin M, Kunzler A, Stoffers-Winterling J, Müssig M, Yuen KSL, Tüscher O, Lieb K, Röthke N, Thrul J, Kreuter F, Sprengholz P, Betsch C, & Stieglitz RD (2020). Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2-pandemic’a systematic literature review and results from the German COSMO-PANEL. Deutsches Arzteblatt International, 117(28), 625–632. 10.3238/arztebl.2020.0625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. (Ed. . (2007). Handbook of emotion regulation. In The Guilford Press. New York, NY, US: The Guilford Press. https://psycnet.apa.org/record/2007-01392-000 [Google Scholar]
- Gur RE, White LK, Shani S, Barzilay R, Moore TM, Emanuel BS, Zackai EH, McDonald-McGinn DM, Matalon N, Weinberger R, Gur RC, & Gothelf D (2021). A binational study assessing risk and resilience factors in 22q11.2 deletion syndrome. Journal of Psychiatric Research, 138, 319–325. 10.1016/J.JPSYCHIRES.2021.03.058 [DOI] [PubMed] [Google Scholar]
- Gur RE, White LK, Waller R, Barzilay R, Moore TM., Kornfield S., Njoroge WFM., Duncan AF., Chaiyachati BH., Parish-Morris J., Maayan L, Himes MM., Laney N., Simonette K., Riis V. & Elovitz MA. (2020). The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Research, 293, 113475. 10.1016/J.PSYCHRES.2020.113475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandler RA, & Soehner A (2011). Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review, 31(2), 225–235. . 10.1016/j.cpr.2010.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston RM, Mohammed A, & Van Der Linden C (2020). Evidence of exacerbated gender inequality in child care obligations in Canada and Australia during the COVID-19 pandemic. Politics & Gender, 16(4), 1131–1141. 10.1017/S1743923X20000574 [DOI] [Google Scholar]
- Kimhi S, Marciano H, Eshel Y, & Adini B (2020). Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Social Science and Medicine, 265, 113389. 10.1016/j.socscimed.2020.113389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield SL, White LK, Waller R, Njoroge W, Barzilay R, Chaiyachati BH, Himes MM, Rodriguez Y, Riis V, Simonette K, Elovitz MA & Gur RE (2021). Risk and resilience factors influencing postpartum depression and mother-infant bonding during COVID-19. Health Affairs, 40(10), 1566–1574. 10.1377/HLTHAFF.2021.00803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EE, Bangen KJ, Avanzino JA, Hou B, Ramsey M, Eglit G, Liu J, Tu XM, Paulus M & Jeste DV (2020). Outcomes of randomized clinical trials of interventions to enhance social, emotional, and spiritual components of wisdom: A systematic review and meta-analysis. JAMA Psychiatry, 77(9), 925–935. 10.1001/jamapsychiatry.2020.0821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzo V, Sardella A, Musetti A, Freda MF, Lemmo D, Vegni E, Borghi L, Plazzi G, Palagini L, Castelnuovo G, Cattivelli R, Mariani R, Michelini G, Manari T, Saita E, Quattropani MC, & Franceschini C (2022). The relationship between resilience and sleep quality during the second wave of the COVID-19 pandemic: A longitudinal study. Nature and Science of Sleep, 14, 41. 10.2147/NSS.S344042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung GM, Ho LM, Chan SKK, Ho SY, Bacon-Shone J, Choy RYL, Hedley AJ, Lam TH, & Fielding R (2005). Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clinical Infectious Diseases, 40(12), 1713–1720 10.1086/429923 [DOI] [PubMed] [Google Scholar]
- Liu X, Liu C, Tian X, Zou G, Li G, Kong L, & Li P (2016). Associations of perceived stress, resilience and social support with sleep disturbance among community-dwelling adults. Stress and Health : Journal of the International Society for the Investigation of Stress, 32(5), 578–586. 10.1002/SMI.2664 [DOI] [PubMed] [Google Scholar]
