Abstract
Background
Acromioclavicular (AC) horizontal instability is a problem affecting not only young athletic patients after a trauma to the AC joint but also older patients who have undergone distal clavicle resection. It may cause pain and poor functional outcomes unless the reconstruction technique specifically addresses the horizontal instability of the clavicle, in addition to the well-known superior instability.
Methods
Three cadaveric specimens underwent dissection of the AC joint capsule to determine the superior attachments of the AC joint capsule. These shoulders subsequently underwent distal clavicle resection and were loaded to a 7-kg weight in the horizontal plane. The horizontal displacement of the clavicle was measured and resection continued to the point of horizontal instability of the clavicle. Thereafter, the reverse coracoacromial ligament reconstruction technique was performed and recreation of horizontal stability assessed. Utilization of the reverse coracoacromial ligament transfer in two clinical cases will also be presented.
Results
The AC joint capsule is continuous with trapezius and deltoid insertions. The average distance between the articular surface and insertion of the capsule on the clavicle is 10 mm and on the acromion is 14.8 mm. Horizontal clavicular translation increased from 2.3 mm when intact to 3.3 mm with capsular transection, 8.7 mm with 5 mm clavicle resection, and finally 15 mm with a 10-mm clavicle resection. Horizontal instability of the clavicle was demonstrated with a 10-mm clavicle resection.
Conclusion
Horizontal instability of the clavicle is evident with distal clavicle resection of greater than 10 mm. A reverse coracoacromial ligament transfer may be a reasonable technique to address horizontal stability of the clavicle during AC joint reconstruction in the context of painful instability.
Keywords: Clavicle, Horizontal, Instability, Coracoacromial ligament
The acromioclavicular (AC) joint is a diarthrodial joint, whose primary stability is passively provided by the integrated function of the coracoclavicular (CC) ligaments, the coracoacromial (CA) ligament, and AC joint capsule.1 While the CC ligament complex provides the primary suspensory restraint of the AC joint against superior translation, the AC joint capsule is the primary restraint against anteroposterior (AP) translation of the distal clavicle. Biomechanical studies have demonstrated that the AC joint capsule provides 90% of the AP stability of the clavicle, with the majority of this stability coming from the posterior and superior portion of the AC joint capsule.1,5 Injuries to the AC joint disrupt these static restraints to varying degrees.
AC joint injuries are very common in the young athletic population, making up 9% of all shoulder girdle injuries and accounting for 12% of dislocations of the upper limb.1 These injuries are often caused by a direct blow to the shoulder during contact sports, while the arm is in an adducted position or by a fall on an adducted arm.1 Surgical intervention is indicated for Rockwood grade IV-VI injuries, with ongoing debate regarding the optimum management strategy for grade III injuries, while initial nonoperative management is indicated for grade I and II injuries.
AC joint instability is a common source of pain and disability. “Horizontal” instability of the AC joint refers to instability of the AC joint owing to disruption of the AC joint capsule with intact CC ligaments. This is a dynamic phenomenon leading to impingement of the lateral clavicle posteriorly against the scapula spine. There are two clinical scenarios in which a patient may present with “horizontal” AC joint instability:
-
1)
Younger patients, without radiographic evidence of AC joint arthritis, have sustained a grade I or II AC joint injury and have failed nonoperative management.
-
2)
Older patients with AC joint pain secondary to arthritis who had resection of the lateral end of the clavicle, producing iatrogenic “horizontal” instability of the AC joint.
Those individuals with AC joint instability may present with pain and clicking in the region of the AC joint, which may be replicated on Speed’s test, ÓBrien test and cross-body adduction testing.1,8 Magnetic resonance imaging (MRI) in such patients may often demonstrate static posterior translation of the clavicle associated with bony edema of the scapula spine, secondary to impingement of the distal clavicle against the scapular spine.
“Horizontal” instability of the AC joint is often under recognized and currently there is no well-described surgical solution to this problem. The purpose of this investigation was to determine the maximal amount of distal clavicle that may be resected before the development of iatrogenic “horizontal” instability of the AC joint and to describe a novel surgical reconstruction technique to neutralize “horizontal” instability of the AC joint: the reverse CA ligament transfer.
