Fig. 1. Adjusted hazard ratios (HRs) for uterine perforation and intrauterine device (IUD) expulsion, by risk factor. Adjusted HRs were calculated using Cox models weighted with propensity score overlap weights. *For the postpartum timing risk factor, the following variables were included in the propensity score models for adjustment: IUD type, menorrhagia, age (tertiles), race and ethnicity, recent smoker (uterine perforation only), duration of look-back period (quartiles, uterine perforation only), calendar year of IUD insertion, body mass index (categorical), dysmenorrhea, uterine leiomyomas, parity, concomitant gynecologic procedure, difficult insertion, health care professional experience, site, calendar year×site, parity×site, age (tertiles)×site, and recent smoker×site (uterine perforation only). HMB, heavy menstrual bleeding; LNG, levonorgestrel. †For the breastfeeding risk factor, the following variables were included in the propensity score models for adjustment: postpartum timing, IUD type, menorrhagia, age (tertiles), race/ethnicity, recent smoker (uterine perforation only), duration of look-back period (quartiles, uterine perforation only), calendar year of IUD insertion, BMI (categorical), dysmenorrhea, uterine fibroids, parity, cesarean delivery any time before the index date (uterine perforation only), cesarean delivery for the most recent delivery (uterine perforation only), concomitant gynecologic procedures, difficult insertion, healthcare professional experience, live birth in 52 weeks before IUD insertion, site, and postpartum×site interaction. ‡For the HMB risk factor, the following variables were included in the propensity score models for adjustment: postpartum status (4 categories), breastfeeding status, IUD type, age (continuous for perforation, tertiles for expulsion), race/ethnicity, recent smoker (uterine perforation only), duration of look-back period (quartiles, uterine perforation only), calendar year of IUD insertion, BMI (categorical), dysmenorrhea, uterine fibroids, parity, cesarean delivery any time before the index date (only for perforation), cesarean delivery for the most recent delivery, live birth for the most recent delivery, concomitant gynecologic procedure, indicator of difficult IUD insertion, healthcare professional experience (quartiles), research site, and age (continuous for perforation and tertile for expulsion)×site interaction. §For the IUD type risk factor, the following variables were included in the propensity score models for adjustment: postpartum status (4 categories), breastfeeding status, menorrhagia diagnosis in the last 52 weeks, age (tertiles), race/ethnicity, recent smoker (uterine perforation only), duration of look-back period (quartiles, uterine perforation only), calendar year of IUD insertion (categorical), BMI (categorical), dysmenorrhea, uterine fibroids, parity, cesarean delivery at any time before the index date, cesarean delivery for the most recent delivery (uterine perforation only), live birth for the most recent delivery, concomitant gynecologic procedure, indicator of difficult IUD insertion, healthcare professional experience (quartiles), live birth in 52 weeks before IUD insertion, research site, and postpartum×site interaction (IUD expulsion only).
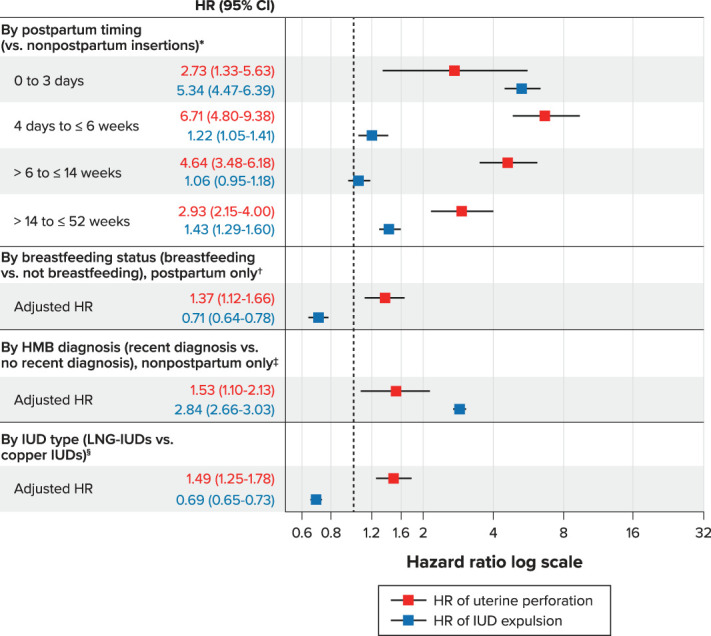
Fassett. Uterine Perforation and Expulsion Risks With IUDs. Obstet Gynecol 2023.
