Abstract
Introduction
Although still rare, pulmonary embolism (PE) in children has been increasing over the years. Data regarding this group of patients are still sparse, which contributes to the lack of standardized prophylaxis protocols and the misdiagnosis. This study aimed to determine the incidence of pediatric PE at a Brazilian tertiary hospital, describe clinical characteristics and identify possible risk factors. We also analyzed the diagnosis and management of PE.
Methods
This was a retrospective review of tertiary Brazilian single-center data of all pediatric patients (0 – 18 years) with acute PE, diagnosed radiologically, from September 2009 to May 2019.
Results
The incidence of PE was 3.3 cases per 10,000 hospitalized children. All the twenty-three cases had some risk factor identified and sixteen of them (69.5%) had more than one risk factor. The most important were central venous catheter (39.1%), malignancy (34.8%) and recent surgery (34.8%). Among the children with identifiable symptoms (69.5%), the most common was dyspnea (56.2%). Only one patient did not receive antithrombotic therapy because of the high bleeding risk and most patients (70.6%) were treated for 3 to 6 months. Among the nineteen patients alive at the end of the six-month follow-up, ten (52.6%) repeated the PE image control. Seven of them (70.0%) had complete or partial resolution of the thrombosis and none had worsening images.
Conclusion
Our lower incidence than that of the current literature may reflect underdiagnosis due to low suspicion of PE. At least one risk factor was identified in all patients, which emphasizes the importance of increasing awareness of high-risk children.
Keywords: Child, Adolescent, Pulmonary embolism, Thromboembolism
Introduction
Pulmonary Embolism (PE) is a potentially life-threatening condition still rare in the pediatric population, but the exact incidence is not known.1 The annual incidence of pediatric PE from first analyses of the Canadian registry in 1994 was 0.86 per 10,000 hospital admissions, while the Pediatric Health Information System database from the United States showed rates up to 9.22 per 10,000 admisisons2, 3, 4 in 2019. Among all the children in the community, PE incidences range from 0.14 to 0.90 per 100,000 per year.5,6
The different incidences reported reflect diagnostic limitations, PE clinically silent and biased population at tertiary centers.3,7 Moreover, the incidence of PE is steadily increasing due to detection of previously undiagnosed patients, as well as the actual increase of the pediatric PE occurrence as a consequence of a higher number of patients at risk for thromboembolic events, such as longer survival of children with critical medical conditions and increased use of the central venous catheter.1,8, 9, 10
The PE characteristics in children are much different from those in adults, not only in terms of incidence, but also of predisposal factors, pathophysiology, clinical presentation and management strategies.7 The PE is a consequence of patient-related and setting-related risk factors, which are usually permanent and temporary conditions, respectively.11 In children, PE is rarely unprovoked and the main risk factors are immobilization, infection, presence of the central venous catheter, recent surgery/trauma, malignancy, nephrotic syndrome, hormonal contraception/pregnancy and obesity.11,12
The underdiagnosis of pediatric PE is evidenced by incidences up to 4.2% in autopsy reports, which is partially attributed to non-specific symptoms masked by underlying conditions.3,13 Additionally, the clinical findings mimic other childhood diseases that are more common, such as pneumonia.14
The combination of symptoms, clinical findings and risk factors provide a pre-test probability of PE in the adult population.11 In adults, when combined with the D-dimer results, the clinical probability score is safer to exclude PE without the need for image tests.14 Several scores already exist as useful tools for diagnosis, but none of them were approved for children.15
The delay or missing PE diagnosis may lead to serious consequences to the child. Overall mortality ranges from 10% to 24%, either attributed to underlying conditions or directly to PE, and morbidity rates are still unknown.2,3,5
Due to the lack of pediatric PE studies, the diagnostic management of a child with suspected PE and the treatment guidelines are extrapolated from the knowledge gained from adult patients.16 A recent multinational survey confirmed the variability in the management of PE, even among academic tertiary centers.17
In Brazil, there is still no knowledge regarding pediatric venous thromboembolism (VTE) or PE epidemiology and clinical characteristics.18 This article reviews the incidence, clinical characteristics, diagnostic workup, risk factors, treatment and outcome of PE in pediatric patients admitted to care at a single Brazilian tertiary center.
