Abstract
Background
Hypertension has affected over 1.13 billion people worldwide in 2015 and it's one of the most preventable risk-factors for morbidity and mortality. Antihypertensives significantly reduce cardiovascular risks. Several studies on antihypertensives' prescribing patterns were conducted worldwide, and guidelines were developed on hypertension management. However, no systematic reviews were conducted globally to synthesize the evidence from these studies. This review aims to evaluate antihypertensives' prescription patterns, and adherence to international guidelines for hypertension management worldwide.
Methods
Full-text antihypertensives' prescribing patterns evaluation studies were included. Reviews, commentaries, guidelines, and editorials were excluded. Various databases were searched including PubMed, Embase, and others. Studies were limited to English only and to articles published from (01/01/2010) to (20/03/2020). Crowe Critical Appraisal Tool (CCAT) was used for quality assessment.
Results
The most commonly prescribed antihypertensives as monotherapy in adult patients with no comorbidities were ACEIs/ARBs (Angiotensin converting enzyme inhibitors/Angiotensin receptor blockers), followed by CCBs (Calcium channel blockers), and BBs (Beta Blockers). Most commonly prescribed dual combinations were thiazide diuretics+ACEIs/ARBs, BBs + CCBs and CCBs+ACEIs/ARBs. Among diabetic patients, the most common agents were ACEIs/ARBs. Among patients with heart diseases, CCBs were prescribed frequently. While patients with kidney diseases, CCBs and ARBs were most prescribed. Of the 40 studies included in the review, only four studies directly assessed the prescribing patterns of antihypertensives in adherence to clinical practice guidelines. And only two studies confirmed adherence to guidelines. Furthermore, the quality of the majority of studies was moderate (50%), while 25% of articles were reported as either high or low quality.
Conclusion
This review revealed that there are areas for improvement for prescribing practices of antihypertensives in concordance with the latest evidence and with clinical practice guidelines.
Keywords: Prescribing patterns, Hypertension, Guidelines, Review
1. Introduction
In 2015, the estimated number of people with hypertension globally was over 1.13 billion.1 According to the World Health Organization (WHO) global report on non-communicable diseases (NCDs) in 2015, one in four men and one in five women had hypertension, defined as elevated systolic and/or diastolic blood pressure (SBP and/or DBP) of 140/90 mmHg or greater.2 Globally, high blood pressure (BP) has doubled over the past 40 years, according to a study published in 2016 by the Noncommunicable Disease Risk Factor Collaboration network (NCD-RisC).3 This increase has primarily been seen in low- and middle-income countries.3 The highest prevalence of hypertension was in the African region were 27% of the adult population was hypertensive.1 On the other hand, the lowest prevalence was found in the Americas, where 18% of the population was hypertensive.1
There has been significant advancement in hypertension management, but it remains a major preventable death and morbidity risk factor. And If not diagnosed early and managed properly, hypertension can be associated with several complications such as renal failure, heart failure (HF), sexual dysfunction, peripheral artery disease (PAD), loss of vision, angina, myocardial infarction (MI), and stroke.4 Reducing blood pressure using lifestyle modifications and/or antihypertensive therapy can significantly decrease the risk of cardiovascular morbidity and premature mortality.5 For example, decreasing SBP by 10-mmHg can significantly lower the risk of major cardiovascular disease (CVD) events by 20%, stroke by 27%, coronary heart disease (CHD) by 17%, HF by 28%, and all-cause mortality by 13%.6 Therefore, it is important to achieve BP control targets to lessen the risk of developing CVDs or other NCDs.
Several clinical practice guidelines for hypertension management have been developed and regularly updated to provide direction and guidance for standardized practice by clinicians.6, 7, 8 One example is the eight Joint National Committee (JNC8) guideline and the American College of Cardiology/American Heart Association (ACC/AHA) 2017.6, 7, 8, 9
Although hypertension treatment is available, it remains suboptimal within various populations in terms of BP control and prognosis.9 The trend of BP control was examined in a systematic review that included studies from US, United Kingdom (UK), Europe, Australia, Canada, Brazil, Mexico, India, Japan, South Africa, Jamaica, Saudi Arabia, Nigeria and other countries.10 Only one in eight people with diabetes and hypertension have controlled blood pressure, according to the review.10 These results suggest that despite the availability of antihypertensive agents and evidence-based recommendations endorsed by several guidelines, BP control is not adequate in the countries originally included in the study.10
While many studies have been conducted to assess the prescribing patterns or trends of antihypertensive medications and adherence to hypertension management guidelines worldwide, there is need to synthesize this available evidence to obtain an aggregate and holistic picture of antihypertensives prescribing globally. This review aimed to systematically evaluate antihypertensive prescribing patterns, and adherence to guidelines for hypertension management.
2. Methods
2.1. Review protocol and registration
We conducted and reported this systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement and its most recent extension PRISMA-S.11,12 The protocol was registered and is available on PROSPERO at the Centre for Reviews and Dissemination, University of York, United Kingdom (CRD42020175853).
2.2. Data sources and search strategy
Systematic and comprehensive search was conducted using the following databases and search engines: PubMed®, EMBASE®, Web of Science®, Scopus®, Trip®, Wiley Online Library®, ProQuest®, Elsevier ScienceDirect®, OpenGrey® and Google Scholar®. Moreover, the bibliographies of retrieved articles were manually searched to locate other relevant articles that were not identified in the electronic search. Different search terms driven from the review question were combined using Boolean operators. Keywords were modified based on individual databases (for example: using MeSH terms in PubMed® and Emtree in EMBASE® databases) (Table 1: Search Terms).
Table 1.
Search Terms.
| Category | Definition/explanation | Search terms |
|---|---|---|
| P | Adult hypertensive patients receiving antihypertensive medications | Hypertensive OR hypertension OR Hypertens* OR High blood pressure OR blood pressure lowering OR beta blocker OR calcium channel blocker OR CCB OR angiotensin converting enzyme inhibitor OR ACEI OR ACE inhibitor OR angiotensin receptor blocker OR ARB OR Diuretic OR thiazide OR renin inhibitor OR Aliskiren OR alpha blocker |
| I | Prescribing of antihypertensives | Prescrib* OR use OR utilize OR utilization OR prescription OR treat* OR manag* OR pharmacotherapy OR therapy |
| C/O | Patterns of antihypertensives prescribing for the management of hypertension and their adherence to guidelines | Type OR Trend OR Pattern OR Habit OR Appropriate* OR Rational* OR Control OR Guideline OR Recommend* OR Adhere* OR Compliance OR Comply OR Proper |
2.3. Eligibility criteria
2.3.1. Inclusion criteria
We included studies examining the prescribing patterns of antihypertensive agents regardless of the study design. Articles were included in this systematic review if they fulfill the following inclusion criteria:
-
-
Assessing and reporting the prescribing patterns of antihypertensives in adult hypertensive patients older than 18
AND/OR
-
-
Evaluating the adherence of antihypertensives prescribing to guidelines
We only included publications published in the last 10 years between January 1, 2010, to March 12, 2021 to cover the most updated studies in hypertension management and to assess if prescribing was in concordance with the most recent hypertension management guidelines.
2.3.2. Exclusion criteria
Reviews, letters, editorials, commentaries, and non-English studies were excluded from the review.
2.4. Studies selection
The electronic databases were searched to identify studies that were potentially eligible for inclusion in the review. Titles and abstracts of studies were screened independently by two study investigators (MH and NA) against the criteria listed above. Articles meeting the review criteria were selected as potentially eligible. Moreover, two reviewers (MH and NA) independently read the full text of each study identified from the title/abstract screening for potential inclusion in the review. Any discrepancies or disagreements, at all the study stages including retrieval and screening of studies, were resolved through discussions with a third peer reviewer (AA or HE).
2.5. Data extraction and quality assessment
Two reviewers independently reviewed the included articles and extracted the data using a pre-formulated data extraction sheet. In addition, the selected studies were assessed for quality using the Crowe Critical Appraisal Tool (CCAT).13 The CCAT is a quality assessment tool that helps researchers to conduct critical appraisal of quantitative and qualitative studies. It has eight domains including preliminaries, introduction, design, sampling, ethical matters, data collection, results, and discussion with a total maximum score of 40. The data extraction form includes the following elements: author(s), the study setting, country and year of publication, tool used for data collection, study design, population characteristics, outcome measures, source of funding, and limitations.
2.6. Data synthesis and analysis
Data was synthesized using a descriptive and narrative approached in this review. Based on the extracted data, we summarized the findings relating to the studies' main objectives and characteristics in Table 2, Table 3. The CCAT scores for each study were compared between two study investigators (MH and NA) and an agreement was made on a final score for each study. Conflicts were resolved through discussions with other investigators. The CCAT tool does not have a cutoff score; thus, we used the 25th, 50th and 75th percentiles to categorize the studies as low, moderate and high quality. Studies with a score below the 25th percentile were considered of low quality, studies with scores between 25th and 75th percentile were identified of moderate quality, while studies with scores above 75th percentile were considered of high quality. Statistical Package for the Social Sciences (SPSS®) version 26 was used to calculate the percentiles of the scores. This approach was previously used by Donnelly et al.13
