Abstract
Chronic immune thrombocytopenia (CITP) is an autoimmune disease whose underlying biologic mechanisms remain elusive. Human endogenous retroviruses (HERVs) derive from ancestral infections and constitute about 8% of our genome. A wealth of clinical and experimental studies highlights their pivotal pathogenetic role in autoimmune diseases. Epigenetic mechanisms, such as those modulated by TRIM28 and SETDB1, are involved in HERV activation and regulation of immune response. We assessed, through a polymerase chain reaction real-time Taqman amplification assay, the transcription levels of pol genes of HERV-H, HERV-K, and HERV-W; env genes of Syncytin (SYN)1, SYN2, and HERV-W; as well as TRIM28 and SETDB1 in whole blood from 34 children with CITP and age-matched healthy controls (HC). The transcriptional levels of all HERV sequences, with the exception of HERV-W-env, were significantly enhanced in children with CITP as compared to HC. Patients on eltrombopag treatment exhibited lower expression of SYN1, SYN2, and HERV-W-env as compared to untreated patients. The mRNA concentrations of TRIM28 and SETDB1 were significantly higher and were positively correlated with those of HERVs in CITP patients. The over-expressions of HERVs and TRIM28/SETDB1 and their positive correlations in patients with CITP are suggestive clues of their contribution to the pathogenesis of the disease and support innovative interventions to inhibit HERV and TRIM28/SETDB1 expressions in patients unresponsive to standard therapies.
Keywords: autoimmune disease, primary immune thrombocytopenia, endogenous retroviruses, SETDB1, TRIM28, genetic pathomechanism, children
1. Introduction
Immune thrombocytopenia (ITP), also called idiopathic or immune thrombocytopenic purpura, is a bleeding disorder characterized by isolated thrombocytopenia with a peripheral blood platelet count < 100 × 109/L [1]. It is the most common hematological disease in childhood [2]. Primary ITP must be distinguished from secondary forms, which are triggered by an underlying disease, such as infections, autoimmune disorders, and drug exposures [3]. Children with ITP are usually well appearing, with only bleeding signs, often with sudden onset and a negative family and past medical history. Primary ITP is often benign and self-limited in childhood, though in 20–30% of cases it may give rise to chronic forms lasting beyond 12 months (CITP, chronic immune thrombocytopenia) [1,4]. Older age, higher initial platelet count, and female gender may be predictive elements for chronic evolution [5,6].
ITP is considered an immune-mediated disease and platelet autoantibodies (PAA) are thought to be important actors [7]. Testing for PAA is, however, not recommended for the diagnosis, due to its poor accuracy. Growing evidence highlights that more complex immune mechanisms, such as T cell-induced effects, are implicated in ITP pathogenesis [8,9]. In particular, loss of tolerance and exposure to infection-driven post-translational changes of platelet antigens, promoting T cell-conditioned B cell responses, or T cells cross-reactive against platelets and pathogen-derived peptides have been suggested [10]. The essential role played by micro-RNAs has also been proposed [11]. Dysregulation of epigenetic processes leading to abnormal gene expression via variations in the DNA methylation and in histone-induced heterochromatin formation, has become an attractive hypothesis too [12,13].
Human endogenous retroviruses (HERVs) originate from ancestral infections of somatic cells with subsequent integration into germ line of primates millions of years ago. During evolution, the continuous mutations have blocked the production of infectious virions. However, HERVs maintain their retroviral structure with three principal genes: group associated antigens (gagitalics is not necessary, but it must be consistent in the whole papper), polymerase (pol), and envelope (env), flanked between two regulatory long terminal repeats (LTRs) [14]. Most HERVs are inactive, but some sequences are transcribed and a few encode proteins. An increasing body of literature heralds the crucial role of HERVs during the intrauterine life [15,16], representing a clear example of how retroviral elements are used by the host for its own survival. For instance, two envelope proteins, called syncytin-1 (SYN1) [17] and syncytin-2 (SYN2) [18], are essential for the placental morphogenesis and contribute to the materno-fetal tolerance [19,20]. Postnatally, the physiologic functions of HERVs remain questionable, whereas their abnormal expressions may induce several hallmarks of cells infected by a virus, leading to innate and adaptive immune responses. HERV alterations have been associated with an increasing number of diseases, including autoimmune disturbances [21,22,23,24]. Actually, HERVs can regulate the expression of close cellular genes [25,26]. Their RNAs, through a copy and paste mechanism, can be reintegrated into the DNA or be recognized as non-self by specific viral receptors, triggering a variety of inflammatory and immune reactions [22,25,26,27,28]. Furthermore, HERV antigens can induce targeted immune responses, including specific and/or cross-reactive antibodies with tissue epitopes [29,30,31,32]. The persistence of aberrant HERV expressions may vary over time [33,34]; their dysregulation can thus determine an episodic or a chronic challenge for the immune system [21], reminiscent of the clinical presentation of ITP.
HERV expression is modulated by environmental factors via epigenetic mechanisms. Tripartite motif containing 28 (TRIM28), also called KAP1 or TIF1-β, is a nuclear co-repressor of Krüppel-associated box domain zinc finger proteins (KRAB-ZFPs) [35,36]. SET domain bifurcated histone lysine methyltransferase 1 (SETDB1), also referred to as ESET, is a methyltransferase with high specificity for the lysine 9 residue of histone H3 [37]. It contributes to orchestrate the heterochromatin formation. Both TRIM28 and SETBD1 play key roles for epigenetic transcriptional modulation of retroviral sequences [38,39]. Furthermore, accumulating data demonstrate their direct involvement in cellular homeostasis and in the control of both innate and adaptive immune responses [40,41].
Despite the wealth of data supporting the role of HERVs, TRIM28, and SETDB1 in eliciting and/or maintaining autoimmune diseases, no studies explored their expressions in patients affected by ITP. Therefore, the aims of this study were to assess and compare the transcriptional levels of pol genes of HERV-H, -K, and -W, the three retroviral families most widely studied [19,21]; env genes of SYN1, SYN2, and HERV-W [17,18,22]; as well as TRIM28 and SETDB1 in whole blood from children affected by CITP and in age-matched healthy controls (HC).
2. Material and Methods
2.1. Study Populations
All children and adolescents affected by CITP (i.e., a primary immune thrombocytopenia lasting for more than 12 months according to the IWG criteria [1]) and regularly followed at the Department of Pediatrics, University of Turin, Regina Margherita Children’s Hospital, Turin, Italy, were enrolled in the study. Patients with secondary forms of thrombocytopenia, associated hematologic/immunologic abnormalities, and/or comorbidities were excluded from the analysis.
Asymptomatic subjects of comparable age who were tested at the same hospital for routine laboratory examinations and whose results were all within the normal reference range were the control group. Subjects with any confirmed or suspected disease, such as infections, cancer, autoimmune disorders, inflammatory diseases, neurological disturbances, or abnormal laboratory results were excluded from the study.
2.2. RNA Extraction and Retrotranscription
Total RNA was extracted from whole blood with RNA Blood Kit (Maxwell automated extractor, Promega, Madison, WI, USA). This kit provides treatment with DNase during the first step of RNA extraction. To exclude contamination with residual genomic DNA, total RNA extracts were directly amplified without reverse transcription. RNA concentration and purity were spectroscopy determined (ND-1000 spectrophotometer, Biochrom Enterprise, Waterbeach, Cambridge, UK) at absorbance of 260 and 280 nm. RNAs were stored at −80 °C until use.
A total of 400 ng of RNA was reverse-transcribed with 2 μL of buffer 10× 4.8 μL of MgCl2 25 mM, 1 μL of RNase inhibitor 20 U/l, 2 μL ImpromII (Promega), 2 μL mix dNTPs 100 mM (Promega), 0.4 μL random hexamers 250 μM (Promega), and dd-water in a final volume of 20 μL. The reaction mix was carried out in a GeneAmp PCR system, 9700 Thermal Cycle (Applied Biosystems, Foster City, CA, USA) under the following conditions: 5 min at 25 °C, 60 min at 42 °C, and 15 min at 70 °C for the inactivation of enzymes; the cDNAs were stored at −20 °C until use.
2.3. Transcription Levels of Pol Genes of HERV-H, -K, and -W; Env Genes of SYN1, SYN2, and HERV-W; as well as of TRIM28 and SETB1 by Real-Time PCR Assay
Transcription levels of pol genes of HERV-H, HERV-K, and HERV-W; env genes of SYN1, SYN2, and HWERV-W; and TRIM28 and SETDB1 were achieved as previously described in detail [23,24,33,34] using the primers and probes reported in Table 1. Briefly, 40 ng of cDNA was amplified in a 20 μL total volume reaction, containing 2.5 U goTaQ MasterMix (Promega), 1.25 mmol/L MgCl2, 200 nmol of specific probes, and 500 nmol of specific primers.
Table 1.