- Lo Y (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, & Herzberg PY (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- Lu ZA, Shi L, Que JY, Zheng YB, Wang QW, Liu WJ, Huang YT, Shi J, Bao YP, & Lu L (2022). Long-term psychological profile of general population following COVID-19 outbreak: Symptom trajectories and evolution of psychopathological network. Epidemiology and Psychiatric Sciences, 31, e69. 10.1017/S2045796022000518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71, 543–562. 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Griffin BJ, Copeland LA, Perkins DF, Richardson CB, Finley EP, & Vogt D (2020). Trajectories of functioning in a population-based sample of veterans: Contributions of moral injury, PTSD, and depression. Psychological Medicine, 1–10. 10.1017/S0033291720004249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malesza M, & Kaczmarek MC (2021). Predictors of anxiety during the COVID-19 pandemic in Poland. Personality and Individual Differences, 170. 10.1016/J.PAID.2020.110419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini AD (2019). When acute adversity improves psychological health: A social–contextual framework. Psychological Review, 126(4), 486. 10.1037/REV0000144 [DOI] [PubMed] [Google Scholar]
- Mancini AD (2020). Heterogeneous Mental Health Consequences of COVID-19: Costs and benefits. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S15. 10.1037/tra0000894 [DOI] [PubMed] [Google Scholar]
- Mancini AD, Bonanno GA, & Clark AE (2011). Stepping off the hedonic treadmill: Individual differences in response to major life events. Journal of Individual Differences, 32(3), 144–152. 10.1027/1614-0001/a000047 [DOI] [Google Scholar]
- Mancini AD, Littleton HL, & Grills AE (2016). Can people benefit from acute stress? Social support, psychological improvement, and resilience after the virginia tech campus shootings. Clinical Psychological Science, 4(3), 401–417. 10.1177/2167702615601001 [DOI] [Google Scholar]
- Mancini AD, Westphal M, & Griffin P (2021). Outside the eye of the storm: Can moderate hurricane exposure improve social, psychological, and attachment functioning? Personality & Social Psychology Bulletin, 146167221990488. 10.1177/0146167221990488 [DOI] [PubMed] [Google Scholar]
- McPherson KE, McAloney-Kocaman K, McGlinchey E, Faeth P, & Armour C (2021). Longitudinal analysis of the UK COVID-19 Psychological Wellbeing Study: Trajectories of anxiety, depression and COVID-19-related stress symptomology. Psychiatry Research, 304, 114138. 10.1016/J.PSYCHRES.2021.114138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertens G, Gerritsen L, Duijndam S, Salemink E, & Engelhard IM (2020). Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74. 10.1016/J.JANXDIS.2020.102258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JT, Robertson CD, Anastopolous AD, Nelson-Gray RO, & Kollins SH (2012). Emotion dysregulation and emotional impulsivity among adults with attention-deficit/hyperactivity disorder: Results of a preliminary study. Journal of Psychopathology and Behavioral Assessment, 34, 510–519. 10.1007/s10862-012-9297-2 [DOI] [Google Scholar]
- Moore TM, White LK, Barzilay R, Calkins ME, Jones JD, Young JF, Gur RC, & Gur RE (2020). Development of a scale battery for rapid assessment of risk and resilience. Psychiatry Research, 288, 112996. 10.1016/j.psychres.2020.112996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Belleville G, Bélanger L, & Ivers H (2011). The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, & Raghunathan T (2007). Assessing the emasurement properties of neighborhood scales: From psychometrics to ecometrics. American Journal of Epidemiology, 165(8), 858–867. 10.1093/aje/kwm040 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide Eighth Edition. Muthén & Muthén. Retrieved from https://www.scirp.org/(S(czeh2tfqyw2orz553k1w0r45))/reference/ReferencesPapers.aspx?ReferenceID=2123077 [Google Scholar]
- Muthén B (2004). Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In The SAGE handbook of quantitative methodology for the social sciences (pp. 346–369). SAGE Publications. 10.4135/9781412986311 [DOI] [Google Scholar]