Materials and methods
Three male cadaveric specimens were used for the dissections. There was no evidence of prior surgery to the AC joint or shoulder girdle for any of the specimens. The cadaveric specimens were intact from the head to the trunk. The cadavers were rigidly secured to a dissection board in such a way as to maintain a static position of the axial skeleton and sternoclavicular joint, however allowing the free motion of the limb which was being dissected.
A saber incision was made, centered over the AC joint and the coracoid tip. Sharp dissection through the skin and fat layers was performed down to the AC joint. The location of the AC joint was identified with a 24-gauge needle. After identifying the anterior and posterior borders of the AC joint, a longitudinal split was made in the AC joint capsule and anterior and posterior periosteal-capsular flaps were raised. At this stage, measurements were performed to identify the anterior and posterior attachments of the AC joint capsule to both the clavicle and the acromion. All measurements were performed using a standardized ruler. Having raised anterior and posterior flaps, the center of the AC joint in the AP axis was identified and the joint gap was measured. None of the specimens were noted to have osteoarthritis of the AC joint.
Bone tunnels were drilled in an AP direction through the lateral acromion and a 2-0 FiberTape (Arthrex, Inc., Naples, FL, USA) was then passed through the tunnels as a traction suture. The acromion was loaded with 7 kg in the AP plane and the degree of displacement between the center of the clavicle and the center of the acromion was measured (Fig. 1). The capsule was then repaired with a 1 vicryl suture and the loading measurements were repeated (Fig. 2).
Figure 1.
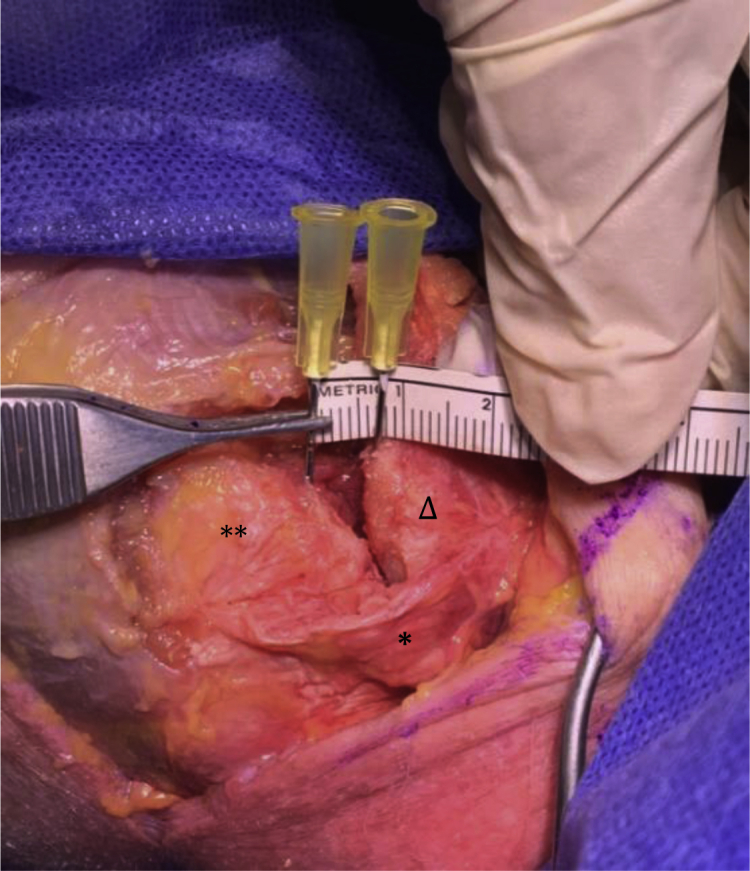
This figure demonstrates the acromion clavicular joint with the capsule (∗) sectioned and the native AC joint gap highlighted between the hypodermic needles. ∗∗, acromion, Δ, clavicle.
Figure 2.

This figure demonstrates the repair of the AC joint capsule with a 1 vicyrl suture and a 7-kg loading force placed on the lateral acromion.