Methods
Subsequent to the Institutional Review Board approval (CAPPesq 3.761.519/Dec 2019), medical records of pediatric patients diagnosed with acute PE at the Instituto da Criança do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (ICr-HCFMUSP) were evaluated. Patient selection was achieved by searching for the discharge diagnostic code I26 (pulmonary embolism) and/or I82 (other venous embolism and thrombosis (primary or secondary diagnosis)) in a database of all patients admitted to the ICr-HCFMUSP. Electronic medical records regarding hospitalization and outpatient follow-up were then reviewed. Then we only included patients with confirmed PE.
The study included patients from 0 to 18 years of age and radiologically confirmed acute PE between September 2009 to May 2019. Over this period, 70,305 pediatric patients were hospitalized. The incidence of PE was then calculated using the ratio between the confirmed acute PEs and the number of pediatric admissions. The PE diagnosis was established by computed tomographic pulmonary angiography (CTPA) or echocardiography, when the CTPA was not possible. The exclusion criteria were the absence of radiological or pathological PE confirmation and non-thromboembolic pulmonary embolism.
At the time of the diagnosis, the main data analyzed were demographic characteristics, risk factors for thromboembolic events, presentation symptoms, the D-dimer level and imaging modality. The antithrombotic therapy, duration of treatment and outcome after six months of follow-up were evaluated.
Results
Our study evaluated 23 patients with PE during a period of 10 years, with an incidence of 3.3 per 10,000 admissions, sixteen of them (69.6%) hospitalized at the time of initial symptoms.
Demographic and clinical characteristics of patients are shown in Table 1. The median age was 11 years (2 days - 17 years) and twelve patients (52.2%) were adolescents (> 10 years).
Table 1.
Characteristics of pediatric patients with PE.
| Characteristics (n = 23) | n (%) |
|---|---|
| Demographics | |
| Age | |
| 2 days – 17 years | 23 (100) |
| < 1 year | 3 (13) |
| 1 – 10 years | 8 (34.8) |
| > 10 years | 12 (52.2) |
| Male sex | 12 (52.2) |
| Setting | |
| Inpatient | 16 (69.6) |
| Outpatient | 7 (30.4) |
| Risk factors | |
| Central venous catheter | 9 (39.2) |
| Malignancy | 8 (34.8) |
| Recent surgery | 8 (34.8) |
| Infection | 7 (30.4) |
| Drugs¹ | 5 (21.7) |
| Nephrotic Syndrome | 3 (13.0) |
| Congenital heart disease | 2 (8.7) |
| Trauma | 1 (4.3) |
| Polycythemia | 1 (4.3) |
| Splenectomy | 1 (4.3) |
| Symptoms/signs | |
| Dyspnea | 9 (39.1) |
| Chest pain | 8 (34.8) |
| Hypoxemia | 7 (30.4) |
| Cough | 1 (4.3) |
Corticosteroids or asparaginase.
All the twenty-three cases had some risk factor identified. The most important were the central venous catheter (39.1%), malignancy (34.8%) and recent surgery (34.8%). Use of prothrombotic medications, such as corticosteroids and asparaginase, were identified in five cases, although none of them included an oral contraceptive. More than one risk factor was present in sixteen of the children (69.5%).
Five patients were asymptomatic and they are described in Table 2. All of them had comorbidities and CTPAs were performed for other reasons. It was not possible to evaluate symptoms in two patients: one due to the lack of data and the other to a critical condition with confusion factors at the time of the PE diagnosis.
Table 2.