Primers and probes used to assess the transcription levels of pol genes of HERV-K, -W, and –H; env genes of Syncytin 1, Syncytin 2, and HERV-W; TRIM28 and SETDB1; and GAPDH.
| Name | Primer/ Probe |
Sequence |
|---|---|---|
| HERV-H pol | Forward | 5′-TGGACTGTGCTGCCGCAA-3′ |
| Reverse | 5′-GAAGSTCATCAATATATTGAATAAGGTGAGA-3′ | |
| Probe | 6FAM-5′-TTCAGGGACAGCCCTCGTTACTTCAGCCAAGCTC-3′-TAMRA | |
| HERV-K pol | Forward | 5′-CCACTGTAGAGCCTCCTAAACCC-3′ |
| Reverse | 5′-TTGGTAGCGGCCACTGATTT-3′ | |
| Probe | 6FAM-5′-CCCACACCGGTTTTTCTGTTTTCCAAGTTAA-3′-TAMRA | |
| HERV-W pol | Forward | 5′-ACMTGGAYKRTYTTRCCCCAA-3′ |
| Reverse | 5′-GTAAATCATCCACMTAYYGAAGGAYMA-3′ | |
| Probe | 6FAM-5′-TYAGGGATAGCCCYCATCTRTTTGGYCAGGCA-3′-TAMRA | |
| Syncytin 1 env | Forward | 5′-ACTTTGTCTCTTCCAGAATCG-3′ |
| Reverse | 5′-GCGGTAGATCTTAGTCTTGG-3′ | |
| Probe | 6FAM-5′-TGCATCTTGGGCTCCAT-3′-TAMRA | |
| Syncytin 2 env | Forward | 5′-GCCTGCAAATAGTCTTCTTT-3′ |
| Reverse | 5′-ATAGGGGCTATTCCCATTAG-3′ | |
| Probe | 6FAM- 5′-TGATATCCGCCAGAAACCTCCC-3′-TAMRA | |
| HERV-W env | Forward | 5′-CTTCCAGAATTGAAGCTGTAAAGC-3′ |
| Reverse | 5′-GGGTTGTGCAGTTGAGATTTCC-3′ | |
| Probe | 6FAM-5′-TTCTTCAAATGGAGCCCCAGATGCAG-3′-TAMRA | |
| TRIM28 | Forward | 5′-GCCTCTGTGTGAGACCTGTGTAGA-3′ |
| Reverse | 5′-CCAGTAGAGCGCACAGTATGGT-3′ | |
| Probe | 6FAM-5′-CGCACCAGCGGGTGAAGTACACC-3′-TAMRA | |
| SETDB1 | Forward | 5′-GCCGTGACTTCATAGAGGAGTATGT-3′ |
| Reverse | 5′-GCTGGCCACTCTTGAGCAGTA-3′ | |
| Probe | 6FAM-5′-TGCCTACCCCAACCGCCCCAT-3′-TAMRA | |
| GAPDH | Forward | 5′-CGAGATCCCTCCAAAATCAA-3′ |
| Reverse | 5′-TTCACACCCATGACGAACAT-3′ | |
| Probe | 6FAM-5′-TCCAACGCAAAGCAATACATGAAC-3′-TAMRA |
All amplifications were performed in a 96-well plate at 95 °C for 10 min, followed by 45 cycles at 95 °C for 15 s and at 60 °C for 1 min. Each sample was run in triplicate. Relative quantification of target gene transcripts was performed using the 2−ΔΔCt method [42]. GAPDH was selected as the reference gene because it has been shown to have good efficiency and excellent reproducibility with constant expression in human leukocyte samples and has been used previously in our studies [23,24,33,34]. Briefly, after normalizing the PCR result of each target gene with the GAPDH, the method includes an additional calibration of this value with the median expression of the same gene obtained in a pool of healthy controls after normalization with the GAPDH. The results, expressed in arbitrary units (RQ), show the variations in target gene expression compared with standard controls. Because we determined the cycle threshold (Ct) for each target in all samples, we argue that our methods were suitable for HERVs, TRIM28, and SETDB1 detection and quantifications.
2.4. Statistical Analysis
One-way ANOVA test was used to compare the age between patients with CITP and the two subgroups (B1 and B2) of HC. Mann–Whitney test was used to compare the transcripts of pol genes of every HERV family; env genes of SYN1, SYN2, and HERV-W; as well as TRIM28 and SETDB1 between children with CITP and control children. Spearman correlation test was performed to estimate the correlations concerning transcription levels of each HERV sequence and TRIM28 or SETDB1 in every group of children. Statistical analyses were performed using Prism software, version 7 (GraphPad Software, La Jolla, CA, USA). In all analyses, p < 0.05 was taken to be statistically significant.
3. Results
3.1. Study Populations
As reported in Table 2, 34 children with CITP were enrolled in the study (Group A). Healthy controls (HC) were subdivided into two subgroups: Group B1 included 64 children and adolescents who had been enrolled as healthy controls in our previous studies on pol gene expressions of HERV-H, -K, and -W [23,24,33,34]; Group B2 included 47 subjects who were tested for expression of env genes of SYN1, SYN2, and HERV-W, and of TRIM28 and SETDB1. The median ages were comparable among the three groups of children (one-way ANOVA, p = 0.1998).
Table 2.
Clinical characteristics of children with chronic immune thrombocytopenia (CITP) and age-matched healthy controls (B1 and B2).
| CITP (n = 34) |
B1 (n = 64) |
B2 (n = 47) |
|
|---|---|---|---|
| Mean age (±SD) | 12.1 (±4.1) years | 10.9 (±3.5) years | 10.6 (±3.2) years |
| Males (%) | 17 (50) | 35 (55.7) | 29 (61.7) |
| Mean duration of CITP (±SD) at time of sampling | 4.4 (±3.1) years | ||
| Ongoing therapy n (%) | Eltrombopag: 11 (31.4) MMF: 2 (5.7) Eltrombopag + MMF: 2 (5.7) Sirolimus: 1 (2.9) |
n: number; SD: standard deviation; %: percentage; MMF: mofetil mycophenolate.
3.2. Expression Levels of Housekeeping Gene
The transcription levels of housekeeping gene GAPDH were similar between patients with CITP and HC: Medians and IQR 25%–75%: Group A: median 22.3, IQR 21.8–22.7; Group B1: median 22.1, IQR 21.6–22.5 (p = 0.4111); Group B2: median 21.8, IQR 21.5–22.4 (p = 0.1432).
3.3. Expressions of HERV-H-pol, HERV-K-pol, HERV-W-pol, SYN1-env, SYN2-env, and HERV-W-env
The pol genes of HERV-H, HERV-K, and HERV-W and the env genes of SYN1, SYN2, and HERV-W were transcriptionally active in all the study populations.
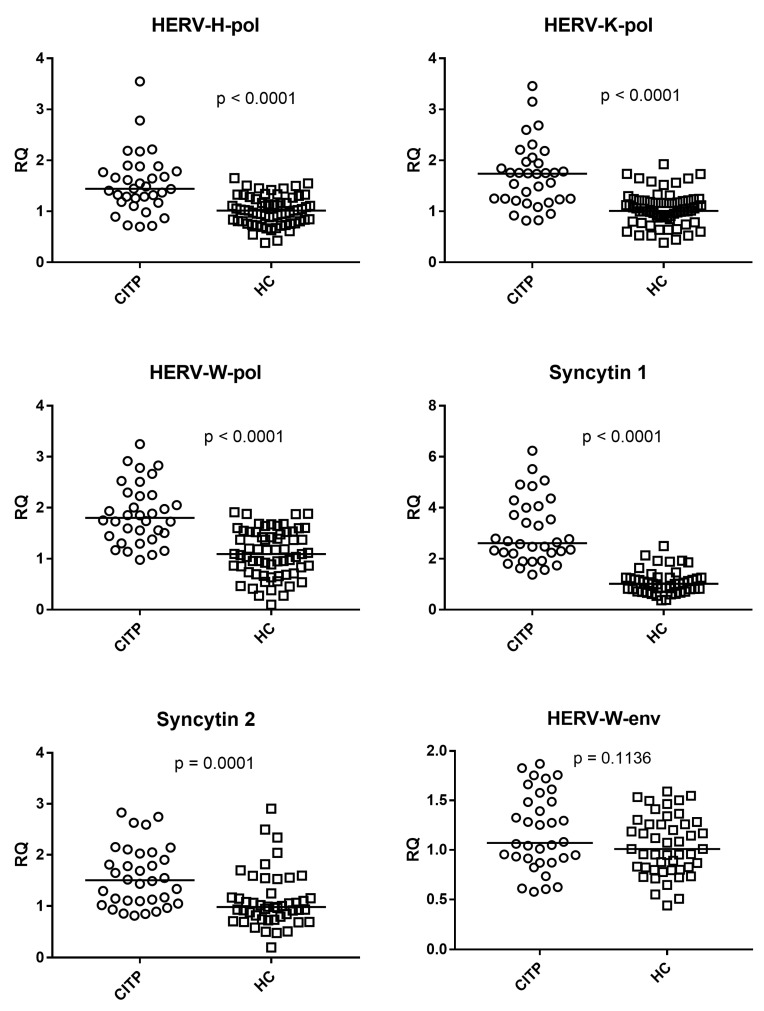
Figure 1 illustrates that the medians of the transcription levels of HERV-H-pol, HERV-K-pol, and HERV-W-pol were significantly higher in patients with CITP (Group A) as compared to 64 healthy controls (Group B1). The same figure also shows that the medians of the mRNA levels of env genes of SYN1 and SYN2 were significantly higher in patients with CITP (Group A) as compared with 47 healthy controls (Group B2), while no statistically significant difference was found for HERV-W-env between the two groups.