Next, a 5-mm resection of the lateral clavicle was performed, and the AC gap was measured at rest and with 7 kg of loading with both the capsule incised and the capsule subsequently repaired. This procedure was repeated with a 10-mm clavicle resection. The resections did not continue beyond 10 mm as after this point the AC joint capsule was no longer able to be satisfactorily repaired, and horizontal instability of the clavicle was demonstrated, whereby posterior impingement of the lateral clavicle against the spine of the scapula occurs.
After the clavicle resections, we performed the surgical reconstruction technique. This is a reverse CA ligament transfer, which involves harvesting the CA ligament from its insertion into the coracoid with a sleeve of periosteum and subsequent fixation of this caudal end of the CA ligament into the end of the distal clavicle, while leaving its origin attached to the acromion. The CA ligament is hereto first identified and dissected from its coracoid attachment with some periosteum and freed along its available length. Thereafter, the CA ligament is prepared with a whipstitch using two number 2 FiberWire (Arthrex, Inc., Naples, FL, USA) sutures. The lateral end of the clavicle, having already been prepared with the clavicle resections, is then drilled with a 2-mm drill in an oblique fashion from posterior to anterior, allowing the passage of the sutures. This drill hole is enlarged at the posterior end to allow for the passage of the CA ligament into a bone tunnel. The sutures are then passed through the clavicular drill hole and tensioned with the clavicle held in a maximal anterior position. The CA ligament is then held in this tunnel with the use of an EndoButton (Smith & Nephew, Inc., Andover, MA, USA). The AC joint capsule is then repaired over the AC joint reconstruction. Figure 3 depicts the reverse CC ligament transfer, while Figure 4 depicts the cadaveric CA ligament transfer.
Figure 3.
Schematic drawing demonstrating the harvesting of the CA ligament from the tip of the coracoid process, subsequent transfer through the clavicular bone tunnel and fixation with an endobutton. ∗ CA ligament transfer through clavicle bone tunnel.
Figure 4.
Cadaveric reverse CA ligament transfer. ∗ CA ligament. ∗∗ EndoButton fixation on the anterior clavicle. † Clavicle. ‡ Acromion. CA, coracoacromial.
The reconstructive technique is further presented in two case studies, with video footage of the prereconstructive and postreconstructive horizontal stability.
Results
Anatomy of the AC joint capsule
Dissection of the AC joint capsule revealed continuity between the trapezius and deltoid insertions with the AC joint capsule itself. The capsule is significantly thicker in the posterior and superior aspect of the capsule compared with the anterior flap of the AC joint, which in one specimen was no more than a thin film of soft tissue.
The distance between the intra-articular end of the distal clavicle and the point of insertion of the AC joint capsule onto the clavicle was measured, along with the distance between the acromial insertion of the AC joint capsule and the intra-articular aspect of the acromion. These results are demonstrated in Table I.
Table I.
This outlines the length of the acromion and clavicle within the insertion of the AC joint capsule. The measurements are taken from the acromial or clavicular edge of the AC joint space and measured to the furthermost point of insertion of the capsule onto bone.
| Specimen | Distance to acromial insertion (mm) | Distance to clavicle insertion (mm) |
|---|---|---|
| 1 | 14 | 15 |
| 2 | 13 | 10 |
| 3 | 16 | 11 |
AC, acromioclavicular.
The effects of sequential distal clavicular resection
The AC joint was loaded in the horizontal plane. The AC joint was identified, and two corresponding central points of the joint were marked. The width of the resting AC joint gap was measured. The joint was loaded in the horizontal plane of the clavicle to 7 kgs. The measurements were taken with the AC joint capsule intact, the AC joint capsule incised and then after a clavicular resection of 5 mm and 10 mm. For each clavicular resection, the AC joint capsule was repaired onto the distal clavicle. We did not perform a 15-mm clavicular resection as the capsule was unable to be repaired onto the distal clavicle, based on the earlier results obtained. The figures highlighting the displacement are highlighted in Table II.
Table II.