Table 2.
Baseline Characteristics of included studies.
| Author/ Year/Code | Country/Setting | Population studied | Inclusion criteria | Exclusion criteria | Study design | Time when data is collected | Tool used for data collection if any | Population Characteristics /number of participant (N) |
|---|---|---|---|---|---|---|---|---|
| Abdulameer/ 2012/A1 47 |
Malaysia (outpatient cardiology clinic) |
Diabetic and ischemic heart disease patients with HTN | HTN with and without comorbidities (DM and IHD) who visited the outpatient clinic and > 18 years |
Exclusion ➔ HTN with renal disease, thyroid disease, HF, liver disease, COPD, MI or patients who have undergone operative revascularization of the coronary vessels and patients with no clear diagnosis or laboratory data |
Cross-sectional cohort study | 2012 | Medical records of patients attending the outpatient clinic |
N = 313
|
| Abougalambou/ 2011/A2 48 |
Malaysia/ outpatient clinic |
Diabetic type II population with HTN | type 2 DM outpatients with regular follow-up at diabetes Hospital University Sains Malaysia clinics study and age above 18 years |
Juvenile Diabetes, Gestational diabetes, advanced CKD and DM due to other causes | Prospective follow-up descriptive study | 2008 | Data records |
N = 1077 - Male: 44.2% - 50- 65 years: 58.1% - >65 years: 22.5% - Malay: 85.1% - Chinese: 13.9% - Lower educational level: 46.1% - Never smoked: 86.4% |
| Adamu/2017/A3 14 |
Nigeria/ Specialists Outpatient Clinics |
Adult hypertensive patients | hypertensive patients ≥ 18 years |
HTN with Complications: HF, CKD, CVA, MI, patients with neoplasm, incomplete medical history and those who refused giving consent |
Cross sectional | 2016 | Patients' case notes, semi-structured questionnaire, BP measurements |
N = 295
|
| Adejumo/ 2017/A4 15 |
Nigeria/ Benin teaching hospital |
Hypertensive patients | HTN patients at The Medical Outpatient Department of the University of Benin Teaching Hospital over a period of 8 weeks from 1st December 2012 to 31st January 2013 |
Not mentioned | Prescription pattern audit (medical records review) | 2012 | Clinic's outpatient files, patients' interviews guided with a form |
N = 224
|
| Alkhaja/2019/A5 16 |
Bahrain/ Primary health care centers |
Hypertensive older adults (65 years and above) | All outpatient prescriptions with antihypertensives with a 3 months or more extended refill order request |
All outpatient prescriptions with antihypertensives prescribed as short-term trial therapy, duplicated prescriptions, and those with a refill order request <3 months |
Observational prescription review | 2019 | Manual collection of written prescriptions |
N = 8746 - ≥ 65 years:24.1% - <65 years:75.9% - Mean age (± SD) of older adults: 72.1 ± 6.6 -Mean age (± SD) of young adults: 51.9 ± 7.7 -Male patients accounted for 46.1% of older adults and 54% of young adults |
| Alba-Leonel/2016/A6 17 |
Mexico/ Community health center |
Hypertensive patients | >20 years hypertensive adults | Incomplete records and pregnant women | Retrospective cross-sectional drug utilization study | 2014 | -Patient's medical records at the community health center -Survey to medical doctors attending patients whom records were collected |
N = 345
|
| Alkaabi/2019/A7 18 |
United Arab Emirates/ Dibba hospital Fujairah |
Adult hypertensive patients | Adult hypertensive patients treated and visiting the outpatient and inpatient facilities of the internal medicine department of study site | Patients with malignant HTN, significant renal and hepatic diseases, and pregnant women |
Prospective observational study | 2018 | Electronic medical records using a data collection form |
N = 588 - Male: 42.9% - 58-67 years: 31% - 68-77 years: 23.3% - Emirati: 79.6% - Diabetes: 8.2% - Hyperlipidemia:23.2% -Diabetes+ hyperlipidemia: 32.7% |
| Adnan/2010/A8 52 |
Ireland | Adult hypertensive patients | Patients ≥16 years old and prescribed any medications between 1st January 2000 and 30th April 2009 Patients co-prescribed ACEIs and ARBs in the same prescription claim and other comorbidities were identified |
Not stated | Observational prescription review | 2010 | Irish Health Service Executive - Primary Care Reimbursement Services (HSE-PCRS) national primary care prescribing database |
N = 18,337
|
| Ahmed/2020/A9 19 |
Saudi Arabia/Al Kharj city /public hospital | Adults hypertensive patients | All outpatient prescriptions that contain amlodipine in 2018 | Prescriptions before or after 2018 containing amlodipine In-patient prescriptions |
Retrospective observational | 2018 | Prescriptions and medical records review |
N = 465 patient prescription for 401 patients
|
| Beg/2014/B120 | India/ Tertiary care teaching hospital |
Adults hypertensive patients | Hypertensive patients attending the hospital |
Not mentioned | Prospective drug utilization study | 2014 (Not mentioned clearly) |
Prescriptions records and patients medical records |
N = 645 prescriptions
|
| Bulatova/ 2013/B2 51 |
Jordan/ Cardiology outpatient clinics at Jordan University Hospital and Albasheer Hospital |
Adults Hypertensive patients |
Adult hypertensive patients ≥18 years | Not mentioned | Cross-sectional observational study | 2007 | Medical files and records and patients interviews |
N = 408
|
| Chang/2016/C1 21 |
United States America and Puerto Rico/Clinical sites (organized into 5 clinical center networks) | Adult Hypertensive patients |
Hypertensive patients (treated or untreated) ≥ 75 years or ≥ 50 years with at least 1cardiovascular risk (history of CVD, Framingham risk score for 10 cardiovascular disease event 15 and above or CKD) Patients with at least 1 antihypertensive at baseline |
History of stroke, DM, polycystic kidney disease, dementia, non-adherence, eGFR<20 mL/min per 1.73 m2 or ≥ 1 g of proteinuria/day |
Cohort based on a randomized controlled trial (SPRINT trial) | 2013 | Data from SPRINT trial on patients baseline characteristics and medications prescribed and BP measurements |
N = 7582 Female:36.7% 60–69 years: 36.2% White:57% Black:30.2% History of CAD: 13.9% |
| Dhanaraj/ 2012/D1 39 |
North India/ Tertiary care center (Nehru Hospital) | Adult diabetic hypertensive patients |
Type II DM hypertensive | Pregnant women, type I DM patients |
Cross-sectional study | 2009 | Not mentioned |
N = 1185 -Average age 55.6 ± 10.1 -Male:52% |
| Elmawardy/ 2016/E1 22 |
Egypt/ Outpatient private clinics |
Adult hypertensive patients | ≥18 years hypertensive being treated and signs the informed consent | Newly diagnosed patients, pregnant, lactating women, those enrolled in other HTN clinical trials | Cross-sectional multicenter observational study | 2012 | Case report forms filled by physicians |
N = 4139 -Mean age (Controlled: 54.2 ± 10.6, Uncontrolled 55.4 ± 9.5) -Mean duration of HTN (Controlled 7.60 ± 6.30 Uncontrolled 8.10 ± 6.40) - Male (controlled (58.98%-uncontrolled 54.71%) |
| Rajasekhar et al. /2016/G1 23 |
India/ RIMS governmental hospital |
Adults hypertensive patients | - >25 years - patients with comorbidities |
-pregnant women - children - CKD patients |
Prospective observational study | 2015 | Patients' prescriptions and personal interviews |
N = 394 - Males: 63.70% - 56-65 years:144 - >65 years: 103
|
| Grigoryan/ 2013/G2 43 |
United States/ primary care centers |
Adults hypertensive patients | - >21 years - at least 2 clinic visits (last 12 months) - in last 2visits ≥140 mmHg SBP or ≥ 90 mmHg diastolic DBP, or if diabetic, ≥130 mmHg SBP or 80 mmHg DBP |
Cognitive impairment, renal insufficiency, serious illness (cancer), recent MI, unstable angina | Data for this study were collected as part of a cluster-randomized trial | 2007–2013 | Patients' medical records |
N = 140 uncontrolled resistant HTN
|
| Gu/2012/G3 44 |
United States | Adults hypertensive patients | All hypertensive patients on antihypertensives | - Lack of prescription medication - Pregnant women |
Cross-sectional study | 2010 From NHANES 2001–2002 To NHANES 2009–2010 |
NHANES survey participants did in-person home interviews |
N = 9320 2001–2002 -Women:68.6% -Men:57.2% - ≥ 60 years: 72.2% −40-59 years: 59.7% -DM:86.6% -CKD:79% -CVD:90.3% -Non-hispanic black:64.5% -Non-hispanic white:65.1% 2003–2004 -Women: 70.7% -Men:63.9% - ≥ 60 years: 76.2% −40-59 years: 63.8% -DM:88.2% -CKD:83.9% -CVD:88.9% -Non-hispanic black:66.8% -Non-hispanic white:68.4% 2005–2006 -Women:77.5% -Men:61.5% - ≥ 60 years: 81.2% −40-59 years: 64.8% -DM:87.5% -CKD:85.6% - CVD:89.8% -Non-hispanic black:72.8% -Non-hispanic white:71.9% 2007–2008 -Women: 76.3% -Men:68.5% - ≥ 60 years: 81.7% −40-59 years: 67.7% -DM:91.3% -CKD:87.2% -CVD:90.6% -Non-hispanic black:70.2% -Non-hispanic white:74.9% 2009–2010 -Women: 82.5% -Men:71.7% - ≥ 60 years: 83.6% −40-59 years: 75.7% -DM:93.4% -CKD:88.3% -CVD:94% -Non-hispanic black:75.3% -Non-hispanic white:78.5% |
| Hanselin/ 2011/H1 45 |
United States/ Claims data from the Medstat MarketScan Commercial Claims and Encounter database |
Resistant HTN patients | 18–89 years HTN diagnosis -Taking ≥4 drugs concurrently based on NDC claims −2 drugs must be a 1st line therapy recommended by JNC-7 guideline (ACEIs, ARBs, BBs, CCBs and/or diuretic) -Enrolled in healthcare plan for minimum 12 months |
HF patients | Retrospective analysis | 2009 | Prescription claims | N = 140,126 Men:54.5% Women:45.5% DM:30.5% CKD: 5.7% IHD:3.3% Old MI:1.5% Acute MI: 1.6% |
| Harman/ 2013/H2 46 |
United States/ African-American men and women residents of metropolitan Jackson, Mississippi |
African American hypertensive adults | Population from the Jackson Heart Study currently taking antihypertensive therapy at the time of Exam I and Exam II | Incomplete records or information on medications | Cohort | Exam I: 2000–2004 Exam II: 2005–2008 |
Not mentioned clearly |
Exam I N = 2415 Age: 60 Women:69% BMI: 33 + −7 DM: 29% MI: 9% CKD: 14% Exam II N= 2577 Age: 63 Women:70% BMI: 33 + −7 DM: 40% out of 2078 MI: 9% CKD: 11% |
| Hussain/ 2015/H3 24 |
Karachi, Pakistan/ Liaquat National Hospital Karachi | Adults hypertensive patients and physicians | Not mentioned | Specialists and consultants | Quantitative | June 2012–August 2012 | Two surveys were conducted in health providers and health receivers. Data of prescriptions, prescription trends, and drug prices were obtained from authentic sources. |