Asymptomatic patients.
| Patient | Age (years) | Setting | Underlying disease | Risk factors | Reason for imaging | Anticoagulation therapy | Treatment duration | Radiological follow-up (6 months) |
|---|---|---|---|---|---|---|---|---|
| #1 | 14 | Inpatient (20 days) | Metastatic osteosarcoma | Malignancy | Tumor staging | Enoxaparin, 1 mg/kg/dose q12h | 10 months | Chronic PE |
| #2 | 2 | Inpatient (22 days) | T-cell acute lymphoblastic leukemia | Malignancy + Drug¹ + Infection + CVC² | Fever of unknown origin | Enoxaparin, 1 mg/kg/dose q12h | 6 months | Chronic PE |
| #3 | 15 | Outpatient | Metastatic Ewing sarcoma | Malignancy | Tumor staging | Enoxaparin, 1.2 mg/kg/dose q12h | 3 months | Complete resolution |
| #4 | 2 | Inpatient (33 days) | Double outlet right ventricle + Interatrial and interventricular communication | Congenital heart disease + Recent surgery + CVC | Postoperative imaging control | Enoxaparin, 1.4 mg/kg/dose q12h | Not reported | Complete resolution |
| #5 | 3 | Inpatient (8 days) | Right adrenocortical carcinoma | Malignancy + Recent surgery | Postoperative imaging control | Enoxaparin, 1 mg/kg/dose q12h | 3 months | Complete resolution |
Asparaginase;
Central venous catheter.
Among the sixteen children (69.5%) with identifiable symptoms/signs, most of them presented dyspnea (56.2%) and there were no reports of syncope or hemoptysis. The median time between initial symptoms and diagnosis was 1 day (0 - 11 days). Only six patients (26%) were admitted due to symptoms attributable to PE. The other ten symptomatic children developed symptoms during hospitalization.
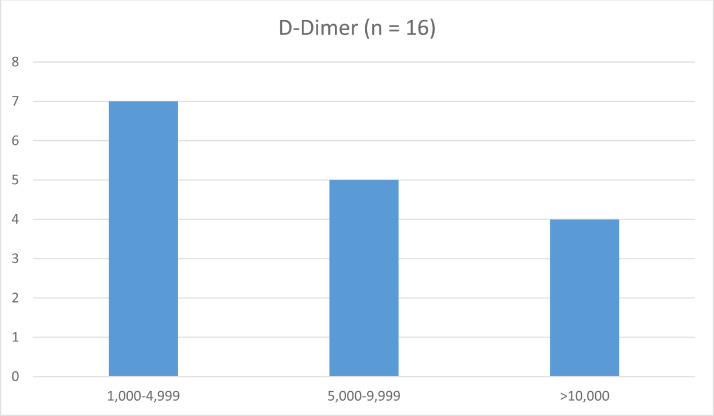
From the sixteen patients (69.5%) who had their D-dimer measured at diagnosis, all had levels higher than 1,000 ng/ml (laboratory reference: < 500 ng/ml) (Figure 1).
Figure 1.
D-dimer level at the time of PE diagnosis.
The imaging modality of choice was the CTPA. An alternative imaging technique (echocardiography) was used in two patients (8.7%). One of them was a newborn in the second day of life and the exam revealed a thrombus measuring 9.8 × 3.4mm, leading to the partial occlusion (70%) of the left pulmonary artery. The other child was a hemodynamically unstable infant with sepsis and cardiovascular failure. The echocardiography evidenced a thrombus measuring 9.0 × 3.5mm at the bifurcation of the pulmonary artery and mild pulmonary hypertension.
Only one patient did not receive antithrombotic therapy because of a high bleeding risk. In four of the patients treated (18.2%), the therapy was initiated with unfractionated heparin (UFH) and continued with low molecular weight heparin (LMWH). Eighteen (78.3%) were treated with LMWH from the beginning of the treatment. Thrombolysis was not performed in any of the cases.
Among 22 patients who received antithrombotic therapy, five patients were lost to the follow-up and twelve of the remaining seventeen (70.6%) received anticoagulation therapy for 3 to 6 months (median of 6 months). Two patients had the treatment interrupted because of bleeding complications: one hemothorax (day 9 of treatment) and one fatal intracranial hemorrhage (day 30 of treatment).