AC joint displacement under different conditions – capsular incision, 5-mm resection, and 10-mm resection. All loaded to 7 kgs in horizontal plane.
| Specimen | AC joint space (mm) | AC displacement loaded (mm) intact AC joint capsule | AC displacement capsule incised and flaps raised, loaded (mm) | AC displacement, 5-mm resection and AC joint capsular repair, loaded (mm) | AC displacement, 10-mm resection and AC joint capsular repair, loaded (mm) |
|---|---|---|---|---|---|
| 1 | 11 | +2 | +4 | +6 | +11 |
| 2 | 7 | +3 | +3 | +8 | +15 |
| 3 | 6 | +2 | +3 | +12 | +19 |
AC, acromioclavicular.
Reverse CA ligament reconstruction
The CA ligament was harvested from its origin on the coracoid with a sleeve of periosteum. The length of the CA ligament was measured in each specimen with specimen 1 having a CA ligament of 25 mm, specimen 2 had a CA length of 35 mm, and finally specimen 3 had a CA ligament of 45 mm in length. Thereafter, the CA ligament transfer was performed as per the surgical technique described previously.
Clinical scenario 1
B.M is a 39-year-old woman, right-hand-dominant caregiver, and current smoker. She caught a falling patient at work and felt sudden onset pain in the AC joint region and heard a loud “pop” in her shoulder. She had sustained a right grade 1 AC joint injury, which was initially managed nonoperatively with non-steroidal anti-inflammatories and a rigorous physiotherapy program. However, this failed owing to ongoing right shoulder pain. An MRI scan performed at another institution found edema of the AC joint and osteolysis of the lateral end of the clavicle, and this was managed with an arthroscopic acromioplasty and AC joint resection. Despite surgical intervention she had ongoing pain, “popping’ sensation and subjective instability of the right AC joint. She then received steroid injections and a physical therapy programme; however, when this failed to resolve her symptoms, she proceeded to an open revision of the index distal clavicle resection. Despite the revision surgery, She presented to our senior author (PCP) with ongoing AC joint pain, subjective instability and intermittent “popping” noises. Her physical examination revealed significant tenderness at the right AC joint with increased horizontal translation of the clavicle compared to the contralateral side when stressing the lateral clavicle. Figure 5 demonstrates the widely resected AC joint on standard AC joint radiographs, while Figure 6 demonstrates the significant edema in the AC joint region on preoperative MRI scan. B.M underwent a reverse CA ligament reconstruction as demonstrated by the schematic drawing in Figure 3 and the intraoperative image in Figure 7. Postoperative radiographs and MRI scan demonstrate the EndoButton fixation and the CA ligament transfer in Figure 8. Seven months postoperatively, she had a significant improvement in pain levels and reported resolution of the instability symptoms in her right AC joint.
Figure 5.

Radiograph demonstrating the widely resected AC joint of B.M.
Figure 6.

The MRI scan of B.M. demonstrating significant edema at the right AC joint. MRI, magnetic resonance imaging.
Figure 7.

The final results of the reverse CA ligament transfer. CA, coracoacromial.
Figure 8.
demonstrates the postoperative images for the reverse CA ligament reconstruction, A: post-op x-rays, B: post-operative MRI scan demonstrating the CA ligament transfer intact (∗). CA, coracoacromial.
Clinical scenario 2
C.W is a 43-year-old man, right hand dominant, fitter welder, and current smoker. Three years prior, he sustained a right grade 1 AC joint injury after falling off a stool and sustained an axial load to his elbow. After initial nonoperative treatment, he experienced ongoing pain after 18 months and underwent a right shoulder arthroscopic acromioplasty and AC joint resection at another institution. When his symptoms failed to improve postoperatively, an MRI scan was performed showing what was considered to be inadequate resection of the AC joint. Subsequently, he underwent an open revision AC joint resection 9 months after his index operation. Despite this revision surgery, he continued to experience pain and clicking in the right shoulder and was unable to return to work despite analgesia, steroid injections, and physiotherapy.