N = 400 Males: 50% |
| Ibaraki/2017/I1 25 |
Japan/ 80 dispensing pharmacies |
Adults hypertensive patients | Inclusion ➔ Antihypertensives prescriptions and prescriptions for diabetes, dyslipidemia, hyperuricemia, and antithrombotic |
Not mentioned (prescriptions review) |
2014 | Prescriptions | N = 10,585 Age: −70-79: 33% −60-69: 24.6% −80-89:23.5% -Female: 55.3% |
|
| Ishida/2019/ I2 26 |
Japan/ database built by Medical Data Vision Co., Ltd. (MDV) | Adults hypertensive patients | - Patients with history of an outpatient visit or hospitalization (for any indication) before the index date -patients prescribed of ≥3 drugs that includes loop, and at least one other antihypertensive drug |
- Patients with no history of attendance during this time -those prescribed loop diuretics, or aldosterone antagonists monotherapy or combination therapy |
Cross-sectional study | 2015 | Prescriptions review |
N = 59,867 -Age: 70 + −11.9 -Male:56.9% -DM: 24.3% -Renal disease:10% -Heart disease (inpatient): 52% |
| Khurshid/2012/K1 40 |
India South Delhi/ Medicine Out-Patient Department of University Teaching Hospital |
Adults antihypertensive patients | Hypertensive patients in Outpatient clinic | - Patients not treated with antihypertensives - mentally retarded -unconscious - drug addicts - unable to comply with their medications |
Prospective analysis of drug utilization | 2007 | Medical records and prescriptions |
N = 192 -Males: 45.4% -Females: 54.6% - <30 years: 7.8% - 30-60 years: 70.3% - >60 years: 21.8% |
| Lin/2013/L1 53 |
Taiwan/ 19 hospitals distributed across four geographical areas of Taiwan |
Adults hypertensive patients | Essential HTN diagnosis with no other concomitant diseases | -Secondary HTN HTN diagnosis -History of malignant HTN - History of cerebrovascular accident or TIA within prior 6 months to enrollment - baseline sitting SBP of 210 mmHg - confirmed MI, or a clinically significant cardiac arrhythmia in the past 12 months - cardiac diseases -neurological disorders - hepatic or neoplastic diseases |
Data retrieved from a nested cross-sectional study | 2003–2004 | Medical records and prescriptions |
N = 2145 -Males:1139 (53.1%) -Females: 1006 (46.89%) −20-49 years: 243 (11.32%) - ≥50 years: 1854 (86.4%) -Diabetes:819 (38.18%) - Kidney disease:124 (5.78%) -Cardiac disease: 571 (26.62%) -Cerebrovascular disease: 195 (9.09%) |
| Maghrabi/ 2013/M1 50 |
Western region Saudi Arabia/ 11 hospitals of different types | Physicians (internists, cardiologists, gynecologists, and family doctors) | -Specialties including cardiologists, internists, and family medicine - Minimum 1-year experience in KSA -public and private sectors -specialized and general sectors -all geographical parts of western region -all socioeconomic levels |
Not mentioned | Qualitative study (not mentioned) | Not mentioned | Semi-structured interviews using prescription profile questionnaire |
N = 277 -internists: 80% -cardiologists: 13% -family medicine doctors:7% -general hospitals:50% -specialized hospitals: 50% -private hospitals: 31% -governmental hospitals: 69% Years of practice experience: - < 15 years: 44% - > 15: 56% Years of experience in KSA: - < 2 years: 21% −2-5 years: 52% - > 5 years: 27% |
| Mbui/2017/M2 27 |
Kenya/ outpatient clinic |
Adults Hypertensive patients | - actively registered hypertensive adults above 18 years the MOPC at Ruiru Sub-County hospital for ≥1 - at least 1 antihypertensive agent - patients visiting the clinic at least 3 times/year - complete medical records |
pregnant patients | Descriptive cross-sectional study | 2015 | Retrospective analysis of medical records and semi-structured interviews |
N = 247 Females:87.4% Males: 12.6% Age (years): 20–39: 11.3% 40–59: 44.1% 60–79: 43.3% ≥80: 1.2% Comorbidities: -Diabetes: 36.8% -CVDs: 2% Treatment duration: - ≤ 1 year: 25.5% - >1–5 years: 72.1% - >5–10 years: 1.6% - >10 years: 0.8% |
| Mohd/2012/M3 41 |
India/Pradesh Outpatient clinics in Rohini superspeciality hospital |
Elderly (>65 years old) hypertensive patients |
-Elderly >65 years hypertensive according to JNC-7 guidelines -receiving therapy |
Not mentioned | Prospective observational study | January–June 2011 | Prescriptions and Medical records review |
N = 100 Age (years): 65–67: 72% 68–70: 26% >70: 2% Educational qualification: -Literate: 76% -Illiterate: 24% Social habits: -Alcoholic: 15% -Smoker: 20% -Both: 8% |
| Murti/2015/M4 28 |
North India/ Outpatient department Research Hospital |
Adult hypertensive patients | prescriptions of antihypertensives in four months (Sep. 2013- Dec. 2013) | Not mentioned | Prospective analysis of drug utilization pattern | 2013 | Prescriptions and medical records review |
N = 137 Males:71.5% Females: 28.5% Mean age: Males:58.47 Females: 52.39 Obese: 56.93% comorbidities: 31.38% -DM:16.05% -CVD risk: 5.10% -CKD:8.75% -Asthma/ Respiratory conditions: 1.45% |
| Pandey/2014/P1 29 |
South Delhi, India IIT Hospital outpatient clinics |
Diabetic and/or hypertensive | -newly registered patients' prescriptions -all diabetic and/or HTN patients with at least one drug |
Not mentioned | Prospective drug utilization review | 2014 | Prescription and medical records review |
N = 595 -Males: 57.31% -Females: 42.69% Hypertensive patients: -Males: 30.9% -Females: 23.70% Diabetic patients: -Males: 7.73% -Females: 7.05% Both: -Males: 18.65% -Females: 11.93% |
| Paradkar/ 2017/P2 30 |
India/ Department of medicine Sir JJ group tertiary care hospitals |
Adult hypertensive patients |
Adult hypertensive patients seeking treatment from OPD | Critically ill or pregnant | Drug utilization study | 2017 | Prescription and medical records review | N = 400 Average age: 53 -Females: 51.8% -Males: 48.2% -Newly diagnosed: 42% -follow ups in OPD: 58% -Diabetics: 76.3% -CAD: 4.5% -Hypothyro idism:2.75% -MDD: 1% |
| Pai/2011/P342 | South India/ tertiary care hospital | Adult hypertensive patients | all adult HTN patients even with co-morbid conditions | Not mentioned | Retrospective cross-sectional analysis of prescriptions | 2010 | Prescriptions review and analysis | N = 214 Males: 101 Females: 99 Mean ages (years) -Females: 63.5 -Males:62.7 ≥1 concurrent disease:65% -DM:47.5% -IHD:16.5% -Hyperlipid-emia: 18% -Renal disease:7.5% -CVD accidents :16% |
| Rachana/ 2014/R1 31 |
India Bangalore /tertiary care hospital |
Adult hypertensive patients | ≥18y HTN adults | serious co-morbid illness like CHF, CKD, stroke, dementia, cognitive/sensory deficits, pregnant lactating women | Retrospective cross-sectional study | 2013 | Prescriptions and medical records review |
N = 300 -Male: 54.66% -Female: 45.33% Mean age: -Male: 58.06 -Female: 62.09 HTN stage: -Normal: 8.66% -prehyperte nsion: 25% -Stage 1: 36.33% -Stage 2:30% |
| Ramli/2010/ R2 49 |
Selangor/ Malaysia Public primary clinics |
Adult hypertensive patients | Hypertensive patients treated there | Patients with co-existing DM | Cross-sectional survey | 2009 | Prescription and medical records review | N = 400 -Male:47.2% -Female: 52.8% Ethnicity: -Malays: 49.8% -Chinese: 40% -Indian: 10% -others:0.2% Mean age: 59.5y |
| Sajith/2014/ S1 32 |
Pune/ India Gynaecology and obstetrics Department at Bharati hospital |
Adult pregnant women with HTN | All pregnant women with HTN | Not mentioned | Prospective study | 2014 | Prescription and medical records review |
N = 104 Age (years) 18–22: 41.3% >32: 3.8% -Chronic HTN: 2 -Gestational HTN: 20 -Eclampsia:8 -Preeclamp sia: 74 |
| Shastry/ 2014/S2 33 |
India/ Tertiary care teaching hospital |
Adult diabetic-hypertensive patients | Patients with diabetes and HTN | Not mentioned | Cross-sectional study | 2014 | Patients medical records and prescriptions review |
N = 336 Male: 48.5% Female: 51.5% Mean age: 64.55±9.51 |
| Si/2018/S3 34 |
Australia | Elderly (>65 years) hypertensive patients | Long concession≥65 years hypertensive patients medications dispensing records from 2006 to 2016 | Not mentioned | Prescription data analysis | 2018 | National prescription claims data from the Australian PBS | −1.6 million person-years of observations −1 million person-years involved antihypertensives 2016: -Males: 65.1% -Females: 59.2% |
| Tamirci/ 2019/T1 35 |
Northern Cyprus/ Community pharmacies |
Adult hypertensive patients | Prescriptions of antihypertensive agents | Not mentioned | Prescription analysis | 2017–2018 | Prescriptions22.1 |
N = 148 prescriptions -Average number of antihypertensives /prescription: 1.2±0.6 |
| Tandon/ 2014/T2 36 |
North India/ Teaching tertiary care hospital |
Adult post-menopausal hypertensive women | Adult post-menopausal hypertensive women | Not mentioned | Observational and cross-sectional prospective prescription audit | 2012 | Prescriptions and medical records |
N = 500 prescriptions -Stage I HTN: 59.6% -Stage II HTN: 36% -diabetic: 6.4% -obesity/ overweight: 7.2% |
| Yazdanshenas/2014/ Y1 37 |
South Los Angeles United States/ African American churches |
African American hypertensive patients | African Americans hypertensive adults aged ≥65 years | Exclusion ➔ Not mentioned |
Cross-sectional study | Not mentioned | Survey and face-to-face interviews |
N = 341 ≥75 y: 39% -Female: 65% -Diabetics: 37% -Kidney diseases: 12% |
| Zhou/2015/ Z1 38 |
United States of America/data from IMS Health National Disease and Therapeutic Index | Adults hypertensive patients | Data from IMS Health National Disease and Therapeutic Index (NDTI) on HTN prescriptions | Not mentioned | Drug utilization patterns | Not mentioned | NDTI monthly audit | HTN treatment visits: % −1997:10.3% −1998:10.6% −1999:10.8% −2000:10.9% −2001:10.4% −2002:10.6% −2003: 11% −2004:11.2% −2005: 11% −2006:10.9% −2007:11.2% −2008:11.4% −2009:11.2% −2010:10.9% −2011:10.9% −2012:10.9% |
HTN: HTN, DM: Diabetes Mellitus, IHD: Ischemic heart disease, HF: Heart failure, CKD: Chronic kidney disease, MI: Myocardial infarction, CVD: Cardiovascular disease, CAD: coronary artery disease, SBP: systolic blood pressure, DBP: diastolic blood pressure COPD: Chronic Obstructive Pulmonary Disease, ACEIs: Angiotensin converting enzyme inhibitors, ARBs: Angiotensin receptor blockers, BBs: Beta blockers, CCBs: Calcium channel blockers, CADs: Centrally acting drugs, HCTZ: Hydrochlorothiazide.
Table 3.
Outcomes and findings of included studies.
| Author/ Year/Code | Outcome measures/results (Type of drugs used including % Adherence to guideline Guideline used if any)** |
Adherence to guidelines |
|---|---|---|
| Abdulameer/ 2012/A1 47 |
Essential HTN: Monotherapy:35.3%
Monotherapy:25%
|
