ABSTRACT
Objective.
This study aimed to describe and critically evaluate the COVID-19 vaccination program for high-risk children in Curacao and provide information about important factors such as parents’ vaccination hesitancy and effective strategies for communicating and delivering information about vaccination.
Methods.
This was a cross-sectional study. It was important to identify children aged 12–17 years who were at high risk of severe COVID-19 infection because of the limited medical facilities on the island; children considered to be at high risk were those with diseases such as obesity, hypertension or diabetes mellitus type 2. These children or their caregivers were invited by their pediatricians to be vaccinated as part of a program run by the Public Health Department of Curacao. These high-risk patients were vaccinated between 30 May 2021 and 25 February 2022 in designated child-friendly spaces, with a pediatrician present for guidance and reassurance. Children received the Pfizer-BioNTech COVID-19 vaccine at the recommended dose for their age. The primary outcome was a description and evaluation of the attendance for vaccination. The secondary outcomes were side effects after vaccination for the age groups 12–15 years and 16–17 years. Reasons for refusal or nonadherence were also registered.
Results.
Altogether 51% (24/47) of those aged 16–17 years who were invited were vaccinated compared with 42% (26/69) of those aged 12–15 years who were invited. Altogether, 46% of these high-risk children were vaccinated compared with 48% of children aged 12–17 years without risk factors. In our population, most patients did not experience any side effects and if they did, the side effects were mild. No cases of myocarditis or pericarditis were observed. A lack of trust in the vaccine and a lack of prioritization of vaccination when scheduling daily activities were important factors in refusal and nonadherence.
Conclusions.
To organize a successful vaccination program in a small community with limited resources for treating high-risk children it is crucial for medical professionals to provide reliable information. Public health initiatives should focus on assuaging parents’ fears about vaccines. In addition, ensuring there is good cooperation between doctors and the Public Health Department can help to make implementation successful. Finally, involving pediatricians and using dedicated areas for vaccinating children can help build trust with parents and caregivers.
Keywords: COVID-19 vaccines, adolescent, child, vaccination hesitancy, public health, Curacao
RESUMEN
Objetivo.
El objetivo de este estudio consistió en describir y realizar una evaluación crítica del programa de vacunación contra la COVID-19 para adolescentes de alto riesgo en Curazao, así como proporcionar información sobre factores importantes, como el recelo de los progenitores con respecto a la vacunación y las estrategias eficaces para comunicar y ofrecer información sobre ella.
Métodos.
Se llevó a cabo un estudio transversal. Debido a las limitaciones de los centros médicos de la isla, era importante seleccionar a los adolescentes de entre 12 y 17 años con un riesgo alto de infección grave por COVID-19; se consideró que tenían un riesgo alto los miembros de este grupo poblacional que presentaban enfermedades como obesidad, hipertensión arterial o diabetes mellitus de tipo 2. Tanto estos adolescentes como sus cuidadores fueron invitados por sus pediatras a vacunarse dentro del marco de un programa impulsado por el Departamento de Salud Pública de Curazao. Estos pacientes de alto riesgo se vacunaron entre el 30 de mayo del 2021 y el 25 de febrero del 2022 en espacios adaptados a la población pediátrica, que contaban con la presencia de un especialista en pediatría para orientarles y tranquilizarles y donde se les administró la vacuna contra la COVID-19 de Pfizer-BioNTech en la dosis recomendada para su edad. El criterio de valoración principal fue la descripción y evaluación de la asistencia para recibir la vacuna. El criterio de valoración secundario fueron los efectos secundarios posteriores a la vacunación en los grupos de edad de 12 a 15 años y de 16 a 17 años. También se registraron los motivos para negarse a recibir la vacuna o para el incumplimiento del calendario de vacunación.
Resultados.
En total, se vacunó al 51% (24/47) de las personas de 16-17 años invitadas, en comparación con el 42% (26/69) de las de 12-15 años. Se vacunó al 46% de esta población de alto riesgo, en comparación con el 48% de la población de 12 a 17 años sin factores de riesgo. En nuestra población, la mayoría de los pacientes no presentaron ningún efecto secundario y cuando los hubo, estos fueron leves. No se observaron casos de miocarditis ni de pericarditis. La falta de confianza en la vacuna y la baja prioridad otorgada a la vacunación a la hora de programar las actividades diarias fueron factores importantes en la negativa a recibir la vacuna o el incumplimiento del calendario de vacunación.