He was referred to the senior author (PCP) for review and consideration for surgical intervention. His physical examination revealed increased horizontal translation of the right clavicle compared to the left, with X-rays demonstrating a widely resected AC joint with an AC gap of 25 mm (Fig. 9). As part of the preoperative workup, an MRI scan was performed showing intact trapezoid and conoid ligaments in Figure 10. He underwent the reverse CA ligament transfer, with intraoperative images shown in Figure 11, with Videos 1 and 2 demonstrating the difference between the preoperative and postoperative horizontal instability of the clavicle. Seven months after his reverse CA ligament transfer, he experiences only mild pain, improved range of motion of the right shoulder and has been able to return to work in his previous occupation as a fitter welder.
Figure 9.
Demonstrates the widely resected AC joint in the left hand image compared with the normal AC joint in the image on the right.
Figure 10.
Preoperative MRI scan demonstrating the intact CC ligament complex in C.W. despite the widely resected AC joint. CC, coracoclavicular; MRI, magnetic resonance imaging.
Figure 11.
The forceps indicates the CA ligament, which has been passed through the bone tunnel on the distal clavicle and anchored with the endobutton demonstrated in the image. CA, coracoacromial.
Discussion
Anatomy of the AC joint
Fukuda et al5 demonstrated that the AC joint capsule provides 90% of the restraint against AP (“horizontal”) translation of the clavicle.1,6, 7, 8, 9 Any surgery on the AC joint must therefore minimize disruption to the stabilizing effect of the AC joint capsule. Several cadaveric studies have described the anatomy of the AC joint capsule with the average distance from the intra-articular surface of the clavicle to the innermost insertion of the capsule ranging from 2.3 to 3.9 mm superiorly with a width of the insertion ranging from 1.6 to 2.9 mm.3,7, 8, 9 These studies concluded that no more than 7 mm of distal clavicle should be excised to prevent iatrogenic disruption of the AC joint capsule attachments.3,7, 8, 9 Outcome studies by a number of authors have demonstrated less pain and improved functional outcomes with distal clavicle resections of <10 mm.3,9 Our findings support the evidence already available that more than 10 mm of distal clavicle resection compromises the AC joint capsule, without the possibility of subsequent adequate repair. Furthermore, an increased degree of displacement between the 5-mm and the 10-mm clavicular resections is observed in our study. This suggests that although the capsule was repaired, the entire insertion could no longer be included in the repair with this amount of bony resection, thus potentially contributing to increased instability in the horizontal plane. However, a clinically significant cutoff value for AC joint displacement in the horizontal plane during either open-shoulder surgery or cadaveric dissection has not yet been established. Some studies suggest 5 mm of translation as being clinically significant, given that this amount of translation can be demonstrated on clinical examination. Further complicating this matter is the natural horizontal laxity of the AC joint, which in some clinical and biomechanical studies has been demonstrated to be as great as 8.5-10.5 mm.2, 3, 4 Further work is therefore needed to define the degree of horizontal displacement of the clavicle resulting in clinically significant symptoms of horizontal AC joint instability.