Essential HTN adherence: 86.27% HTN + DM adherence: 78.13% HTN + IHD adherence: 95.08% HTN + DM + IHD adherence: 75.92% Total adherence to guidelines: 85.30% Guideline name ➔ Malaysian Guideline |
| Abougalambou/ 2011/A2 48 |
CCBs: 7.01% ACEIs: 18.3% ACEIs + CCBs: 16.8% ARBs + CCBs: 14.32% Achieving target
|
NA |
| Adamu/2017/A3 14 |
Monotherapy:
- CCBs: 52.1% (males) 62.9% (females) - ACEIs: 63.8% (males) 55.4% (females) - BBs: 10.1% (males) 14.9% (females) - ARBs: 2.9% (males) 3.59% (females) Two-drug therapy:
|
NA |
| Adejumo/ 2017/A4 15 |
Overall % - Diuretics: 64.7% - CCBs: 54.9% - ACEIs:44.6% Monotherapy: 17.8% Two drugs: 49.6%
|
NA |
| Alkhaja/2019/A5 16 |
Patients on Monotherapy Young adults:31.37% Older adults:22.64% - ACEIs young adults: 43.40% older adults: 35.64% - Diuretics young adults: 7.30% older adults: 10.90% - CCBs young adults: 12.53% older adults: 20.55% -BBs young adults: 16.95% older adults: 17.19% Patients on Two Drug combination -Perindopril + Indapamide Young adults:28.11% Older adults:16.11% -Valsartan + HCTZ young adults: 24.39% older adults: 22.55% |
NA |
| Alba-Leonel/2016/A6 17 |
Overall
|
NA |
| Alkaabi/2019/A7 18 |
Monotherapy: 32.1% -CCBs: 20.8% -ARBs: 35.7% -Diuretics: 6.4% -ACEIs: 20.2% - BBs: 15.9% Two drug combo: 35.5% - ARBs + CCBs:30.9% -ACEs + CCBs:21.9% -ACEIs + Diuretics:13.8% -ACEIs + BBs: 12.4% Three-drug combo: 23.1% Four drugs combo: 8.2% |
NA |
| Adnan/2010/A8 52 |
General medical services (GMS) ACEIs + ARBs: - January 2000:0.16/1000 GMS eligible population - April 2009: 5.10/1000 GMS eligible population -December 2008: 5.98/1000 GMS eligible population Males: -January 2000: 0.41 -April 2009: 5.90 Females: -January 2000: 0.17 -April 2009: 4.49 -Highest trend of co-prescribing among ≥65 years DM: -January 2000: 0.97 -April 2009: 25.72 HTN: -January 2000: 0.59 -April 2009: 12.72 CHF: -January 2000: 0.77 -April 2009: 12.07 IHD: -January 2000: 0.35 -April 2009: 10.43 |
NA |
| Ahmed/2020/A9 19 |
Amlodipine prescriptions: 465 out of 3540 prescriptions (13.13%) | NA |
| Beg/2014/B120 |
Monotherapy: 75.9% -ARBs: 33.57% -ACEIs:16.79% -BBs: 13.63% -CCBs: 11.91% Dual-therapy: 24.1%
|
NA |
| Bulatova/ 2013/B2 51 |
Monotherapy: 22.3% -ACEIs: 27.5% -ARBs: 23.1% -BBs: 48.4% -CCBs: 14.4% -Thiazides: 5.5% Two drug combination: 27.2% Three drug combination: 27.9% >3 drugs combination: 18.4% |
NA |
| Chang/2016/C1 21 |
Monotherapy: 32% - Thiazide: 16% -ACEIs/ARBs: 43% -CCBs:19.4% BBs: 20.2% Two drugs: 39.1% -Thiazides +ACEIs/ARBs:28.8% -ACEIs/ARBs +BBs:17.4% -ACEIs/ARBs+CCBs = 17.9% |
NA |
| Dhanaraj/ 2012/D1 39 |
Untreated: 4% Monotherapy: 41% - ACEIs: 47% - ARBs: 36% - CCBs: 12% - BBs: 5% Dual therapy: 65% - ACEI+ARB: 21% -ARB + diuretic:18% -ARB + CCB:16% -ACEI+CCB:17% -ACEI+diuretic:13% Three drugs combination: 30% -ACEI+ARB + diuretic: 30% ARB + CCB + diuretic: 21% ≥ 4 or more drugs: 6% |
NA |
| Elmawardy/ 2016/E1 22 |
BBs: 25.6% Diuretics: 24% ACEIs: 21.8% ARBs: 13.9% CCBs: 12.5% Uncontrolled% -ARBs: 49.4% -CCBs: 61.4% -Diuretics: 62.2% -BBs: 63.1% -ACEIs: 63.3% -Centrally Acting Drugs: 69.2% |
NA |
| Rajasekhar et al. /2016/G1 23 |
Monotherapy: 50.76% - CCBs: 50% - ARBs: 32.5% Dual therapy: 42.13% - ARBs+CCBs: 27.71% - BBs + CCBs: 20.48% -CCBs+ diuretics: 19.27% Triple therapy: 6.09% -ARBs+CCBs+ diuretics: 33.3% -ARBs+ACEIs+ diuretics:25% Monotherapy DM: ARBs: 42/105 CCBs: 41/105 BBs: 15/105 ACEIs: 7/105 CVA: ARBs: 15/32 CCBs: 10/32 ACEIs: 4/32 BBs: 3/32 CAD: CCBs: 5/13 ARBs: 4/13 BBs: 4/13 CCF: CCBs: 5/8 ARBs: 3/8 Dual therapy DM: ARBs+CCBs: 28/81 BBs + CCBs: 23/81 CCBs+Diuretics: 14/81 CCBs+ACEIs: 7/81 ARBs+BBs: 2/81 ACEIs+Diuretics: 2/81 BBs + ACEIs: 2/81 ARBs+Diuretics: 1/81 BBs + Diuretics: 1/81 ARBs+ACEIs: 1/81 CVA: ARBs+CCBs: 10/20 BBs + CCBs: 4/20 CCBs+Diuretics: 2/20 ARBs+BBs: 2/20 CCBs+alpha-blockers: 1/20 ARBs+Diuretics: 1/20 CAD: CCBs+Diuretics: 5/14 BBs + CCBs: 4/14 ARBs+ACEIs: 3/14 ARBs+Diuretics: 1/14 CCBs+ACEIs: 1/14 Congestive cardiac failure patients: CCBs+Diuretics: 3/7 BBs + CCBs: 2/7 ARBs+BBs: 1/7 BBs + ACEIs: 1/7 |
NA |
| Grigoryan/ 2013/G2 43 |
Monotherapy:16% Dual therapy: 34% Triple therapy: 50% Uncontrolled resistant HTN - Diuretics:91% -Diuretic/ACEIs/ BBs: 8/34 -Diuretic/ARBs /BBs: 2/34 |
NA |
| Gu/2012/G3 44 |
2001–2002 Diuretics:30% Monotherapy: 2.7% Polytherapy:27.3% Thiazides:22.4% Monotherapy: 1.6% Polytherapy: 20.8% BBs: 20.3% Monotherapy: 4.6% Polytherapy: 15.7% CCBs: 19.2% Monotherapy: 5.5% Polytherapy: 13.7% ACEIs: 25.5% Monotherapy: 9.7% Polytherapy:15.8% ARBs: 10.5% Monotherapy:3% Polytherapy:7% 2003–2004 Diuretics:32.1% Monotherapy: 2.5% Polytherapy: 29.6% Thiazides:24.4% Monotherapy: 1.6% Polytherapy: 22.5% BBs:25.4% Monotherapy:5.9% Polytherapy:19.6% CCBs: 20.7% Monotherapy: 3.8% Polytherapy: 16.9% ACEIs: 29.8% Monotherapy: 8.8% Polytherapy:21% ARBs: 14.5% Monotherapy: 2.9% Polytherapy: 11.6% 2005–2006 Diuretics:34% Monotherapy: 4.8% Polytherapy:29.2% Thiazides: 26.3% Monotherapy: 4.1% Polytherapy: 22.2% BBs: 30.1% Monotherapy: 8.5% Polytherapy: 21.6% CCBs: 21.7% Monotherapy: 3.1% Polytherapy:18.6% ACEIs: 29.4% Monotherapy: 6.9% Polytherapy: 22.5% ARBs: 14.5% Monotherapy:3.2% Polytherapy:11.3% 2007–2008 Diuretics: 34.7% Monotherapy:2.7% Polytherapy:32% Thiazides: 26.7% Monotherapy: 2.1% Polytherapy:24.5% BBs: 27.7% Monotherapy:5.6% Polytherapy:22% CCBs: 19.4% Monotherapy: 3.2% Polytherapy: 16.2% ACEIs: 29.3% Monotherapy: 9.3% Polytherapy:20% ARBs: 20.3% Monotherapy:5.9% Dual:14.4% 2009–2010 Diuretics: 35.8% Monotherapy:3.3% Polytherapy:32.5% Thiazides: 27.6% Monotherapy:2.5% Polytherapy:25.1% BBs: 31.9% Monotherapy:5.9% Polytherapy:25.9% CCBs: 20.9% Monotherapy:3.7% Polytherapy:17.2% ACEIs: 33.3% Monotherapy: 11.2% Polytherapy: 22.2% ARBs: 22.2% Monotherapy: 4.9% Polytherapy: 16.1% |
Guideline used: JNC7 Concordance: yes |
| Hanselin/ 2011/H1 45 |
ACEIs: 60% ARBs: 51.8% BBs: 80% CCBs: 83.6% -Dihydropyridi ne: 69.7% - Non-dihydropyridine: 15% Diuretics: 93.2% -Aldosterone antagonist: 5.9% -Loop: 18.8% -Thiazide: 79.8% -Alpha-1 adrenergic antagonist: 12.2% -Alpha-2 adrenergic agonist: 14.1% |
NA |
| Harman/ 2013/H2 46 |
Exam I: BP control with: -Thiazide: 54% -Dihydropyridine CCBs: 24% -Non-dihydropyridine CCBs: 14% -ACEIs: 38% -BBs: 23% -ARBs: 17% -Loop: 11% -Potassium sparing: 15% Monotherapy -Thiazide: 31% -CCBs: 25% -ACEIs: 20% -BBs: 9% -ARBs: 7% Exam II: BP control with: Thiazide: 59% -Dihydropyridine CCBs: 27% -Non-dihydropyridine CCBs: 11% -ACEIs: 38% -BBs: 23% -ARBs: 30% -Loop: 12% -Potassium sparing: 16% Monotherapy -Thiazide: 35% |
NA |
| Hussain/ 2015/H3 24 |
Patients survey results: -BBs: 33% -ACEIs: 18% -CCBs:13% -ARBs: 8% -Non-thiazide diuretics:8% Physicians' survey results for first line medication without indication: -Diuretics: 17% -ACEIs: 34% -CCBs: 4% -BBs: 34% |
NA |
| Ibaraki/2017/I1 25 |
CCBs: 73.5% ARBs: 62.7% ACEIs: 6.1% Diuretics: 16.5% BBs: 13.6% Alpha-blocker: 2.4% DM patients: Monotherapy ACEIs: 53.1% CCBs: 43% Combination therapy -CCB and ARB was the most frequent prescription pattern in patients taking two antihypertensive drugs |
NA |
| Ishida/2019/ I2 26 |
With heart disease: -CCBs: 65.3% -ARBs: 57.5% -BBs: 39.9% -Loop: 17.7% -Thiazide: 10.2% -ACEIs: 11.8% -Aldosterone antagonists: 8.8% -Alpha blocker:4.8% -Direct renin inhibitor: 0.5% Without heart disease: -CCBs: 68.5% -ARBs: 62.4% -BBs: 10.9% -Loop: 3% -Thiazide: 9.5% -ACEIs: 6.2% -Aldosterone antagonists: 1.7% -Alpha blocker:4.4% -Direct renin inhibitor: 0.3% Monotherapy Overall population: CCBs: ≈ 48% ARBs: ≈ 35% BBs: ≈ 11% ACEIs: ≈ 4% Alpha-blockers: ≈ 2% Diuretics (Thiazides): ≈ 1% DM patients: CCBs: ≈ 34% ARBs: ≈50% BBs: ≈8% ACEIs: ≈ 7% Alpha-blockers: ≈ 1% Diuretics (Thiazides): ≈ 0.5% Renal disease patients: CCBs: ≈ 42% ARBs: ≈ 36% BBs: ≈ 14% ACEIs: ≈ 5% Alpha-blockers: ≈ 4% Diuretics (Thiazides): ≈ 2% 2-drug combinations: Overall population: CCBs+ARBs: ≈ 60% CCBs+BBs: ≈9% ARBs+BBs: ≈ 6% CCBs+ACEIs: ≈ 5% ARBs+Diuretics (Thiazides): ≈ 4% Other combinations: ≈ 15% DM patients: CCBs+ARBs: ≈ 63% CCBs+BBs: ≈ 7% ARBs+BBs: ≈ 8% CCBs+ACEIs: ≈ 6% ARBs+Diuretics (Thiazides): ≈ 4% Other combinations: ≈ 14% Renal disease patients: CCBs+ARBs: ≈ 47% CCBs+BBs: ≈ 8% ARBs+BBs: ≈ 6% CCBs+ACEIs: ≈ 5% ARBs+Diuretics (Thiazides): ≈ 2% Other combinations: ≈ 32% 3-drug combinations: Overall population: CCBs+ARBs+BBs: ≈29% CCBs+ARBs+Diuretics (Thiazides): ≈ 21% CCBs+ARBs+Diuretics (Loop): ≈ 8% CCBs+ARBs+Alpha-blockers: ≈ 6% CCBs+BBs + ACEIs: ≈ 4% Other combinations: ≈ 33% DM patients: CCBs+ARBs+BBs: ≈ 26% CCBs+ARBs+Diuretics (Thiazides): ≈ 20% CCBs+ARBs+Diuretics (Loop): ≈ 10% CCBs+ARBs+Alpha-blockers: ≈ 8% CCBs+BBs + ACEIs: ≈ 4% Other combinations: ≈ 33% Renal disease patients: CCBs+ARBs+BBs: ≈ 20% CCBs+ARBs+Diuretics (Thiazides): ≈ 10% CCBs+ARBs+Diuretics (Loop): ≈ 27% CCBs+ARBs+Alpha-blockers: ≈ 7% CCBs+BBs + ACEIs: ≈ 4% Other combinations: ≈ 45% |
NA |
| Khurshid/2012/K1 40 |
Overall pattern: -Diuretics: 42.2% - BBs: 41.2% - CCBs: 39.1% - ACEIs: 26% - ARBs: 23.4% - alpha-1 blockers: 23.4% Monotherapy (45.3%): - BBs: 28.8% - Diuretics: 24.1% - CCBs: 21.8% - ACEIs: 18.4% - ARBs: 5.7% - alpha-1 blockers: 1.1% Multiple drug therapy (54.7%) - Two drug combination: 75.2% -CCB + BBs: 40.9% - ACEIs +diuretics:14.3% Three drug combination: 18.0% |
NA |
| Lin/2013/L1 53 |
-Diuretics: 20.8% -BBs: 38.7% -CCBs: 59.3% -ACEIs: 20.4% -ARBs: 38.7% -Monothera py: 775 (36.13%) -Dual-drug therapy:864 (40.27%) -Triple-drug therapy:388 (18.08%) - Quadro-drug therapy:75 (3.5%) Diuretics: DM patients: 17.5% CVD patients: 27.7% Cerebrovascular disease patients: 16.4% Kidney disease patients: 29.8% BBs: DM patients: 32.5% CVD patients: 43.6% Cerebrovascular disease patients: 38.5% Kidney disease patients: 36.2% CCBs: DM patients: 58.4% CVD patients: 57.8% Cerebrovascular disease patients: 65.1% Kidney disease patients: 52.4% ACEIs: DM patients: 22.3% CVD patients: 22.2% Cerebrovascular disease patients: 28.2% Kidney disease patients: 25% ARBs: DM patients: 42.7% CVD patients: 44.5% Cerebrovascular disease patients: 36.9% Kidney disease patients: 39.5% |
NA |
| Maghrabi/ 2013/M1 50 |
Mild uncomplicated HTN in all hospitals: BBs: ≈ 8% Diuretics: ≈30% ACEIs: ≈ 32% CCBs: ≈ 20% Direct vasodilators: ≈ 3% ARBs: ≈ 9% COMB: ≈ 10% Severe uncomplicated HTN in all hospitals: BBs: ≈ 11% Diuretics: ≈ 14% ACEIs: ≈ 12% CCBs: ≈ 15% Amlodipine: ≈ 5% Direct vasodilators: ≈ 20% ARBs: ≈ 3% COMB: ≈ 40% Young uncomplicated HTN in all hospitals: BBs: ≈ 25% Diuretics: ≈ 13% ACEIs: ≈ 30% CCBs: ≈ 23% Direct vasodilators: ≈ 1% ARBs: ≈ 5% COMB: ≈ 7% Pregnant uncomplicated HTN: BBs: ≈ 6% Diuretics: ≈ 4% CCBs: ≈ 10% Amlodipine: ≈ 60% Direct vasodilators: ≈ 17% COMB: ≈ 5% HTN+ renal disease in all hospitals: BBs: ≈ 7% Diuretics: ≈ 7% ACEIs: ≈ 23% CCBs: ≈ 40% Amlodipine: ≈ 5% Direct vasodilators: ≈ 7% ARBs: ≈ 7% COMB: ≈ 6% HTN + DM BBs: ≈ 0.5% Diuretics: ≈ 3% ACEIs: ≈ 72% CCBs: ≈ 7% Amlodipine: ≈ 1% Direct vasodilators: ≈ 1% ARBs: ≈ 12% COMB: ≈ 5% |