Four patients (17.4%) died. One died due to cardiorespiratory failure secondary to PE, which was diagnosed after 11 days from the presentation symptoms, and was the only case not treated because of the high bleeding risk. Another child died because of intracranial hemorrhage 30 days after anticoagulation was initiated. Two deaths were due to unrelated causes (sepsis and malignancy).
Among the nineteen patients alive at the end of the six-month follow-up, ten (52.6%) repeated the PE image control. Seven of them (70.0%) had complete or partial resolution of the thrombosis and none had worsening images.
Discussion
One of the main limitations in increasing knowledge on pediatric PE is its low incidence. Nevertheless, we obtained a considerable number of patients from a pediatric reference center in Brazil, which is comparable to a recent Portuguese study.19 Our resulting incidence of 3.3 per 10,000 hospitalized children was previously reported by Biss et al. (2008).3 Multicenter data from the United States published by Rajpurkar et al. (2019) are higher and ranged from 5.12 - 9.22 per 10,000 admissions,4 similar to recent findings from a Portuguese center.19 One possible cause for our lower incidence is the still incipient knowledge on pediatric VTE and PE in Brazil.
The peak of incidence of PE was in adolescence, however the classical bimodal distribution (< 1 year of age and adolescence) was not found in our study.6 The low incidence of PE in children < 1 year and, more specifically, newborns is probably due to the existence of a specific neonatal center at the HCFMUSP hospital complex.
Although we found similar frequencies of PE between male and female patients, the finding was different in the adolescent group. Only four of the 12 adolescents were female (33.3%) and none of them reported the use of a hormonal contraceptive, an important risk factor for PE, which has been extensively described.11,12 The fact that most of our patients were hospitalized and had underlying diseases could justify this lower percentage of female adolescents, in comparison to the Portuguese study.19
In contrast to the adult population, PE is rarely unprovoked in children and adolescents. Our study identified at least one risk factor in all patients and the presence of the central venous catheter was the most common, found in nine children (39.3%). Previous reports have already implicated the central venous catheter as the most important isolated risk factor associated with thromboembolic events in childhood2,5 and its increasing implication with pediatric PE, due to the requirement for the administration of new drugs or prolonged parenteral nutrition.20
Malignancy, nephrotic syndrome and congenital heart disease are the main comorbidities associated with PE in children.3 Malignancy and nephrotic syndrome were found in eight (34.8%) and three (13.0%) of our patients, respectively. All the patients with nephrotic syndrome were at home at the time of the first symptoms of PE. They were diagnosed on the same day or 1 day after the initial symptoms, which demonstrates a high clinical suspicion of PE in this condition. Congenital heart disease was present in only two patients (8.7%) and this may be justified by the existence of a specific heart hospital at the HCFMUSP hospital complex at the ICr.
The PE following trauma or recent surgery (previous 4 weeks) was diagnosed in nine patients (39.3%). These are recognized predictors of the PE diagnosis in adults and children.21 Two or more risk factors were identified in the majority of patients (69.5%), which emphasizes the awareness of conditions involving nonspecific symptoms.
Given the lack of definitive recommendations regarding thrombophilia investigation, our center performs these tests only in certain clinical situations, such as unprovoked PE and a positive family history of VTE and/or thrombophilia. Therefore, this variable was not evaluated in our study.22,23
Incidental PE was included in our study due to two main reasons. First, to compare our data with other studies that also include them and second, because there is no consensus regarding the management of asymptomatic PE, most of the clinicians do not differentiate between symptomatic and asymptomatic PE.17
Although high levels of D-dimer were observed in all of our patients who were tested, the role of D-dimer testing remains unknown in the diagnosis of PE in children. The test is not specific and can be a false positive in the presence of severe underlying conditions, common in tertiary centers like ours.15 Despite this, prospective studies are necessary to elucidate the role of D-dimer and the development of diagnostic prediction models using this test in children and adolescents.12
Current imaging techniques to establish the diagnosis of PE in children are the ventilation/perfusion scan (V/Q scan) and CTPA. They replaced the historically gold-standard pulmonary angiograph, which was too invasive and expensive. The V/Q scan is a safe method, which has been used for years. However, it requires the cooperation of the patient (often children older than 5 - 7 years) and the findings are nonspecific to the PE. The V/Q scan was not performed in any of our patients. The CTPA is now the preferred imaging modality because of the high sensibility and specificity, in addition to the possibility of the evaluation of parenchymal and mediastinal structures.24 The CTPA was not performed in only two of our patients due to technical difficulties.