Figure 1.
Transcription levels of pol genes of HERV-H, HERV-K, HERV-W and of env genes of Syncytin 1, Syncytin 2, and HERV-W in whole blood from patients with chronic immune thrombocytopenia (CITP) and healthy controls (HC). RQ: Relative Quantification. Circles and squares show the median of three individual measurements, horizontal lines are the median values. Statistical analysis: Mann–Whitney test was used to compare the transcriptional levels of each target gene between children with CITP and HC.
Medians and IQR 25%–75%: HERV-H-pol: Group A median 1.44, IQR 1.20–1.78; Group B1 median 1.02, IQR 0.81–1.27; HERV-K-pol: Group A median 1.74, IQR 1.24–1.96; Group B1 median 1.01, IQR 0.87–1.21; HERV-W-pol: Group A median 1.80, IQR 1.46–2.24; Group B1 median 1.09, IQR 0.73–1.53; SYN1-env: Group A median 2.61, IQR 2.21–3.93; Group B2 median 1.01, IQR 0.81–1.24; SYN2-env: Group A median 1.50, IQR 1.10–1.99; Group B2 median 0.98, IQR 0.77–1.16; HERV-W-env: Group A median 1.07, IQR 0.92–1.49; Group B2 median 1.00, IQR 0.81–1.26.
The values of each HERV RNA quantification for individual patients are reported in Supplementary Table S1.
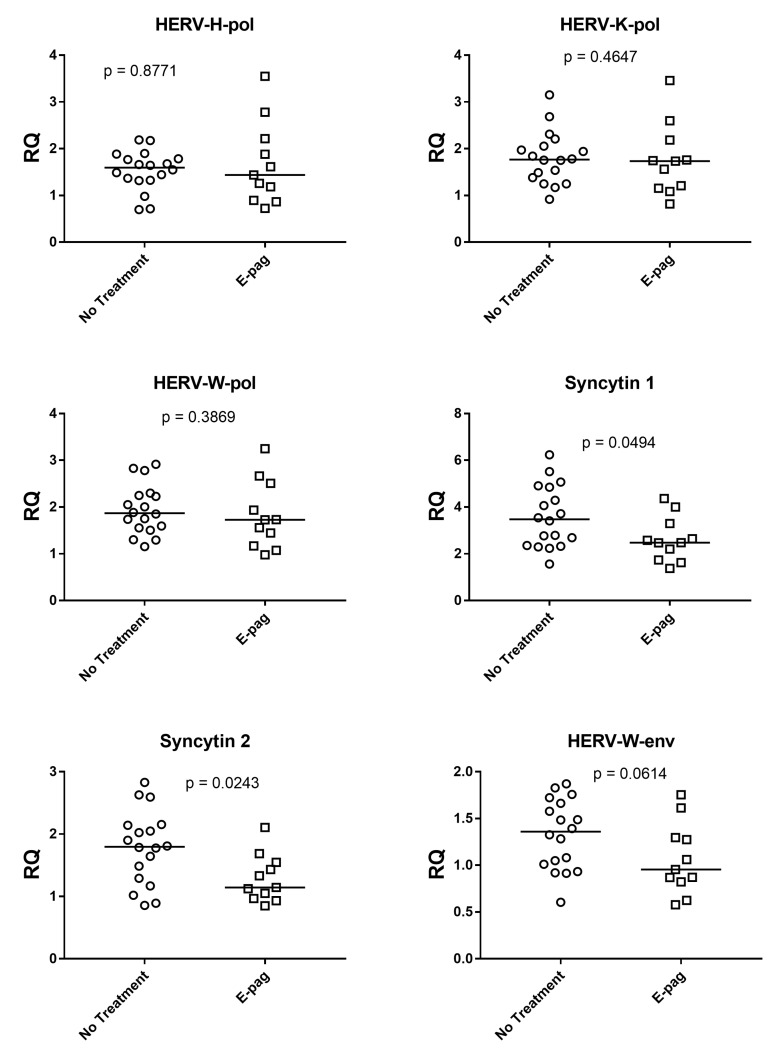
3.4. HERV Expressions in Patients with and without Eltrombopag Treatment
As illustrated in Figure 2, the expressions of SYN1 and SYN2 were inhibited significantly, with borderline p value for HERV-W-env, in the 11 patients on eltrombopag treatment alone as compared to the 18 patients without any treatment (including no administration of steroids or IVIgG). When expressions of HERV-env genes from patients on eltrombopag alone were compared to those from HC, only SYN1 showed significantly higher values (Supplementary Figure S1). No differences were found for HERV-pol genes between patients on eltrombopag treatment alone and those with no therapy. Medians and IQR 25%–75%: SYN1: on eltrombopag (E-pag) median 2.48, IQR 1.97–2.97; no treatment (No-T) median 3.48, IQR 2.44–4.71; SYN2: E-pag median 1.14, IQR 1.01–1.49; No-T median 1.80, IQR 1.34–2.12; HERV-W-env: E-pag median 0.95, IQR 0.85–1.28; No-T median 1.36, IQR 1.02–1.64; HERV-H-pol: E-pag median 1.44, IQR 1.04–2.05; No-T median 1.60, IQR 1.34–1.78; HERV-K-pol: E-pag median 1.73, IQR 1.18–1.97; No-T median 1.77, IQR 1.41–2.03; HERV-W-pol: E-pag median 1.73, IQR 1.31–2.22; No-T median 1.87, IQR 1.56–2.24.
Figure 2.
Transcription levels of pol genes of HERV-H, HERV-K, and HERV-W as well as of env genes of Syncytin 1, Syncytin 2, and HERV-W in whole blood from 11 patients on eltrombopag treatment alone (E-pag) and 18 patients with no treatment. RQ: Relative Quantification. Circles and squares show the median of three individual measurements, horizontal lines are the median values. Statistical analysis: Mann–Whitney test was used to compare the transcriptional levels of each target gene.
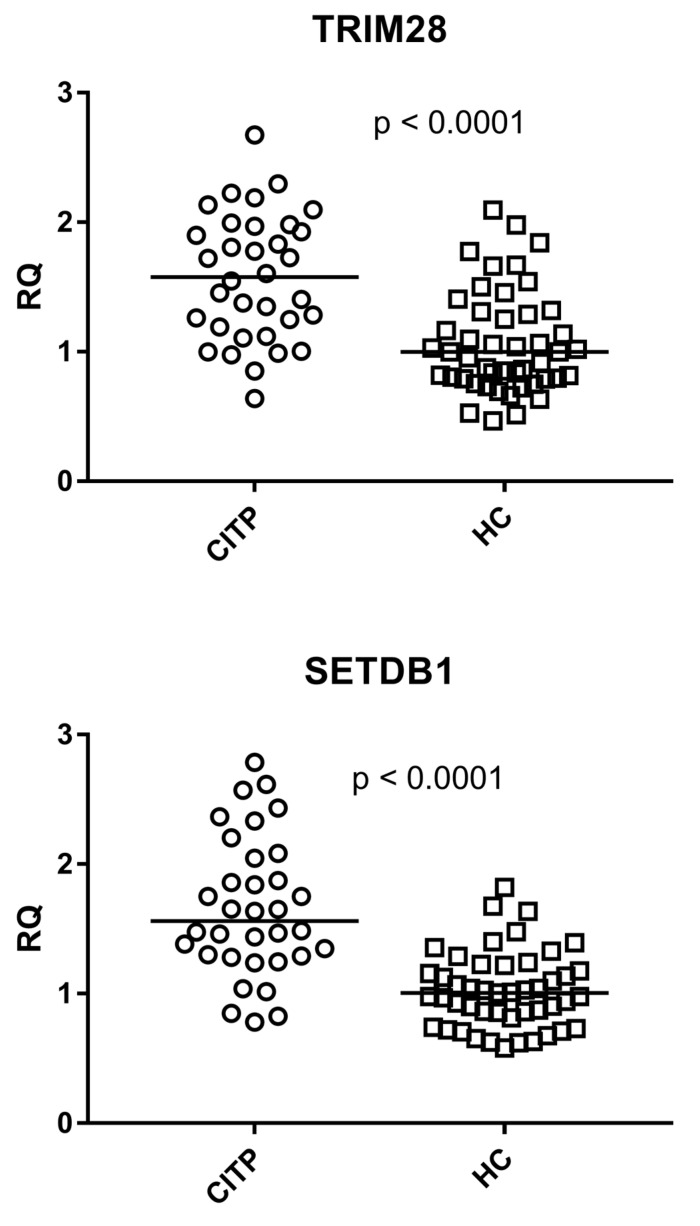
3.5. Expressions of TRIM28 and SETDB1
As detailed in Figure 3, the transcriptional levels of TRIM28 and SETDB1 were significantly higher in patients with CITP (Group A) than HC (Group B2). Medians and IQR 25%–75%: TRIM28: Group A median 1.56, IQR 1.21–1.96; Group B2 median 1.00, IQR 0.79–1.30; SETDB1: Group A median 1.56, IQR 1.29–2.00; Group B2 median 1.00, IQR 0.84–1.20.