NA |
| Mbui/2017/M2 27 |
Overall ACEIs: 48.2% ARBs: 27.1% CCBs: 26% BBs: 28.7% Thiazide diuretics: 40.5% Other diuretics:4.8% Methyldopa: 0.8% Hydralazine: 0.8% Monotherapy ACEI:20.2% ARB:8.5% BB:4.5% Thiazide:3.6% CCB:3.2% Two drug Combination -Thiazide diuretic + ACEI: 14.2% -CCB + ARB: 14.2% - CCB + BB:6.1% - Thiazide diuretic + BB:4.9% - CCB + thiazide diuretic:4.9% |
NA |
| Mohd/2012/M3 41 |
CCBs: -Amlodipine: 38% ARBs: -Losartan: 11% -Telmisartan: 10% BBs: -Atenolol: 6% -Metoprolol: 5% Diuretics: -HCTZ: 1% -Furosemide: 1% DM: -Losartan:3% -Telmisartan: 4% -Amlodipine: 5% -Telmisartan+ HCTZ: 1% CVA
|
NA |
| Murti/2015/M4 28 |
Monotherapy: 27.73% Multidrug therapy: 72.26%
-Diuretics: 29.90%/28.94% -ACEIs: 22.42%/18.42% -ARBs: 17.75%/10.52% -BBs: 25.23%/18.42% -CCBs: 26.16%/23.68% Dual therapy: -CCBs+BBs: 18.97% -ARBs/ACEIs+ diuretics: 8.75% -ARBs/ACEIs+ CCBs: 5.1% -ACEIs+BBs: 3.64% -CCBs+diuretics: 13.13% |
Guideline adherence: Yes Name of guideline: JNC7 |
| Pandey/2014/P1 29 |
ACEIs:19.18% BBs: 17.56% Amlodipine: 15% Atenolol+amlodipine: 14.05% |
NA |
| Paradkar/ 2017/P2 30 |
-Enalapril:60% -Amlodipine: 56.3% -Atenolol: 12% -Chlorthalido ne: 1% Diabetics: -Enalapril:59% -Amlodipine: 39.7% -Atenolol: 1.3% -Monotherapy: 71.8% -Dual-therapy: 24.8% -Triple-therapy: 3.4% |
Concordance to JNC8: 87.5% |
| Pai/2011/P342 |
Multiple drug therapy: 51% −2 drugs: 67.7% −3 drugs: 27.5% −3 drugs and more: 4.9% -ARB + diuretic (25.4%) most frequently prescribed two-drug combination followed by a combination of two diuretics (10.8%) and CCBs+ BBs (9.8%) Monotherapy: 49% Overall: -Diuretics: 43.5% -ACEIs: 29.5% -ARBs: 21% -CCBs: 49% -BBs: 29% -Prazosin: 2% -Clonidine:2% DM patients: Overall -Diuretics: 43.1% -ACEIs: 40% -ARBs: 17.9% -BBs:26.3% -CCBs: 29.5% 2 drug combination:42.1% Diuretics + diuretics/CCB/ARB/BB/ACEI: 29.4% Other combinations (CCB + ACEI, CCB + BB, ARB + CCB,ACEI + CCB, ACEI + BB): 12.6% 3 drug combination: 6.3% 4 drug combination: 2.1% |
NA |
| Rachana/ 2014/R1 31 |
-Monotherapy: 48.94% -Polytherapy: 16.01% -Fixed-dose combination: 35.04% Overall: BBs: 24.07% CCBs: 38.59% Diuretics: 13.2% ARBs: 17.35% ACEIs: 6.21% Alpha-blockers:0.51% Monotherapy BBs: 25.3% CCBs: 41.97% Diuretics: 5.55% ARBs: 19.13% ACEIs: 6.79% Alpha-blockers:1.23% Fixed dose combination Thiazide+ARBs:45.68% BBs + CCB:23.27% Thiazide+CCB:10.34% Thiazide+ACEIs:9.48% Polytherapy BBs + CCBs:56.66% BBs + ARBs:9.43% |
NA |
| Ramli/2010/ R2 49 |
-Monotherapy: 45.7% -Dual therapy: 43.3% −3 or more agents: 11% Monotherapy -BBs: 31.1% -CCBs (sa): 29% -ACEIs: 13.7% -CCBs(la): 12.6% -Diuretics: 12% -Alpha-blocker: 1.6% |
NA |
| Sajith/2014/ S1 32 |
Combination therapy: 67.31% CAD + CCB: 28.8% CCB + BB:11.5% CAD + CCB+ BB:15.4% Monotherapy: 32.69% -Centrally-acting antiadrenergic drugs: 17.3% -CCBs: 15.4% |
|
| Shastry/ 2014/S2 33 |
Overall on Diuretics: 13.4% -HCTZ: 45 patients -Furosemide: 28 patients -Spironolacto ne: 23 patients Diuretics monotherapy: 4.4% Two drug combo: 35.6% Diuretic+ACEIs: 17.7% Diuretic+ARBs: 13.33% Three drug combo: 46.7% Diuretic+ARBs+BBs:13.33% Diuretic+ARBs+CCBs: 11.11% Four drug combo: 13.3% |
NA |
| Si/2018/S3 34 |
2006 ACEIs/ARBs: ≈55% CCBs: ≈ 30% BBs: ≈ 28% ACEIs/ARBs (FDC): ≈ 25% Other diuretics: ≈ 17% Low ceiling diuretics: ≈ 10% Other antihypertensives: ≈ 6% 2007 ACEIs/ARBs: ≈57% CCBs: ≈ 30% BBs: ≈ 29% ACEIs/ARBs (FDC): ≈ 26% Other diuretics: ≈ 16% Low ceiling diuretics: ≈ 10% Other antihypertensives: ≈ 6% 2008 ACEIs/ARBs: ≈57% CCBs: ≈ 29% BBs: ≈ 29% ACEIs/ARBs (FDC): ≈ 28% Other diuretics: ≈ 17% Low ceiling diuretics: ≈ 8% Other antihypertensives: ≈ 7% 2009 ACEIs/ARBs: ≈58% CCBs: ≈ 29% BBs: ≈ 29% ACEIs/ARBs (FDC): ≈ 28% Other diuretics: ≈ 17% Low ceiling diuretics: ≈ 8% Other antihypertensives: ≈ 7% 2010 ACEIs/ARBs: ≈ 59% CCBs: ≈ 28% BBs: ≈ 28% ACEIs/ARBs (FDC): ≈ 27% Other diuretics: ≈ 15% Low ceiling diuretics: ≈ 7% Other antihypertensives: ≈ 5% 2011 ACEIs/ARBs: ≈ 58% CCBs: ≈ 26% BBs: ≈ 26% ACEIs/ARBs (FDC): ≈ 30% Other diuretics: ≈ 15% Low ceiling diuretics: ≈ 6% Other antihypertensives: ≈ 6% 2012 ACEIs/ARBs: ≈ 58% CCBs: ≈ 28% BBs: ≈ 26% ACEIs/ARBs (FDC): ≈ 31% Other diuretics: ≈ 15% Low ceiling diuretics: ≈ 5% Other antihypertensives: ≈ 5% 2013 ACEIs/ARBs: ≈ 57% CCBs: ≈ 27% BBs: ≈ 30% ACEIs/ARBs (FDC): ≈ 31% Other diuretics: ≈ 15% Low ceiling diuretics: ≈ 5% Other antihypertensives: ≈ 6% 2014 ACEIs/ARBs: ≈ 55% CCBs: ≈ 25% BBs: ≈ 31% ACEIs/ARBs (FDC): ≈ 32% Other diuretics: ≈ 16% Low ceiling diuretics: ≈ 4% Other antihypertensives: ≈ 6% 2015 ACEIs/ARBs: ≈ 55% CCBs: ≈ 24% BBs: ≈ 30% ACEIs/ARBs (FDC): ≈ 33% Other diuretics: ≈ 17% Low ceiling diuretics: ≈ 3% Other antihypertensives: ≈ 6% 2016 ACEIs/ARBs: ≈ 54% CCBs: ≈ 23% BBs: ≈ 31% ACEIs/ARBs (FDC): ≈ 33% Other diuretics: ≈ 17% Low ceiling diuretics: ≈ 3% Other antihypertensives: ≈ 5% |
NA |
| Tamirci/ 2019/T1 35 |
-BBs: 22.1% -ARBs: 22.1% -CCBs: 20.4% -ACEIs: 17.7% -Diuretics: 13.8% -Anti-adrenergic drugs:3.9% Monotherapy: 73.0% Dual combinations:23% -ARBs+diuretics (52.9%) -Loop diuretics + potassium spairing diuretics (11.8%) -CCB + ARBs (8.8%) -BBs + ARBs (5.9%) - CCBs +antiadrenergics (5.9%) Triple combination: 4% |
NA |
| Tandon/ 2014/T2 36 |
Monotherapy -ARBs: 24.8% -CCBs: 19.4% -ACEIs: 11% -BBs: 2.8% -Diuretics: 2% -Dual-therapy: 31.6% -Triple-therapy: 2.2% -Four drugs: 1% |
Adherence to guidelines - Stage 1: 100% - Stage 2: 43.32% Guideline name: JNC7 |
| Yazdanshenas/2014/ Y1 37 |
Monotherapy: 29% -ACEIs/ARBs: 43% -CCBs: 27% -BBs: 12% -Diuretics: 18% Dual therapy: 35% -ACEI/ARB + CCB: 27% -ACEI/ARB + diuretics: 22% -ACEI/ARB + BB: 17% -CCB + diuretics (14%); Triple therapy: 22% -Diuretics +ACEI/ARB + BB: 39% -ACEI/ARB + CCB + diuretics: 17% -BB + CCB + diuretics: 16% -ACEI/ARB+ BB + CCB:28% Four drugs combo: 9% DM OR CKD: Monotherapy: 26% (Most common ACEIs/ARBs or CCBs) Dual therapy: 38% (Most common ACEI/ARB + diuretics or ACEI/ARB + CCB) Three agents: 23% (Most common combinations were ACEI/ARB + BB + CCB or ACEI/ARB + BB + Diuretics) |
NA |
| Zhou/2015/ Z1 38 |
-Amlodipine and Lisinopril: most commonly prescribed over the examined period Most commonly prescribed in 2012: -Lisinopril -Amlodipine -Metoprolol -HCTZ -HCTZ/ Lisinopril -Losartan -Atenolol -Valsartan -HCTZ/ Triamterene -HCTZ/ Valsartan |
NA |
3. Results
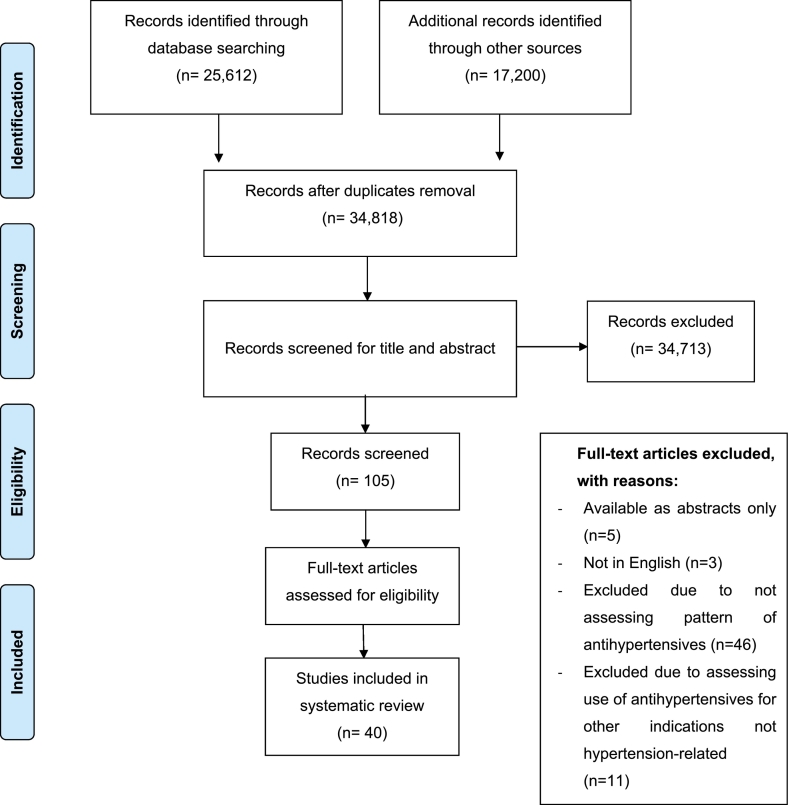
The search of electronic databases identified 25,612 records, in addition to 17,200 records identified from Google Scholar®. Forty articles were found eligible for inclusion after removal of duplicates, screening of abstracts and assessment of full-text articles as per the study's eligibility criteria. Fig. 1 illustrates the flow diagram of articles' inclusion as recommended by Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) checklist.11
Fig. 1.
PRISMA flow diagram.
Table 2 summarizes the studies' characteristics and Table 3 presents the main outcomes and results of the included studies.
3.1. Study characteristics
3.1.1. Study date and country of publication
Most of the studies (n = 25 out of 40)14, 15., 16., 17, 18, 19., 20., 21, 22., 23., 24., 25., 26, 27., 28, 29, 30, 31., 32., 33, 34, 35, 36., 37., 38. were published between 2014 and 2020. The majority of studies were conducted in India (n = 13),20,23,28, 29, 30, 31., 32., 33,36,39, 40, 41., 42. followed by United States (USA) (n = 6),21,37,38,43., 44., 45., 46 and Malaysia (n = 3).47., 48., 49 Other studies were conducted in Japan (n = 2),25,26 Nigeria (n = 2),14,15 Saudi Arabia (n = 2),19,50 Egypt (n = 1),22 Jordan (n = 1),51 Pakistan (n = 1),24 Bahrain (n = 1),16 Kenya (n = 1),27 Australia (n = 1),34 Cyprus (n = 1),35 Ireland (n = 1),52 United Arab Emirates (n = 1),18 Taiwan (n = 1),53 and Mexico (n = 1).17
3.1.2. Study setting
Fifteen studies were executed in hospitals,15,18, 19., 20.,23,24,30, 31., 32., 33,36,39,42,50,53 while 10 studies were conducted in outpatient clinics.14,22,27., 28, 29,40,41,47,48,51 Six studies were based on national prescribing databases,26,34,38,44,45,52 and four studies were conducted in primary care centers.16,17,43,49 Two studies were conducted in pharmacies25,35 and one study was in five clinical sites.21 One study involved African American men and women residents of metropolitan Jackson, Mississippi46 and one study was done in African American churches located in South Los Angeles.37
3.1.3. Study design
The predominant study design utilized by most studies was cross-sectional design (n = 16)14,17,22,26,27,31,33,36,37,39,42,44,47,49,51,53 followed by 11 retrospective studies.15,16,19,24,25,30,34,35,38,45,52 Ten studies adopted a prospective study design.18,20,23,28,29,32,40,41,46,48 Two studies were based on randomized controlled trials (RCTs)21,43 and one study was qualitative using semi-structured interviews.50
3.1.4. Patients' characteristics
The majority of studies included adult hypertensive patients aged 18 years and above (n = 25),14,15,17, 18, 19., 20., 21, 22., 23., 24., 25., 26, 27., 28,30,31,35,38,40,43,44,49,51, 52., 53 while three studies were conducted among elderly patients only.16,34,41 Two studies included only African American hypertensive patients37,46 while the rest included patients regardless of their ethnicity.
The number of study participants in included studies ranged from 100 patients41 to 140,126 patients.45 Four studies specifically targeted patients with type 2 diabetes29,33,39,48 and one study included patients with diabetes and those with IHD.47 One study targeted patients with resistant hypertension.45
3.2. Prescribing patterns of antihypertensive agents
The prescribing patterns of antihypertensive medications across the different studies included in the review are presented in Table 3. The prescribing patterns of antihypertensive agents varied across the 40 included studies. In the subsections below, we synthesized and stratified the data in relation to the prescribing patterns of antihypertensives among adult patients in studies that did not provide specific information for patients with different comorbidities, adult patients in studies that provided specific information for patients with different comorbidities, diabetic patients with hypertension, elderly patients with hypertension, African American patients, and pregnant patients with hypertension.