Conclusiones.
Si se quiere organizar un programa de vacunación exitoso en una comunidad pequeña y con recursos limitados para tratar a la población adolescente de alto riesgo, es crucial que el personal médico proporcione una información fiable. Las iniciativas de salud pública deben centrarse en disipar los temores de los progenitores sobre las vacunas. Asimismo, el hecho de asegurar una buena cooperación entre el personal médico y el Departamento de Salud Pública puede contribuir al éxito de la iniciativa. Por último, la involucración de pediatras y el uso de espacios específicos para la vacunación de la población adolescente pueden ayudar a generar un clima de confianza en progenitores y cuidadores.
Palabras clave: Vacunas contra la COVID-19, adolescente, niño, vacilación a la vacunación, salud pública, Curazao
RESUMO
Objetivo.
Este estudo teve como objetivo descrever e avaliar de maneira crítica o programa de vacinação contra a COVID-19 para adolescentes de alto risco em Curaçao e dar informações sobre fatores importantes, como a hesitação vacinal dos pais e estratégias efetivas para comunicar e fornecer informações sobre a vacinação.
Métodos.
Este foi um estudo transversal. Era importante identificar os adolescentes entre 12 e 17 anos que tinham alto risco de infecção grave por COVID-19 devido à escassez de estabelecimentos de saúde na ilha; os adolescentes considerados de alto risco tinham obesidade, hipertensão arterial ou diabetes mellitus tipo 2. Esses adolescentes e seus cuidadores foram convidados por seus pediatras a serem vacinados como parte de um programa do Departamento de Saúde Pública de Curaçao. Esses pacientes de alto risco foram vacinados entre 30 de maio de 2021 e 25 de fevereiro de 2022 em espaços adaptados para adolescentes e com a presença de um pediatra para orientação e segurança. Os adolescentes receberam a vacina Pfizer-BioNTech COVID-19 na dose recomendada para a idade. O desfecho primário foi a descrição e a avaliação do comparecimento à vacinação. Os desfechos secundários foram os efeitos colaterais após a vacinação nas faixas etárias de 12 a 15 anos e de 16 a 17 anos. Os motivos de recusa ou não adesão também foram registrados.
Resultados.
No total, 51% (24/47) dos adolescentes convidados de 16 a 17 anos de idade foram vacinados, em comparação com 42% (26/69) dos adolescentes convidados de 12 a 15 anos de idade. No total, 46% desses adolescentes de alto risco foram vacinados, em comparação com 48% dos adolescentes de 12 a 17 anos sem fatores de risco. Na população do estudo, a maioria dos pacientes não apresentou nenhum efeito colateral e, quando presentes, os efeitos colaterais foram leves. Não foram observados casos de miocardite ou pericardite. A falta de confiança na vacina e a falta de priorização da vacinação ao programar as atividades diárias foram fatores importantes para recusa e não adesão.
Conclusões.
Para organizar um programa de vacinação bem-sucedido em uma pequena comunidade com recursos limitados para o tratamento de adolescentes de alto risco, é fundamental que os profissionais médicos apresentem informações confiáveis. As iniciativas de saúde pública devem se concentrar em aliviar o medo dos pais em relação às vacinas. Além disso, garantir que haja boa cooperação entre os médicos e o Departamento de Saúde Pública pode ajudar no sucesso da implementação. Por fim, o envolvimento de pediatras e o uso de áreas exclusivas para a vacinação de adolescentes podem ajudar a criar confiança nos pais e cuidadores.
Palavras-chave: Vacinas contra COVID-19, adolescente, criança, hesitação vacinal, saúde pública, Curaçao
Countries worldwide have been challenged to contain the spread of severe acute respiratory syndrome coronavirus 2 (known as SARS-CoV-2), and the World Health Organization (WHO) has launched a global campaign to ensure prevention, early diagnosis and medical treatment for infection with the virus (1). Public health measures to suppress transmission, including social distancing and travel restrictions, have reduced the spread of the virus. At the same time, these protective actions have radically transformed social life and disrupted national and household economies (2). These measures have been an economic disaster, especially for small island developing states that depend on tourism. One of the most promising solutions to this disruption is vaccination. This technology can provide individual- and population-level immunity, and through these, the eventual conditions for the resumption of routine social and economic activities (3). Since vaccines were introduced, they have become the primary method of containing the virus.