Figure 3.
Expression of TRIM28 and SETDB1 in whole blood from 34 patients with chronic immune thrombocytopenia (CITP) and 47 healthy controls (HC). RQ: Relative Quantification. Circles and squares show the median of three individual measurements, horizontal lines are the median values. Statistical analysis: Mann–Whitney test was used to compare the transcriptional levels of each target gene between children with CITP and control children.
The mRNA values of TRIM28 and SETDB1 for individual patients are reported in Supplementary Table S1.
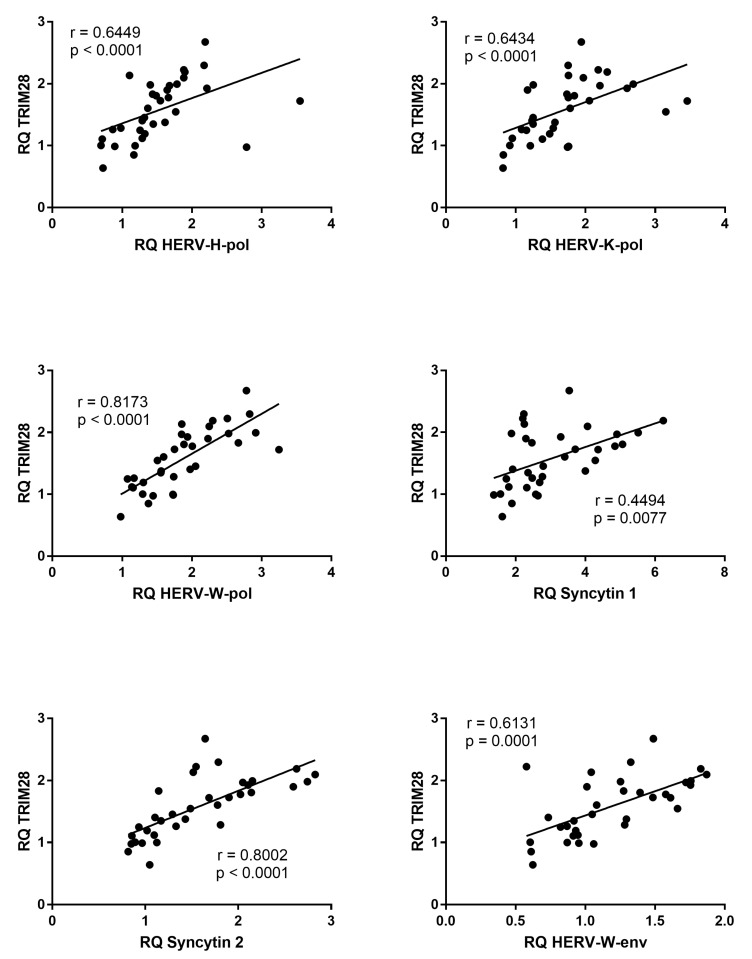
3.6. Correlations between Expressions of TRIM28 and HERVs
The mRNA levels of all HERV sequences positively correlated with the mRNA levels of TRIM28 in patients with CITP (Figure 4), whereas no significant correlations were found in HC (Supplementary Figure S2).
Figure 4.
Correlations between transcription levels of TRIM28 and HERV sequences in whole blood from 34 patients with chronic immune thrombocytopenia. RQ: Relative Quantification. Circles show the mean of three individual measurements. Line: Linear regression line. Statistical analysis: Spearman correlation test.
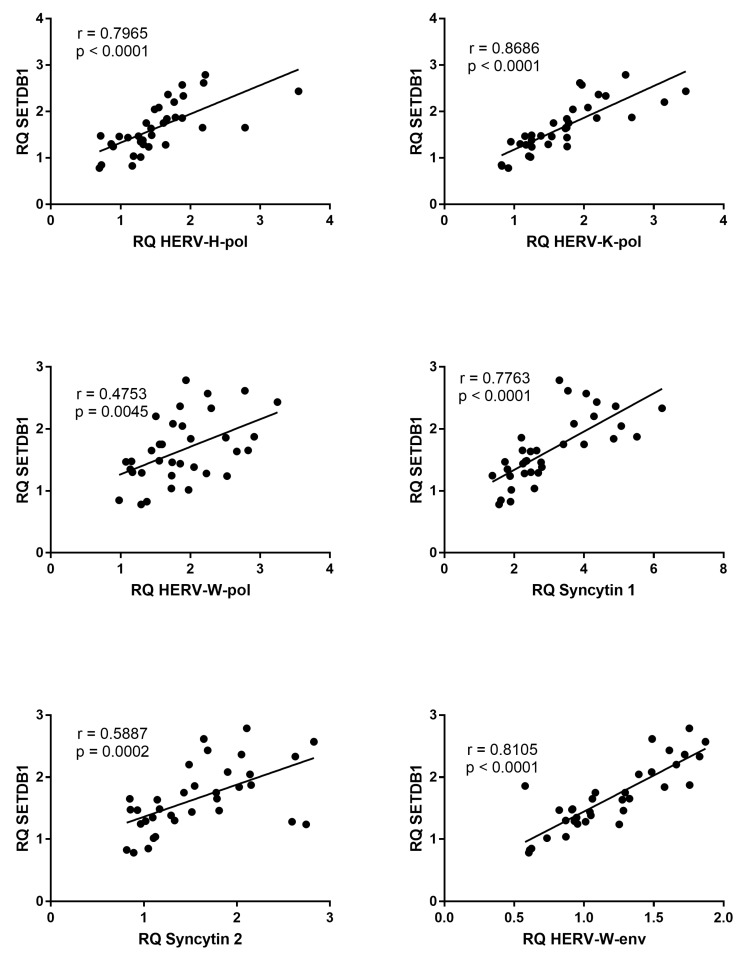
3.7. Correlations between Expressions of SETDB1 and HERVs
The transcription levels of all HERV sequences were positively correlated with those of SETDB1 in patients with CITP (Figure 5); whereas, no significant correlations were found in healthy children (Supplementary Figure S3).
Figure 5.
Correlations between transcription levels of SETDB1 and HERV sequences in whole blood from 34 patients with chronic immune thrombocytopenia. RQ: Relative Quantification. Circles show the mean of three individual measurements. Line: Linear regression line. Statistical analysis: Spearman correlation test.
3.8. Expressions of TRIM28 and SETDB1 in Patients with and without Eltrombopag Treatment
The median transcriptional levels of TRIM28 and SETDB1 were lower in the 11 patients on eltrombopag treatment alone as compared to the 18 patients with no treatment, but they did not reach statistically significant differences, with borderline p value for TRIM28 (Supplementary Figure S4). Medians and IQR 25%–75% of TRIM28: on eltrombopag: median 1.26, IQR 0.99–1.76; no treatment: median 1.75, IQR 1.37–1.99 (p = 0.0682). Medians and IQR 25%–75% of SETDB1: on eltrombopag: median 1.64, IQR 1.27–1.80; no treatment: median 1.80, IQR 1.46–2.17 (p = 0.3397).
4. Discussion
Current results highlight for the first time that children and adolescents with CITP exhibit higher transcriptional levels of pol genes of HERV-H, -K, and -W and env genes of SYN1 and SYN2 in whole blood as compared to age-matched healthy subjects. Some clues that endogenous retroviruses could be involved in inducing alterations in platelet count can be found in the literature. Retrovirus-like particles were detected in lysates of purified platelets [43,44]. Reverse transcriptase activity and HERV-K-pol-related RNAs were found at high levels in platelets of patients with essential thrombocythemia [45]. A HERV-K-gag protein was evidenced in the cytoplasm and viral particles in the cell membrane and into vacuoles of megakaryocytes from two patients with essential thrombocythemia; whereas, none of these elements were found in megakaryocytes from a normal subject [46]. Furthermore, non-autoimmune mice developed microvascular platelet aggregation and thrombocytopenia upon transplantation of a hybridoma clone secreting monoclonal antibodies reactive with an endogenous retroviral env component [47].
The cause and the clinical relevance of the enhanced expression of HERV sequences in CITP children remain elusive. Several experimental studies demonstrate that defective transcription of TRIM28 and SETDB1 may lead to increased HERV activation, via DNA hypomethylation and limited chromatin condensation [38,39]. The mRNA levels of TRIM28 and SETDB1 were, however, not compromised, but increased in our patients, suggesting that the HERV overexpression cannot be ascribed to reduced transcription of TRIM28 or SETDB1. Interestingly enough, no impaired TRIM28/SETDB1 transcriptions were also observed in other settings of children with immune-mediated diseases characterized by upregulation of HERV sequences [33,34,48]. To this purpose, it must be underlined that the protein complex TRIM28/SETDB1 is crucial for keeping endogenous retroviruses in a silent state in pluripotent stem cells and early embryos [49,50]. In contrast, when these cells differentiate into various somatic cells, transcription of retroviral elements becomes independent of such repressors [51], which may also act as transcriptional activators rather than as repressors [52,53]. This might be the case in CITP patients too. In this context, it is worth noting the positive correlations found between mRNA levels of TRIM28 or SETDB1 and HERVs. This suggests that the former might play relevant regulatory functions on the latter. Upstream regulatory pathways could, however, justify the simultaneously increased expression of cellular genes, such as TRIM28/SETDB1, and retroviral sequences. Furthermore, their functional interactions might derive from post-translational conditions between encoded proteins, while we evaluated only their transcriptional landscape.
