Key Points
Question
Does immediate coronary angiography after out-of-hospital cardiac arrest (OHCA) with a presumed cardiac cause but without ST-segment elevation improve clinical outcomes at 1 year compared with a delayed or selective invasive approach?
Findings
In this secondary analysis of a randomized clinical trial including 554 patients with OHCA, there was no difference in all-cause mortality at 1 year between the immediate angiography group and a strategy in which angiography was deferred for at least 24 hours or abandoned.
Meaning
Immediate angiography for hemodynamically stable patients with OHCA without ST-segment elevation does not improve clinical outcomes at 1 year compared with a delayed or selective strategy.
Abstract
Importance
Myocardial infarction is a frequent cause of out-of-hospital cardiac arrest (OHCA). The long-term effect of early coronary angiography on patients with OHCA with possible coronary trigger but no ST-segment elevation remains unclear.
Objective
To compare the clinical outcomes of early unselective angiography with the clinical outcomes of a delayed or selective approach for successfully resuscitated patients with OHCA of presumed cardiac origin without ST-segment elevation at 1-year follow-up.
Design, Setting, and Participants
The TOMAHAWK trial was a multicenter, international (Germany and Denmark), investigator-initiated, open-label, randomized clinical trial enrolling 554 patients between November 23, 2016, to September 20, 2019. Patients with stable return of spontaneous circulation after OHCA of presumed cardiac origin but without ST-segment elevation on the postresuscitation electrocardiogram were eligible for inclusion. A total of 554 patients were randomized to either immediate coronary angiography after hospital admission or an initial intensive care assessment with delayed or selective angiography after a minimum of 24 hours. All 554 patients were included in survival analyses during the follow-up period of 1 year. Secondary clinical outcomes were assessed only for participants alive at 1 year to account for the competing risk of death.
Interventions
Early vs delayed or selective coronary angiography and revascularization if indicated.
Main Outcomes and Measures
Evaluations in this secondary analysis included all-cause mortality after 1 year, as well as severe neurologic deficit, myocardial infarction, and rehospitalization for congestive heart failure in survivors at 1 year.
Results
A total of 281 patients were randomized to the immediate angiography group and 273 to the delayed or selective group, with a median age of 70 years (IQR, 60-78 years). A total of 369 of 530 patients (69.6%) were male, and 268 of 483 patients (55.5%) had a shockable arrest rhythm. At 1 year, all-cause mortality was 60.8% (161 of 265) in the immediate angiography group and 54.3% (144 of 265) in the delayed or selective angiography group without significant difference between the treatment strategies, trending toward an increase in mortality with immediate angiography (hazard ratio, 1.25; 95% CI, 0.99-1.57; P = .05). For patients surviving until 1 year, the rates of severe neurologic deficit, myocardial infarction, and rehospitalization for congestive heart failure were similar between the groups.
Conclusions and Relevance
This study found that a strategy of immediate coronary angiography does not provide clinical benefit compared with a delayed or selective invasive approach for patients 1 year after resuscitated OHCA of presumed coronary cause and without ST-segment elevation.
Trial Registration
ClinicalTrials.gov Identifier: NCT02750462
This secondary analysis of a randomized clinical trial examines whether immediate coronary angiography after out-of-hospital cardiac arrest with a presumed cardiac cause but without ST-segment elevation improves clinical outcomes at 1 year compared with a delayed or selective invasive approach.
Introduction
Prognosis for patients experiencing out-of-hospital cardiac arrest (OHCA) is poor, with a survival rate of less than 10%.1 Even among patients initially resuscitated successfully and admitted to the hospital, mortality reaches up to 65%.2 Because acute coronary syndromes are by far the most frequent underlying etiology, accounting for up to 60% of OHCA cases of cardiac cause, it has been hypothesized that immediate coronary angiography possibly followed by revascularization may improve prognosis.3 For patients with ST-segment elevation on the postresuscitation electrocardiogram, there is clinical consensus that coronary angiography should be performed as soon as possible, although to our knowledge no randomized clinical trial supports this recommendation.4 In the far larger population of patients without ST-segment elevation, there has been considerably more controversy regarding the general indication and timing of coronary angiography because the spectrum of underlying causes is broad, including etiologies other than acute coronary syndromes.5,6
The TOMAHAWK randomized clinical trial showed no significant difference in the primary end point of 30-day all-cause mortality between routine immediate coronary angiography (possibly followed by revascularization) and a deferred or selective approach for resuscitated patients with OHCA without ST-segment elevation with or without shockable rhythm.7 However, longer-term follow-up is needed to capture the whole spectrum of possible differential effects between the 2 treatment strategies. Theoretically, early revascularization in acute myocardial infarction could preserve myocardial function and prevent deleterious consequences of myocardial injury, such as heart failure or life-threatening arrhythmias that might become apparent only in the long term. Thus far, only 1 randomized trial (COACT) reported 1-year data in non–ST-segment elevation OHCA of possible cardiac origin and found no significant difference in survival nor in any other clinical end point between an immediate or delayed invasive strategy.8,9 However, in contrast to the TOMAHAWK trial, the population was limited to patients with a shockable arrest rhythm, which make up only approximately 60% of OHCA patients without ST-segment elevation myocardial infarction.10 Here, we report the 1-year results of the TOMAHAWK trial, which included patients with OHCA without ST-segment elevation irrespective of the initial OHCA rhythm.