The most common initial antithrombotic therapy for PE is the UFH and LMWH. The UFH is the preferable drug if the patient has a high risk for bleeding or presents hemodynamic instability because of the advantages of the short half-life and availability of a reversal agent.25
The optimal duration of therapy in PE has not been established yet and ranges mostly from 3 to 6 months.26,27 The American Society of Hematology (ASH) guideline published in 2018 recommends anticoagulation for 3 months or less in PE if the provoking factor has resolved. The exact time of treatment was not defined.28
Severe bleeding occurred in 9.1% of the patients and both of these children were receiving LMWH, which is often associated with a lower risk of bleeding (2.9 - 5%).29 The first patient had the diagnosis of metastatic neoplasm. He had been treated with LMWH for 30 days and the laboratory test evidenced appropriate anticoagulation at the time of bleeding (intracranial fatal hemorrhage). The second patient had infective endocarditis and presented with evidence of supra-therapeutic anticoagulation after nine days of LMWH, when the drug was discontinued. The next day, he was diagnosed with hemothorax.
Overall mortality was 17.4%, although in only one patient (4.3%) death was related to PE and in another one (4.3%), a hemorrhagic complication of anticoagulation. Current data on morbidity and mortality varies among studies. Biss et al. (2008) found similar incidences regarding overall mortality (21.4%), deaths directly related to PE (8.9%) and hemorrhagic complication (3.6%).3 Portuguese data from Lopes de Bragança et al. (2021) are even more similar to ours: overall mortality was 17.3% and PE-related mortality was 6.9%.19
Despite recent data evidence having increased pediatric venous thromboembolism rates, including PE, there is no evidence on the efficacy of thrombosis prophylaxis due to the lack of randomized clinical trials. Most of the published guidelines focus on hospitalized adolescents and present variable risk stratification.30,31 The CHAT (The Children's Hospital-Acquired Thrombosis) project is a multicenter registry of pediatric hospital-acquired thromboembolism to evaluate the presence of risk factors. The second phase of the study was published in 2020 and used the database from CHAT to retrospectively validate risk assessment models identified from a previous review. An independent risk assessment model will be prospectively validated (third phase) to evaluate the safety and efficacy of thromboprophylaxis.32,33
Conclusion
To our knowledge, this is the first Brazilian report on pediatric PE. Previous studies are from developed countries, mostly the United States and Canada, and we still do not know if these data can be extrapolated to distinct populations. Our data are comparable to some large centers, regarding time to diagnosis, risk factors and complication rates due to PE or anticoagulation treatment. However, recent studies have reported increasing rates of PE that are not consistent with our data and we should be concerned about misdiagnosis in our population due to the low index of suspicion and diagnostic limitations.
Retrospective analysis from a single center is the main limitation of the present study. We probably missed some cases due to the incorrect completion of the discharge document, lacking the ICD code for PE, and this can be another explanation for our lower incidence. The existence of a specific heart center and a neonatal center at the HCFMUSP hospital complex probably justifies the underrepresentation of children with congenital heart disease and newborns diagnosed with PE, respectively.
Our hospital is a national reference center with multiple pediatric specialties and this is important to increase the external validity of this study at other reference hospitals. However, our findings probably cannot be extrapolated to all pediatric centers due to the biased population of a tertiary hospital.
The knowledge about our epidemiological and clinical data is the first step towards improving the assistance for the children with PE in Brazil. In addition, even single center studies including distinct populations like ours may contribute to form the basis for prospective and multicenter trials due to the low worldwide number of cases. These studies are needed to answer questions mainly related to pre-test probability scores for the diagnosis, prophylaxis and ideal management of PE in children and adolescents.