3.2.1. Prescribing patterns of antihypertensives among adult patients in studies that did not provide specific information for patients with different comorbidities
Twenty-two studies assessed the prescribing of antihypertensives among adult patients without providing prescribing data for different patient sub-populations, particularly those with comorbidities.14, 15., 16., 17, 18, 19., 20., 21, 22.,24,27., 28, 29,31,35,38,40,43., 44., 45.,49,51 Of these, 15 studies provided prescribing data for antihypertensives as monotherapy, dual therapy or combination therapy.14, 15., 16.,18,20,21,27,28,31,35,40,43,44,49,51
The percentage of patients on monotherapy ranged in these studies from 15.8% among females in a Nigerian study14 to 75.9% in a study conducted in India.20 The most commonly used antihypertensive agents as monotherapy were ACEIs or ARBs in eight studies,14,16,18,20,21,27,44,51CCBs in six studies,14,18,28,31,40,49 BBs in 5 studies,16,31,40,49,51 and diuretics in three studies.14,28,40
On the other hand, 11 studies reported the percentage of patients on dual therapy.14,15,18,20,21,28,31,35,43,49,51 This percentage ranged from 23.0% in a study conducted in Cyprus35 to 64.7% in a study done in North India.39 The most common dual therapy was (thiazide diuretics+ACEIs/ARBs) (n = 9),14, 15., 16.,20,21,27,31,35,40 (BBs + CCBs) (n = 4),20,28,31,40 (CCBs+ACEIs/ARBs) (n = 3),18,21,27 and (thiazide diuretics+CCBs) (n = 2).14,28 Furthermore, the use of triple therapy was reported in seven studies18,28,35,40,43,49,51 with the percentage of prescribing varying from 4.0%35 to 50.0%.43
Seven studies reported the overall percentage of patients using a specific class of antihypertensive agents.15,17,27,28,35,40,44 Diuretics were the most commonly used antihypertensives in four studies (57.1%),15,28,40,44 while ACEIs/ARBs were the most commonly used agents in two studies (28.6%).27,35
3.2.2. Prescribing patterns of antihypertensives among adult patients in studies that provided information for patients with specific comorbidities
Eight studies assessed the prescribing patterns of antihypertensives among adult healthy patients, while providing prescribing data for patients with specific comorbidities.23,25,26,30,42,47,50,53 Five studies reported the percentage of patients on monotherapy23,30,42,47,53 with the percentage ranged from 35.3% in a study in Malaysia47 to 71.8% in a study in India.30 Three studies reported the most common agents used as monotherapy23,26,47 with two studies stating that CCBs were the most commonly used agents as monotherapy23,26 and BBs were the most frequently agents in one study.47
Four studies reported the percentage of patients on dual therapy23,30,47,53 ranging from 24.8% in a study in India30 to 47.1% in a study in Malaysia.47 The most common dual combination therapy was (ARBs+CCBs) in two studies23,26 and (ARBs+diuretics) in one study.42
Overall prescribing of antihypertensives was presented in five studies.25,30,42,50,53 CCBs were the most commonly prescribed agents in three studies,25,30,53 while ACEIs and diuretics were the most common agents in two studies respectively.42,50
3.2.3. Prescribing patterns of antihypertensives among adult hypertensive patients with diabetes
Fourteen studies assessed the prescribing patterns of antihypertensive medications among hypertensive patients with diabetes.23,25,30,33,37,39,41,42,47,48,50,52,53 Eight studies reported ACEIs/ARBs as the most commonly used antihypertensives as monotherapy.23,25,26,30,37,39,47,48 The percentage of diabetic patients on monotherapy varied from 25.0%47 to 71.8%.30 Seven studies reported the most commonly used antihypertensives as dual therapy23,25,26,33,37,39,48 with (ACEIs/ARBs+CCBs) being the most common combination in five studies.23,25,26,37,48 Five studies reported the percentage of diabetic patients on dual therapy30,33,37,39,42 with percentages ranging from 24.8%30 to 65.0%.39 Six studies presented the proportion of diabetic patients on triple antihypertensive therapy.26,30,33,37,39,42 One study reported the prescribing patterns of antihypertensive agents among patients with different comorbidities in Taiwan including those with diabetes.53 CCBs, ARBs, and BBs were prescribed to 58.4%, 42.7%, and 32.5% of diabetic patients,53 respectively. Another study indicated that 72% of diabetic patients in Saudi Arabia receive ACEIs.50
3.2.4. Prescribing patterns of antihypertensives among patients with ischemic heart disease or other heart diseases
Five studies investigated the prescribing of antihypertensives in patients with IHD or other heart diseases.23,26,47,52,53 According to a study conducted in Taiwan, CCBs, ARBs, and BBs were prescribed to 57.8%, 44.5%, and 43.6% of patients with hypertension and CVDs, respectively.53 In another study among hypertensive patients with CVDs in Japan, 65.3%, 57.5%, and 39.9% were on CCBs, ARBs, and BBs, respectively.26 Another study in 2012 in Malaysia indicated that about 83.0% of patients with hypertension and IHD were prescribed a combination of ACEIs and BBs.47 A study in 2016 in India found that CCBs were the most commonly used agents as monotherapy and CCBs combined with diuretics were the most common dual therapy in patients with hypertension and CAD.23
3.2.5. Prescribing patterns of antihypertensives among patients with chronic kidney disease or other renal diseases
Three studies investigated the prescribing of antihypertensives among patients with CKD or renal disease.26,50,53 The most common antihypertensive agents used as monotherapy in one study were CCBs and ARBs.26 In addition, the most common two-drug combination was CCBs plus ARBs.26 Similarly, in another study in Taiwan 52.4%, 39.5%, and 36.2% of patients with hypertension and kidney disease were receiving CCBs, ARBs, and BBs, respectively.53 Another study in Saudi Arabia reported that 40.0% of hypertensive patients with kidney disease were on CCBs, while 23.0% were on ACEIs.50
3.2.6. Prescribing patterns of antihypertensives among elderly patients with hypertension
Three studies investigated the prescribing of antihypertensives among elderly patients with hypertension.16,34,41 In two of the three studies, ACEIs/ARBs were the most frequently prescribed agents.16,34 The other remaining study reported that CCBs, specifically amlodipine are as the most prescribed antihypertensive agents.41 Another study presented the prescribing data for antihypertensives among post-menopausal women with hypertension. In this sub-population, ARBs were the most frequently prescribed antihypertensives.36
3.2.7. Prescribing patterns among African American patients
Two studies presented the prescribing patterns of antihypertensives among African American patients with hypertension.37,46 In the first study,46 thiazide diuretics were identified as the most commonly prescribed antihypertensives as monotherapy, while in the other study, ACEIs or ARBs were reported as the most prescribed antihypertensives as monotherapy.37
3.2.8. Prescribing patterns of antihypertensives among pregnant patients with hypertension
Two studies outlined the prescribing of antihypertensives among pregnant patients with hypertension.32,50 Amlodipine was the most commonly prescribed agent in pregnant patients with uncomplicated hypertension in one study in Saudi Arabia,50 while centrally acting agents were the most frequently prescribed agents in another study in India.32
3.3. Adherence of antihypertensives prescribing to clinical practice guidelines
Of the 40 studies included in the review, only four studies directly assessed the prescribing patterns of antihypertensives in adherence to clinical practice guidelines.28,36,44,47 The guidelines included JNC 7 (n = 3)28,36,44 and Malaysian guidelines (n = 1).47 Two studies confirmed adherence of antihypertensives prescribing to guidelines.28,44 Abdulameer et al. study suggested 85.3% total adherence to guidelines47 while Tandon et al. found 100.0% adherence to guidelines in patients with stage 1 hypertension and 43.32% adherence in stage 2 hypertension.36
3.4. Quality assessment of included studies
CCAT scores were computed to assess the quality of each included study (Table 4). The 25th, 50th and the 75th percentiles were 40.6%, 51.3% and 61.3%, respectively. Ten articles (25.0%) were considered of low quality, while 10 articles (25.0%) were considered of high quality. The average scores for each domain of the CCAT tool were calculated for the 40 included articles. The lowest average score was 1.6 for sampling, followed by 2.1 for data collection. The highest average domain score was 3.3 for ethical matters.
Table 4.
Quality of studies used assessed using Crowe Critical Appraisal Tool (CCAT) in scores and percentages.
| Preliminaries [/5] | Introduction [/5] | Design [/5] | Sampling [/5] | Data collection [/5] | Ethical matters [/5] | Results [/5] | Discussion [/5] | Total [/40] | |
|---|---|---|---|---|---|---|---|---|---|
| Abdulameer, et al./ 201247 | 4 | 5 | 4 | 2 | 5 | 4 | 4 | 3 | 31 (77.5%) |
| Abougalambou, et al./ 201148 | 4 | 3 | 2 | 1 | 1 | 4 | 3 | 3 | 21 (52.5%) |
| Adamu, et al./ 201714 | 4 | 4 | 3 | 2 | 2 | 4 | 3 | 3 | 25 (62.5%) |
| Adejumo, et al./ 201715 | 3 | 3 | 2 | 3 | 2 | 4 | 3 | 2 | 22 (55%) |
| AlKhaja, et al./ 201916 | 4 | 4 | 3 | 4 | 2 | 4 | 4 | 4 | 29 (72.5%) |
| Alba-Leonel, et al./ 201617 | 4 | 2 | 3 | 1 | 1 | 1 | 3 | 3 | 18 (45%) |
| Alkaabi, et al./ 201918 | 3 | 3 | 3 | 3 | 3 | 5 | 4 | 4 | 28 (70%) |
| Adnan, et al./ 201052 | 4 | 3 | 3 | 1 | 3 | 1 | 3 | 4 | 22 (55%) |
| Ahmed, et al./ 202019 | 1 | 2 | 1 | 1 | 1 | 4 | 2 | 1 | 13 (32.5%) |
| Beg, et al./ 201420 | 3 | 2 | 1 | 1 | 1 | 3 | 2 | 2 | 15 (37.5%) |
| Bulatova, et al./ 201351 | 3 | 2 | 2 | 1 | 1 | 4 | 3 | 3 | 19 (47.5%) |
| Chang, et al./ 201621 | 3 | 4 | 3 | 1 | 2 | 4 | 3 | 3 | 23 (57.5%) |
| Dhanaraj, et al./ 201239 | 3 | 3 | 3 | 1 | 2 | 3 | 4 | 3 | 22 (55%) |
| Elmawardy, et al./ 201622 | 4 | 3 | 3 | 1 | 2 | 3 | 3 | 3 | 22 (55%) |
| Rajasekhar Giri, et al./ 201623 | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 13 (32.5%) |
| Grigoryan, et al./ 201343 | 2 | 2 | 3 | 1 | 3 | 2 | 3 | 3 | 19 (47.5%) |
| Gu, et al./ 201244 | 5 | 5 | 5 | 4 | 5 | 4 | 5 | 5 | 38 (95%) |
| Hanselin, et al./ 201145 | 4 | 4 | 4 | 5 | 4 | 4 | 3 | 4 | 32 (80%) |
| Harman, et al./ 201346 | 3 | 4 | 1 | 1 | 1 | 3 | 2 | 2 | 17 (42.5%) |
| Hussain, et al./ 201524 | 2 | 2 | 2 | 1 | 2 | 4 | 4 | 3 | 20 (50%) |
| Ibaraki, et al./ 201725 | 2 | 1 | 1 | 1 | 2 | 3 | 3 | 3 | 16 (40%) |
| Ishida, et al./ 201926 | 3 | 3 | 3 | 3 | 3 | 4 | 4 | 4 | 27 (67.5%) |
| Khurshid, et al./ 201240 | 3 | 3 | 2 | 1 | 2 | 4 | 3 | 2 | 20 (50%) |
| Lin, et al./ 201353 | 4 | 3 | 4 | 1 | 3 | 5 | 4 | 4 | 28 (70%) |
| Maghrabi, et al./ 201350 | 3 | 4 | 2 | 1 | 2 | 1 | 2 | 2 | 17 (42.5%) |
| Mbui, et al./ 201727 | 2 | 2 | 4 | 4 | 3 | 5 | 3 | 4 | 27 (67.5%) |
| Mohd, et al./ 201241 | 3 | 2 | 2 | 1 | 2 | 3 | 3 | 2 | 18 (45%) |
| Murti, et al./ 201528 | 2 | 3 | 1 | 1 | 2 | 1 | 2 | 1 | 13 (32.5%) |
| Pandey, et al./ 201429 | 3 | 2 | 1 | 1 | 1 | 5 | 2 | 1 | 16 (40%) |
| Paradkar, et al./ 201730 | 4 | 4 | 1 | 5 | 2 | 4 | 3 | 3 | 26 (65%) |
| Pai, et al./ 201142 | 3 | 2 | 2 | 1 | 1 | 5 | 3 | 2 | 19 (47.5%) |
| Rachana, et al./ 201431 | 3 | 3 | 2 | 1 | 2 | 5 | 3 | 3 | 22 (55%) |
| Ramli, et al./ 201049 | 3 | 4 | 2 | 1 | 1 | 1 | 2 | 2 | 16 (40%) |
| Sajith, et al./ 201432 | 3 | 2 | 1 | 1 | 1 | 1 | 3 | 2 | 14 (35%) |
| Shastry, et al./ 201433 | 2 | 3 | 1 | 1 | 1 | 4 | 2 | 2 | 16 (40%) |
| Si, et al./ 201834 | 2 | 2 | 3 | 1 | 3 | 4 | 4 | 4 | 23 (57.5%) |
| Tamirci, et al./ 201935 | 2 | 2 | 1 | 1 | 2 | 3 | 2 | 2 | 15 (37.5%) |
| Tandon, et al./ 201436 | 4 | 2 | 2 | 1 | 2 | 4 | 3 | 3 | 21 (52.5%) |
| Yazdanshenas, et al./ 201437 | 3 | 4 | 2 | 1 | 1 | 2 | 3 | 3 | 19 (47.5%) |
| Zhou, et al./ 201538 | 3 | 4 | 3 | 1 | 3 | 2 | 3 | 3 | 22 (55%) |
| Average scores | 3.05 | 2.925 | 2.325 | 1.625 | 2.1 | 3.3 | 3 | 2.775 | 21.1(52.75%) |
- Below 25th percentile ➔ <16.25 ➔ low quality.
- Between 25th and 75th ➔ 16.25–24.5 ➔ Moderate quality.
- Above 75th percentile ➔ > 24.5 ➔ High quality.
4. Discussion
To the best of our knowledge, this systematic review is the first to assess the prescribing patterns of antihypertensives and adherence of prescribing practices to international clinical practice guidelines for hypertension management. The review included 40 eligible studies that were published within the last 10 years and summarized the most commonly prescribed antihypertensives in different populations.
A systematic review of antihypertensive prescribing patterns in Low- and Middle-Income countries (LMICs)54 was conducted by Arshad et al. in 2021. The authors searched the literature from 2000 to 2018 and retrieved 26 studies. Besides mentioning only the most commonly prescribed drugs among diabetics, the review did not show the prescribing patterns among populations with different comorbidities. Additionally, Arshad et al. reported that the included studies and results were based on small hospital-based studies without any community-based literature and indicated not using real-world prescriptions of antihypertensives which in turn affected their results' interpretations and reliability.54
In comparison, the current review summarized various prescribing patterns among different populations including diabetics, cardiovascular disease and chronic kidney disease patients, African Americans, elderly, and pregnant patients in the most recent available literature from 2010 to 2020 in both community and hospital settings and in both low- and middle-income countries.