Curacao is a small island developing state in the Caribbean, with a population of 160 000. There is a high prevalence of obesity, hypertension and diabetes mellitus type 2, all risk factors for developing severe COVID-19 infection (4). Because intensive care beds and the medical workforce capacity are limited, avoiding overburdening the health care system has been important. In February 2021, the first vaccinations were offered to adults on the island.
Although the disease in children and adolescents has been reasonably mild (5), there is a risk of multisystem inflammatory syndrome developing in children, a severe inflammatory response that affects multiple organ systems and can be life-threatening (6). Similar to adults, children and adolescents can also develop what is known as long COVID – that is, prolonged symptoms after infection (7).
The Pfizer-BioNTech COVID-19 vaccine was approved by the United States Food and Drug Administration and the European Medicines Agency in December 2020 for individuals aged 16 years and older (8). In April 2021, the Netherlands started vaccinating adolescents considered to be at high risk for severe disease. Because Curacao is historically connected to the Netherlands, we decided to follow their example and started organizing a COVID-19 vaccination program for high-risk children. Worldwide, there is a lot of experience establishing vaccination programs for children. Also, in Curacao there is a national youth vaccination program that includes vaccines against diphtheria, whooping cough (pertussis), tetanus, polio, Haemophilus influenzae type B, hepatitis B, Streptococcus pneumoniae, mumps, measles and rubella. This program is coordinated by the Curacao Public Health Department, and current vaccination coverage is up to 80% (Youth Health Care Department, Ministry of Health, unpublished data, 2022).
The aim of this study was to describe and critically evaluate the coverage of our COVID-19 vaccination program for high-risk children aged 12–17 years. Additionally, important factors affecting vaccination hesitancy on the part of parents or caregivers were identified.
METHODS
Selecting participants
We performed a cross-sectional study, adopting the Netherlands’ criteria for high-risk children (Box 1). On Curacao, however, there is a unique, small community setting, with only one pediatric hospital department at the Curacao Medical Center, no pediatric intensive care unit and limited access to medication. Emergency referral to a pediatric intensive care unit abroad means sending a patient by air ambulance – often without their parents – to a referral center in Colombia, where a foreign language is spoken. Therefore, the pediatric department at the Medical Center further broadened the criteria for vaccinating high-risk children, after the Pediatric Association of the Netherlands approved pediatric vaccination (Box 2). The need to vaccinate adolescents in high-risk groups was discussed by pediatricians at the Medical Center (LJFJ and AJD) with the Public Health Department, which is responsible for the COVID-19 vaccination program. With the Department’s authorization, 8 of the 10 pediatricians on the island – who mostly work at the Curacao Medical Center – reviewed the high-risk patients in their care and entered them into an online database. Two pediatricians did not respond to this request, both of whom work mainly in private practice.
BOX 1. Criteria for determining whether a person is at high risk for developing a severe COVID-19 infection, Pediatric Association of the Netherlands, 2021.
Hematological malignancy in the past 5 years
Kidney failure (i.e. on dialysis or preparing for dialysis)
Organ, stem cell or bone marrow transplantation
Severe primary immune deficiency
Neurological condition leading to respiratory problems
Down syndrome
Severe obesity (body mass index ≥ 40)
Source: Box developed by the authors based on information from the Pediatric Association of the Netherlands (2021).
BOX 2. Additional criteria for determining whether a person is at high risk for developing a severe COVID-19 infection, Curacao, 2021.
Type 1 or type 2 diabetes mellitus
Severe respiratory disorders
Chronic impairment of cardiac function
Receiving immunosuppressive medication
Sickle cell disease
Obesity (body mass index ≥ 30)
Source: Information developed by the authors.
Procedure
All eligible patients aged 16–17 years or their caregivers, or both, were contacted by their own pediatrician, and verbal information was given about the vaccination, sometimes during multiple conversations. Pediatricians noted in the database whether consent was given for vaccination. After 4 weeks, the list of patients who had provided informed consent was given to the Public Health Department, which then called all patients or their caregivers, or both, to inform them about the date, time and location for vaccination. All patients were scheduled for 30 May 2021 using walk-in hours. In the meantime, we, as staff members of the Curacao Medical Center, tried to raise awareness and offer accessible information about the vaccination program by giving interviews to a local radio station and newspaper. Articles were also posted on several of the hospital’s social media pages.
