Figure 2. Reclassification in the Primary Event Population.
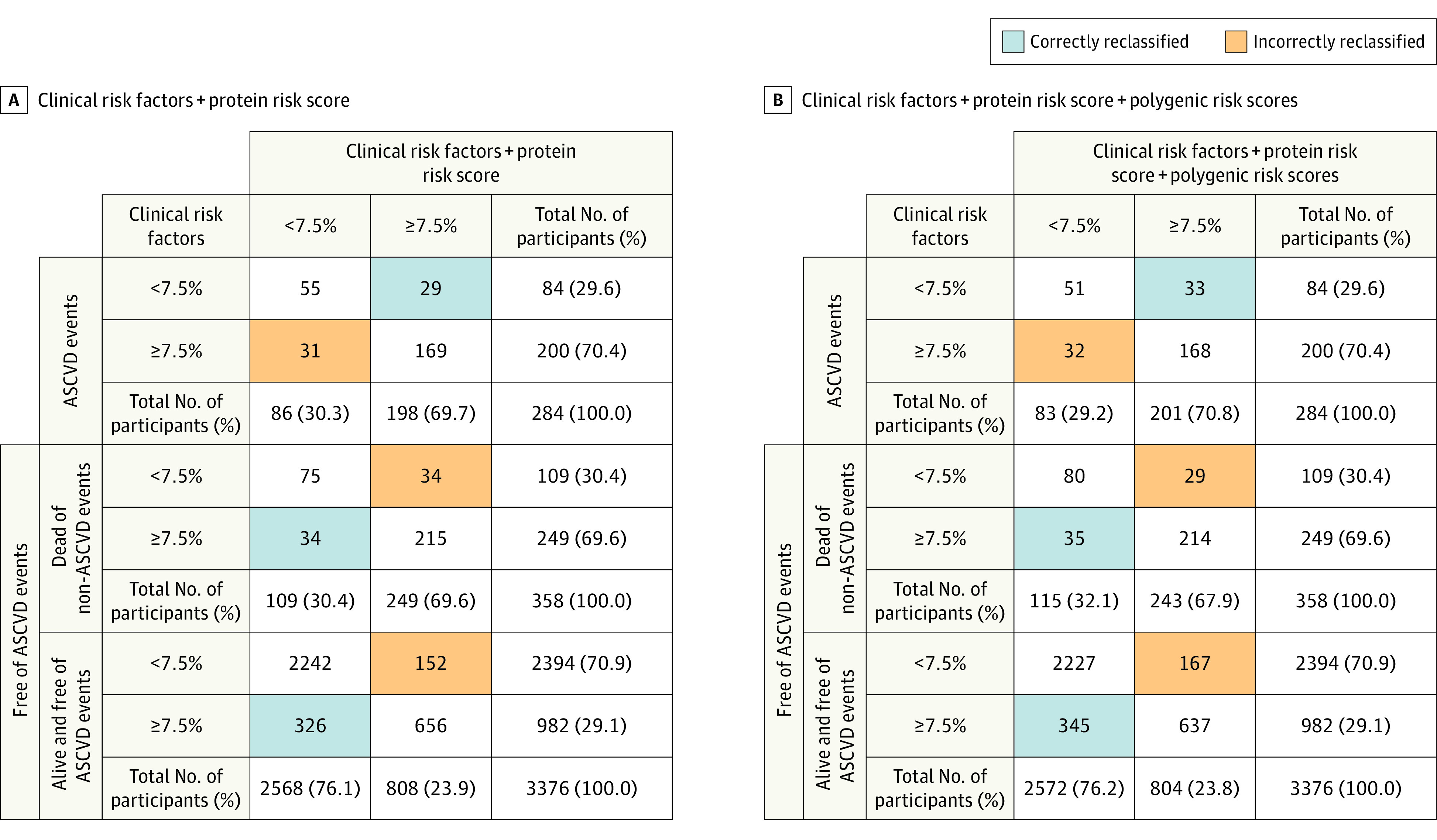
The figure shows reclassification results when protein risk score and polygenic risk scores are added on top of clinical risk factors (age, sex, statin use, hypertension treatment, type 2 diabetes, body mass index [calculated as weight in kilograms divided by height in meters squared], and smoking status at the time of plasma collection) in the primary event population test set (4018 participants; 465 events; 284 events within 10 years). The results are shown for predicted 10-year risk using a 7.5% risk threshold to separate between low and intermediate risk. Three groups are considered: (i) those with an atherosclerotic cardiovascular disease (ASCVD) event within 10 years; (ii) those who die of causes other than ASCVD within 10 years; and (iii) those who survive 10 years without an ASCVD event.
Panel A shows a reclassification table for the addition of protein risk score on top of the clinical risk factors. The total categorical net reclassification improvement is 0.040 (95% CI, −0.009 to 0.094) and 0.044 (95% CI, −0.013 to 0.096) when excluding those who die from non-ASCVD causes. Net reclassification improvement for ASCVD events is −0.007 (95% CI, −0.056 to 0.046), 0.047 (95% CI, 0.035 to 0.059) for ASCVD nonevents (groups [ii] and [iii]), and 0.052 (95% CI, 0.039 to 0.064) for those who survive 10 years without ASCVD event (group [iii]).
Panel B shows a reclassification table when both protein risk score and polygenic risk scores are added on top of the clinical risk factors. The total net reclassification improvement is 0.053 (95% CI, −0.006 to 0.110) and 0.056 (95% CI, −0.001 to 0.114) when excluding those who die from non-ASCVD causes. Net reclassification improvement for ASCVD events is 0.004 (95% CI, −0.054 to 0.058), 0.049 (95% CI, 0.037 to 0.061) for ASCVD nonevents (groups [ii] and [iii]), and 0.053 (95% CI, 0.039 to 0.066) for those who survive 10 years without ASCVD event (group [iii]).