In this review, the most commonly prescribed antihypertensives as monotherapy in adult hypertensive patients with no comorbidities were ACEIs/ARBs, followed by CCBs, and BBs. The most commonly prescribed dual combination therapies were thiazide diuretics plus ACEIs/ARBs, BBs plus CCBs, and CCBs plus ACEIs/ARBs. In terms of the prescribing of ACEIs/ARBs and CCBs, these results are reassuring as these agents are considered as first-line agents for treating hypertension in non-black patients with no compelling indications.6,8 However, one important and worthwhile point is that in this review, diuretics were the most commonly prescribed agents as monotherapy in only three studies, despite the fact that they are also recommended as one of the preferred agents in treatment guidelines in non-black patients with hypertension.6,8 This recommendation is supported by randomized clinical trials that demonstrate the effectiveness of thiazide diuretics in reducing cardiovascular and cerebrovascular morbidities.55 Moreover, the review finding of the use of BBs as first line agents in many studies is alarming as BBs are not recommended as first-line agents by guidelines in patients with no comorbidities.6,8 In fact, compared with other antihypertensive drugs used in the treatment of hypertension, BBs offer inferior protection against stroke and all-cause mortality, especially among elderly patients.56
Among the diabetic population, the review found that the most commonly prescribed antihypertensives were ACEIs/ARBs. These results are in concordance with guidelines where ACEIs/ARBs maybe considered as first-line agents in patients with diabetes especially in the presence of albuminuria.6,8 Evidence confirms that ACEI/ARBs, as compared with other antihypertensive agents, can halt the progression of moderately increased albuminuria to severe albuminuria in patients with diabetes.57., 58., 59.
In patients with IHD, this review has revealed that CCBs were the most prescribed agents, followed by ARBs and BBs. This finding is discouraging as guidelines recommend that patients with stable IHD should be treated with medications including (BBs, ACEIs, or ARBs) for compelling indications such as previous MI and stable angina.6 In addition to controlling angina symptoms, studies have supported the survival benefit of BBs in patients with acute MI.60., 61, 62. Furthermore, a meta-analysis of four randomized controlled trials has demonstrated that the 30-day mortality is significantly lower in MI patients treated with either ACEIs or ARBs as compared to those on placebo.63
Furthermore, among African American patients with hypertension, the review has shown that thiazide diuretics were identified as the most commonly prescribed antihypertensives as monotherapy in one study,46 while ACEIs or ARBs were the most prescribed monotherapy in another study.37 When monotherapy is used for black hypertensive patients, dihydropyridine CCBs and thiazide diuretics are recommended as initial treatment by treatment guidelines.6,8,64 In addition, evidence demonstrates that African American patients have less reduction in BP as compared to white patients when treated with ACEIs or ARBs as monotherapy.65,66 However, this study was conducted on under-served African American elderly hypertensive patients which could explain the clear deviation from hypertension management guidelines.37
In patients with CKD, the most common agents used as monotherapy were CCBs and ARBs. On the other hand, to slow kidney disease progression, guidelines recommend that adult patients with hypertension and CKD (stage 3 or higher or stage 1 or 2 with albuminuria) should be treated with an ACEI or ARB if ACEIs are not tolerated.6,8
While many studies described the prescribing patterns of anti-hypertensive agents, this systematic review concluded that there are significant gaps in the literature. First, only four studies quantitatively measured adherence to guidelines while the rest provided prescribing data without presenting numerical information on the extent of adherence to national or international guidelines. Second, twenty-two studies provided the general prescribing data for anti-hypertensive without presenting actual data for patients with specific comorbidities, ethnicities and sociodemographic characteristics. To provide an accurate and an in-depth assessment of prescribing practices of antihypertensives, there is need to conduct studies that would quantify the percentage of alignment of hypertension prescribing practices with guidelines as well as examine their suitability in patients with specific comorbidities. Moreover, prescribing data for antihypertensives was lacking for many countries. Further studies need to be implemented in the Middle East, Australia, North and South America and Europe to investigate the prescribing of antihypertensives in these areas and assess its appropriateness in line with the most updated national and international hypertension management guidelines. These studies could help in identifying gaps in practices in these countries and could serve as quality assurance tools for their current hypertension management.
The overall quality of studies was considered acceptable with the majority having moderate to high quality scores. The lowest scores were concerning sampling and data collection. Most studies adapted cross sectional or retrospective designs with a low number of studies that used prospective methodology. In addition, several studies were limited by their small sample size and were confined to only one or two medical centers, which in turn affected the generalizability of their results. Moreover, many studies were restricted by their short duration. Consequently, it is recommended to conduct robust large and long-term studies with big representative samples in order to have a better holistic understanding of prescribing of antihypertensives.
Overall, this review has demonstrated that the prescribing of antihypertensives for hypertension management is not optimal and is not well aligned with hypertension guidelines in many countries. Therefore, more concerted efforts are needed to bridge the gap between practice and evidence and to improve the prescribing practices for hypertension management. These efforts can include, but not restricted to, offering continuous professional development for prescribers, designing and implementing treatment protocols or clinical pathways based on latest evidence and clinical practice guidelines, initiating quality improvement strategies and restructuring the curricula of new medical graduates in order to have competent physicians ready to optimally prescribe antihypertensives as per best evidence.
4.1. Limitations
Our systematic review had some limitations. Due to the heterogeneity of study results and outcomes we were not able to conduct a meta-analysis. Moreover, comparing the study results between different countries was very challenging due to the variability in study designs and presented data across studies. We might have missed some studies published in Arabic or other languages by restricting our search strategies to English only studies.
Notably, this systematic review did not assess the factors that affect physicians' prescribing of antihypertensives and their reasons for prescribing particular antihypertensives over others. In order to design strategic plans, policies or guidelines to improve blood pressure control and management, future studies or reviews are needed to systematically assess the prescribing process and decision making of physicians when treating hypertensive patients.
5. Conclusion
This systematic review provided an overview on the prescribing of antihypertensives worldwide and conformity to guidelines. This review concluded that there are areas for improvement of prescribing practices of antihypertensives in concordance with the latest evidence and with clinical practice guidelines. To advance antihypertensive prescribing, interventions must be designed and executed.
Funding
This work was supported by a student grant (grant number QUST-2-CPH-2020-20) from Qatar University Office of Research and Graduate Studies. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of Qatar University.
Authors' contribution
-
•
MH: is the lead principal investigator of the study leading its design and execution. She wrote the study manuscript
-
•
HE and AA: contributed in discussions related to the design of the research project, and review of all the drafts throughout the project
-
•
NA: contributed to retrieval, screening and critical appraisal of articles and writing the manuscript
Declaration of Competing Interest
Nothing to declare
Contributor Information
Nada Nabil Abdelkader, Email: na1303710@student.qu.edu.qa.
Ahmed Awaisu, Email: aawaisu@qu.edu.qa.
Hazem Elewa, Email: hazem.elewa@qu.edu.qa.
Maguy Saffouh El Hajj, Email: maguyh@qu.edu.qa.
Appendix A. Appendix
Databases search strategies:
PubMed:
((Hypertensive[Title/Abstract] OR hypertension[Title/Abstract] OR Hypertens*[Title/Abstract] OR High blood pressure[Title/Abstract] OR blood pressure lowering[Title/Abstract] OR beta blocker[Title/Abstract] OR calcium channel blocker[Title/Abstract] OR CCB[Title/Abstract] OR angiotensin converting enzyme inhibitor[Title/Abstract] OR ACEI[Title/Abstract] OR ACE inhibitor[Title/Abstract] OR angiotensin receptor blocker[Title/Abstract] OR ARB[Title/Abstract] OR Diuretic[Title/Abstract] OR thiazide[Title/Abstract] OR renin inhibitor[Title/Abstract] OR Aliskiren[Title/Abstract] OR alpha blocker[Title/Abstract] AND ((2010/1/1:2021/3/12[pdat]) AND (english[Filter]))) AND (Prescrib*[Title/Abstract] OR use[Title/Abstract] OR utilize[Title/Abstract] OR utilization[Title/Abstract] OR prescription[Title/Abstract] OR treat*[Title/Abstract] OR manag*[Title/Abstract] OR pharmacotherapy[Title/Abstract] OR therapy[Title/Abstract] AND ((2010/1/1:2021/3/12[pdat]) AND (english[Filter])))) AND (Type[Title/Abstract] OR Trend[Title/Abstract] OR Pattern[Title/Abstract] OR Habit[Title/Abstract] OR Appropriate*[Title/Abstract] OR Rational*[Title/Abstract] OR Control[Title/Abstract] OR Guideline[Title/Abstract] OR Recommend*[Title/Abstract] OR Adhere*[Title/Abstract] OR Compliance[Title/Abstract] OR Comply[Title/Abstract] OR Proper[Title/Abstract] AND ((2010/1/1:2021/3/12[pdat]) AND (english[Filter]))) Filters: English, from 2010/1/1–2021/3/12.
Embase:
(hypertensive:ti OR hypertension:ti OR hypertens*:ti OR ‘high blood pressure’:ti OR ‘blood pressure lowering’:ti OR ‘beta blocker’:ti OR ‘calcium channel blocker’:ti OR ccb:ti OR ‘angiotensin converting enzyme inhibitor’:ti OR acei:ti OR ‘ace inhibitor’:ti OR ‘angiotensin receptor blocker’:ti OR arb:ti OR diuretic:ti OR thiazide:ti OR ‘renin inhibitor’:ti OR aliskiren:ti OR ‘alpha adrenergic receptor blocking agent’:ti) AND (prescrib*:ti OR use:ti OR utilize:ti OR utilization:ti OR prescription:ti OR treat*:ti OR manag*:ti OR pharmacotherapy:ti OR therapy:ti) AND (type:ti OR trend:ti OR pattern:ti OR habit:ti OR appropriate*:ti OR rational*:ti OR control:ti OR guideline:ti OR recommend*:ti OR adhere*:ti OR compliance:ti OR comply:ti OR proper:ti) AND [english]/lim AND [2010−2021]/py.
PROQUEST:
abstract(Hypertensive OR hypertension OR High blood pressure OR blood pressure lowering OR beta blocker OR calcium channel blocker OR CCB OR angiotensin converting enzyme inhibitor OR ACEI OR ACE inhibitor OR angiotensin receptor blocker OR ARB OR Diuretic OR thiazide OR renin inhibitor OR Aliskiren OR alpha blocker) AND abstract(Prescribe OR use OR utilize OR utilization OR prescription OR treat OR manage OR pharmacotherapy OR therapy) AND abstract(Type OR Trend OR Pattern OR Habit OR Appropriate OR Rational OR Control OR Guideline OR Recommend OR Adhere OR Compliance OR Comply OR Proper)
Regarding the other databases the same search strategy was followed as written in Table 1.
Data availability
The datasets obtained in the present study are available from the corresponding author on reasonable request.
References
- 1.Hypertension Key Fact., Page Hypertension Key Fact. https://www.who.int/news-room/fact-sheets/detail/hypertension (Accessed 11 March 2020.
- 2.Noncommunicable Diseases Country Profiles., Page Noncommunicable Diseases Country Profiles. https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (Accessed 11 March 2020.
