Abstract
Tracheobronchial stenosis (TBS) in adults derives from congenital and acquired conditions, including prolonged mechanical intubation, expiratory central airway collapse, infectious or inflammatory disease, and malignancy. The most common clinical presentation is shortness of breath, recurrent infections, and chronic cough. TBS is usually diagnosed via computed tomography or bronchoscopy, with the latter doubling as a therapeutic tool. We present a case of an atypical fibrotic bridge connecting the walls of the distal trachea and fibrotic bronchial stenosis treated with electrocautery knife and balloon dilation, in an adult patient with bronchopulmonary dysplasia.
Keywords: bronchial stenosis, bronchoscopy, electrocautery knife, fibrotic bridge
An adult patient with a history of bronchopulmonary dysplasia presented symptoms of tracheobronchial stenosis. We found an unusual tracheal fibrotic bridge connecting the lateral walls of the distal trachea, with adjacent fibrotic stenosis in the left and right mainstem bronchi, treated with an electrocautery knife and balloon dilation without complications.
INTRODUCTION
Tracheobronchial stenosis (TBS) can result from several acquired or congenital conditions in adults. The most common causes are trauma due to prolonged intubation and/or tracheostomy, tracheobronchomalacia, dynamic collapse, malignancy, lung transplantation, sarcoidosis, tuberculosis, and congenital. 1 Symptomatic presentation of TBS includes coughing, wheezing, stridor dyspnea, or recurrent respiratory infections and is diagnosed by chest imaging, pulmonary function tests, and direct visualization via bronchoscopy. 1 , 2 Management will largely depend on the cause, location, and extension of the stenosis, comprising bronchoscopic or surgical approaches. 1 , 2 In our case, TBS was due to a rare fibrotic bridge in the distal trachea and concurrent left and right mainstem bronchi stenosis, treated with electrocautery and balloon dilation.
CASE REPORT
A 33‐year‐old female with a past medical history of premature birth at 21 weeks, bronchopulmonary dysplasia (BPD), multiple pneumothoraces, Nissen fundoplication, patent ductus arteriosus status‐post ligation, presented for evaluation of TBS. Since 2023, the patient had had three episodes of pneumonia requiring hospitalization. She presented with occasional coughing. There were concerns that the Nissen fundoplication had failed, leading to subsequent airway damage by regurgitation and aspiration; therefore, she started proton pump inhibitor therapy with improved epigastric symptoms.
Prior pulmonary function testing demonstrated severe obstruction and air trapping. Chest computed tomography (CT) revealed significant air trapping noted bilaterally and moderate narrowing of the distal trachea with stenosis of the proximal mainstem bronchi more severe on the right than the left, likely contributing to persistent infections. An outside bronchoscopy showed significant airway narrowing in the right mainstem bronchus (RMB), for which airway dilation was recommended, and we consulted with our service for another opinion.
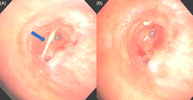
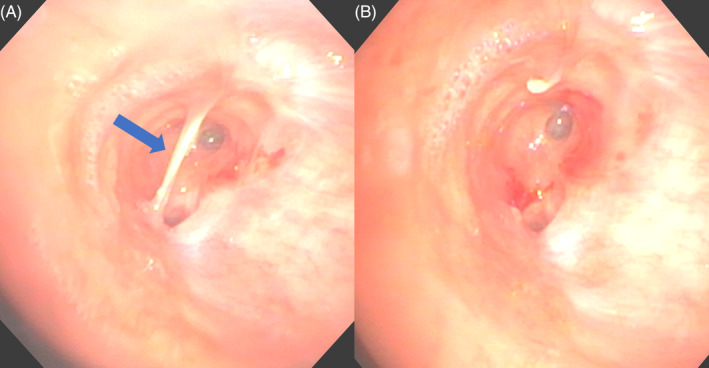
Due to worsening symptoms and increased oxygen requirements, we performed the bronchoscopic evaluation. Through flexible bronchoscopy, we visualized a fibrotic bridge connecting the lateral walls of the distal trachea (Figure 1A and Video 1) and used an electrocautery hybrid knife to cut through the bridge (Figure 1B and Video 1). We noted fibrotic bronchial stenosis at the left mainstem bronchus (LMB) (Figure 2A) and complete RMB occlusion (Figure 2B). Electrocautery cuts and balloon dilation were performed on the LMB and RMB (Figure 2C, D). No immediate complications were noted after the procedure. At the one‐month follow‐up, the patient reported improvement in exertional shortness of breath and exercise capacity and was reevaluated via bronchoscopy, confirming distal tracheal patency with absence of the previous fibrotic bridge.