Conflicts of interest
None.
References
- 1.Rajpurkar M, Warrier I, Chitlur M, Sabo C, Frey MJ, Hollon W, et al. Pulmonary embolism-experience at a single children's hospital. Thromb Res. 2007;119(6):699–703. doi: 10.1016/j.thromres.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Andrew M, David M, Adams M, Ali K, Anderson R, Barnard D, et al. Venous thromboembolic complications (VTE) in children: first analyses of the Canadian Registry of VTE. Blood. 1994;83(5):1251–1257. [PubMed] [Google Scholar]
- 3.Biss TT, Brandão LR, Kahr WH, Chan AK, Williams S. Clinical features and outcome of pulmonary embolism in children. Br J Haematol. 2008;142:808–818. doi: 10.1111/j.1365-2141.2008.07243.x. [DOI] [PubMed] [Google Scholar]
- 4.Rajpurkar M, Huang Y, Raffini L. Additional analysis of pediatric pulmonary embolism using the Pediatric Health Information System database. Blood Adv. 2019;3(17) doi: 10.1182/bloodadvances.2019000071. 2604-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Ommen CH, Heijboer H, Buller HR, Hirasing RA, Heijmans HAS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in the Netherlands. J Pediatr. 2001;139(5):676–681. doi: 10.1067/mpd.2001.118192. [DOI] [PubMed] [Google Scholar]
- 6.Stein PD, Kayali F, Olson RE. Incidence of venous thromboembolism in infants and children: data from the National Hospital Discharge Survey. J Pediatr. 2004;145(4):563–565. doi: 10.1016/j.jpeds.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 7.Ramiz S, Rajpurkar M. Pulmonary embolism in children. Pediatr Clin N Am. 2018;65:495–507. doi: 10.1016/j.pcl.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Raffini L, Huang Y-S, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children's hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124(4):1001–1008. doi: 10.1542/peds.2009-0768. [DOI] [PubMed] [Google Scholar]
- 9.Byard RW. Fatal embolic events in childhood. J Forensic Leg Med. 2013;20:1–5. doi: 10.1016/j.jflm.2012.04.036. [DOI] [PubMed] [Google Scholar]
- 10.Patocka C, Nemeth J. Pulmonary embolism in pediatrics. J Emerg Med. 2012;42:105–116. doi: 10.1016/j.jemermed.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing G-J, Harjola V-P, et al. ESC Scientific Document Group, 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC) Eur Heart J. 2019;00:1–61. [Google Scholar]
- 12.Biss TT, Rajpurkar M, Williams S, van Ommen CH, Chan AKC, Goldenberg N. Recommendations for future research in relation to pediatric pulmonary embolism: communication from the SSC of the ISTH. J Thromb Haemost. 2017;16:405–408. doi: 10.1111/jth.13902. [DOI] [PubMed] [Google Scholar]
- 13.Dijk FN, Curtin J, Lord D, Fitzgerald DA. Pulmonary embolism in children. Paediatr Respir Rev. 2012;13(2):112–122. doi: 10.1016/j.prrv.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83:416–420. [PubMed] [Google Scholar]
- 15.Biss TT, Brandão LR, Kahr WH, Chan AK, Williams S. Clinical probability score and D-dimer estimation lack utility in the diagnosis of childhood pulmonary embolism. J Thromb Haemost. 2009;7:1633–1638. doi: 10.1111/j.1538-7836.2009.03572.x. [DOI] [PubMed] [Google Scholar]
- 16.Van Ommen CH, Peters M. Acute pulmonary embolism in childhood. Thromb Res. 2006;118:13–25. doi: 10.1016/j.thromres.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Rajpurkar M, Williams S, Goldenberg NA, Van Ommen CH, Chan AKC, Thomas R, et al. Results of a multinational survey of diagnostic and management practices of thromboembolic pulmonary embolism in children. Thromb Res. 2019;183:98–105. doi: 10.1016/j.thromres.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Mello TT, Carneiro JDA, Mello GA, Bizzacchi JMA. Venous thromboembolism in childhood: where is Brazil after 20 years? Hematol Transfus Cell Ther. 2020;42(1):62–69. doi: 10.1016/j.htct.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopes de Bragança R, Gorito V, Cibele DG, Gonçalves LR, Ribeiro A, Baptista MJ, et al. Pulmonary embolism in pediatric age: A retrospective study from a tertiary center. Pediatr Pulmonol. 2021;56(8):2751–2760. doi: 10.1002/ppul.25527. [DOI] [PubMed] [Google Scholar]