Methods
TOMAHAWK is an investigator-initiated, randomized, international, multicenter, open-label clinical trial with the primary objective to examine whether successfully resuscitated patients after OHCA of possible cardiac origin without ST-segment elevation benefit from immediate coronary angiography for treating or ruling out acute coronary events compared with initial intensive care evaluation including delayed or selective coronary angiography. The design and the short-term results have been published previously.7,11 In summary, the TOMAHAWK study showed that a strategy of performing immediate angiography provided no benefit over a delayed or selective strategy with respect to the 30-day risk of death from any cause (mortality of 143 of 265 patients [54.0%] in the immediate angiography group vs 122 of 265 patients [46.0%] in the delayed angiography group; hazard ratio, 1.28; 95% CI, 1.00-1.63; log-rank P = .06). The composite secondary end point of death or severe neurologic deficit at 30 days occurred more frequently in the immediate angiography group, indicating possible harm for an emergency invasive approach (relative risk, 1.16; 95% CI, 1.00-1.34).
Safety aspects of this randomized clinical trial were monitored by a dedicated data safety and monitoring board. Written informed consent was obtained for all patients in a dedicated stepwise consent process (further detailed in the eAppendix in Supplement 1). The protocol was approved by the ethics committees of all participating sites (Supplement 2). The trial is registered at ClinicalTrials.gov (NCT02750462). The Consolidated Standards of Reporting Trials (CONSORT) reporting guideline for randomized clinical trials was applied to the study.
Patients
Patients aged 30 years or older with resuscitated OHCA of presumed cardiac origin and return of spontaneous circulation without ST-segment elevation with both shockable and nonshockable arrest rhythms were eligible for inclusion. Patients with hemodynamic or electrical instability were not enrolled. A detailed list of inclusion and exclusion criteria can be found in the eAppendix in Supplement 1. A dedicated stepwise consent process was implemented (further detailed in the eAppendix in Supplement 1).
Randomization and End Points
If eligibility criteria were met, patients were randomized to immediate coronary angiography or initial intensive care assessment and delayed or selective angiography in a 1:1 ratio. Details of treatment after randomization can be found in the eAppendix in Supplement 1.
The primary end point of the trial was 30-day all-cause mortality. The outcomes were reported previously.7 For the 1-year analysis, results are reported for the following prespecified secondary end points: all-cause mortality, severe neurologic deficit (Cerebral Performance Category scores 3-5, defined as severe cerebral disability [3], coma or vegetative state [4], and brain death [5]),12 myocardial infarction, and rehospitalization for congestive heart failure. Definitions of end points are provided in the eAppendix in Supplement 1. The end points severe neurologic deficit, myocardial infarction, and rehospitalization for congestive heart failure were adjudicated by a clinical event committee consisting of experts from the fields of cardiology and neurology. Members of the committee were not otherwise involved in the conduct of the study and were not blinded to treatment allocation because unblinded source data were necessary for adjudication.
Statistical Analysis
Analysis of 1-year end points was performed in the intention-to-treat population, defined as all patients randomized to either treatment group except 4 patients with severe violation of the study’s inclusion criteria (further detailed in the eAppendix in Supplement 1). For the end point all-cause mortality, a Cox model stratified by study site was used to obtain the hazard ratio and 95% CI, and a 2-sided log-rank test was used to obtain the P value. P < .05 was considered to indicate statistical significance. Assuming noninformative censoring, patients lost to follow-up and those with administrative censoring were treated equally. End points other than all-cause death were compared using relative risks with 95% CIs. To compensate for the competing risk of death, the primary analysis for all end points other than all-cause mortality was performed for patients with 1-year survival only.
A post hoc landmark analysis was performed for all-cause mortality, with a landmark at 30 days. Predefined subgroup analyses for 1-year mortality were performed for sex, diabetes, age (<65 and ≥65 years), targeted temperature management (received vs not received), shockable vs nonshockable rhythm, time from arrest to return of spontaneous circulation (<15 vs ≥15 minutes), and confirmed myocardial infarction as OHCA trigger. Data were analyzed from September 1, 2021, to July 31, 2022. Statistical analyses were performed using SAS version 9.4.
