Figure 3. Neutrophil function and heterogeneity in oral mucosa.
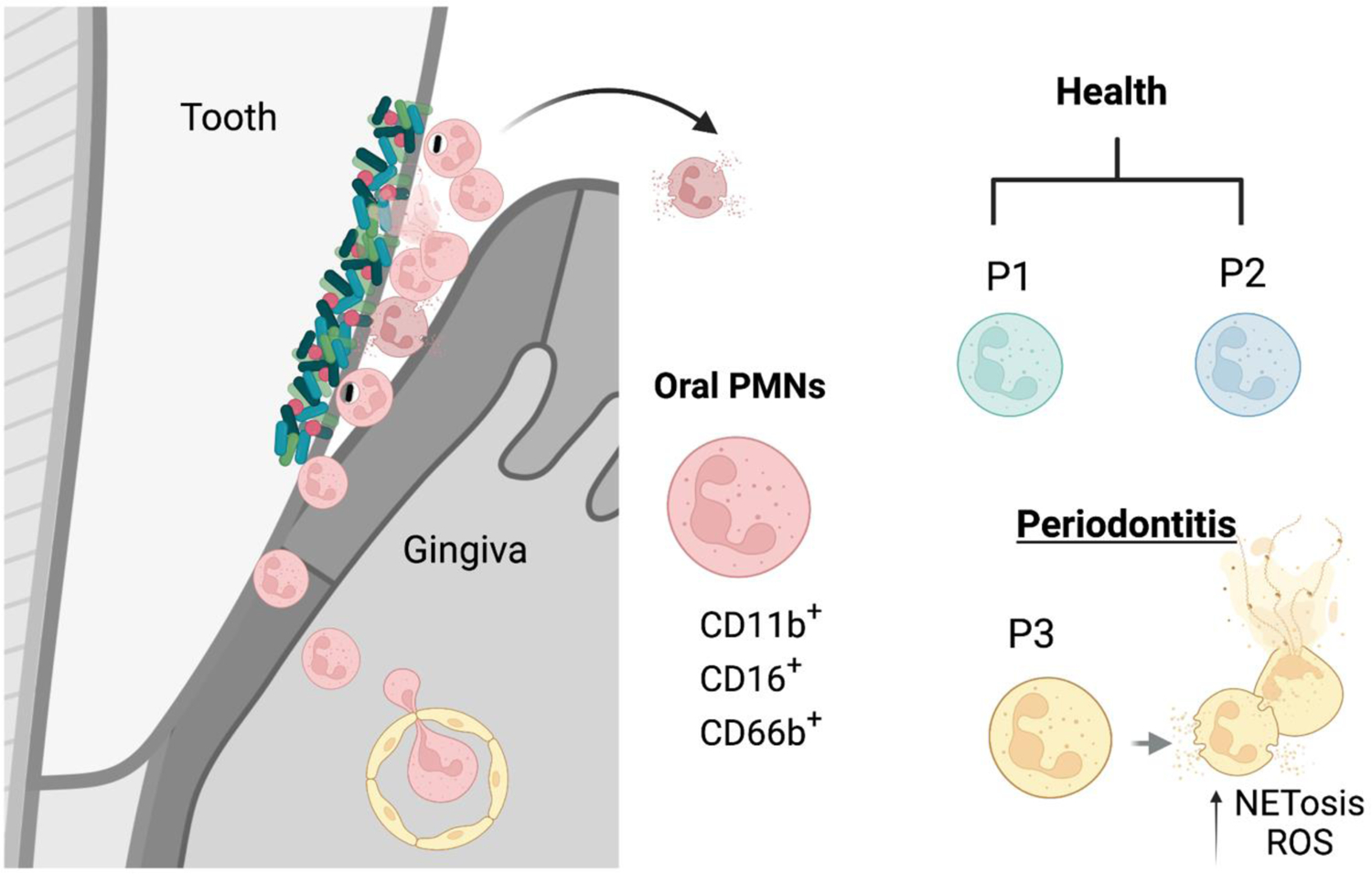
The gingival crevice, the epithelium of the periodontal pocket, is a site of constant transmigration of neutrophils even in health. Neutrophils constantly transmigrate from the vasculature to the gingival tissue and through the bottom of the pocket into the oral cavity. This tissue has a great extent of homeostatic inflammation that is primarily characterized by neutrophil responses. Neutrophils transmigrating into the oral cavity have been subclassified into two populations of health-associated para-inflammatory neutrophils (P1 and P2) and a proinflammatory subtype (P3) in periodontitis. Oral neutrophils express CD11b, CD16, CD66 and varying levels of CD10, CD18, CD55, CD63, CD64, and CD170. P3 neutrophils in particularly are characterized by increased expression of activation markers and increased propensity towards ROS production and NETosis.
