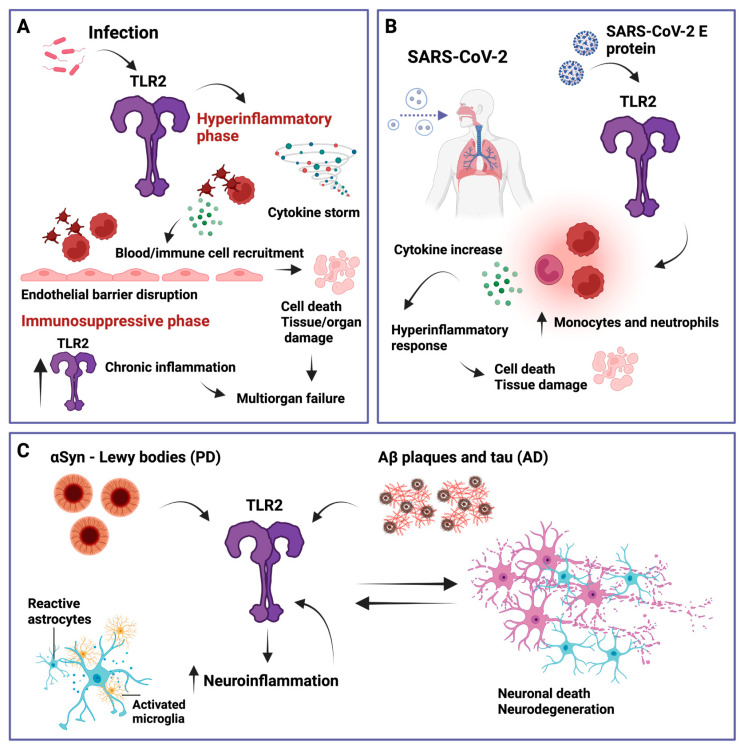
Figure 3.
Simplified overview of TLR2 involvement in several relevant inflammatory diseases. (A) Sepsis. When immune regulation fails and a hyperinflammatory state is induced via elevated cytokine production (cytokine storm), sepsis can be triggered by TLR2, which further activates platelets and other immune cells that then interact with endothelial cells, leading to endothelial barrier disruption, cell death, and tissue and organ damage. In addition, TLR2 has been shown to be elevated during the immunosuppressive phase of sepsis which can lead to multiorgan failure. (B) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). TLR2 can recognize the SARS-CoV-2 envelope (E) protein, leading to an increase in inflammatory monocytes and neutrophils, inducing a hyperinflammatory response that can cause cell death and tissue damage. (C) Parkinson’s disease (PD) and Alzheimer’s disease (AD). TLR2 can recognize α-synuclein (αSyn) and amyloid-β (Aβ) plaques and tau, respectively. This promotes neuroinflammation characterized by reactive astrocytes and activated microglia, which further increase TLR2 levels, leading to a feedback loop of neuronal cell death, further TLR2 upregulation, and neuroinflammation. Created with BioRender.com.