Results
Patients
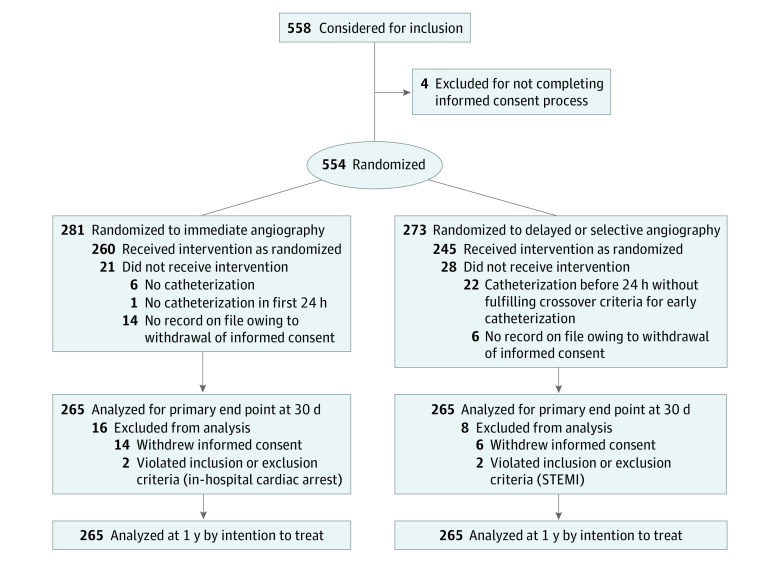
Between November 23, 2016, and September 20, 2019, 554 patients after OHCA of presumed cardiac origin without ST-segment elevation were randomized to immediate angiography (n = 281) or delayed or selective angiography (n = 273) at 31 trial sites in Germany and Denmark (Figure 1). The baseline characteristics of the 554 patients are shown in Table 1. The patients’ median age was 70 years (IQR, 60-78 years), 369 of 530 patients were male (69.6%), 161 were female (30.4%), and approximately one-third had previously known coronary artery disease (79 of 229 [34.5%] in the immediate angiography group and 93 of 229 [40.6%] in the delayed or selective angiography group). Slightly more than half of the overall population (268 of 483 [55.5%]) had a shockable arrest rhythm. Although the arrest was witnessed in 89.5% (462 of 516) of the overall population, bystander cardiopulmonary resuscitation was performed for only 58.9% (294 of 499). The median time from arrest to the beginning of basic life support was 2 minutes (IQR, 0-8 minutes) for patients randomized to immediate angiography and 1 minute (IQR, 0-5 minutes) for patients in the delayed or selective angiography group. The median time from cardiac arrest to return of spontaneous circulation was similar in both groups (15 minutes; IQR, 9-20).
Figure 1. Study Flowchart for the Intention-to-Treat Population.
STEMI indicates ST-segment elevation myocardial infarction.
Table 1. Baseline and Procedural Characteristics.
| Characteristic | Patients, No./total No. (%) | |
|---|---|---|
| Immediate angiography (n = 265) | Delayed or selective angiography (n = 265) | |
| Age, median (IQR), y | 69 (59-78) | 71 (60-79) |
| Sex | ||
| Male | 185/265 (69.8) | 184/265 (69.4) |
| Female | 80/265 (30.2) | 81/265 (30.6) |
| BMI, median (IQR) | 26.5 (24.5-29.4) | 26.2 (24.2-29.4) |
| Diabetes mellitus | 71/244 (29.1) | 74/251 (29.5) |
| Hypertension | 161/240 (67.1) | 162/234 (69.2) |
| Current smoker | 49/164 (29.9) | 59/171 (34.5) |
| Dyslipidemia | 80/227 (35.2) | 84/228 (36.8) |
| Known coronary artery disease | 79/229 (34.5) | 93/229 (40.6) |
| Arrest witnessed | 236/259 (91.1) | 226/257 (87.9) |
| Shockable first monitored rhythm | 126/241 (52.3) | 142/242 (58.7) |
| Bystander cardiopulmonary resuscitation | 142/247 (57.5) | 152/252 (60.3) |
| Time from arrest to basic life support, median (IQR), min | 2 (0-8) | 1 (0-5) |
| Time from arrest to return of spontaneous circulation, median (IQR), min | 15 (10-20) | 15 (8-20) |
| Glasgow Coma Scale score on admission, median (IQR)a | 3 (3-3) | 3 (3-3) |
| Systolic blood pressure on admission, median (IQR), mm Hg | 110 (95-130) | 110 (95-130) |
| Left ventricular ejection fraction on admission, median (IQR), % | 45 (38-56) | 44 (30-50) |
| Coronary angiography performed | 253/265 (95.5) | 165/265 (62.3) |
| Time from arrest to coronary angiography, median (IQR), h | 2.9 (2.2-3.9) | 46.9 (26.1-116.6) |
| Severity of coronary artery disease | ||
| No significant disease | 99/252 (39.3) | 46/165 (27.9) |
| 1-Vessel disease | 37/252 (14.7) | 21/165 (12.7) |
| 2-Vessel disease | 32/252 (12.7) | 26/165 (15.8) |
| 3-Vessel disease | 84/252 (33.3) | 72/165 (43.6) |
| Culprit lesion identified | 94/247 (38.1) | 67/156 (42.9) |
| Percutaneous coronary intervention performed | 93/250 (37.2) | 70/162 (43.2) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
The Glasgow Coma Scale score is the summation of scores for eye, verbal, and motor responses. The minimum score is 3, which indicates deep coma or a brain-dead state. The maximum is 15, which indicates a fully awake patient.