Viral infections often precede the onset of primary ITP by a few weeks. The virus-driven stimulation of the immune system is thought to be highly implicated in inducing targeted injuries [54,55]. Several viruses, such as herpesviruses [56,57], HIV [58], HCV [33], influenza type A [59], and SARS-CoV-2 [34,60] can trigger HERV transactivation. Exogenous viral infections elicit an inflammatory response via the TLR/NF-kB pathway resulting in the synthesis of interferons (IFNs) and pro-inflammatory cytokines. After passage into the nucleus, NF-kB binds to target elements of HERV proviruses and, with the synergistic action of IFNs and inflammatory cytokines, enhances HERV transcriptions [61]. The HERV expression increases the cell resistance to secondary infections [27], but it exposes the cell to the potential negative effects of endogenous retroviruses. Actually, HERVs can alter the transcription of adjacent cellular genes [25,26]. Their mRNAs can be retro-transcribed into DNA causing significant mutations of cellular genes or, if being sensed as non-self by viral receptors, may induce inflammatory and immune reactions [14]. Furthermore, retroviral epitopes can trigger specific antibodies or share molecular mimicry with a few body tissues [29,30,31,32]. The final result may be an autoimmune-mediated destruction and a defective production of platelets [62]. Actually, a wealth of clinical [21,23,24] and experimental findings [22,63,64] supports the pathogenetic role of HERVs in autoimmune diseases. HERV-encoded proteins are targets of specific reaction in patients with SLE [32]. Higher quantities of surface HERV-H and HERV-W env proteins with specific seroreactivity were found in leukocytes from patients affected by multiple sclerosis [29]. A significant up-regulation in HERV-K mRNA concentrations [65] and enhanced antibody response to a HERV-K-gag [30] and -env [31] peptides were observed in patients with rheumatoid arthritis, while a HERV-K superantigen was detected in those with juvenile arthritis [66].
The number of HERVs with high mRNA levels in CITP patients suggests that their upregulation is a wide and complex phenomenon. As regards the single HERV genes, pol genes of HERV-H, HERV-K, and HERV-W contribute to the production of reverse polymerase, that catalyzes the mRNA retro-transcription into the DNA. This may result in new mutations or dysregulated transcription of cellular genes. It must be underlined that the primers and probes we used revealed preserved sequences of many pol genes from different HERV families, which, however, did not allow outlining of the effects of single HERV loci. SYN1 and SYN2 share syncytial and immunomodulatory properties. They target T-cell activation and significantly suppress T-cell functions [19,20]. SYN1 is usually detectable in all circulating leucocytes; upon stimulation it promotes rapid activation of monocytes [19] and release of chemokines and cytokines [67,68]. Taken together, all these findings support a critical role of HERV over-expressions in CITP. However, as for other immuno-mediated diseases, whether their activation is a cause or an effect of autoimmune reactions remains an unresolved enigma.
Eltrombopag is a nonpeptide thrombopoietin receptor agonist used for treatment of CITP as a highly effective and well-tolerated therapy for achieving hemostatic platelet counts [69,70]. A third of our patients were on eltrombopag therapy alone. Interestingly enough, these patients exhibited significantly impaired transcriptions of SYN1, SYN2, and HERV-W-env as compared to untreated patients. One wonders whether this downregulation of HERV-env sequences may contribute, at least in part, to the positive effects of eltrombopag treatment in patients with CITP.
Epigenetic processes encompass chromatin-based mechanisms in the regulation of gene expression with no structural DNA changes. Environmental factors can cause epigenetic alterations, such as those induced by TRIM28 and SETDB1. TRIM28, through binding to lysine residues of target proteins, causes their phosphorylation and proteasome-driven degradation. TRIM28 recruits SETDB1 for SUMOylation, a post-translational event involved in several cell functions, such as protein degradation, RNA splicing, and transcriptional inhibition [71,72]. TRIM28 and SETDB1 are implicated in a multitude of epigenetic processes [72] and exert relevant actions on both innate and adaptive immune responses [39,40,41]. They influence B cell lineage differentiation and T cell lineage commitment and activation [73,74]. In particular, through the complex with KRAB-ZFPs and forkhead box P3 (Foxp3), TRIM28/SETDB1 control the expansion of T cells into regulatory phenotypes [40,73], conditioning the Treg suppressor activity or distribution of DCs and T cell priming toward inflammatory effector cells [73,75,76]. Notably, Foxp3 gene polymorphisms are also candidate risk factors in autoimmune diseases, including CITP [1,9].
5. Conclusions
Better understanding of the physiopathology of ITP and the failure of tolerance checkpoints responsible for autoantibody formation may open the way to new diagnostic and prognostic approaches and innovative therapeutic strategies. For instance, early detection and longitudinal analysis of the variables here taken into consideration might predict acute or chronic evolution of ITP and allow a patient-tailored therapy. A number of anti-HERV therapeutic strategies might be adopted, such as specific anti-RNAs, monoclonal antibodies, cytotoxic T lymphocytes against HERV antigens, and antiretroviral therapies [77,78,79]. HIV+ subjects are treated for years with cocktails of antiretroviral drugs; their optimal doses and side effects are well-known also in children. In HIV+ subjects, antiretroviral therapy blocks the activation not only of HIV, but also of HERVs [80,81], and resolution of thrombocytopenia has been noticed in coincidence with a specific treatment in a seropositive patient [82]. A combined use of antiretrovirals for six months in patients with amyotrophic lateral sclerosis to block the HERV-K hyperexpression showed an apparent better disease course in those with positive antiviral results [83]. The downregulation of syncytins and HERV-W-env in patients on eltrombopag treatment, if confirmed by targeted studies, may pave the way for its use in patients in whom enhanced activation of HERV-env sequences is thought to be responsible for their pathology. Accumulating evidence highlights that dysregulations in epigenetic mechanisms are involved in the development of CITP. Abnormal epigenetic changes can be targeted by specific small molecule compounds [84]. Therefore, given the strict interactions of HERVs and TRIM28/SETDB1 with the immune system, our results suggest that they might be implicated the physiopathology of CITP and support innovative therapeutic interventions to inhibit their expression in patients affected by CITP unresponsive to standard therapy.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/genes14081569/s1, Supplementary Table S1: Transcription levels of pol genes of HERV-H, HERV-K, and HERV-W; of env genes of Syncytin 1, Syncytin 2, and HERV-W; and of TRIM28 and SETDB1 in whole blood of 34 patients with chronic immune thrombocytopenia. Supplementary Figure S1: Transcription levels of env genes of Syncytin 1, Syncytin 2 and HERV-W in whole blood from 11 patients on Eltrombopag treatment alone and 47 healthy controls. Supplementary Figure S2: Correlations between transcription levels of TRIM28 and HERV sequences in whole blood from healthy controls. Supplementary Figure S3: Correlations between transcription levels of SETDB1 and HERV sequences in whole blood from healthy controls. Supplementary Figure S4: Transcription levels of TRIM28 and SETDB1 in whole blood from 11 patients on Eltrombopag treatment alone and 18 patients with no treatment.