FIGURE 1.
(A) Bronchoscopic view of fibrotic bridge connecting lateral walls at the level of the distal trachea (blue arrow). (B) Post‐electrocautery hybrid knife cut of the fibrotic bridge revealing a patent trachea and right mainstem bronchus occlusion.
VIDEO 1.
Flexible bronchoscopy view of fibrotic bridge connecting the lateral walls at the level of the distal trachea (at 3 s). The flexible bronchoscope is manoeuvred past the bridge to visualize left mainstem stenosis (at 16 s) and complete occlusion of the right mainstem bronchus (at 20 s). Electrocautery hybrid knife is used to cut the fibrotic bridge without complications (at 28 s).
FIGURE 2.
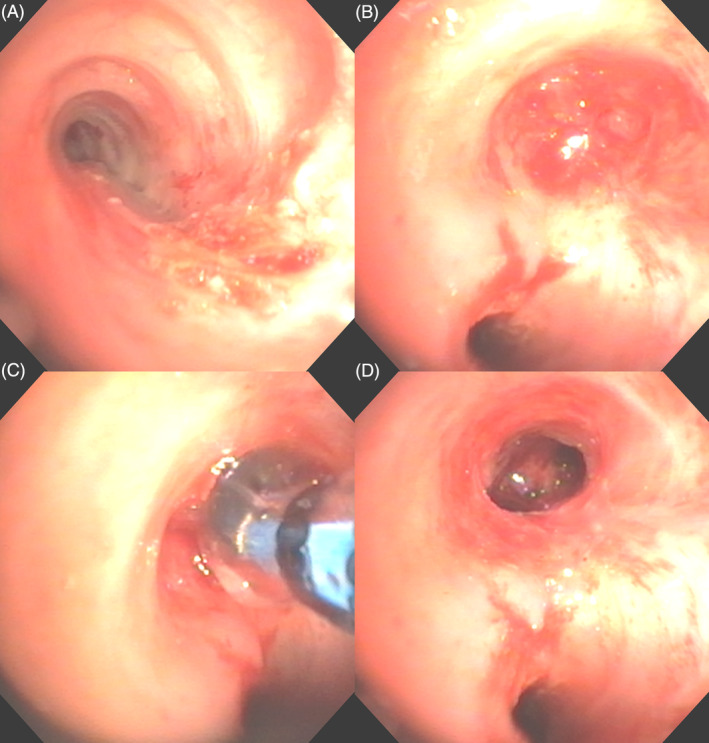
(A) Bronchoscopic view of left mainstem bronchus stenosis. (B) Bronchoscopic view of right mainstem bronchus complete occlusion. (C) Balloon dilation for re‐expansion of right mainstem bronchus. (D) Bronchoscopic view post‐electrocautery hybrid knife cuts and balloon dilation of patent left and right mainstem bronchi.