Treatment and Procedures
Early in-hospital treatment and procedures are displayed in Table 1. Coronary angiography was performed for 253 of 265 patients (95.5%) in the immediate group and for 165 of 265 patients (62.3%) in the delayed or selective angiography group after a median of 2.9 hours (IQR, 2.2-3.9 hours) and 46.9 hours (IQR, 26.1-116.6 hours), respectively. A total of 22 of 273 patients (8.1%) randomized to delayed or selective angiography underwent coronary angiography within the first 24 hours after hospital admission without meeting prespecified criteria for early emergency catheterization, thereby violating the study protocol. Targeted temperature management was performed for 410 of 525 patients (78.1%) in the overall population (immediate angiography, 204 of 263 patients [77.6%]; delayed or selective angiography, 206 of 262 patients [78.6%]). The time from hospital admission to the beginning of targeted temperature management was slightly longer for patients randomized to immediate angiography (median, 153 minutes [IQR, 67-242] vs 119 minutes [IQR, 30-205]).
End Points
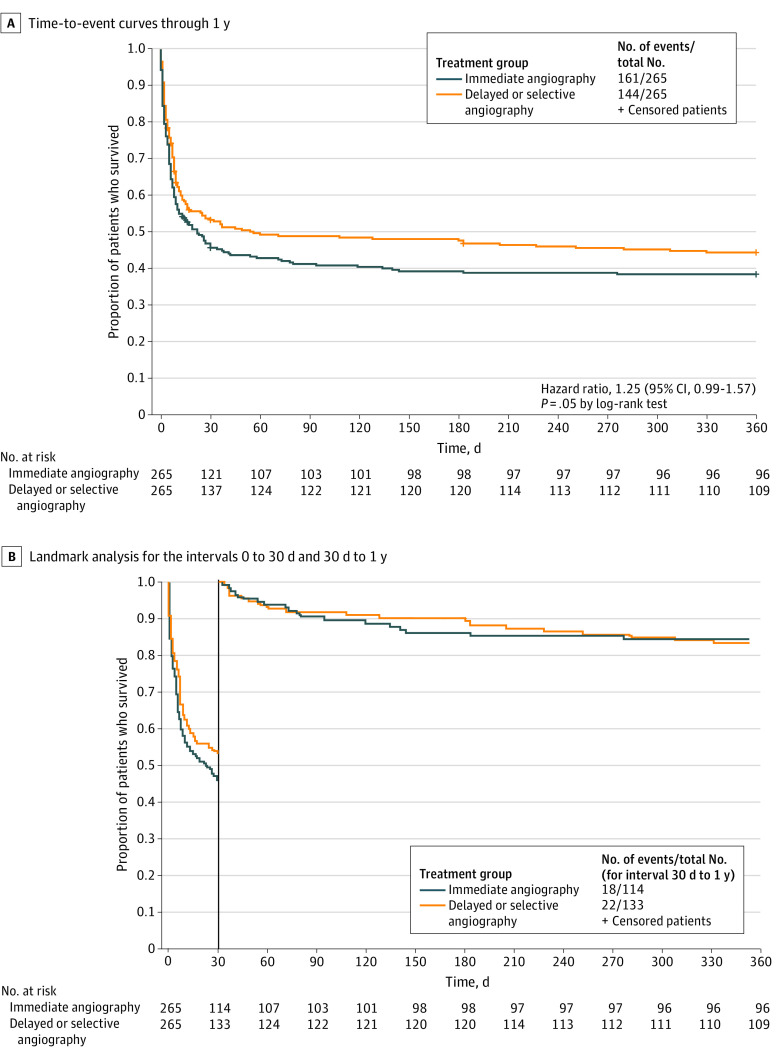
All patients whose data had been analyzed for the primary end point at 30 days were also available for analysis of 1-year all-cause mortality in the intention-to-treat population (Figure 1). All-cause mortality was 60.8% (161of 265) in the immediate angiography group and 54.3% (144 of 265) in the delayed or selective angiography group, without decisive difference between the treatment strategies, trending toward an increase in mortality with immediate angiography (hazard ratio, 1.25; 95% CI, 0.99-1.57; log-rank P = .05) (Table 2 and Figure 2A). These results were consistent across all predefined subgroups (Figure 3). For the surviving patients, the rates of severe neurologic deficit (relative risk, 1.47; 95% CI, 0.66-3.26), myocardial infarction (relative risk, 0.00; 95% CI, 0.00-1.47), and rehospitalization for congestive heart failure (relative risk, 0.92; 95% CI, 0.27-3.08) were similar at 1 year (Table 2). A post hoc landmark analysis (30 days to 1 year) revealed that mortality rates after the first month were markedly lower than in the first 30 days (40 vs 265 deaths) (Figure 2B). There was no difference in all-cause mortality between the treatment groups in the period between 30 days and 1 year (relative risk, 0.95; 95% CI, 0.54-1.67) (Figure 2B).