The Pfizer-BioNTech COVID-19 vaccine was used at one third of the recommended adult dosage (i.e. 10 μg instead of 30 μg), as advised by the manufacturer for administration in pediatric patients.
Specific days were planned so that patients could be vaccinated in a child-friendly environment. During all of these days, a pediatrician was present to offer extra guidance and medical support. On the first day, there were also three CliniClowns for additional distraction and support. (CliniClowns are specially trained clowns that bring resilience and lightness to sick children and people living with a disability or dementia.) A private room was available for children who needed tailored assistance. Staff offered personal and flexible approaches, including the possibility of vaccinating children in their parents’ car. Children who were having second thoughts received up to 45 minutes of extra attention from staff.
Three months later, all of the vaccinated adolescents or their caregivers were contacted and asked whether the adolescent had experienced side effects, such as pain at the injection site, fever or malaise. All of the adolescents who had not been vaccinated or their caregivers were also contacted to ask about their reasons for refusal or nonadherence.
In June 2021, when the Pfizer-BioNTech COVID-19 vaccine was approved for children aged 12–15 years, a similar vaccination cycle was used for this group, again with the recommended pediatric dosage for the vaccine. The last patients in this group were vaccinated on 25 February 2022.
The only statistical analysis performed was to determine the percentage that had been vaccinated.
Ethical approval
Project approval was given by the local medical ethics board, which required verbal informed consent from caregivers, and written informed consent was also obtained.
RESULTS
Adolescents aged 16–17 years
Among those aged 16–17 years, 47 were identified as being in a high-risk group, according to the newly described indications. A total of 24 (51%) of them were vaccinated; 9 (19%) consented initially but did not attend for vaccination; 2 (4%) refused immediately when contacted; 4 (9%) could not be reached by telephone; and 8 (17%) retracted or did not give written informed consent.
Of the 9 patients or caregivers who initially agreed to the vaccination but did not attend, one was afraid of needles. Three patients did not trust the vaccine, one did not want to be vaccinated after recently taking postoperative medication and four patients could not be reached after the initial contact (Figure 1).
FIGURE 1. Inclusion criteria for COVID-19 vaccination for adolescents aged 16–17 years at high risk for severe disease, Curacao, 2021.
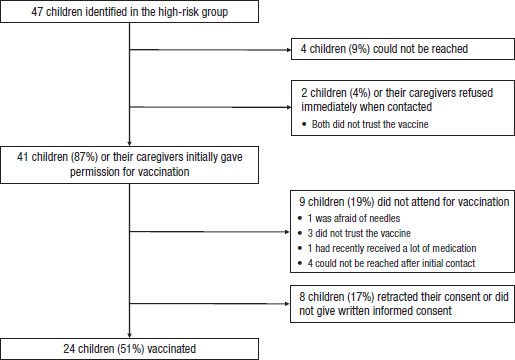
Source: Figure developed by the authors based on the results of their study.
The follow-up interview about side effects was conducted 3 months after vaccination. Of the 24 patients who were vaccinated in this age group, 8 did not experience any side effects. Three patients reported pain at the injection site; one reported fever and one reported malaise. No complications required consultation with a pediatrician; 11 patients were not reached by phone (Figure 2).
FIGURE 2. Number of side effects among 29 children and adolescents aged 12–17 years vaccinated with Pfizer-BioNTech COVID-19 vaccine, Curacao, 2021.
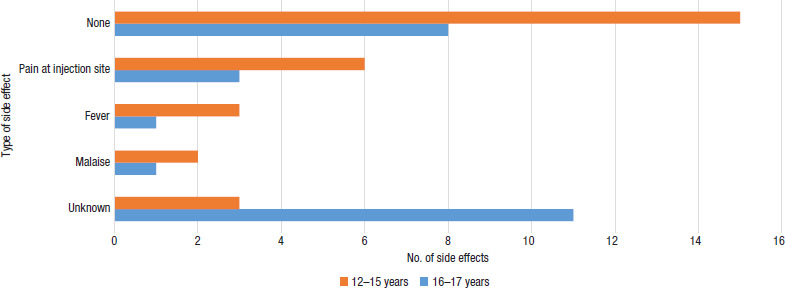
Source: Figure developed by the authors based on the results of their study.
Children aged 12–15 years
A total of 69 children aged 12–15 years were identified as being at high risk. A total of 29 (42%) were vaccinated; 15 (22%) children for whom consent was initially given did not attend for vaccination; consent was refused immediately for 10 (14%) children; and 15 (22%) could not be reached by telephone (Figure 3).