Author Contributions
P.-A.T., U.R. and M.B. (Margherita Branca) conceived and designed the study. P.-A.T. and M.B. (Massimiliano Bergallo) drafted the first manuscript. C.C., S.G., M.D., P.M. and I.G. performed laboratory tests. I.G. and M.B. (Massimiliano Bergallo) performed statistical analyses. E.P., F.L., M.B. (Margherita Branca) and U.R. recruited patients, collected clinical data, and contributed to their analysis. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Clinical data were treated in accordance with the principles of the Helsinki Declaration (World Medical Association General Assembly, Seoul, Republic of Korea, October 2008). The study protocol was approved by the ethics committee of Azienda Ospedaliera-Universitaria Città della Salute e della Scienza, Turin (code 00313 23/07/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The tests were performed using leftovers of laboratory samples; data were gathered anonymously.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Rodeghiero F., Stasi R., Gernsheimer T., Michel M., Provan D., Arnold D.M., Bussel J.B., Cines D.B., Chong B.H., Cooper N., et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: Report from an international working group. Blood. 2009;113:2386–2393. doi: 10.1182/blood-2008-07-162503. [DOI] [PubMed] [Google Scholar]
- 2.Terrell D.R., Beebe L.A., Vesely S.K., Neas B.R., Segal J.B., George J.N. The incidence of immune thrombocytopenic purpura in children and adults: A critical review of published reports. Am. J. Hematol. 2010;85:174–180. doi: 10.1002/ajh.21616. [DOI] [PubMed] [Google Scholar]
- 3.Provan D., Stasi R., Newland A.C., Blanchette V.S., Bolton-maggs P., Bussel J.B., Chong H., Cines D.B., Gernsheimer T.B., Godeau B., et al. Review article International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168–186. doi: 10.1182/blood-2009-06-225565. [DOI] [PubMed] [Google Scholar]
- 4.Imbach P., Kuhne T., Muller D., Berchtold W., Zimmerman S., Elalfy M., Buchanan G.R. ITP: 12 months follow-up data from the prospective registry I of the Intercontinental Childhood ITP Study Group (ICIS). Pediatr. Blood Cancer. 2006;46:351–356. doi: 10.1002/pbc.20453. [DOI] [PubMed] [Google Scholar]
- 5.Glanz J., France E., Xu S., Hayes T., Hambidge S. A population-based, multisite cohort study of the predictors of chronic idiopathic thrombocytopenic purpura in children. Pediatrics. 2008;121:e506–e512. doi: 10.1542/peds.2007-1129. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt D.E., Wendtland Edslev P., Heitink-Pollé K.M.J., Mertens B., Bruin M.C.A., Kapur R., Vidarsson G., van der Schoot C.E., Porcelijn L., van der Bom J.G., et al. A clinical prediction score for transient versus persistent childhood immune thrombocytopenia. J. Thromb. Haemost. 2021;19:121–130. doi: 10.1111/jth.15125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cines D.B., Bussel J.B., Liebman H.A., Luning Prak E.T. The ITP syndrome: Pathogenic and clinical diversity. Blood. 2009;113:6511–6521. doi: 10.1182/blood-2009-01-129155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Provan D., Semple J.W. Recent advances in the mechanisms and treatment of immune thrombocytopenia. EBioMedicine. 2022;76:103820. doi: 10.1016/j.ebiom.2022.103820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang D., Zhang X., Li H., Xue F., Zhang L., Yang R. Association of FOXP3 gene polymorphisms with chronic immune thrombocytopenia in a Chinese Han population. Int. J. Lab. Hematol. 2021;43:1104–1109. doi: 10.1111/ijlh.13525. [DOI] [PubMed] [Google Scholar]
- 10.Swikels M., Rijkers M., Voorberg J., Vidarsson G., Leebeek F.W.G., Jansen A.J.G. Emerging concepts in immune thrombocytopenia. Front. Immunol. 2018;9:880. doi: 10.3389/fimmu.2018.00880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao Y., Cui S., Wang Y., Xu R. The extensive regulation of microRNA in immune thrombocytopenia. Clin. Appl. Thromb. Hemost. 2022;28:10760296221093595. doi: 10.1177/10760296221093595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao H., Xue F., Xu J., Fang Z. Aberrant histone methylation in the patients with immune thrombocytopenia. Platelets. 2014;25:207–210. doi: 10.3109/09537104.2013.859664. [DOI] [PubMed] [Google Scholar]
- 13.Gkoutsias A., Makis A. The role of epigenetics in childhood autoimmune diseases with hematological manifestations. Pediatr. Investig. 2022;6:36–46. doi: 10.1002/ped4.12309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson W.E. Origins and evolutionary consequences of ancient endogenous retroviruses. Nat. Rev. Microbiol. 2019;17:355–370. doi: 10.1038/s41579-019-0189-2. [DOI] [PubMed] [Google Scholar]
- 15.Grow E.J., Flynn R.A., Chavez S.L., Bayless N.L., Wossidlo M., Wesche D.J., Martin L., Ware C.B., Blish C.A., Chang H.Y., et al. Intrinsic retroviral reactivation in human preimplantation embryos and pluripotent cells. Nature. 2015;52:221–225. doi: 10.1038/nature14308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heidmann O., Béguin A., Paternina J., Berthier R., Deloger M., Bawa O., Heidmann T. HEMO, an ancestral endogenous retroviral envelope protein shed in the blood of pregnant women and expressed in pluripotent stem cells and tumors. Proc. Natl. Acad. Sci. USA. 2017;114:E6642–E6651. doi: 10.1073/pnas.1702204114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blond J.L., Lavillette D., Cheynet V., Bouton O., Oriol G., Chapel-Fernandes S., Mandrand B., Mallet F., Cosset F.L. An envelope glycoprotein of the human endogenous HERV-W is expressed in the human placenta and fuses cells expressing the type D mammalian retrovirus receptor. J. Virol. 2000;74:3321–3329. doi: 10.1128/JVI.74.7.3321-3329.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blaise L.S., de Parseval N., Benit L., Heidmann T. Genomewide screening for fusogenic human endogenous retrovirus envelopes identifies syncytin 2, a gene conserved on primate evolution. Proc. Natl. Acad. Sci. USA. 2003;100:13013–13018. doi: 10.1073/pnas.2132646100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Montojo M., Rodriguez-Martin E., Ramos-Mozo P., Ortega-Madueño I., Dominguez-Mozo M.I., Arias-Leal A., García-Martínez M.Á., Casanova I., Galan V., Arroyo R., et al. Syncytin-1/HERV-W envelope is an early activation marker of leukocytes and is upregulated in multiple sclerosis patients. Eur. J. Immunol. 2020;50:685–694. doi: 10.1002/eji.201948423. [DOI] [PubMed] [Google Scholar]
- 20.Lokossou A.G., Toudic C., Nguyen P.T., Elisseeff X., Vargas A., Rassart É., Lafond J., Leduc L., Bourgault S., Gilbert C., et al. Endogenous retrovirus-encoded Syncytin-2 contributes to exosome-mediated immunosuppression of T cells. Biol. Reprod. 2020;102:185–198. doi: 10.1093/biolre/ioz124. [DOI] [PubMed] [Google Scholar]
- 21.Ukadike K.C., Mustelin T. Implications of endogenous retroelements in the etiopathogenesis of systemic lupus erythematosus. J. Clin. Med. 2021;10:856. doi: 10.3390/jcm10040856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perron H., Dougier-Reynaud H.L., Lomparski C., Popa I., Firouzi R., Bertrand J.B., Marusic S., Portoukalian J., Jouvin-Marche E., Villiers C.L., et al. Human endogenous retrovirus protein activates innate immunity and promotes experimental allergic encephalomyelitis in mice. PLoS ONE. 2013;8:e80128. doi: 10.1371/journal.pone.0080128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tovo P.A., Rabbone I., Tinti D., Galliano I., Trada M., Daprà V., Cerutti F., Bergallo M. Enhanced expression of human endogenous retroviruses in new-onset type 1 diabetes: Potential pathogenetic and therapeutic implications. Autoimmunity. 2020;53:283–288. doi: 10.1080/08916934.2020.1777281. [DOI] [PubMed] [Google Scholar]
- 24.Tovo P.A., Opramolla A., Pizzol A., Calosso G., Daprà V., Galliano I., Calvi C., Pinon M., Cisarò F., Rigazio C., et al. Overexpression of endogenous retroviruses in children with celiac disease. Eur. J. Pediatr. 2021;180:2429–2434. doi: 10.1007/s00431-021-04050-x. [DOI] [PubMed] [Google Scholar]
- 25.Isbel L., Whitelaw E. Endogenous retroviruses in mammals: An emerging picture of how ERVs modify expression of adjacent genes. Bioessays. 2012;34:734–738. doi: 10.1002/bies.201200056. [DOI] [PubMed] [Google Scholar]
- 26.Chuong E.B., Elde N.C., Feschotte C. Regulatory evolution of innate immunity through co-option of endogenous retroviruses. Science. 2016;351:1083–1087. doi: 10.1126/science.aad5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rolland A., Jouvin-Marche E., Viret C., Faure M., Perron H., Marche P.N. The envelope protein of a human endogenous retrovirus-W family activates innate immunity through CD14/TLR4 and promotes Th1-like responses. J. Immunol. 2006;176:7636–7644. doi: 10.4049/jimmunol.176.12.7636. [DOI] [PubMed] [Google Scholar]