Table 2. Clinical Outcomes at 1 Yeara.
| Outcome | Patients, No./total No. (%) | Effect size (95% CI)b | |
|---|---|---|---|
| Immediate angiography | Delayed or selective angiography | ||
| All-cause mortality | 161/265 (60.8) | 144/265 (54.3) | HR, 1.25 (0.99-1.57) |
| Severe neurologic deficit in survivors (CPC scores 3-5)c | 12/89 (13.5) | 9/98 (9.2) | RR, 1.47 (0.66-3.26) |
| Myocardial infarction in survivors | 0/87 | 3/101 (3.0) | RR, 0.00 (0.00-1.47) |
| Rehospitalization for congestive heart failure in survivors | 4/87 (4.6) | 5/100 (5.0) | RR, 0.92 (0.27-3.08) |
Abbreviations: CPC, Cerebral Performance Category; HR, hazard ratio; RR, relative risk.
All end points other than all-cause mortality were analyzed only for patients who survived 1 year.
The delayed angiography group is used as the reference group for HRs and RR estimates. The 95% CIs have not been adjusted for multiplicity, and therefore inferences drawn from these intervals may not be reproducible.
The CPC score evaluates neurologic outcome in the survivors and ranges from 1 to 5. Scores of 3, 4, and 5 reflect poor outcome (severe neurologic disability, persistent vegetative state, or brain death, respectively).
Figure 2. All-Cause Mortality End Point.
Event rates indicate Kaplan-Meier estimates.
Figure 3. Forest Plot of the End Point 1-Year All-Cause Mortality in Prespecified Subgroups.
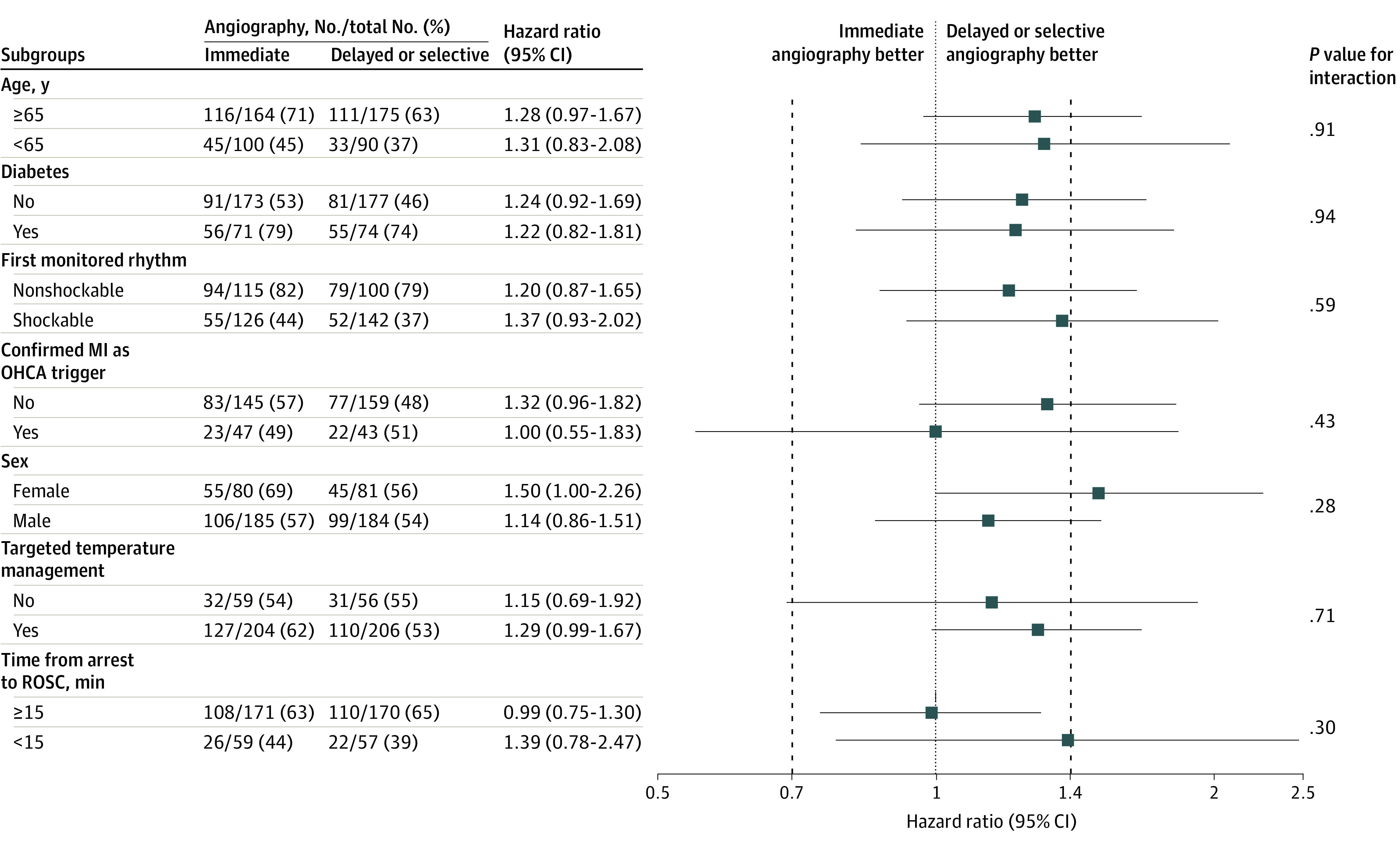
MI indicates myocardial infarction; OHCA, out-of-hospital cardiac arrest; and ROSC, return of spontaneous circulation.
Discussion
This international multicenter randomized clinical trial compared a strategy of immediate unselected coronary angiography with that of a delayed or selective approach for patients after successfully resuscitated OHCA of presumed cardiac origin with shockable and nonshockable arrest rhythm and no ST-segment elevation. The main results are displayed in the structured graphic abstract. The prespecified follow-up analysis presented here showed no difference between the 2 approaches regarding all-cause mortality within 1 year. Also, no differences were found in the incidence of severe neurologic deficit, myocardial infarction, or rehospitalization for heart failure at 1 year. However, a signal of higher mortality for patients who had been randomized to immediate angiography was observed, comparable to the 30-day results.7 Theoretic causes for a potential detrimental effect of emergency angiography might include delays in alternative diagnoses of OHCA and in optimal postresuscitation intensive care therapy. However, the observed trend regarding mortality might also be a chance finding, given that such result was not observed in the other randomized trials in the field. As demonstrated by landmark analysis, mortality occurred predominantly within the first weeks after the cardiac arrest, whereas thereafter mortality up to 12 months was markedly lower in both groups. The low absolute numbers of myocardial infarction or rehospitalization for congestive heart failure mirror the generally favorable clinical course in survivors but might also partially be a consequence of the competing risk of death, thereby reducing the number of patients who can potentially experience these events.
