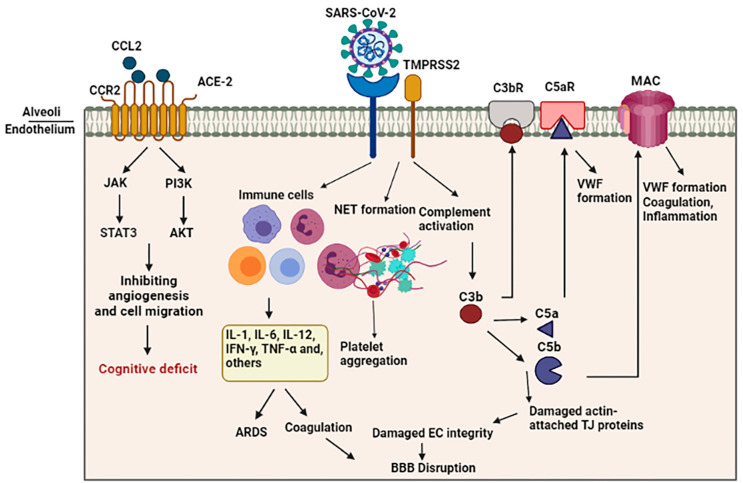
Figure 2.
Schematic representation of indirect BBB disruption resulting from vascular dysfunction in COVID-19. The virus acts via binding of the spike glycoprotein of the virus to the angiotensin converting enzyme 2 (ACE2) on the cell surface. Disharmonic and disturbed immune reaction in COVID-19 patients lead to wide local and systemic inflammation by generating cytokine storm, leading to ARDS and vascular coagulation. Alternatively, it may lead to the formation of neutrophil extracellular traps (NETs), composed of chromatin and microbicidal proteins, which participate in the pathobiology of thrombosis and platelets aggregation. Activation of the complement system results in the generation of C5a and C5b, which are involved in the inflammation and activation of platelets. This C5b forms the membrane attack complex (MAC) to activate microvascular coagulation and inflammation.