Horizontal instability of the AC joint and the reconstructive options
AC joint instability remains a difficult problem for the upper limb surgeon. Furthermore, “horizontal” instability of the AC joint may develop after an injury to the AC capsule. Such injuries are difficult to quantify through the use of standard radiographs, thus leading to horizontal instability being under diagnosed or neglected.1 Failure to treat such instability can lead to chronic AC joint injury and poor patient-reported outcomes with respect to pain and functional abilities.6 Clinically, these patients report significant pain, clicking or subjective instability in their shoulder, as highlighted by the cases of B.M and C.W. Physical examination may demonstrate positive provocative AC joint tests such as cross-arm adduction, Paxinos test, and O’Brien’s test. However, these tests lack the sensitivity and specificity for horizontal instability of the AC joint. Tauber emphasized the importance of assessing posterior translation of the clavicle with respect to a stabilized acromion to evaluate for horizontal instability.10 Tauber determined the AC joint to be stable if there was <50% AP translation compared with the contralateral side, with the joint subluxated if >50% translation was able to be demonstrated.10
More than 60 surgical techniques are described for the reconstruction of the AC joint, thus underlining the lack of consensus regarding a gold standard approach for these injuries. Moreover, many of the reconstruction techniques were described for high-grade dislocation of the AC joint whereby the CC ligaments have been disrupted and primarily address the vertical instability of the AC joint. Increasingly the importance of horizontal stability of the clavicle is recognized, with a number of studies demonstrating that combined AC capsular reconstruction and CC ligament reconstruction result in superior patient-reported outcomes compared with CC ligament reconstruction alone.1,3
For the low-grade Rockwood injuries that fail nonoperative management, the current standard treatment is arthroscopic or open distal clavicle excision, as demonstrated with clinical scenario 1 (B.M).1 This current surgical practice reflects a poor understanding of the pathoanatomy of the clinical problem. Low-grade Rockwood injuries (I and II) result from disruption of the AC joint capsule, and instead of repairing the damaged soft tissues, this soft tissue rupture is managed with the excision of bone. Moreover, the AC joint capsule has a wide insertional footprint and further disruption of the remaining AC joint capsule through the resection of the distal clavicle compounds the AC joint instability. Therefore, for patients with Rockwood grade I and II AC joint injuries, it is the senior author’s (PCP) standard surgical practice to perform an open limited AC joint debridement with repair of the AC joint capsule onto the lateral end of the clavicle through transosseous sutures without resection of the clavicle. This would have been the preferred treatment method for patient B.M; however, by the time of her presentation to the senior author, she required a reverse CA ligament transfer to treat the horizontal instability of the clavicle.
In the second clinical scenario, iatrogenic “horizontal” instability of the AC joint can occur as a result of surgical resection of the lateral end of the clavicle for chronically painful AC joint osteoarthritis. The surgery can disrupt the AC joint capsule and excessive resection of the lateral end of the clavicle can render the AC joint capsule not repairable. Ongoing pain following such surgery can sometimes be attributed to inadequate clavicle resection leading to further resection of the lateral end of the clavicle, compounding the instability. The senior author’s surgical preference is an arthroscopic resection of the AC joint with the aim of creating a 1-cm AC joint space, by removing bone from both the acromion and lateral end of the clavicle and thereby reducing the risk of AC joint capsular disruption. In patients who have ongoing pain after adequate resection of the AC joint (1-cm gap), symptoms should not be attributed to inadequate resection, but instead, other causes should be considered.
In this cadaveric study, we described the capsular anatomy of the AC joint, created “horizontal” instability of the AC joint by excessive resection of the lateral end of the clavicle and described a novel surgical technique by a reverse CA ligament transfer as a salvage surgical option for this difficult and often unrecognized clinical problem. We presented two patients as clinical case examples who both had iatrogenic AC joint “horizontal” instability after primary and subsequent repeat resection of the AC joint. In both cases, the index surgeon failed to recognize this clinical entity. They were surgically treated with a reverse CA ligament transfer that improved their symptoms. To the best of our knowledge, we are not aware of a reverse CA ligament transfer being described for salvage reconstruction of the AC joint with iatrogenic “horizontal” instability.
There are a myriad of surgical techniques for surgical reconstruction of high-grade AC joint dislocations. Most are focused on coracoclavicular fixation. Increasingly, surgeons recognize the need to also include an AC joint reconstruction in addition to the CC reconstruction. This reverse CA ligament transfer can potentially be also used for the AC joint component to supplement a CC reconstruction.
Limitations
Of course this study has some limitations. Our study was performed on cadaver shoulders and does not account for the effect of healing after surgery. The effects of disrupting the AC joint capsule and stepwise increasing the lateral end clavicle resection were measured by static translation of the clavicle and do not take into account any active muscle-stabilizing effect. Furthermore, only a limited number of cadaver specimens were available for this study. However, this study highlights the underrecognized clinical entity of horizontal” instability of the AC joint, describes a novel surgical technique, and demonstrated the feasibility of this reverse CA ligament transfer as a salvage surgical option. This can provide a basis for future projects looking at the biomechanical properties of this AC joint reconstruction and its clinical application.