These results are in line with those of the COACT study, the only other randomized trial, to our knowledge, that has thus far presented longer-term results. Similar to the TOMAHAWK trial, there were no significant differences in clinical outcomes between immediate and delayed coronary angiography at 1 year.9 The clinically most meaningful difference between both trials is that the COACT study enrolled only patients with OHCA with a shockable arrest rhythm, whereas the TOMAHAWK trial recruited patients with both shockable and nonshockable rhythms and thus a broader risk spectrum. In addition to the 2 large trials (TOMAHAWK and COACT), 4 small randomized trials comparing immediate and delayed or selective coronary angiography in OHCA have been published.13,14,15,16 At short-term follow-up, there was also no benefit of emergency angiography.
When all available studies are summarized, a consistent pattern of a lack of prognostic benefit of immediate coronary angiography for survivors of OHCA without ST-segment elevation is observed. Although speculative, there are several possible explanations for this finding. First, the overall prognosis for most patients with OHCA is primarily influenced by neurologic rather than cardiac injury. Cardiac interventions will influence prognosis only if they are at least partially in the causal pathway leading to the clinical outcome. Observational data raise the question of whether the subgroup of patients with OHCA who are at low risk for neurologic injury might benefit from early coronary angiography.17,18 Integrating models to correlate with neurologic outcome into trial designs could help to find subgroups of patients for whom early angiography might be beneficial.18,19 In this regard, dedicated cardiac arrest centers including multidisciplinary teams of interventional cardiologists, as well as emergency medicine and critical care specialists, might be best suited to find individualized clinical pathways.20 Second, in the overall population of patients with OHCA without ST-segment elevation, the number of patients with a coronary culprit lesion is relatively low (40% in the TOMAHAWK trial). It is only for these patients that a potential benefit of immediate coronary revascularization can be expected. However, associating the presence of a culprit lesion noninvasively has proven to be difficult. Several easily measured markers such as shockable arrest rhythm, clinical history, electrocardiogram changes other than ST-segment elevation, echocardiographic abnormalities, and troponin values have shown only modest sensitivity and specificity.21,22,23,24,25,26,27
Limitations
The trial has several limitations. First, although prespecified, outcomes at 1 year are exploratory only. Second, physicians and intensive care unit staff members were not blinded to treatment randomization. Management of OHCA involves complex clinical decision-making; thus, residual bias cannot be ruled out. Third, the end points analyzed might not comprehensively cover the complete spectrum of clinical outcomes; for example, we did not measure cardiac functional parameters such as left ventricular ejection fraction systematically. Fourth, data on medical treatment in the surviving patients were not assessed during long-term follow-up. Psychosocial impact in survivors is also an important aspect to be considered. Analyses on quality of life were prespecified in the present trial and will be reported separately. Fifth, owing to the inclusion and exclusion criteria the results do not apply to patients with ST-segment elevation or cardiogenic shock after OHCA, for whom immediate angiography is still strongly recommended, although randomized trials supporting these recommendations are not available.