DISCUSSION
TBS is the narrowing of the tracheobronchial tree. It may be localized or diffuse, congenital, or acquired, caused by benign or malignant disorders, and exhibit various symptoms such as dyspnea, wheezing, or stridor in patients with severe stenosis. Depending on the level of TBS, obstruction can result in long‐term pulmonary issues, such as recurrent pneumonia, emphysema, or atelectasis. 1 , 2 Our case was unique as a fibrous bridge was encountered in the distal trachea, with fibrous stenosis in the RMB and LMB. This kind of structure has been scarcely reported in the literature, with only one other case report describing similar tracheal fibrotic bridges secondary to prolonged intubation and tracheostomy post‐COVID‐19 infection. 3
The most common cause of iatrogenic TBS is prolonged intubation and tracheostomy, with rates likely increasing after the COVID‐19 pandemic. 3 Infectious diseases such as tuberculosis and systemic conditions like relapsing polychondritis, granulomatosis, and sarcoidosis frequently result in TBS. 1 TBS has been reported in patients with BPD, as in our case, though the stenosis is caused by artificial ventilation and suctioning, not the actual disease process of BPD. 4 , 5 Gastroesophageal reflux disease has also been shown to be a cause of the development of tracheal and bronchial stenosis, which can also occur late after corrective surgery. 6
Multiple modalities are present to diagnose TBS, including chest CT, magnetic resonance imaging, and endoscopy, the gold standard. 1 , 2 Bronchoscopy also doubles as a therapeutic tool to relieve the obstruction. Surgery for TBS is usually reserved for more advanced cases and, most commonly, bronchogenic carcinomas. 1 Bronchoscopy allows for balloon dilatation, ablative techniques, electrocautery, argon plasma coagulation, laser therapy, and airway stenting, all of which are utilized for relieving the obstruction causing stenosis. 2 In our case, we used electrocautery to cut through the fibrotic bridge in the distal trachea and fibrotic bronchial stenosis in LMB and RMB, as well as balloon dilation, to reexpand the airway, which resulted in immediate relief to the patient in symptoms and function.
In conclusion, fibrous bridges are rarely encountered as a cause for TBS and our experience of this single case indicates that they can be effectively treated with bronchoscopic interventions providing immediate relief.
AUTHOR CONTRIBUTIONS
Ishaq J. Wadiwala was responsible for writing the main draft and patient data collection. Alejandra Yu Lee‐Mateus and Bakr Alhayek revised and edited the manuscript. David Abia‐Trujillo, Ryan Chadha and Britney N. Hazelett were involved in manuscript review, and Sebastian Fernandez‐Bussy was responsible for manuscript review and scientific checking.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICS STATEMENT
The authors declare that appropriate written informed consent was obtained for the publication of this manuscript and accompanying images.
Wadiwala IJ, Yu Lee‐Mateus A, Alhayek B, Abia‐Trujillo D, Chadha R, Hazelett BN, et al. Atypical distal tracheal fibrous bridge and bronchial stenosis in an adult patient with bronchopulmonary dysplasia. Respirology Case Reports. 2023;11:e01203. 10.1002/rcr2.1203
Associate Editor: Semra Bilaceroglu
DATA AVAILABILITY STATEMENT
Data sharing not applicable‐no new data generated.
REFERENCES
- 1. Puchalski J, Musani AI. Tracheobronchial stenosis: causes and advances in management. Clin Chest Med. 2013;34:557–567. [DOI] [PubMed] [Google Scholar]
- 2. Pasick LJ, Anis MM, Rosow DE. An updated review of subglottic stenosis: etiology, evaluation, and management. Curr Pulmonol Rep. 2022;11:29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zuccatosta L, Zamacona BR, Porcarelli F, Mei F, Gonnelli F, Gasparini S, et al. Case report: tracheal stenosis due to fibrotic bridges in a post‐tracheostomy COVID‐19 patient. Front Med. 2022;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bailey C, Kattwinkel J, Teja K, Buckley T. Shallow versus deep endotracheal suctioning in young rabbits: pathologic effects on the tracheobronchial wall. Pediatrics. 1988;82:746–751. [PubMed] [Google Scholar]
- 5. Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir Med. 2017;132:170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cardoso PFG, Minamoto H, Bibas BJ, Pego‐Fernandes PM. Impact of gastroesophageal reflux in the pathogenesis of tracheal stenosis. Transl Cancer Res. 2020;9:2123–2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable‐no new data generated.


