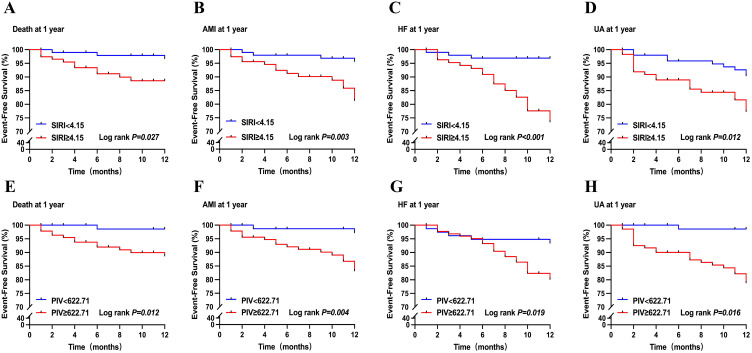
Figure 7.
Kaplan–Meier survival analysis. (A). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher mortality rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (B). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher new-onset nonfatal acute myocardial infarction (AMI) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (C). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher congestive heart failure (HF) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (D). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher revascularization in unstable angina (UA) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (E). Patients with a high PIV (PIV ≥ 622.71) had a much higher mortality rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (F). Patients with a high PIV (PIV ≥ 622.71) had a much higher new-onset nonfatal acute myocardial infarction (AMI) rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (G). Patients with a high PIV (PIV ≥ 622.71) had a much higher congestive heart failure (HF) rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (H). Patients with a high PIV (PIV ≥ 622.71) had much a higher revascularization in unstable angina (UA) rate at long-term follow-up than patients with a low PIV (PIV < 622.71).
Abbreviations: SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value.