FIGURE 3. Inclusion criteria for COVID-19 vaccination for children aged 12–15 years at high risk for severe disease, Curacao, 2021.
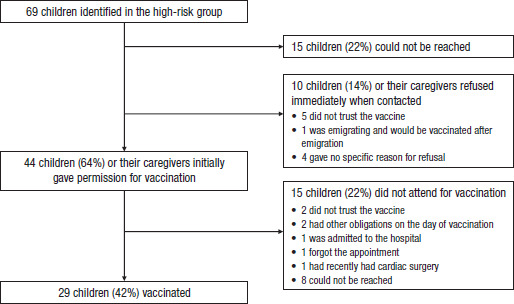
Source: Figure developed by the authors based on the results of their study.
Of the 25 children who were not vaccinated, 7 did not trust it. Two patients had other obligations on the day of their appointment; one patient was admitted to the hospital and one patient forgot the appointment. For one patient the vaccine came too soon after cardiac surgery, and one patient’s caregiver refused because of upcoming emigration. Eight patients could not be reached. The caregivers for four patients gave no specific reasons for refusal.
Of the 29 patients who were vaccinated, 15 did not experience any side effects. Six patients reported pain at the injection site; three reported fever and two reported malaise. No complications required consultation with a pediatrician. Three patients were not reached by phone (Figure 2).
Comparison between age groups
Among those aged 16–17 years, 51% of eligible children were vaccinated compared with 42% of those aged 12–15 years. Thus 46% of these high-risk children were vaccinated compared with 48% of children aged 12–17 years who did not have risk factors. Children who were not at high risk were vaccinated later, during the general national COVID-19 vaccination program (Public Health Department, Ministry of Health, Curacao, unpublished data, 2021–2022).
DISCUSSION
To our knowledge, Curacao was the first Caribbean island to organize COVID-19 vaccinations for high-risk children in 2021. The program started by vaccinating high-risk children aged 16–17 years and has since been extended to all children aged 5 years and older. Our findings may be applicable to the entire pediatric vaccination program, especially with the recent authorization by the US Food and Drug Administration of vaccines for children aged 6 months and older.
Worldwide, no data have been published on the actual number of high-risk children who have been vaccinated against COVID-19. However, two systematic reviews have been published about parents’ willingness to vaccinate their children against COVID-19 (9, 10). The overall proportion of parents that intended to vaccinate their children against COVID-19 was 60.1%, while the proportion of parents that refused to vaccinate their children was 22.9%, and the proportion of parents who were unsure was 25.8% (10). The highest rate of willingness to vaccinate was 91.4%, observed in Brazil (11), and the lowest rate of willingness to vaccinate was 21.6%, found in North America (12). The main reasons parents gave in the reviews for being reluctant to vaccinate their children were concerns about safety, the novelty of or lack of evidence for the vaccines and doubts about their effectiveness (9). The main predictors of parents’ intention to vaccinate their children were the attitudes of the father, older age of the parents, having a higher income, perceiving higher levels of threat from COVID-19 and having positive attitudes towards vaccination (e.g. as evidenced by children having a complete vaccination history and the uptake of COVID-19 vaccine among parents) (10). In the reviews, participants who had been exposed to scientific and positive information about COVID-19 vaccines were more willing to have their children vaccinated. A lack of official information or receiving misinformation was one of the main reasons for vaccine hesitancy among caregivers (9).
Our attendance rates for vaccination were close to those found by the systematic reviews for parents’ willingness to have their children vaccinated. This indicates that willingness may be a good predictor of the actual outcome. In addition, the main reason for refusal among our patients was comparable to data from the systematic reviews, namely mistrust.
Vaccinations are largely accepted in low- and middle-income countries. According to the results of the 2018 Wellcome Global Monitor – a survey of 140 000 individuals in 140 countries about public attitudes to health and science – 95% of participants in South Asia and 92% in East Africa described vaccination as safe in comparison with western Europe, where only 59% of participants believed vaccines to be safe (13). With newer vaccines, however, people tend to be more hesitant. Research using the vaccine hesitancy scale developed by WHO’s Strategic Advisory Group of Experts on Immunization suggested that even among a predominantly provaccine population of 2 265 respondents from Bangladesh, China, Ethiopia, Guatemala and India – where 95% agreed that childhood vaccines are important for their child’s health – more than 50% agreed with or were neutral about the statement that “new vaccines carry more risks than older vaccines” (14). Surveys among parents from high-income countries show that individuals are naturally willing to take more risks with new vaccines for infants when the direct benefits are greater (15). In contrast to these data, it has been difficult to introduce COVID-19 vaccination programs. The influence of social media and the historically short time frame in which the vaccines were developed have contributed to hesitancy among many persons.