Conclusion
The “horizontal” stability of the AC joint is often forgotten, unrecognized, and must be restored when performing reconstructive surgery of the AC joint. This cadaveric study simulated this problem and describes a reverse CA ligament transfer to address “horizontal” instability of the clavicle. Additional clinical studies to determine the functional outcomes of patients treated with this method would be beneficial to further establish its beneficial effect and add to the body of literature on “horizontal” AC joint instability.
Disclaimers
Funding: No funding was disclosed by the author(s).
Conflicts of interest: The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
The Health and Disability Ethics Committee of North Shore Hospital deemed that formal ethics approval was not required for this work.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xrrt.2021.05.003
Supplementary data
Demonstrates horizontal instability of the distal clavicle prior to performing the reverse coracoacromial ligament transfer.
Demonstrates the significantly improved stability of the ACJ following the reverse coracoacromial ligament transfer.
References
- 1.Aliberti G.M., Kraeutler M.J., Trojan J.D., Mulcahey M.K. Horizontal instability of the acromioclavicular joint. A systematic review. Am J Sports Med. 2020;48:504–510. doi: 10.1177/0363546519831013. [DOI] [PubMed] [Google Scholar]
- 2.Beitzel K., Obopilwe E., Chowaniec D.M., Niver G.E., Nowak M.D., Hanypsiak B.T., et al. Biomechanical comparison of arthroscopic repairs for acromioclavicular joint instability: suture button systems without biological augmentation. Am J Sports Med. 2011;39:2218–2225. doi: 10.1177/0363546511416784. [DOI] [PubMed] [Google Scholar]
- 3.Beitzel K., Sablan N., Chowaniec D.M., Obopilwe E., Cote M.P., Arciero R.A., et al. Sequential resection of the distal clavicle and its effects on horizontal acroioclavicular joint translation. Am J Sports Med. 2012;40:681–685. doi: 10.1177/0363546511428880. [DOI] [PubMed] [Google Scholar]
- 4.Debski R.E., Parsons I.M., 3rd, Fenwick J., Vangura A. Ligament mechanics during three degree-of-freedom motion at the acromioclavicular joint. Ann Biomed Eng. 2000;28:612–618. doi: 10.1114/1.1304848. [DOI] [PubMed] [Google Scholar]
- 5.FukudaK, Craig E.V., An K.N., Cofield R.H., Chao E.Y.S. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434–440. [PubMed] [Google Scholar]
- 6.Maier D., Jaeger M., Reising K., Feucht M.J., Sudkamp N.P., Izadpanah K. Injury patterns of the acromioclavicular ligament complex in acute acromioclavicular joint dislocations: a cross-sectional, fundamental study. BMC Musculoskelet Disord. 2016;17:385. doi: 10.1186/s12891-016-1240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakazawa M., Nimura A., Mochizuki T., Koizumi M., Sato T., Akita K. The orientation and variation of the acromioclavicular ligament. An anatomic study. Am J Sports Med. 2016;44:2690–2695. doi: 10.1177/0363546516651440. [DOI] [PubMed] [Google Scholar]
- 8.Pandhi N.G., Esquivel A.O., Hanna J.D., Lemos D.W., Staron J.S., Lemos S.E. The biomechanical stability of distal clavicle excision versus symmetric acromioclavicular joint resection. Am J Sports Med. 2013;41:291–295. doi: 10.1177/0363546512469873. [DOI] [PubMed] [Google Scholar]
- 9.Stine I.A., Vangsness C.T. Analysis of the capsule and ligament insertions about the acromiocavicular joint: a cadaveric study. Arthroscopy. 2009;25:968–974. doi: 10.1016/j.arthro.2009.04.072. [DOI] [PubMed] [Google Scholar]
- 10.Tauber M., Valler D., Lichtenberg S., Magosch P., Moroder P., Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44:482–489. doi: 10.1177/0363546515615583. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demonstrates horizontal instability of the distal clavicle prior to performing the reverse coracoacromial ligament transfer.
Demonstrates the significantly improved stability of the ACJ following the reverse coracoacromial ligament transfer.








