Figure 1.
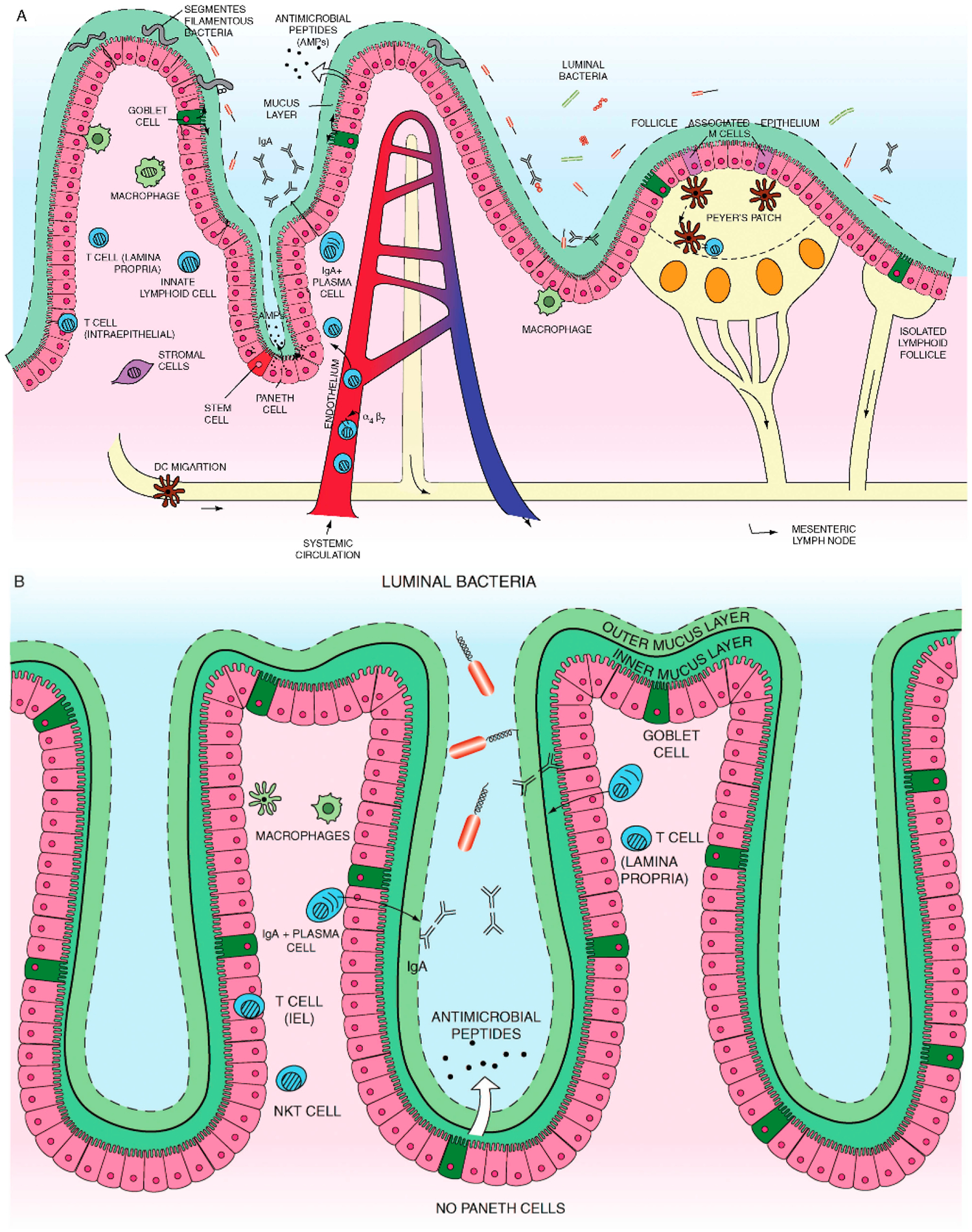
(A) Small intestine mucosal immune system landscape. The intestinal epithelial cell (IEC) layers form villi and crypt structures and are composed of different cell lineages. Goblet cells secrete mucus. Paneth cells, found only in the small intestine, can be found at the base of the crypts and are the main secretors of antimicrobial peptides. The base of the crypts also contains the IEC stem cell populations. Immune cells can be found in organized tissue such as Peyer’s patches and throughout the lamina propria. They include macrophages, dendritic cells, intra-epithelial lymphocytes, lamina propria effector T cells, IgA secreting plasma cells, innate lymphoid cells and stromal cells such as fibroblasts. Antigen presenting cells in Peyer’s patches or mesenteric lymph nodes interact with and activate local lymphocytes, which consequently upregulate expression of the integrin α4β7. Such cells then enter the systemic circulation but home towards the gut, in response to chemokine ligands such as CCL25. (B) Colon (large intestine) mucosal immune system. The colon has a much higher bacterial load and a markedly different immune cell composition.
The colon contains only crypts, no villi. Also there are no Paneth cells, which mean that enterocytes have a much more important contribution to antimicrobial peptide production. However, there is a high prevalence of goblet cells. The mucus forms dual layers, with a thick largely sterile inner layer and a thinner outer layer. There are no Peyer’s patches. While the immune cell types present are similar to those found in the small intestine it is likely that there may be at least subtle differences. In particular natural killer T cells are found more frequently and have a more significant role in the colon. Adapted with permission from “Recent advances in inflammatory bowel disease: Mucosal immune cells in intestinal inflammation” by Cader and Kaser, Gut 2013, 62, 1653–1664, BMJ Publishing Group Limited [48].