- 28.Dembny P., Newman A.G., Singh M., Hinz M., Szczepek M., Krüger C., Adalbert R., Dzaye O., Trimbuch T., Wallach T., et al. Human endogenous retrovirus HERV-K(HML-2) RNA causes neurodegeneration through Toll-like receptors. JCI Insight. 2020;5:e131093. doi: 10.1172/jci.insight.131093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brudek T., Christensen T., Aagaard L., Petersen T., Hansen H.J., Møller-Larsen A. B cells and monocytes from patients with active multiple sclerosis exhibit increased surface expression of both HERV-H env and HERV-W env, accompanied by increased seroreactivity. Retrovirology. 2009;6:104. doi: 10.1186/1742-4690-6-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nelson P.N., Roden D., Nevill A., Freimanis G.L., Trela M., Ejtehadi H.D., Bowman S., Axford J., Veitch A.M., Tugnet N., et al. Rheumatoid arthritis is associated with IgG antibodies to human endogenous retrovirus gag matrix: A potential pathogenic mechanism of disease? J. Rheumatol. 2014;41:1952–1960. doi: 10.3899/jrheum.130502. [DOI] [PubMed] [Google Scholar]
- 31.Mameli G., Erre G.L., Caggiu E., Mura S., Cossu D., Bo M., Cadoni M.L., Piras A., Mundula N., Colombo E., et al. Identification of a HERV-K env surface peptide highly recognized in rheumatoid arthritis (RA) patients: A cross-sectional case–control study. Clin. Exp. Immunol. 2017;189:127–131. doi: 10.1111/cei.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perl A., Nagy G., Koncz A., Gergely P., Fernandez D., Doherty E., Telarico T., Bonilla E., Phillips P.E. Molecular mimicry and immunomodulation by the HRES-1 endogenous retrovirus in SLE. Autoimmunity. 2008;41:287–297. doi: 10.1080/08916930802024764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tovo P.A., Garazzino S., Daprà V., Alliaudi C., Silvestro E., Calvi C., Montanari P., Galliano I., Bergallo M. Chronic HCV infection is associated with overexpression of human endogenous retroviruses that persists after drug-induced viral clearance. Int. J. Mol. Sci. 2020;21:3980. doi: 10.3390/ijms21113980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tovo P.A., Garazzino S., Daprà V., Pruccoli G., Calvi C., Mignone F., Alliaudi C., Denina M., Scolfaro C., Zoppo M., et al. COVID-19 in children: Expressions of type I/II/III interferons, TRIM28, SETDB1, and endogenous retroviruses in mild and severe cases. Int. J. Mol. Sci. 2021;22:7481. doi: 10.3390/ijms22147481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Friedman J.R., Fredericks W.J., Jensen D.E., Speicher D.W., Huang X.P., Neilson E.G., Rauscher F.J. 3rd. KAP-1, a novel corepressor for the highly conserved KRAB repression domain. Genes Dev. 1996;10:2067–2078. doi: 10.1101/gad.10.16.2067. [DOI] [PubMed] [Google Scholar]
- 36.Sobocinska J., Molenda S., Machnik M., Oleksiewicz U. KRAB-ZFP transcriptional regulators acting as oncogenes and tumor suppressors: An Overview. Int. J. Mol. Sci. 2021;23:2212. doi: 10.3390/ijms22042212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schultz D.C., Ayyanathan K., Negorev D., Maul G.G., Rauscher F.J. 3rd. SETDB1: A novel KAP-1-associated histone H3, lysine 9-specific methyltransferase that contributes to HP1-mediated silencing of euchromatic genes by KRAB zinc-finger proteins. Genes Dev. 2002;16:919–932. doi: 10.1101/gad.973302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turelli P., Castro-Diaz N., Marzetta F., Kapopoulou A., Raclot C., Duc J., Tieng V., Quenneville S., Trono D. Interplay of TRIM28 and DNA methylation in controlling human endogenous retroelements. Genome Res. 2014;24:1260–1270. doi: 10.1101/gr.172833.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang Y., Liu Y., Lu H., Sun S.C., Jin W., Wang X., Dong C. Epigenetic activation during T helper 17 cell differentiation is mediated by Tripartite motif containing 28. Nat. Commun. 2018;12:1424. doi: 10.1038/s41467-018-03852-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gehrmann U., Carpier J.M., Burgdorf N., Hoyler T., Suarez G., Joannas L., Heurtebise-Chrétien S., Durand S., Panes R., Bellemare-Pelletier A., et al. Critical role for TRIM28 and HP1/in the epigenetic control of T cell metabolic reprograming and effector differentiation. Proc. Natl. Acad. Sci. USA. 2019;116:25839–25849. doi: 10.1073/pnas.1901639116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adoue V., Binet B., Malbec A., Fourquet J., Romagnoli P., van Meerwijk J.P.M., Amigorena S., Joffre O.P. The histone methyltransferase SETDB1 controls T helper cell lineage integrity by repressing endogenous retroviruses. Immunity. 2019;50:629–644. doi: 10.1016/j.immuni.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 42.Livak K.J., Schmittgenb T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2-DDCT method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 43.Brodsky I., Fuscaldo A.A., Erlick B.J., Kingsbury E.W., Schultz G.M., Fuscaldo K.E. Analysis of platelets from patients with thrombocythemia for reverse transcriptase and virus-like particles. J. Natl. Cancer Inst. 1975;55:1069. doi: 10.1093/jnci/55.5.1069. [DOI] [PubMed] [Google Scholar]
- 44.Brodsky I., Fuscaldo A.A., Erlick B.J., Fuscaldo K.E. Effect of busulfan on oncornavirus-like activity in platelets and chromosomes in polycythemia vera and essential thrombocythemia. J. Natl. Cancer Inst. 1977;59:61. doi: 10.1093/jnci/59.1.61. [DOI] [PubMed] [Google Scholar]
- 45.Boyd M.T., Foley B., Brodsky I. Evidence for copurification of HERV-K-related transcripts and a reverse transcriptase activity in human platelets from patients with essential thrombocythemia. Blood. 1997;90:4022–4030. doi: 10.1182/blood.V90.10.4022. [DOI] [PubMed] [Google Scholar]
- 46.Morgan D., Brodsky I. Human endogenous retrovirus (HERV-K)eg particles in megakaryocytes cultured from essential thromocythemia peripheral blood stem cells. Exp. Hematol. 2004;32:520–525. doi: 10.1016/j.exphem.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Miyazawa M., Tabata N., Fujisawa R., Hashimoto K., Shiwaku H., Takei Y.A. Roles of endogenous retroviruses and platelets in the development of vascular injury in spontaneous mouse models of autoimmune diseases. Int. J. Cardiol. 2000;75((Suppl. 1)):S65–S73. doi: 10.1016/S0167-5273(00)00193-5. [DOI] [PubMed] [Google Scholar]
- 48.Tovo P.A., Monti G., Daprà V., Montanari P., Calvi C., Alliaudi C., Sardo A., Galliano I., Bergallo M. Enhanced expression of endogenous retroviruses and of TRIM28 and SETDB1 in children with food allergy. Clin. Transl. Allergy. 2022;12:e12124. doi: 10.1002/clt2.12124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matsui T., Leung D., Miyashita H., Maksakova I.A., Miyachi H., Kimura H., Tachibana M., Lorincz M.C., Shinkai Y. Proviral silencing in embryonic stem cells requires the histone methyltransferase ESET. Nature. 2010;464:927–931. doi: 10.1038/nature08858. [DOI] [PubMed] [Google Scholar]
- 50.Rowe H.M., Kapopoulou A., Corsinotti A., Fasching L., Macfarlan T., Tarabay Y., Viville S., Jakobsson J., Pfaff S.L., Trono D. TRIM28 repression of retrotransposon-based enhancers is necessary to preserve transcriptional dynamics in embryonic stem cells. Genome Res. 2013;23:452–461. doi: 10.1101/gr.147678.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wiznerowicz M., Jakobsson J., Szulc J., Liao S., Quazzola A., Beermann F., Aebischer P., Trono D. The Kruppel-associated box repressor domain can trigger de novo promoter methylation during mouse early embryogenesis. J. Biol. Chem. 2007;282:34535–34541. doi: 10.1074/jbc.M705898200. [DOI] [PubMed] [Google Scholar]