Conclusions
In conclusion, this secondary analysis showed that the risk of all-cause death at 1 year was not significantly different between immediate vs delayed or selective coronary angiography for patients after resuscitated OHCA of presumed cardiac cause and without ST-segment elevation, challenging the long-held belief that an emergency invasive approach is beneficial in this patient population.
eAppendix.
eReferences.
Trial Protocol
Nonauthor Collaborators. TOMAHAWK Investigators
Data Sharing Statement
References
- 1.Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61. doi: 10.1186/s13054-020-2773-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grunau B, Kime N, Leroux B, et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA. 2020;324(11):1058-1067. doi: 10.1001/jama.2020.14185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geri G, Passouant O, Dumas F, et al. Etiological diagnoses of out-of-hospital cardiac arrest survivors admitted to the intensive care unit: insights from a French registry. Resuscitation. 2017;117:66-72. doi: 10.1016/j.resuscitation.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 4.Ibanez B, James S, Agewall S, et al. ; ESC Scientific Document Group . 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 5.Dumas F, Cariou A, Manzo-Silberman S, et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian Region Out of Hospital Cardiac Arrest) registry. Circ Cardiovasc Interv. 2010;3(3):200-207. doi: 10.1161/CIRCINTERVENTIONS.109.913665 [DOI] [PubMed] [Google Scholar]
- 6.Zanuttini D, Armellini I, Nucifora G, et al. Predictive value of electrocardiogram in diagnosing acute coronary artery lesions among patients with out-of-hospital-cardiac-arrest. Resuscitation. 2013;84(9):1250-1254. doi: 10.1016/j.resuscitation.2013.04.023 [DOI] [PubMed] [Google Scholar]
- 7.Desch S, Freund A, Akin I, et al. ; TOMAHAWK Investigators . Angiography after out-of-hospital cardiac arrest without ST-segment elevation. N Engl J Med. 2021;385(27):2544-2553. doi: 10.1056/NEJMoa2101909 [DOI] [PubMed] [Google Scholar]
- 8.Lemkes JS, Janssens GN, van der Hoeven NW, et al. Coronary angiography after cardiac arrest without ST-segment elevation. N Engl J Med. 2019;380(15):1397-1407. doi: 10.1056/NEJMoa1816897 [DOI] [PubMed] [Google Scholar]
- 9.Lemkes JS, Janssens GN, van der Hoeven NW, et al. Coronary angiography after cardiac arrest without ST segment elevation: one-year outcomes of the COACT randomized clinical trial. JAMA Cardiol. 2020;5(12):1358-1365. doi: 10.1001/jamacardio.2020.3670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dumas F, Bougouin W, Geri G, et al. Emergency percutaneous coronary intervention in post-cardiac arrest patients without ST-segment elevation pattern: insights from the PROCAT II registry. JACC Cardiovasc Interv. 2016;9(10):1011-1018. doi: 10.1016/j.jcin.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 11.Desch S, Freund A, Graf T, et al. Immediate unselected coronary angiography versus delayed triage in survivors of out-of-hospital cardiac arrest without ST-segment elevation: design and rationale of the TOMAHAWK trial. Am Heart J. 2019;209:20-28. doi: 10.1016/j.ahj.2018.12.005 [DOI] [PubMed] [Google Scholar]
- 12.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480-484. doi: 10.1016/S0140-6736(75)92830-5 [DOI] [PubMed] [Google Scholar]
- 13.Elfwén L, Lagedal R, Nordberg P, et al. Direct or Subacute Coronary Angiography in Out-of-Hospital Cardiac Arrest (DISCO)—an initial pilot-study of a randomized clinical trial. Resuscitation. 2019;139:253-261. doi: 10.1016/j.resuscitation.2019.04.027 [DOI] [PubMed] [Google Scholar]
- 14.Hauw-Berlemont C, Lamhaut L, Diehl JL, et al. ; EMERGE Investigators . Emergency vs delayed coronary angiogram in survivors of out-of-hospital cardiac arrest: results of the randomized, multicentric EMERGE trial. JAMA Cardiol. 2022;7(7):700-707. doi: 10.1001/jamacardio.2022.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kern KB, Radsel P, Jentzer JC, et al. Randomized pilot clinical trial of early coronary angiography versus no early coronary angiography after cardiac arrest without ST-segment elevation: the PEARL study. Circulation. 2020;142(21):2002-2012. doi: 10.1161/CIRCULATIONAHA.120.049569 [DOI] [PubMed] [Google Scholar]