- 20.Navanandan N, Stein J, Mistry R. Pulmonary embolism in children. Pediatr Emer Care. 2019;35:143–153. doi: 10.1097/PEC.0000000000001730. [DOI] [PubMed] [Google Scholar]
- 21.Hennelly KE, Ellison AM, Neuman MI, Kline JA. Clinical variables that increase the probability of pulmonary embolism diagnosis in symptomatic children. Res Pract Thromb Haemost. 2020;4:124–130. doi: 10.1002/rth2.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Ommen CH, Nowak-Göttl U. Inherited thrombophilia in pediatric venous thromboembolic disease: why and who to test. Front Pediatr. 2017;5:50. doi: 10.3389/fped.2017.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davila J. Transfusion Medicine and Hemostasis. Elsevier; 2019. Thrombophilia testing in the pediatric population; pp. 875–879. [Google Scholar]
- 24.Victoria T, Mong A, Altes T, Jawad AF, Hernandez A, Gonzalez L, et al. Evaluation of pulmonary embolism in a pediatric population with high suspicion. Pediatr Radiol. 2009;39:35–41. doi: 10.1007/s00247-008-1037-0. [DOI] [PubMed] [Google Scholar]
- 25.Zaidi AU, Hutchins KK, Rajpurkar M. Pulmonary embolism in children. Front Pediatr. 2017;5:170. doi: 10.3389/fped.2017.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buck JR, Connors RH, Coon WW, Weintraub WH, Wesley JR, Coran AG. Pulmonary embolism in children. J Pediatr Surg. 1981;16(3):385–391. doi: 10.1016/s0022-3468(81)80700-2. [DOI] [PubMed] [Google Scholar]
- 27.Hancock H, Wang M, Gist K, Gibson E, Myamoto S, Mourani P, et al. Cardiac findings and long-term thromboembolic outcomes following pulmonary embolism in children: a combined retrospective-prospective inception cohort study. Cardiol Young. 2013;23(3):344–352. doi: 10.1017/S1047951112001126. [DOI] [PubMed] [Google Scholar]
- 28.Monagle P, Cuello CA, Augustine C, Bonduel M, Brandão LR, Capman T, et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism. Blood Adv. 2018;2(22):3292–3316. doi: 10.1182/bloodadvances.2018024786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radulescu V. Anticoagulation therapy in children. Semin Thromb Hemost. 2017;43:877–885. doi: 10.1055/s-0036-1598004. [DOI] [PubMed] [Google Scholar]
- 30.Faustino EV, Raffini LJ. Prevention of hospital-acquired venous thromboembolism in children: a review of published guidelines. Front Pediatr. 2017;5:9. doi: 10.3389/fped.2017.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petty JK. Venous thromboembolism prophylaxis in the pediatric trauma patient. Semin Pediatr Surg. 2017;26(1):14–20. doi: 10.1053/j.sempedsurg.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Jaffray J, Mahajerin A, Young G, Goldenberg N, Ji L, Sposto R, et al. A multi-institutional registry of pediatric hospital-acquired thrombosis cases: The Children's Hospital-Acquired Thrombosis (CHAT) project. Thromb Res. 2018;161:67–72. doi: 10.1016/j.thromres.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 33.Mahajerin A, Jaffray J, Branchford B, Stillings M, Krava E, Young G, et al. Comparative validation study of risk assessment models for pediatric hospital-acquired venous thromboembolism. J Thromb Haemost. 2020;18:633–641. doi: 10.1111/jth.14697. [DOI] [PubMed] [Google Scholar]