- 52.Santoni de Sio F.R., Barde I., Offner S., Kapopoulou A., Corsinotti A., Bojkowska K., Genolet R., Thomas J.H., Luescher I.F., Pinschewer D., et al. KAP1 regulates gene networks controlling T-cell development and responsiveness. FASEB J. 2012;26:4561–4575. doi: 10.1096/fj.12-206177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Randolph K., Hyder U., D’Orso I. KAP1/TRIM28: Transcriptional activator and/or repressor of viral and cellular programs? Front. Cell Infect. Microbiol. 2022;12:834636. doi: 10.3389/fcimb.2022.834636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chabert A., Hamzeh-Cognasse H., Pozzetto B., Cognasse F., Schattner M., Gomez R.M., Garraud O. Human platelets and their capacity of binding viruses: Meaning and challenges? BMC Immunol. 2015;16:26. doi: 10.1186/s12865-015-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Raadsen M., Du Toit J., Langerak T., van Bussel B., van Gorp E., Goeijenbier M. Thrombocytopenia in virus infections. J. Clin. Med. 2021;10:877. doi: 10.3390/jcm10040877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mameli G., Poddighe L., Mei A., Uleri E., Sotgiu S., Serra C., Manetti R., Dolei A. Expression and activation by Epstein Barr virus of human endogenous retroviruses-W in blood cells and astrocytes: Inference for multiple sclerosis. PLoS ONE. 2012;7:e44991. doi: 10.1371/journal.pone.0044991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Assinger A., Yaiw K.C., Göttesdorfer I., Leib-Mösch C., Söderberg-Nauclér C. Human cytomegalovirus (HCMV) induces human endogenous retrovirus (HERV) transcription. Retrovirology. 2013;10:132. doi: 10.1186/1742-4690-10-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Van der Kuyl A.C. HIV infection and HERV expression: A review. Retrovirology. 2012;9:6. doi: 10.1186/1742-4690-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu H., Bergant V., Frishman G., Ruepp A., Pichlmair A., Vincendeau M., Frishman D. Influenza A virus infection reactivates human endogenous retroviruses associated with modulation of antiviral immunity. Viruses. 2022;14:1591. doi: 10.3390/v14071591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marston J.L., Greenig M., Singh M., Bendall M.L., Duarte R.R.R., Feschotte C., Iñiguez L.P., Nixon D.F. SARS-CoV-2 infection mediates differential expression of human endogenous retroviruses and long interspersed nuclear elements. JCI Insight. 2021;6:e147170. doi: 10.1172/jci.insight.147170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Manghera M., Ferguson-Parry J., Lin R., Douville R.N. NF-κB and IRF1 induce endogenous retrovirus K expression via interferon-stimulated response elements in its 5' long terminal repeat. J. Virol. 2016;90:9338–9349. doi: 10.1128/JVI.01503-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khodadi E., Asnafi A.A., Shahrabi S., Shahjahani M., Saki N. Bone marrow niche in immune thrombocytopenia: A focus on megakaryopoiesis. Ann. Hematol. 2016;95:1765–1776. doi: 10.1007/s00277-016-2703-1. [DOI] [PubMed] [Google Scholar]
- 63.Ito K., Baudino L., Kihara M., Leroy V., Vyse T.J., Evans L.H., Izui S. Three Sgp loci act independently as well as synergistically to elevate the expression of specific endogenous retroviruses implicated in murine lupus. J. Autoimmun. 2013;43:10–17. doi: 10.1016/j.jaut.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bashratyan R., Regn D., Rahman M.J., Marquardt K., Fink E., Hu W.Y., Elder J.H., Binley J., Sherman L.A., Dai Y.D. Type 1 diabetes pathogenesis is modulated by spontaneous autoimmune responses to endogenous retrovirus antigens in NOD mice. Eur. J. Immunol. 2017;47:575–584. doi: 10.1002/eji.201646755. [DOI] [PubMed] [Google Scholar]
- 65.Freimanis G., Hooley P., Ejtehadi H.D., Ali H.A., Veitch A., Rylance P.B., Alawi A., Axford J., Nevill A., Murray P.G., et al. A role for human endogenous retrovirus-K (HML-2) in rheumatoid arthritis: Investigating mechanisms of pathogenesis. Clin. Exp. Immunol. 2010;160:340–347. doi: 10.1111/j.1365-2249.2010.04110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sicat J., Sutkowski N., Huber B.T. Expression of human endogenous retrovirus HERV-K18 superantigen is elevated in juvenile rheumatoid arthritis. J. Rheumatol. 2005;32:1821–1831. [PubMed] [Google Scholar]
- 67.Tolosa J.M., Parsons K.S., Hansbro P.M., Smith R., Wark P.A. The placental protein syncytin-1 impairs antiviral responses and exaggerates inflammatory responses to influenza. PLoS ONE. 2015;10:e0118629. doi: 10.1371/journal.pone.0118629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X., Liu Z., Wang P., Li S., Zeng J., Tu X., Yan Q., Xiao Z., Pan M., Zhu F. Syncytin-1, an endogenous retroviral protein, triggers the activation of CRP via TLR3 signal cascade in glial cells. Brain Behav. Immun. 2018;67:324–334. doi: 10.1016/j.bbi.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 69.Bussel J.B., Cheng G., Saleh M.N., Psaila B., Kovaleva L., Meddeb B., Kloczko J., Hassani H., Mayer B., Stone N.L., et al. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N. Engl. J. Med. 2007;357:2237–2247. doi: 10.1056/NEJMoa073275. [DOI] [PubMed] [Google Scholar]
- 70.Giordano P., Lassandro G., Barone A., Cesaro S., Fotzi I., Giona F., Ladogana S., Miano M., Marzollo A., Nardi M., et al. Use of Eltrombopag in children with chronic immune thrombocytopenia (ITP): A real life retrospective multicenter experience of the Italian Association of Pediatric Hematology and Oncology (AIEOP) Front. Med. 2020;7:66. doi: 10.3389/fmed.2020.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liang Q., Deng H., Li X., Wu X., Tang Q., Chang T.H., Peng H., Rauscher F.J., 3rd, Ozato K., Zhu F. Tripartite motif-containing protein 28 is a small ubiquitin-related modifier E3 ligase and negative regulator of IFN regulatory factor 7. J. Immunol. 2011;187:4754–4763. doi: 10.4049/jimmunol.1101704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Krischuns T., Günl F., Henschel L., Binder M., Willemsen J., Schloer S., Rescher U., Gerlt V., Zimmer G., Nordhoff C., et al. Phosphorylation of TRIM28 enhances the expression of IFN-β and proinflammatory cytokines during HPAIV infection of human lung epithelial cells. Front. Immunol. 2018;9:2229. doi: 10.3389/fimmu.2018.02229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou X.F., Yu J., Chang M., Zhang M., Zhou D., Cammas F., Sun S.C. TRIM28 mediates chromatin modifications at the TCRα enhancer and regulates the development of T and natural killer T cells. Proc. Natl. Acad. Sci. USA. 2012;109:20083–20088. doi: 10.1073/pnas.1214704109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Takikita S., Muro R., Takai T., Otsubo T., Kawamura Y.I., Dohi T., Oda H., Kitajima M., Oshima K., Hattori M., et al. A Histone methyltransferase ESET is critical for T cell development. J. Immunol. 2016;197:2269–2279. doi: 10.4049/jimmunol.1502486. [DOI] [PubMed] [Google Scholar]
- 75.Huang C., Martin S., Pfleger C., Du J., Buckner J.H., Bluestone J.A., Riley J.L., Ziegler S.F. Cutting Edge: A novel, human-specific interacting protein couples FOXP3 to a chromatin-remodeling complex that contains KAP1/TRIM28. J. Immunol. 2013;190:4470–4473. doi: 10.4049/jimmunol.1203561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chikuma S., Yamanaka S., Nakagawa S., Ueda M.T., Hayabuchi H., Tokifuji Y., Kanayama M., Okamura T., Arase H., Yoshimura A. TRIM28 expression on dendritic cells prevents excessive T cell priming by silencing endogenous retrovirus. J. Immunol. 2021;206:1528–1539. doi: 10.4049/jimmunol.2001003. [DOI] [PubMed] [Google Scholar]
- 77.Hartung H.P., Derfuss T., Cree B.A., Sormani M.P., Selmaj K., Stutters J., Prados F., MacManus D., Schneble H.M., Lambert E., et al. Efficacy and safety of temelimab in multiple sclerosis: Results of a randomized phase 2b and extension study. Mult. Scler. 2021;9:422–440. doi: 10.1177/13524585211024997. [DOI] [PubMed] [Google Scholar]
- 78.Giménez-Orenga K., Oltra E. Human endogenous retrovirus as therapeutic targets in neurologic disease. Pharmaceuticals. 2021;14:495. doi: 10.3390/ph14060495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Baldwin E.T., Götte M., Tchesnokov E.P., Arnold E., Hagel M., Nichols C., Dossang P., Lamers M., Wan P., Steinbacher S., et al. Human endogenous retrovirus-K (HERV-K) reverse transcriptase (RT) structure and biochemistry reveals remarkable similarities to HIV-1 RT and opportunities for HERV-K-specific inhibition. Proc. Natl. Acad. Sci. USA. 2022;119:e2200260119. doi: 10.1073/pnas.2200260119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Laderoute M.P., Giulivi A., Larocque L., Bellfoy D., Hou Y., Wu H.X., Fowke K., Wu J., Diaz-Mitoma F. The replicative activity of human endogenous retrovirus K102 (HERV-K102) with HIV viremia. AIDS. 2007;21:2417–2424. doi: 10.1097/QAD.0b013e3282f14d64. [DOI] [PubMed] [Google Scholar]
- 81.Bowen L.N., Tyagi R., Li W., Alfahad T., Smith B., Wright M., Singer E.J., Nath A. HIV-associated motor neuron disease: HERV-K activation and response to antiretroviral therapy. Neurology. 2016;87:1756–1762. doi: 10.1212/WNL.0000000000003258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gentile I., Bonadies G., Buonomo A.R., Minei G., Borrelli F., Foggia M., Chiurazzi F., Borgia G. Resolution of autoimmune thrombocytopenia associated with raltegravir use in an HIV-positive patient. Platelets. 2013;2:574–577. doi: 10.3109/09537104.2012.735721. [DOI] [PubMed] [Google Scholar]
- 83.Garcia-Montojo M., Fathi S., Norato G., Smith B.R., Rowe D.B., Kiernan M.C., Vucic S., Mathers S., van Eijk R.P.A., Santamaria U., et al. Inhibition of HERV-K (HML-2) in amyotrophic lateral sclerosis patients on antiretroviral therapy. J. Neurol. Sci. 2021;423:17358. doi: 10.1016/j.jns.2021.117358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garcia-Martinez L., Zhang Y., Nakata Y., Chan H.L., Morey L. Epigenetic mechanisms in breast cancer therapy and resistance. Nat. Commun. 2021;12:786. doi: 10.1038/s41467-021-22024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.