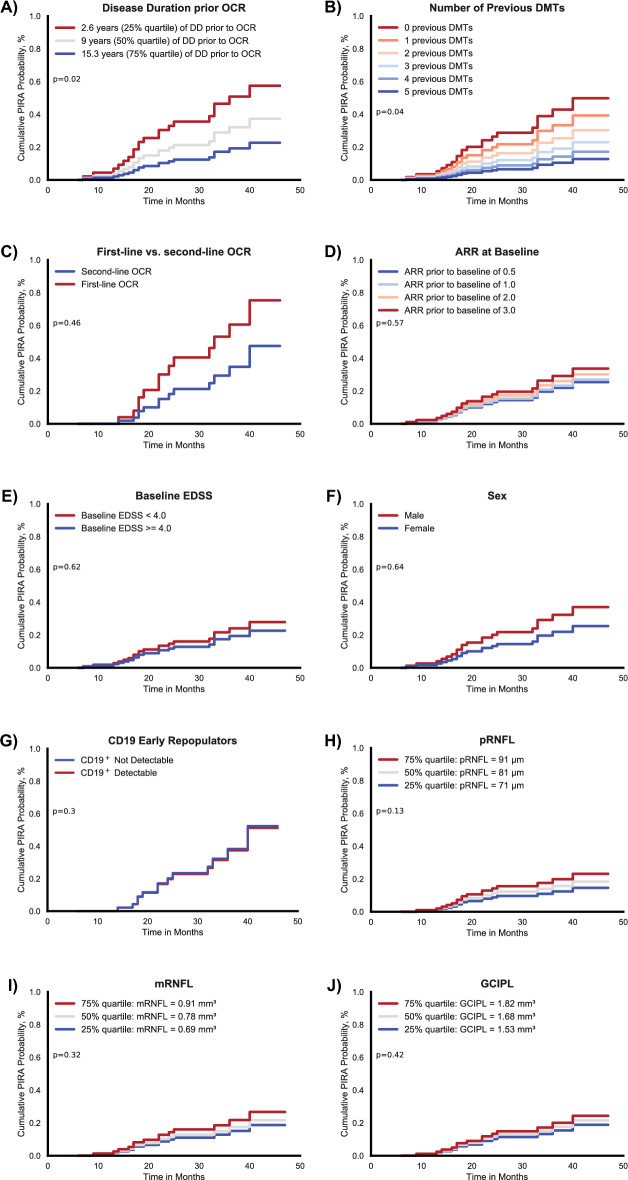
Figure 4.
Factors associated with PIRA development probability. Kaplan-Meyer estimates of clinical, demographical, and OCT factors associated with PIRA event probabilities. The panels (A)–(I) depict the cumulative probabilities of developing PIRA according to different categories: (A) Disease duration prior to ocrelizumab stratified by quartiles (2.6 years, 9 years, 15.3 years). A shorter disease duration showed a significantly increased probability to developing PIRA (p = 0.02). (B) Number of DMTs used previously to ocrelizumab. Less previous DMTs was associated to a higher PIRA probability (p = 0.04). Other factors did not show significant alterations in PIRA probability: (C) Ocrelizumab as a first-line therapy vs. second-line, (D) ARR in the 2 years prior to ocrelizumab initiation, (E) EDSS at ocrelizumab initiation, (F) male vs. female and detectability of CD19+ cells in blood counts 6–12 months after OCR initiation (G). OCT based retinal measures were also not significantly associated with PIRA development probability with (H) showing peripapillary RNFL thickness, (I) showing macular RNFL volume and (J) showing macular GCIPL volume. OCT factors were stratified by quartiles with the worse of the two eyes taken into analysis. PIRA progression independent of relapse activity; OCR ocrelizumab; DD disease duration; DMTs disease-modifying therapies; ARR annualized relapse rate; EDSS expanded disability status scale; pRNFL peripapillary retinal nerve fiber layer; mRNFL macular retinal nerve fiber layer; mGCIPL macular ganglion cell and inner plexiform layer.