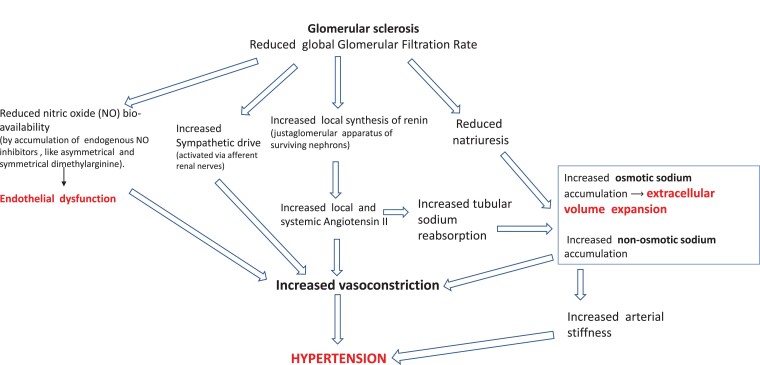
Figure 3.
Main pathophysiological alterations leading to hypertension in CKD. High renin and aldosterone levels are common among CKD patients. Angiotensin II, a direct vasoconstrictor, increases vascular resistance and arterial pressure. Angiotensin II also enhances, in a direct manner, sodium reabsorption in the proximal tubule and stimulates via aldosterone hypersecretion sodium reabsorption in the collecting duct. Furthermore, renal function loss per se reduces sodium excretion, which amplifies sodium retention. Non-osmotic sodium accumulation activates pro-hypertensive mechanisms via the inflammatory-immune system (see text). Due to sodium retention and volume expansion secondary to reduced GFR, endogenous cardiotonic steroids (ouabain and other ouabain-like steroids) are increased in CKD patients. High levels of these steroid compounds contribute to raise BP by impairing vasodilatory mechanisms.