There have been reports of side effects after vaccination, and the most common are pain at the injection site and mild flu-like symptoms. Rare cases of myocarditis and pericarditis have been reported in adolescents, mostly males and mainly following the second dose of vaccine. Nevertheless, the benefits of COVID-19 vaccination to individuals and at the population level clearly seem to outweigh the risks of myocarditis after vaccination (16). In our population, most children and adolescents did not experience any side effects and if they did, the side effects were mild. No cases of myocarditis or pericarditis were observed.
One of the strengths of the design of our vaccination program was the individualized approaches that we developed, based on the unique situation we have as a small island developing state. In addition, pediatricians contacted their own patients and offered them reliable information about the vaccine. Sometimes it was necessary to do this in multiple conversations, for example when patients or caregivers needed more time or had additional questions. To optimize vaccine uptake it is necessary to provide tailored and targeted communication materials and balanced information about vaccines that address both the benefits and risks (17). In our case, the information provided by pediatricians to the community through newspapers, radio and social media helped to build trust about the vaccine. Clear communication about the details of the vaccination program (e.g. date, location, time) helped to create greater adherence.
In addition, the presence of a pediatrician at the vaccination location generated confidence for patients and caregivers. These experiences are in line with the findings from a cross-sectional online survey in Switzerland that showed parents of younger children favor their pediatrician’s or family doctor’s office over vaccination centers when their child needs to be vaccinated (18). Finally, good cooperation with the Public Health Department is essential to ensure the successful logistics for such a program.
Some limitations to our study are reflected in our local setting. Because of our relatively small community, the sample size was correspondingly small. Furthermore, many of the eligible patients or their caregivers could not be reached by phone to give appropriate information or for follow up. One possible explanation could be that because of poverty not everybody has a working cellphone or telephone connection at home. Therefore, it is important to invest in community campaigns to address vaccination and to take advantage of the media to reach as many people as possible. Such campaigns need to focus on the doubts that patients and caregivers have about a new vaccine in terms of its safety, the perceived lack of evidence and its effectiveness. It also should be noted that messages and campaigns that are too aggressive often have the effect of arousing fear, which may lead those who receive the messages to ignore or repress them (19).
Another communication strategy could be for public health officers and doctors to visit neighborhoods to start conversations about the importance of vaccination; in this way, they could immediately respond to people’s doubts or reasons for hesitancy. Ideally, people would be able to be vaccinated at the same time. This could solve the problem of people not having transportation to a vaccination location. Offering vaccinations for children at schools could also be useful.
To our knowledge, this is the only paper that compares coverage of a COVID-19 vaccination program for children and adolescents with that of Curacao’s national youth vaccination program. Our attendance rate is lower than that of the national youth vaccination program, which reaches up to 80% of children. The most important reasons for refusing COVID-19 vaccination in our cross-sectional study were mistrust of the vaccine, priority-setting by parents and problems with transportation. This again emphasizes the importance of building trust in the vaccines being used.
Conclusions
High rates of vaccination coverage are indispensable to control the COVID-19 pandemic. This is the main reason why the COVID-19 vaccine roll out is expanding to the pediatric population. When organizing a vaccination program for children it is important to have health care workers provide reliable information. Targeted public health strategies should aim to reassure parents and address their concerns about vaccines. In addition, ensuring good cooperation between doctors and the Public Health Department can help to make implementation more successful. Finally, involving pediatricians and using dedicated vaccination areas for children can help build trust with parents.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the Revista Panamericana de Salud Pública/Pan American Journal of Public Health or the Pan American Health Organization.
Acknowledgement.
We thank the Curacao Public Health Department for their help with organizing the COVID-19 vaccination program. We thank all the pediatricians that helped us and the patients who took part in the vaccination program.
Funding Statement
None.
Footnotes
Author contributions.
