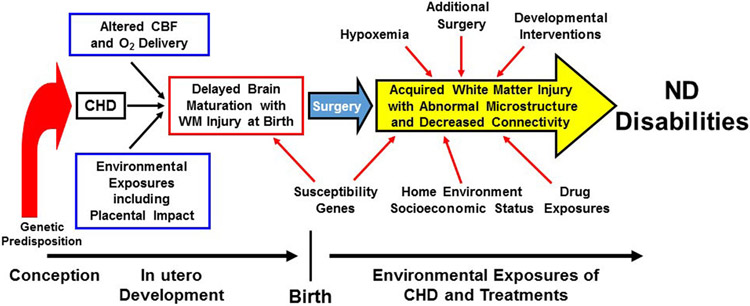
Figure 1.
Risk Factors for Neurological and Neurodevelopmental Abnormalities. Schematic representation of prenatal, perioperative, and social/environmental factors that contribute to neurodevelopmental disabilities in CHD. Prenatally, abnormal cardiac anatomy can alter blood flow and oxygenation to the developing brain, leading to impaired brain development. Concurrently, other pregnancy exposures including abnormal placental development and function and parental well-being can also have a negative impact on the brain. Genetic disruption of brain development may also occur via underlying genetics syndromes or pathogenic variants. Susceptibility genes (i.e., apolipoprotein E ε2) can further contribute to postoperative neurodevelopmental deficits. A variety of physiologic/intensive care exposures, such as hypoxemia, additional surgery, and drug exposure are important predictors in the neurocritical care arena. Finally, home environment and socioeconomic status can have a positive or negative influence, depending on the infant’s environment, whereas developmental care interventions that begin in the intensive care unit and continue after discharge may have neurodevelopmental benefit. CBF, cerebral blood flow; ND, neurodevelopment; WM, white matter. Adapted with permission from J. William Gaynor.