- Muthén B (2003). Statistical and substantive checking in growth mixture modeling: Comment on bauer and curran. Psychological Methods, 8(3), 369–377. 10.1037/1082-989X.8.3.369 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén B (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Özdin S, & Bayrak Özdin Ş (2020). Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. The International Journal of Social Psychiatry, 66(5), 504–511. 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palagini L, Moretto U, Novi M, Masci I, Caruso D, Drake CL, & Riemann D (2018). Lack of resilience is related to stress-related sleep reactivity, hyperarousal, and emotion dysregulation in insomnia disorder. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine, 14(5), 759–766. 10.5664/JCSM.7100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, Hatch S, Wessely S & Abel KM (2020). Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry, 7(7):567–568. doi: 10.1016/S2215-0366(20)30237-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power K (2020). The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice, and Policy, 16(1), 67–73. 10.1080/15487733.2020.1776561 [DOI] [Google Scholar]
- Prati G, & Mancini AD (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. doi: 10.1017/S0033291721000015Prime [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, & Browne D (2020). Risk and resilience in family well-being during the COVID-19 pandemic. The American Psychologist, 75(5), 631–643. 10.1037/AMP0000660 [DOI] [PubMed] [Google Scholar]
- Renna ME, Fresco DM, & Mennin DS (2020). Emotion regulation therapy and its potential role in the treatment of chronic stress-related pathology across disorders. Chronic Stress, 4, 2470547020905787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renna ME, Quintero JM, Fresco DM, & Mennin DS (2017). Emotion regulation therapy: A mechanism-targeted treatment for disorders of distress. Frontiers in Psychology, 8, 6. 10.3389/fpsyg.2017.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E, & Daly M (2021). Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: Longitudinal evidence from the Understanding America Study. British Journal of Health Psychology, 26(2):570–587. doi: 10.1111/bjhp.12493. [DOI] [PubMed] [Google Scholar]
- Schäfer SK, Kunzler AM, Kalisch R, Tüscher O, & Lieb K (2022). Trajectories of resilience and mental distress to global major disruptions. Trends in Cognitive Sciences, 26(12), 1171–1189. 10.1016/J.TICS.2022.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider RL, Long EE, Arch JJ, & Hankin BL (2021). The relationship between stressful events, emotion dysregulation, and anxiety symptoms among youth: Longitudinal support for stress causation but not stress generation. Anxiety, Stress, and Coping, 34(2), 157. 10.1080/10615806.2020.1839730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman AC, Williams ML, Amick BC, Hudson TJ, & Messias EL (2020). Mental health outcomes associated with the COVID-19 pandemic: Prevalence and risk factors in a southern US state. Psychiatry Research, 293, 113476. 10.1016/j.psychres.2020.113476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, & Yehuda R (2014). Resilience definitions, theory, and challenges: Interdisciplinary perspectives. European Journal of Psychotraumatology, 5. 10.3402/ejpt.v5.25338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Taylor SE (2016). Tend and befriend: Biobehavioral bases of affiliation under stress. 10.1111/j.1467-8721.2006.00451.X, 15(6), 273–277. [DOI] [Google Scholar]
- Tyra AT, Griffin SM, Fergus TA, & Ginty AT (2021). Individual differences in emotion regulation prospectively predict early COVID-19 related acute stress. Journal of Anxiety Disorders, 81, 102411. 10.1016/j.janxdis.2021.102411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungar M, & Theron L (2020). Resilience and mental health: How multisystemic processes contribute to positive outcomes. The Lancet Psychiatry, 7(5), 441–448. 10.1016/S2215-0366(19)30434-1 [DOI] [PubMed] [Google Scholar]
- von Dawans B, Fischbacher U, Kirschbaum C, Fehr E, & Heinrichs M (2012). The social dimension of stress reactivity: Acute stress increases prosocial behavior in humans. Psychological Science, 23(6), 651–660. 10.1177/0956797611431576 [DOI] [PubMed] [Google Scholar]
- White LK, Barzilay R, Moore TM, Calkins ME, Jones JD, Himes MM, Young JF, Gur RC, & Gur RE (2022). Risk and resilience measures related to psychopathology in youth. Child Psychiatry and Human Development, 1–12. 10.1007/S10578-021-01296-2/TABLES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