LJFJ, SML and AJD conceived the original idea for and planned the vaccination program. LJFJ collected the data and wrote the paper. CtP did the follow up at 3 months. All authors reviewed and approved the final version of the manuscript.
Conflicts of interest.
None declared.
Funding.
None.
REFERENCES
- 1.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–9. [DOI] [PMC free article] [PubMed]
- 2.Tatapudi H, Das R, Das TK. Impact assessment of full and partial stay-at-home orders, face mask usage, and contact tracing: an agent-based simulation study of COVID-19 for an urban region. Glob Epidemiol. 2020;2:100036. doi: 10.1016/j.gloepi.2020.100036. [DOI] [PMC free article] [PubMed] [Google Scholar]; Tatapudi H, Das R, Das TK. Impact assessment of full and partial stay-at-home orders, face mask usage, and contact tracing: an agent-based simulation study of COVID-19 for an urban region. Glob Epidemiol. 2020;2:100036. [DOI] [PMC free article] [PubMed]
- 3.Schoch-Spana M, Brunson EK, Long R, Ruth A, Ravi SJ, Trotochaud M, et al. The public’s role in COVID-19 vaccination: human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 2021;39:6004–6012. doi: 10.1016/j.vaccine.2020.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]; Schoch-Spana M, Brunson EK, Long R, Ruth A, Ravi SJ, Trotochaud M, et al. The public’s role in COVID-19 vaccination: human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine. 2021;39:6004-12. [DOI] [PMC free article] [PubMed]
- 4.Gao YD, Ding M, Dong X, Zhang JJ, Kursat Azkur A, Azkur D, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76(2):428–455. doi: 10.1111/all.14657. [DOI] [PubMed] [Google Scholar]; Gao YD, Ding M, Dong X, Zhang JJ, Kursat Azkur A, Azkur D, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76(2):428-55. [DOI] [PubMed]
- 5.Mehta NA, Mytton OT, Mullins EW, Fowler TA, Falconer CL, Murphy OB, et al. SARS-CoV-2 (COVID-19): What do we know about children? A systematic review. Clin Infect Dis. 2020;71(9):2469–2479. doi: 10.1093/cid/ciaa556. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mehta NA, Mytton OT, Mullins EW, Fowler TA, Falconer CL, Murphy OB, et al. SARS-CoV-2 (COVID-19): What do we know about children? A systematic review. Clin Infect Dis. 2020; 71(9): 2469–79. [DOI] [PMC free article] [PubMed]
- 6.Flood J, Shingleton J, Bennett E, Walker B, Amin-Chowdhury Z, Oligbu G, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS): prospective, national surveillance, United Kingdom and Ireland, 2020. Lancet Reg Health Eur. 2021;3:100075. doi: 10.1016/j.lanepe.2021.100075. [DOI] [PMC free article] [PubMed] [Google Scholar]; Flood J, Shingleton J, Bennett E, Walker B, Amin-Chowdhury Z, Oligbu G, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS): prospective, national surveillance, United Kingdom and Ireland, 2020. Lancet Reg Health Eur 2021;3:100075. [DOI] [PMC free article] [PubMed]
- 7.Ludvigsson JF. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021;110(3):914–921. doi: 10.1111/apa.15673. [DOI] [PMC free article] [PubMed] [Google Scholar]; Ludvigsson JF. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021;110(3):914-21. [DOI] [PMC free article] [PubMed]
- 8.Tanne JH. Covid-19: FDA panel votes to approve Pfizer BioNTech vaccine. BMJ. 2020;371:m4799. doi: 10.1136/bmj.m4799. [DOI] [PubMed] [Google Scholar]; Tanne JH. Covid-19: FDA panel votes to approve Pfizer BioNTech vaccine. BMJ 2020;371:m4799. [DOI] [PubMed]
- 9.Chen F, He Y, Shi Y. Parents' and guardians' willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines (Basel) 2022;10:179. doi: 10.3390/vaccines10020179. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chen F, He Y, Shi Y. Parents' and guardians' willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines (Basel). 2022;10:179. [DOI] [PMC free article] [PubMed]
- 10.Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. 2022;157:106994. doi: 10.1016/j.ypmed.2022.106994. [DOI] [PMC free article] [PubMed] [Google Scholar]; Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. 2022;157:106994. [DOI] [PMC free article] [PubMed]