- 3.N.C.D.R.F. Collaboration Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.EJ S.J. Maclaughlin., editor. Pharmacotherapy: A Pathophysiologic Approach. McGraw-Hill Education; New York: 2023. 11e NY. [Google Scholar]
- 5.Ettehad D., Emdin C.A., Kiran A., et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 6.Whelton P.K., Carey R.M., Aronow W.S., et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;71(2018):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Cuspidi C., Tadic M., Grassi G., Mancia G. Treatment of hypertension: the ESH/ESC guidelines recommendations. Pharmacol Res. 2018;128:315–321. doi: 10.1016/j.phrs.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 8.James P.A., Oparil S., Carter B.L., et al. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint National Committee (JNC 8) JAMA. 2014;311(2014):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 9.Dorans K.S., Mills K.T., Liu Y., He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLean D.L., Simpson S.H., McAlister F.A., Tsuyuki R.T. Treatment and blood pressure control in 47,964 people with diabetes and hypertension: a systematic review of observational studies. Can J Cardiol. 2006;22:855–860. doi: 10.1016/s0828-282x(06)70304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G., P. Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 12.Rethlefsen M.L., Kirtley S., Waffenschmidt S., et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev. 2021;10:39. doi: 10.1186/s13643-020-01542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crowe M., Sheppard L., Campbell A. Comparison of the effects of using the Crowe critical appraisal tool versus informal appraisal in assessing health research: a randomised trial. Int J Evid Based Healthc. 2011;9:444–449. doi: 10.1111/j.1744-1609.2011.00237.x. [DOI] [PubMed] [Google Scholar]
- 14.Adamu U., Abdulahi A., Ibrahim F., Ibok I. Pattern of medication use among hypertensives attending a specialist outpatients Clinic in North-Central Nigeria. J Pharm Res Int. 2017;17:1–8. [Google Scholar]
- 15.Adejumo O., Okaka E., Iyawe I. Prescription pattern of antihypertensive medications and blood pressure control among hypertensive outpatients at the University of Benin Teaching Hospital in Benin City, Nigeria. Malawi Med J. 2017;29:113–117. doi: 10.4314/mmj.v29i2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Khaja K.A.J., James H., Veeramuthu S., Tayem Y.I., Sridharan K., Sequeira R.P. Antihypertensive prescribing pattern in older adults: implications of age and the use of dual single-pill combinations. High Blood Press Cardiovasc Prev. 2019;26:535–544. doi: 10.1007/s40292-019-00353-1. [DOI] [PubMed] [Google Scholar]
- 17.Alba-Leonel A., Carvajal A., Fierro I., et al. Prescription patterns of antihypertensives in a community health Centre in Mexico City: a drug utilization study. Fundam Clin Pharmacol. 2016;30:276–281. doi: 10.1111/fcp.12179. [DOI] [PubMed] [Google Scholar]
- 18.Alkaabi M.S., Rabbani S.A., Rao P.G.M., Ali S.R. Prescription pattern of antihypertensive drugs: an experience from a secondary care hospital in the United Arab Emirates. J Res Pharm Pract. 2019;8:92–100. doi: 10.4103/jrpp.JRPP_18_85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed N.J. Prescribing trends of amlodipine in outpatient setting. J Pharm Res Int. 2020;32:15–19. [Google Scholar]
- 20.Beg M., Dutta S., Varma A., et al. Study on drug prescribing pattern in hypertensive patients in a tertiary care teaching hospital at Dehradun, Uttarakhand. Int J Med Sci Public Health. 2014;3:922. [Google Scholar]
- 21.Chang T.I., Evans G., Cheung A.K., et al. Patterns and correlates of baseline thiazide-type diuretic prescription in the systolic blood pressure intervention trial. Hypertension. 2016;67:550–555. doi: 10.1161/HYPERTENSIONAHA.115.06851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El Mawardy R., Okba A. Antihypertensive treatment and blood pressure control in patients with hypertension in daily clinical practice: a cross-sectional, multicenter, observational study in Egypt. Curr Med Res Opin. 2017;33:39–45. doi: 10.1080/03007995.2016.1232706. [DOI] [PubMed] [Google Scholar]
- 23.Rajasekhar D.G., Prasanna D.G., Chandrakanth P. Prescribing pattern of antihypertensive drugs based on compelling indications with hypertension. Int J Pharm Pharm Sci. 2016;8:72–75. [Google Scholar]
- 24.Hussain I.M., Naqvi B.S., Qasim R.M., Ali N. Current trends in treatment of hypertension in Karachi and cost minimization possibilities. Pak J Med Sci. 2015;31:1021–1026. doi: 10.12669/pjms.315.7438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ibaraki A., Goto W., Iura R., Tominaga M., Tsuchihashi T. Current prescription status of antihypertensive drugs with special reference to the use of diuretics in Japan. Hypertens Res. 2017;40:203–206. doi: 10.1038/hr.2016.120. [DOI] [PubMed] [Google Scholar]
- 26.Ishida T., Oh A., Hiroi S., Shimasaki Y., Tsuchihashi T. Current prescription status of antihypertensive drugs in Japanese patients with hypertension: analysis by type of comorbidities. Clin Exp Hypertens. 2019;41:203–210. doi: 10.1080/10641963.2018.1465074. [DOI] [PubMed] [Google Scholar]
- 27.Mbui J.M., Oluka M.N., Guantai E.M., et al. Prescription patterns and adequacy of blood pressure control among adult hypertensive patients in Kenya; findings and implications. Expert Rev Clin Pharmacol. 2017;10:1263–1271. doi: 10.1080/17512433.2017.1371590. [DOI] [PubMed] [Google Scholar]
- 28.Murti K., Khan M.A., Dey A., Sethi M.K., Das P., Pandey K. Prescription pattern of anti-hypertensive drugs in adherence to JNC- 7 guidelines. Am J Pharmacol Toxicol. 2015;10 [Google Scholar]
- 29.Pandey V., Hoda U., Aqil M., et al. Evaluation of prescribing patterns in diabetic and hypertensive patients in a South Delhi hospital. Int J Basic Clin Pharmacol. 2014;3:490. [Google Scholar]
- 30.Paradkar S.G., Sinha S.R. Drug utilization among hypertensive patients in the outpatient department of medicine in a tertiary care hospital: a cross-sectional study. Clin Exp Hypertens. 2018;40:150–154. doi: 10.1080/10641963.2017.1346112. [DOI] [PubMed] [Google Scholar]
- 31.Pr R., Hv A., Shivamurthy M. Anti hypertensive prescribing patterns and cost analysis for primary hypertension: a retrospective study. J Clin Diagn Res. 2014;8 doi: 10.7860/JCDR/2014/9567.4890. Hc19-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sajith M., Nimbargi V., Modi A., Sumariya R., Pawar A. Incidence of pregnancy induced hypertension and prescription pattern of antihypertensive drugs in pregnancy. Int J Adv Sci Res. 2014;5:163–170. [Google Scholar]
- 33.Shastry R., Adhikari M.R.P., Ullal S.D., Kotian S. Usage of diuretics among diabetic-hypertensive patients. Asian J Med Sci. 2014;6:14–17. [Google Scholar]
- 34.Si S., Ofori-Asenso R., Briffa T., et al. Dispensing patterns of blood pressure lowering agents in older Australians from 2006 to 2016. J Cardiovasc Pharmacol Ther. 2019;24:242–250. doi: 10.1177/1074248418812184. [DOI] [PubMed] [Google Scholar]
- 35.Tamirci M., Demirdamar R. Antihypertensive drug utilization in two districts of Northern Cyprus. Rational Pharmacother Cardiol. 2019;15:467–477. [Google Scholar]
- 36.Tandon V.R., Sharma S., Mahajan S., et al. Antihypertensive drug prescription patterns, rationality, and adherence to Joint National Committee-7 hypertension treatment guidelines among Indian postmenopausal women. J Midlife Health. 2014;5:78–83. doi: 10.4103/0976-7800.133994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yazdanshenas H., Bazargan M., Orum G., Loni L., Mahabadi N., Husaini B. Prescribing patterns in the treatment of hypertension among underserved African American elderly. Ethn Dis. 2014;24:431–437. [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou M., Daubresse M., Stafford R.S., Alexander G.C. National trends in the ambulatory treatment of hypertension in the United States, 1997-2012. PloS One. 2015;10 doi: 10.1371/journal.pone.0119292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dhanaraj E., Raval A., Yadav R., Bhansali A., Tiwari P. Prescription pattern of antihypertensive agents in T2DM patients visiting tertiary Care Centre in North India. Int J Hypertens. 2012;2012 doi: 10.1155/2012/520915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khurshid F., Aqil M., Alam M., Kapur P., Pillai K. Antihypertensive medication prescribing patterns in a university teaching hospital in South Delhi. Int J Pharm Sci Res. 2012;3:2057–2063. [Google Scholar]
- 41.Mohd A.H., Mateti U.V., Konuru V., Parmar M.Y., Kunduru B.R. A study on prescribing patterns of antihypertensives in geriatric patients, Perspect. Clin Res. 2012;3:139–142. doi: 10.4103/2229-3485.103595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pai P.G., Shenoy J., Sanji N. Prescribing Patterns of antihypertensive drugs in a South Indian tertiary care hospital. Drug Invent Today. 2011;3:38–40. [Google Scholar]
- 43.Grigoryan L., Pavlik V.N., Hyman D.J. Characteristics, drug combinations and dosages of primary care patients with uncontrolled ambulatory blood pressure and high medication adherence. J Am Soc Hypertens. 2013;7:471–476. doi: 10.1016/j.jash.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gu Q., Burt V.L., Dillon C.F., Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–2114. doi: 10.1161/CIRCULATIONAHA.112.096156. [DOI] [PubMed] [Google Scholar]
- 45.Hanselin M.R., Saseen J.J., Allen R.R., Marrs J.C., Nair K.V. Description of antihypertensive use in patients with resistant hypertension prescribed four or more agents. Hypertension. 2011;58:1008–1013. doi: 10.1161/HYPERTENSIONAHA.111.180497. [DOI] [PubMed] [Google Scholar]
- 46.Harman J., Walker E.R., Charbonneau V., Akylbekova E.L., Nelson C., Wyatt S.B. Treatment of hypertension among African Americans: the Jackson heart study. J Clin Hypertens (Greenwich) 2013;15:367–374. doi: 10.1111/jch.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abdulameer S.A., Sahib M.N., Aziz N.A., Hassan Y., Alrazzaq H.A., Ismail O. Physician adherence to hypertension treatment guidelines and drug acquisition costs of antihypertensive drugs at the cardiac clinic: a pilot study. Patient Prefer Adherence. 2012;6:101–108. doi: 10.2147/PPA.S27223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abougalambou S.S., Abougalambou A.S., Sulaiman S.A., Hassali M.A. Prevalence of hypertension, control of blood pressure and treatment in hypertensive with type 2 diabetes in Hospital University Sains Malaysia. Diabetes Metab Syndr. 2011;5:115–119. doi: 10.1016/j.dsx.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 49.Ramli A., Miskan M., Ng K., et al. Prescribing of antihypertensive agents in public primary care clinics - is it in accordance with current evidence? Malays Fam Phys. 2010;5:36–40. [PMC free article] [PubMed] [Google Scholar]
- 50.Maghrabi I. Evaluation of antihypertensive prescribing patterns in the western region of Saudi Arabia and its compliance with national guidelines. Saudi J Health Sci. 2013;2:118–126. [Google Scholar]
- 51.Bulatova N., Yousef A.M., AbuRuz S., Farha R. Hypertension management and factors associated with blood pressure control in Jordanian patients attending cardiology clinic. Trop J Pharm Res. 2013;12 [Google Scholar]
- 52.Adnan W.A. Wan Md, Zaharan N.L., Bennett K., Wall C.A. Trends in co-prescribing of angiotensin converting enzyme inhibitors and angiotensin receptor blockers in Ireland. Br J Clin Pharmacol. 2011;71:458–466. doi: 10.1111/j.1365-2125.2010.03835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin C.S., Chu Y.H., Hung Y.J., Lee D.Y., Chen C.Y. Outpatient hypertension control and prescribing habits for hypertension in Taiwan. Acta Cardiol Sin. 2013;29:539–549. [PMC free article] [PubMed] [Google Scholar]
- 54.Arshad V., Samad Z., Das J., et al. Prescribing Patterns of antihypertensive medications in low- and middle-income countries: a systematic review. Asia Pac J Public Health. 2021;33:14–22. doi: 10.1177/1010539520965280. [DOI] [PubMed] [Google Scholar]
- 55.Olde Engberink R.H., Frenkel W.J., van den Bogaard B., Brewster L.M., Vogt L., van den Born B.J. Effects of thiazide-type and thiazide-like diuretics on cardiovascular events and mortality: systematic review and meta-analysis. Hypertension. 2015;65:1033–1040. doi: 10.1161/HYPERTENSIONAHA.114.05122. [DOI] [PubMed] [Google Scholar]
- 56.Thomopoulos C., Bazoukis G., Tsioufis C., Mancia G. Beta-blockers in hypertension: overview and meta-analysis of randomized outcome trials. J Hypertens. 2020;38:1669–1681. doi: 10.1097/HJH.0000000000002523. [DOI] [PubMed] [Google Scholar]
- 57.Makino H., Haneda M., Babazono T., et al. Prevention of transition from incipient to overt nephropathy with telmisartan in patients with type 2 diabetes. Diabetes Care. 2007;30:1577–1578. doi: 10.2337/dc06-1998. [DOI] [PubMed] [Google Scholar]
- 58.Parving H.H., Lehnert H., Bröchner-Mortensen J., Gomis R., Andersen S., Arner P. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345:870–878. doi: 10.1056/NEJMoa011489. [DOI] [PubMed] [Google Scholar]
- 59.Ravid M., Savin H., Jutrin I., Bental T., Katz B., Lishner M. Long-term stabilizing effect of angiotensin-converting enzyme inhibition on plasma creatinine and on proteinuria in normotensive type II diabetic patients. Ann Intern Med. 1993;118:577–581. doi: 10.7326/0003-4819-118-8-199304150-00001. [DOI] [PubMed] [Google Scholar]
- 60.Bangalore S., Steg G., Deedwania P., et al. β-Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. Jama. 2012;308:1340–1349. doi: 10.1001/jama.2012.12559. [DOI] [PubMed] [Google Scholar]
- 61.Freemantle N., Cleland J., Young P., Mason J., Harrison J. beta blockade after myocardial infarction: systematic review and meta regression analysis. Bmj. 1999;318:1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nakatani D., Sakata Y., Suna S., et al. Impact of beta blockade therapy on long-term mortality after ST-segment elevation acute myocardial infarction in the percutaneous coronary intervention era. Am J Cardiol. 2013;111:457–464. doi: 10.1016/j.amjcard.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 63.Indications for ACE inhibitors in the early treatment of acute myocardial infarction: systematic overview of individual data from 100,000 patients in randomized trials. ACE Inhibitor Myocardial Infarction Collaborative GroupCirculation. 1998;97:2202–2212. doi: 10.1161/01.cir.97.22.2202. [DOI] [PubMed] [Google Scholar]
- 64.Williams B., Mancia G., Spiering W., et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Eur Heart J. 2018;39(2018):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 65.Materson B.J., Reda D.J., Cushman W.C., et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on antihypertensive agents. N Engl J Med. 1993;328:914–921. doi: 10.1056/NEJM199304013281303. [DOI] [PubMed] [Google Scholar]
- 66.Wright J.T., Jr., Dunn J.K., Cutler J.A., et al. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. Jama. 2005;293:1595–1608. doi: 10.1001/jama.293.13.1595. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets obtained in the present study are available from the corresponding author on reasonable request.