- 16.Viana-Tejedor A, Ariza-Solé A, Martínez-Sellés M, et al. Role of coronary angiography in patients with a non-diagnostic electrocardiogram following out of hospital cardiac arrest: rationale and design of the multicentre randomized controlled COUPE trial. Eur Heart J Acute Cardiovasc Care. 2020;9(4 suppl):S131-S137. doi: 10.1177/2048872618813843 [DOI] [PubMed] [Google Scholar]
- 17.Bougouin W, Dumas F, Karam N, et al. ; Sudden Death Expertise Center . Should we perform an immediate coronary angiogram in all patients after cardiac arrest? insights from a large French registry. JACC Cardiovasc Interv. 2018;11(3):249-256. doi: 10.1016/j.jcin.2017.09.011 [DOI] [PubMed] [Google Scholar]
- 18.Pareek N, Kordis P, Beckley-Hoelscher N, et al. A practical risk score for early prediction of neurological outcome after out-of-hospital cardiac arrest: MIRACLE2. Eur Heart J. 2020;41(47):4508-4517. doi: 10.1093/eurheartj/ehaa570 [DOI] [PubMed] [Google Scholar]
- 19.Pareek N, Beckley-Hoelscher N, Kanyal R, et al. MIRACLE2 score and SCAI grade to identify patients with out-of-hospital cardiac arrest for immediate coronary angiography. JACC Cardiovasc Interv. 2022;15(10):1074-1084. doi: 10.1016/j.jcin.2022.03.035 [DOI] [PubMed] [Google Scholar]
- 20.Pareek N, Rees P, Quinn T, et al. British Cardiovascular Interventional Society consensus position statement on out-of-hospital cardiac arrest 1: pathway of care. Interv Cardiol. 2022;17:e18. doi: 10.15420/icr.2022.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dumas F, Manzo-Silberman S, Fichet J, et al. Can early cardiac troponin I measurement help to predict recent coronary occlusion in out-of-hospital cardiac arrest survivors? Crit Care Med. 2012;40(6):1777-1784. doi: 10.1097/CCM.0b013e3182474d5e [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Tejada J, Jurado-Román A, Rodríguez J, et al. Post-resuscitation electrocardiograms, acute coronary findings and in-hospital prognosis of survivors of out-of-hospital cardiac arrest. Resuscitation. 2014;85(9):1245-1250. doi: 10.1016/j.resuscitation.2014.06.001 [DOI] [PubMed] [Google Scholar]
- 23.Lee SE, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B. Combined ECG, echocardiographic, and biomarker criteria for diagnosing acute myocardial infarction in out-of-hospital cardiac arrest patients. Yonsei Med J. 2015;56(4):887-894. doi: 10.3349/ymj.2015.56.4.887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sideris G, Voicu S, Dillinger JG, et al. Value of post-resuscitation electrocardiogram in the diagnosis of acute myocardial infarction in out-of-hospital cardiac arrest patients. Resuscitation. 2011;82(9):1148-1153. doi: 10.1016/j.resuscitation.2011.04.023 [DOI] [PubMed] [Google Scholar]
- 25.Stær-Jensen H, Nakstad ER, Fossum E, et al. Post-resuscitation ECG for selection of patients for immediate coronary angiography in out-of-hospital cardiac arrest. Circ Cardiovasc Interv. 2015;8(10):e002784. doi: 10.1161/CIRCINTERVENTIONS.115.002784 [DOI] [PubMed] [Google Scholar]
- 26.Voicu S, Sideris G, Deye N, et al. Role of cardiac troponin in the diagnosis of acute myocardial infarction in comatose patients resuscitated from out-of-hospital cardiac arrest. Resuscitation. 2012;83(4):452-458. doi: 10.1016/j.resuscitation.2011.10.008 [DOI] [PubMed] [Google Scholar]
- 27.Waldo SW, Chang L, Strom JB, O’Brien C, Pomerantsev E, Yeh RW. Predicting the presence of an acute coronary lesion among patients resuscitated from cardiac arrest. Circ Cardiovasc Interv. 2015;8(10):e002198. doi: 10.1161/CIRCINTERVENTIONS.114.002198 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix.
eReferences.
Trial Protocol
Nonauthor Collaborators. TOMAHAWK Investigators
Data Sharing Statement