- 11.Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani G. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines (Basel) 2021;9:1115. doi: 10.3390/vaccines9101115. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani G. COVID-19 vaccine hesitancy among parents of children and adolescents living in Brazil. Vaccines (Basel). 2021;9:1115. [DOI] [PMC free article] [PubMed]
- 12.Marquez RR, Gosnell ES, Thikkurissy S, Schwartz SB, Cully JL. Caregiver acceptance of an anticipated COVID-19 vaccination. J Am Dent Assoc. 2021;152:730–739. doi: 10.1016/j.adaj.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]; Marquez RR, Gosnell ES, Thikkurissy S, Schwartz SB, Cully JL. Caregiver acceptance of an anticipated COVID-19 vaccination. J Am Dent Assoc. 2021;152:730–9. [DOI] [PMC free article] [PubMed]
- 13.Wellcome . Wellcome Global Monitor 2018. London: Wellcome; 2019. [cited 2018 December 1]. Available from: https://wellcome.org/reports/wellcome-global-monitor/2018. [Google Scholar]; Wellcome. Wellcome Global Monitor 2018. London: Wellcome; 2019 [cited 2018 December 1]. Available from: https://wellcome.org/reports/wellcome-global-monitor/2018
- 14.Wagner AL, Masters NB, Domek GJ, Mathew JL, Sun X, Asturias EJ, et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines (Basel) 2019;7:155. doi: 10.3390/vaccines7040155. [DOI] [PMC free article] [PubMed] [Google Scholar]; Wagner AL, Masters NB, Domek GJ, Mathew JL, Sun X, Asturias EJ, et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines (Basel). 2019;7:155. [DOI] [PMC free article] [PubMed]
- 15.Bakhache P, Rodrigo C, Davie S, Ahuja A, Sudovar B, Crudup T, Rose M. Health care providers’ and parents’ attitudes toward administration of new infant vaccines–a multinational survey. Eur J Pediatr. 2013;172:485–492. doi: 10.1007/s00431-012-1904-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Bakhache P, Rodrigo C, Davie S, Ahuja A, Sudovar B, Crudup T, Rose M. Health care providers’ and parents’ attitudes toward administration of new infant vaccines–a multinational survey. Eur J Pediatr. 2013;172:485–92. [DOI] [PMC free article] [PubMed]
- 16.Gargano JW, Wallace M, Hadler SC, Langley G, Su JR, Oster ME, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the Advisory Committee on Immunization Practices–United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gargano JW, Wallace M, Hadler SC, Langley G, Su JR, Oster ME, et al. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: update from the Advisory Committee on Immunization Practices–United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021;70:977-82. [DOI] [PMC free article] [PubMed]
- 17.Dubé E, Gagnon D, Vivion M. Optimizing communication material to address vaccine hesitancy. Can Commun Dis Rep. 2020;46(2-3):48–52. doi: 10.14745/ccdr.v46i23a05. [DOI] [PMC free article] [PubMed] [Google Scholar]; Dubé E, Gagnon D, Vivion M. Optimizing communication material to address vaccine hesitancy. Can Commun Dis Rep. 2020;46 (2-3):48-52. [DOI] [PMC free article] [PubMed]
- 18.Wagner A, Liberatore F, Schmelzer S, Dratva J. Confident and altruistic – parents’ motives to vaccinate their children against COVID-19: a cross-sectional online survey in a Swiss vaccination centre. Swiss Med Wkly. 2022;152:w30156. doi: 10.4414/smw.2022.w30156. [DOI] [PubMed] [Google Scholar]; Wagner A, Liberatore F, Schmelzer S, Dratva J. Confident and altruistic – parents’ motives to vaccinate their children against COVID-19: a cross-sectional online survey in a Swiss vaccination centre. Swiss Med Wkly. 2022;152:w30156. [DOI] [PubMed]
- 19.Babicki M, Pokorna-Kałwak D, Doniec Z, Mastalerz-Migas A. Attitudes of parents with regard to vaccination of children against COVID-19 in Poland. A Nationwide Online Survey. Vaccines (Basel) 2021;9(10):1192. doi: 10.3390/vaccines9101192. [DOI] [PMC free article] [PubMed] [Google Scholar]; Babicki, M, Pokorna-Kałwak D, Doniec Z, Mastalerz-Migas A. Attitudes of parents with regard to vaccination of children against COVID-19 in Poland. A Nationwide Online Survey. Vaccines (Basel). 2021;9(10):1192. [DOI] [PMC free article] [PubMed]


